ABSTRACT
In vitro susceptibilities for 47 antibiotics were determined in 30 genetic diverse strains of Francisella tularensis by the broth microdilution method following Clinical and Laboratory Standards Institute (CLSI) methods. The F. tularensis strains demonstrated susceptibility to aminoglycosides, fluoroquinolones, and tetracyclines. There was a distinct difference in macrolide susceptibilities between A and B type strains, as has been noted previously. The establishment and comparison of antibiotic susceptibilities of a diverse but specific set of F. tularensis strains by standardized methods and the establishment of population ranges and MIC50/90 values provide reference information for assessing new antibiotic agents and a baseline to monitor any future emergence of resistance, whether natural or intentional.
KEYWORDS: Francisella tularensis, antibiotics, susceptibility testing
TEXT
Francisella tularensis is the causative agent of tularemia, a zoonotic infection in humans, usually transmitted as a result of contact with infected animals or insect bites (1). It also has potential misuse in biowarfare and bioterrorism (2). While the disease is not usually fatal, underlying medical conditions can lead to possibly fatal complications. Antibiotic therapy usually resolves the infection (1). The species is also divided into several biovars, based on metabolic differences, virulence, and geographic location (3). There is scattered information on MICs under a variety of nonstandardized testing conditions, with mostly type B (F. tularensis subsp. holarctica) strains (4–15). A more recent report utilizing standardized testing methods with a variety of North American type A strains (16) has provided some additional data; however, this study looked at only eight antibiotics representing five classes. With a lack of comparative data on type strains and with a variety of antibiotic classes, we report here specific antibiotic susceptibility results according to Clinical and Laboratory Standards Institute (CLSI) microdilution broth methodology for 30 strains of F. tularensis (17). This information will be highly useful as baseline data in the event of wartime or terrorist release, as well as for naturally acquired and laboratory-acquired infections.
The F. tularensis strains used in this study are shown in Table 1, and they were obtained from the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) collection and selected to represent the established biovars and geographic diversity (18). Most antibiotics were obtained from U.S. Pharmacopoeia (Rockville, MD), with the following exceptions: ceftriaxone and fusidic acid were from Sigma Chemical Co. (St. Louis, MO), cethromycin was from Advanced Life Sciences; telithromycin was from Sanofi-Aventis, garenoxacin was from Schering-Plough, gemifloxacin was from Oscient, ertapenem was from Merck, faropenem was from Replidyne, and tigecycline was from Wyeth. Most stock solutions (5 mg/ml) were prepared for each drug in the appropriate solvents, based on the current CLSI recommendations (19), and stored at −70°C until use. The amoxicillin-clavulanate (2:1) stock was 5 mg/2.5 mg per ml. The co-trimoxazole stock contained 5 mg/ml sulfamethoxazole and 0.26 mg/ml trimethoprim (19:1). MICs were determined by the microdilution method in 96-well plates, as previously described (20), with the exception of the addition of IsoVitaleX (Becton Dickinson) to a final concentration of 2% (17, 21). Antibiotics were serially diluted 2-fold in 50 μl of cation-adjusted Mueller-Hinton broth (CAMHB). The antibiotic range was 64 to 0.008 μg/ml, based on a final well volume of 100 μl after inoculation. The inocula were prepared by picking several colonies from 36- to 48-h chocolate agar (CA) plates grown at 35°C suspended and diluted with CAMHB to a bacterial cell density of 106 CFU/ml (conversion factor of 3.9 × 1010 CFU/ml/optical density at 600 nm [OD600]). To each well of the 96-well plate, 50 μl of this dilution was added, for a final inoculum of approximately 5 × 104 CFU/well (5 × 105 CFU/ml). The plates were incubated at 35°C and read visually at both 24 and 48 h. It was observed that several strains grew poorly or not at all if the IsoVitaleX supplement was included in premade antibiotic susceptibility testing (AST) plates. The addition of freshly reconstituted IsoVitaleX to the CAMHB inoculum at a concentration of 4% (final concentration in wells, 2%) yielded consistent results with good growth in the control and sub-MIC antibiotic wells. The observation was that for many of the more fastidious strains, premade frozen/thawed AST plates either did not support growth, or growth was greatly slowed or reduced and generally inconsistent. It is presumed that some component(s) in the supplement required for growth for these strains is labile under freeze, storage, and thaw conditions. The susceptibility results were more consistent and reproducible for all strains when the supplement was made up fresh and included in the inoculum. Quality control of all antibiotic stocks was verified by using Staphylococcus aureus ATCC 29213, Pseudomonas aeruginosa ATCC 27853, and Escherichia coli ATCC 25922, according to CLSI standards (19), and read at 18 to 24 h and again at 48 h (17). All bacterial work was carried out under biosafety level 3 (BSL-3) laboratory conditions.
