Abstract
Aim
To assess the prevalence, distribution, and associated risk factors of severe early childhood caries (S-ECC) among 12- to 36-month-old children of district Sirmaur, Himachal Pradesh, India.
Materials and methods
The present study was conducted on a random sample of 510 children, both boys and girls, between 12 and 36 months of age randomly selected from various government-sponsored day-care centers, private day-care centers, and vaccination centers. Caries was recorded using World Health Organization criteria. Statistical analysis was done by using chi-square test and Mann-Whitney test. A two-sided p value was calculated for each statistical test. Multiple logistic regressions were done to calculate the risk of S-ECC from independent variables.
Results
In the present study, S-ECC was found in 21% of 510, 12 to 36 months old children of Sirmaur district, Himachal Pradesh. The S-ECC was found to be significantly higher in 25 to 36 months old children’s age group and was 27.8% in them as compared with 8% in 12 to 24 months old children.
Conclusion
Providing anticipatory guidance and education to parents is essential for the promotion of optimal oral health of their children. There is a need for moving upstream to propose and implement policies and programs to improve the oral health of the very young, especially in a developing country like India, which lacks much data on S-ECC.
How to cite this article
Mangla RG, Kapur R, Dhindsa A, Madan M. Prevalence and associated Risk Factors of Severe Early Childhood Caries in 12- to 36-month-old Children of Sirmaur District, Himachal Pradesh, India. Int J Clin Pediatr Dent 2017;10(2):183-187.
Keywords: Prevalence, Risk factors, Severe early childhood caries.
INTRODUCTION
Early childhood caries (ECC), a term suggested at a 1994 Centers for Disease Control and Prevention workshop, denotes any form of caries occurring in the primary dentition of infants and youngsters.1
The disease of ECC is defined as “the presence of 1 or more decayed (noncavitated or cavitated lesions), missing (due to caries), or filled tooth surfaces“ in any primary tooth in a child 71 months of age or younger. In children younger than 3 years of age, any sign of smooth surface caries is indicative of severe early childhood caries (S-ECC). From ages 3 through 5, one or more cavitated, missing (due to caries), or filled smooth surfaces in primary maxillary anterior teeth, or a decayed, missing, or filled score of >4 (age 3), >5 (age 4), and >6 (age 5) surfaces constitutes S-ECC.2
Severe early childhood caries is a specific form of rampant decay of primary teeth in infants. The lesions develop quickly and occur in surfaces generally considered to be at low risk for caries. This caries pattern is observed in late infancy and early childhood.3 In contrast to the extensive reporting of the changing patterns of dental caries in the permanent dentition, there are fewer reports on trends in dental caries in primary teeth, particularly in preschool children under 3 years of age.4
Children who have caries in their primary teeth in infancy or as toddlers tend to develop additional dental decay in their primary teeth and are also more likely to develop dental caries in their permanent dentition. Therefore, the most important target group for instituting preventive programs seems to be infants and toddlers.5
Sirmaur is the most southeastern district of Himachal Pradesh, India. It has an area of 2,825 km2 and a population of 5.3 lakh.6
Focusing on 12- to 36-month-old children attending government-sponsored day-care centers, private day-care centers, and vaccination centers in Sirmaur district of Himachal Pradesh, the present study aimed to identify occurrence, distribution, and associated risk factors of S-ECC in 12- to 36-month-old children of district Sirmaur, Himachal Pradesh.7
MATERIALS AND METHODS
The present study was conducted on a random sample of 510 children, both male and female, between 12 and 36 months of age. The children were randomly selected from various government-sponsored day-care centers, private day-care centers, and vaccination centers from southeast part of Sirmaur district, Himachal Pradesh. The proposed study was reviewed by the ethical committee of Maharishi Markandeshwar University and clearance was obtained for the same.
Prior to the visit, written official permission to conduct the study was taken from all the concerned authorities as under:
Child Development Project Officer for government-sponsored day-care centers.
Principal/in-charge of various private day-care centers.
Chief Medical Officer of Sirmaur for various vaccination centers.
Parents/caretaker of the child.
Prior information was provided through in-charge of respective centers to the caregivers of the children attending various government-sponsored and private day-care centers regarding the dental examination of their child and the interview of the caregiver to be conducted. At the vaccination centers, the caregiver of the children attending these centers was informed of the nature of investigation, and prior permission and informed written consent of parents or caretakers were taken at the respective centers.