TABLE 1.
F. tularensis strain information
| F. tularensis strain | Source/yra | Biovar |
|---|---|---|
| ATCC 6223 | Utah/1920 | A2 |
| ATCC 15482 | Utah/1950 | N (novicida) |
| DS89-R-54 | unk/1989 | A1 |
| DS88-R-675 | unk/1988 | A1 |
| DS88-R-160 | unk/1988 | A1 |
| DSAL91-1623 | unk/1991 | B |
| DSAZ91-1624 | unk/1991 | A2 |
| DST6755 | unk | A1 |
| LVS | Russia/unk | B |
| SchuS4-1 | Ohio/1941 | A1 |
| Strain 425 | Montana/1941 | B |
| JAP | Japan/1957 | B |
| 38A | unk/1960 | A2 |
| HUGH | unk/1948 | A1 |
| DS87-R-200 | unk/1987 | A1 |
| MAX B | unk/1953 | B |
| DS88-R-147 | unk/1988 | A1 |
| SCHERM | unk/1954 | A1 |
| Larsen NIH 38 | unk/1953 | A2 |
| VT68 | Vermont/1968 | B |
| SCHU-S5 | Ohio/1958 | A1 |
| MAX A | unk/1953 | B |
| IN99-1009 | Indiana/1999 | B |
| CO01-3027 | Colorado/2001 | A |
| MA00-2987 | Massachusetts/2000 | A |
| CA02-0099 | California/2002 | A |
| KY00-1708 | Kentucky/2000 | B |
| UT02-1927 | Utah/2002 | A |
| OR01-1807 | Oregon/2001 | B |
| OK00-2732 | Oklahoma/2000 | A |
unk, unknown.
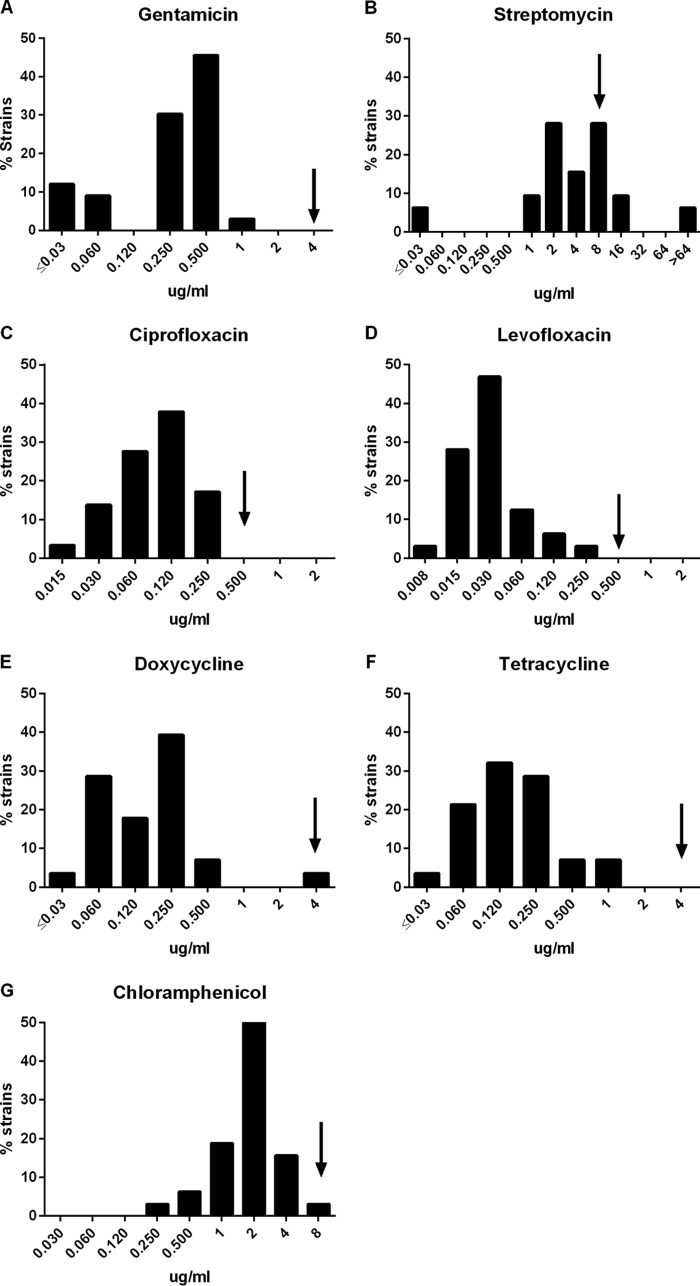
The broth dilution susceptibility data are presented in Table 2. Few susceptibility breakpoints have been established for F. tularensis. The CLSI has developed some interpretive criteria based in part on the data presented here, other published in vitro distribution data, and animal efficacy studies (17). Standard testing at 35°C provided MIC90s that could be interpreted as susceptible for gentamicin (Fig. 1A), streptomycin (Fig. 1B), ciprofloxacin (Fig. 1C), levofloxacin (Fig. 1D), doxycycline (Fig. 1E), tetracycline (Fig. 1F), and chloramphenicol (Fig. 1G), using the F. tularensis breakpoints (17). The range and MIC90 values for these antibiotics were in general agreement with the results from a CDC study (16). Differences observed between the two studies may be due to the greater strain distribution in this collection, particularly among the B biovar strains. Amikacin, netilmicin, tobramycin, gatifloxacin, gemifloxacin, moxifloxacin, ofloxacin, nalidixic acid, ceftazidime, cefotaxime, cefotetan, ceftriaxone, and co-trimoxazole may be active based on Enterobacteriaceae breakpoints (19). Some additional cephalosporins, macrolides, and rifampin may also have susceptibilities in efficacious ranges, but CLSI has no comparable breakpoints to use as a reference. Beta-lactams, carbapenems, and earlier generation cephalosporin MIC90 values would indicate poor activity based on the same criteria. The generally high susceptibilities to beta-lactams can be attributed to a class A β-lactamase shown to be present in the genome of F. tularensis (22). There was a notable shift in the distribution of susceptibilities for macrolides between the A and B type strains (Fig. 2). Variation due to distinct differences between the A and B strains may cause some B strain macrolide values to be in a poor activity range. Macrolide resistance has been observed with the B strains which are prevalent in Europe and, as a result, are contraindicated for treatment (8, 10). With the exception of the macrolide distribution, no other differences were observed between A and B strains for other antibiotics.
TABLE 2.
F. tularensis susceptibility values for 30 strains
| Antibiotic | Range (μg/ml) | MIC50 (μg/ml) | MIC90 (μg/ml) |
|---|---|---|---|
| Amikacin | ≤0.03 to 8 | 1 | 2 |
| Gentamicin | ≤0.03 to 1 | 0.25 | 0.5 |
| Netilmicin | ≤0.03 to 0.5 | 0.25 | 0.25 |
| Streptomycin | ≤0.03 to >64 | 4 | 8 |
| Tobramycin | ≤0.03 to 0.5 | 0.12 | 0.25 |
| Azithromycin | 0.12 to 16 | 1 | 1 |
| Cethromycin | ≤0.03 to 8 | 0.12 | 0.5 |
| Telithromycin | ≤0.03 to 16 | 0.25 | 1 |
| Clarithromycin | ≤0.03 to >64 | 0.5 | 4 |
| Solithromycin | ≤0.015 to 4 | 0.03 | 2 |
| Garenoxacin | ≤0.004 to 0.12 | 0.008 | 0.03 |
| Ciprofloxacin | 0.015 to 0.25 | 0.12 | 0.25 |
| Gatifloxacin | ≤0.004 to 1 | 0.015 | 0.06 |
| Gemifloxacin | ≤0.004 to 0.12 | 0.008 | 0.03 |
| Levofloxacin | 0.008 to 0.25 | 0.03 | 0.06 |
| Moxifloxacin | ≤0.004 to 0.12 | 0.008 | 0.06 |
| Nalidixic acid | 0.25 to 16 | 0.5 | 2 |
| Ofloxacin | 0.015 to 0.06 | 0.015 | 0.06 |
| Sparfloxacin | ≤0.004 to 0.06 | ≤0.004 | 0.12 |
| Novobiocin | ≤0.03 to 1 | 0.06 | 0.5 |
| Amoxicillin-clavulanate (2:1) | 0.5 to >64 | 16 | 16 |
| Amoxicillin | 4 to >64 | >64 | >64 |
| Ampicillin | 4 to >64 | >64 | >64 |
| Penicillin G | 2 to >64 | >64 | >64 |
| Piperacillin | 0.03 to >64 | 32 | >64 |
| Imipenem | 0.06 to >64 | 0.12 | 8 |
| Ertapenem | 0.06 to >64 | 1 | 8 |
| Faropenem | 0.12 to 16 | 2 | 4 |
| Meropenem | 0.12 to >64 | 1 | 16 |
| Cefepime | 0.12 to >64 | 4 | 16 |
| Ceftazidime | 0.03 to >64 | 0.12 | 1 |
| Cefotaxime | 0.03 to >64 | 1 | 2 |
| Cefotetan | 0.25 to >64 | 2 | 8 |
| Cefuroxime | 0.5 to >64 | 4 | 16 |
| Cefazolin | 0.5 to >64 | >64 | >64 |
| Ceftriaxone | ≤0.03 to >64 | 0.25 | 2 |
| Ceftaroline | 0.06 to >8 | 0.25 | 8 |
| Aztreonam | 0.5 to >64 | 2 | 8 |
| Sulfamethoxazole | 4 to >256 | 128 | >256 |
| Co-trimoxazole (19:1) | 0.25 to 8 | 1 | 4 |
| Trimethoprim | 0.25 to >64 | 4 | 16 |
| Doxycycline | ≤0.03 to 4 | 0.12 | 0.25 |
| Tetracycline | ≤0.03 to 1 | 0.12 | 0.25 |
| Tigecycline | ≤0.03 to 0.5 | 0.12 | 0.25 |
| Rifampin | ≤0.03 to 2 | 0.12 | 0.5 |
| Chloramphenicol | 0.25 to 8 | 2 | 4 |
| Fusidic acid | ≤0.03 to 32 | 2 | 8 |
FIG 1.
Thirty F. tularensis strain susceptibility distributions for 7 antibiotics with established CLSI breakpoints. Arrow indicates the CLSI breakpoint for each antibiotic tested: gentamicin (A), streptomycin (B), ciprofloxacin (C), levofloxacin (D), doxycycline (E), tetracycline (F), and chloramphenicol (G).
FIG 2.
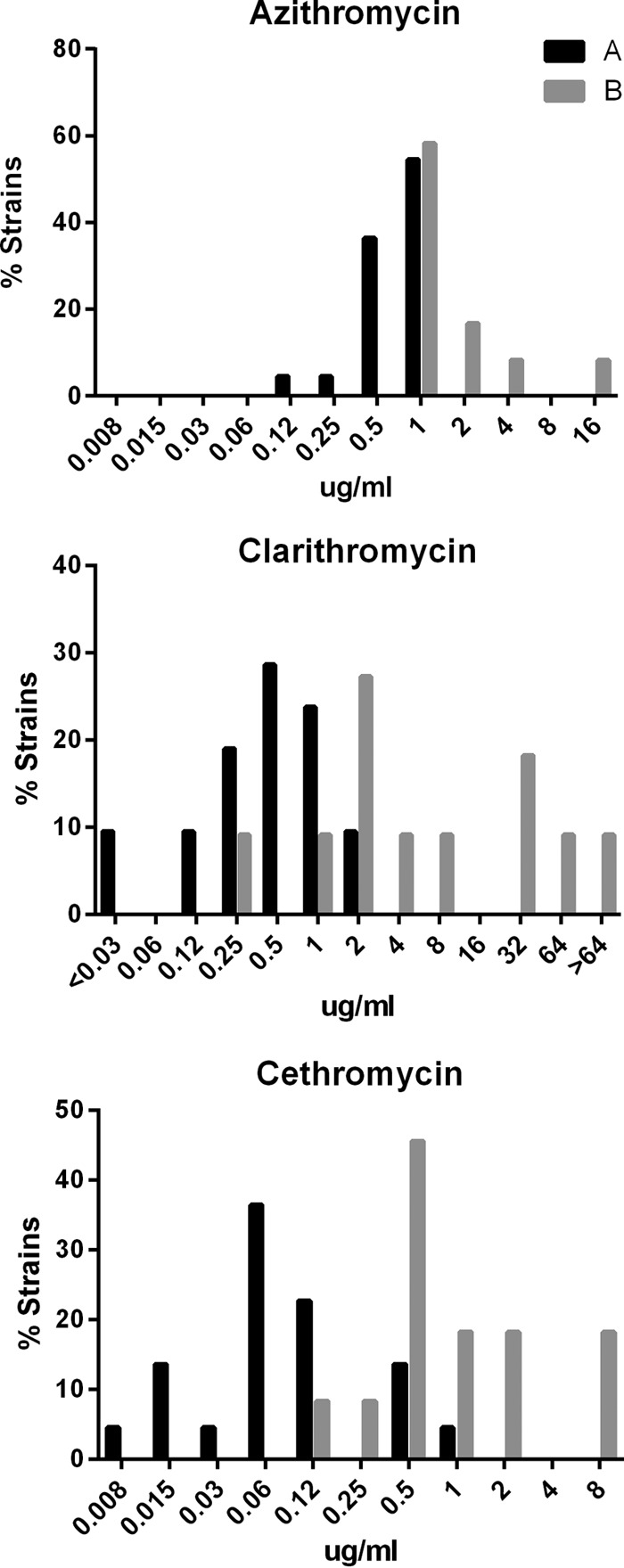
MIC distributions of F. tularensis A and B biovar strains for macrolides.
The establishment of a broad set of antibiotic susceptibility ranges for a number of defined and archived strains of F. tularensis will be helpful to serve as references in future testing of new antibiotics as they are developed. The establishment of a set of MIC90s will also aid in animal model-F. tularensis infection efficacy evaluations both in terms of which antibiotics to evaluate and the development of doses in combination with pharmacokinetic/pharmacodynamic studies.
ACKNOWLEDGMENTS
The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army or the University of Florida.
The research described herein was sponsored by the Defense Threat Reduction Agency, project no. 02-4-2C-013.
REFERENCES
- 1.Sjöstedt A. 2007. Tularemia: history, epidemiology, pathogen physiology, and clinical manifestations. Ann N Y Acad Sci 1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- 2.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Tonat K, Working Group on Civilian Biodefense. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2736–2773. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 3.Staples JE, Kubota KA, Chalcraft LG, Mead PS, Petersen JM. 2006. Epidemiologic and molecular analysis of human tularemia, United States, 1964–2004. Emerg Infect Dis 12:1113–1118. doi: 10.3201/eid1207.051504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Syrjälä H, Schildt R, Räisäinen S. 1991. In vitro susceptibility of Francisella tularensis to fluoroquinolones and treatment of tularemia with norfloxacin and ciprofloxacin. Eur J Clin Microbiol Infect Dis 10:68–70. doi: 10.1007/BF01964409. [DOI] [PubMed] [Google Scholar]
- 5.Johansson A, Urich SK, Chu MC, Sjöstedt A, Tärnvik A. 2002. In vitro susceptibility to quinolones of Francisella tularensis subspecies tularensis. Scand J Infect Dis 34:327–330. doi: 10.1080/00365540110080773. [DOI] [PubMed] [Google Scholar]
- 6.Kiliç S, Celebi B, Acar B, Ataş M. 2013. In vitro susceptibility of isolates of Francisella tularensis from Turkey. Scand J Infect Dis 45:337–341. doi: 10.3109/00365548.2012.751125. [DOI] [PubMed] [Google Scholar]
- 7.Yesilyurt M, Kilic S, Çelebi B, Çelik M, Gul S, Erdogan F, Ozel G. 2011. Antimicrobial susceptibilities of Francisella tularensis subsp. holarctica strains isolated from humans in the Central Anatolia region of Turkey. J Antimicrob Chemother 66:2588–2592. doi: 10.1093/jac/dkr338. [DOI] [PubMed] [Google Scholar]
- 8.Georgi E, Schacht E, Scholz HC, Splettstoesser WD. 2012. Standardized broth microdilution antimicrobial susceptibility testing of Francisella tularensis subsp. holarctica strains from Europe and rare Francisella species. J Antimicrob Chemother 67:2429–2433. doi: 10.1093/jac/dks238. [DOI] [PubMed] [Google Scholar]
- 9.Ulu Kiliç A, Kiliç S, Celebi B, Sencan I. 2013. In vitro activity of tigecycline against Francisella tularensis subsp. holarctica in comparison with doxycycline, ciprofloxacin and aminoglycosides. Mikrobiyol Bul 47:189–191. (In Turkish.) doi: 10.5578/mb.4179. [DOI] [PubMed] [Google Scholar]
- 10.Kreizinger Z, Makrai L, Helyes G, Magyar T, Erdelyi K, Gyuranecz M. 2013. Antimicrobial susceptibility of Francisella tularensis subsp. holarctica strains from Hungary, central Europe. J Antimicrob Chemother 68:370–373. doi: 10.1093/jac/dks399. [DOI] [PubMed] [Google Scholar]
- 11.Ikähemo I, Syrjala H, Karhukorpi J, Schildt R, Koskela M. 2000. In vitro antibiotic susceptibility of Francisella tularensis isolated from humans and animals. J Antimicrob Chemother 46:287–290. doi: 10.1093/jac/46.2.287. [DOI] [PubMed] [Google Scholar]
- 12.García del Blanco N, Gutierrez Martín CB, de la Puente Redondo VA, Rodriguez Ferri EF. 2004. In vitro susceptibility of field isolates of Francisella tularensis subsp. holarctica recovered in Spain to several antimicrobial agents. Res Vet Sci 76:195–198. doi: 10.1016/j.rvsc.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Kudelina RI, Olsufiev NG. 1980. Sensitivity to macrolide antibiotics and lincomycin in Francisella tularensis holarctica. J Hyg Epidemiol Microbiol Immunol 24:84–91. [PubMed] [Google Scholar]
- 14.Scheel O, Hoel T, Sandvik T, Berdal BP. 1993. Susceptibility pattern of Scandinavian Francisella tularensis isolates with regard to oral and parenteral antimicrobial agents. APMIS 101:33–36. doi: 10.1111/j.1699-0463.1993.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 15.Tomaso H, Al Dahouk S, Hoefer E, Splettstoesser W, Treu T, Dierich M, Neubauer H. 2005. Antimicrobial susceptibilities of Austrian Francisella tularensis holarctica biovar II strains. Int J Antimicrob Agents 26:279–284. doi: 10.1016/j.ijantimicag.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Urich SK, Petersen JM. 2008. In vitro susceptibility of isolates of Francisella tularensis types A and B from North America. Antimicrob Agents Chemother 52:2276–2278. doi: 10.1128/AAC.01584-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clinical and Laboratory Standards Institute. 2010. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria; approved guideline—2nd ed, CLSI document M45-A2. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 18.Johansson A, Farlow J, Larsson P, Dukerich M, Chambers E, Bystrom M, Fox J, Chu M, Forsman M, Sjostedt A, Keim P. 2004. Worldwide genetic relationships among Francisella tularensis isolates determined by multiple-locus variable-number tandem repeat analysis. J Bacteriol 186:5808–5818. doi: 10.1128/JB.186.17.5808-5818.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clinical and Laboratory Standards Institute. 2013. Performance standards for antimicrobial susceptibility testing; informational supplement. CLSI document M100-S23. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 20.Heine HS, Hershfield J, Marchand C, Miller L, Halasohoris S, Purcell BK, Worsham PL. 2015. In vitro antibiotic susceptibilities of Yersinia pestis determined by broth microdilution following CLSI methods. Antimicrob Agents Chemother 59:1919–1921. doi: 10.1128/AAC.04548-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker CN, Hollis DG, Thornsberry C. 1985. Antimicrobial susceptibility testing of Francisella tularensis with a modified Mueller-Hinton broth. J Clin Microbiol 22:212–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Antunes NT, Frase H, Toth M, Vakulenko SB. 2012. The class A β-lactamase FTU-1 is native to Francisella tularensis. Antimicrob Agents Chemother 56:666–671. doi: 10.1128/AAC.05305-11. [DOI] [PMC free article] [PubMed] [Google Scholar]