In this study, the required data were collected and recorded using printed proformas, which consisted of name of the child, age, sex, address, phone number, parent’s education, occupation locality and included questions about child’s dietary, feeding, oral hygiene habits, illnesses, etc.
Oral hygiene practices (use of toothbrush, materials used, and frequency of brushing) were also recorded. This proforma was filled by the examiner.
Clinical examinations were carried out at the immunization center’s medical room or classroom at the day-care centers with the aid of a mouth mirror, Community Periodontal Index (CPI) probe, and under natural light or where required with the aid of battery-operated head light/torch light.
The subjects were examined on an upright chair. Disposable mouth masks and gloves were used during the examination. The subjects were examined using an autoclaved plain mouth mirror and CPI probe. Caries was recorded as per World Health Organization criteria.7
Data Analysis
Data were entered into a database, checked for errors, and analyzed by Statistical Package for the Social Sciences software (release 6.1 version). Statistical analysis was done using chi-square test and Mann-Whitney test. A two-sided p value was calculated for each statistical test. We applied multiple logistic regression to calculate the risk of S-ECC from independent variables.
RESULTS
Out of 510 [220 females (43.18%) and 290 (56.86%) males] 12- to 36-month-old children examined, 175 (34.3%) children were in the age group of 12 to 24 months and 335 (65.7%) were in the age group of 25 to 36 months. In the present study, S-ECC was found in 21% of 510, 12 to 36 months old children of Sirmaur district, Himachal Pradesh (Graph 1). The S-ECC was found to be significantly higher in 25 to 36 months old children’s age group and was 27.8% in them as compared with 8% in 12 to 24 months old children (Table 1, Graph 2).
Graph 1:
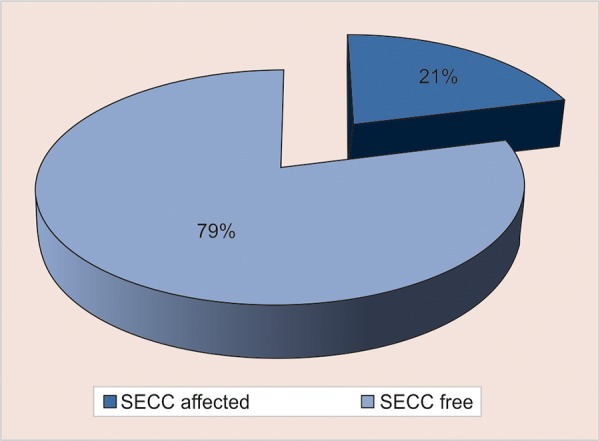
Prevalence of S-ECC in 12 to 36 months old children in Sirmaur district, Himachal Pradesh
Table 1: Occurrence of ECC and S-ECC according to age groups
| ECC | S-ECC | ||||||||||
| Age groups |
Total number of children (%) |
N | % | N | % | ||||||
| 12-24 months | 175 (34.3) | 14 | 8 | 14 | 8 | ||||||
| 25-36 months | 335 (65.7) | 105 | 32 | 93 | 27.8 | ||||||
| Total | 510 | 119 (23.3) | 23.3 | 107 | 21 | ||||||
| p-value χ2 | 0.000* | 37.673 | 0.000* | 27.076 | |||||||
*Stands for statistically significant as p ≤ 0.005
Graph 2:
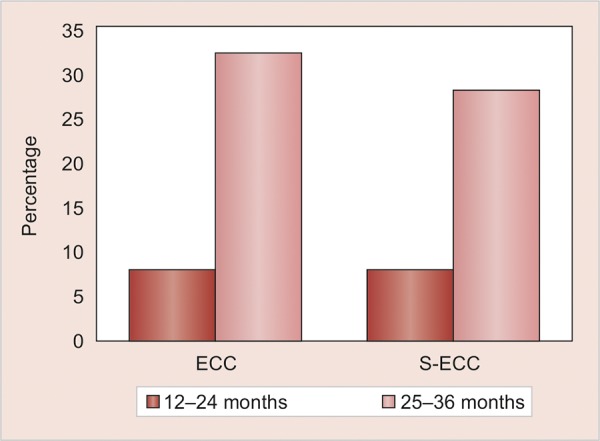
Occurrence of ECC and S-ECC according to age groups
Mean decayed, filled teeth (dft) scores in the study population was found to be 1.01 ± 2.373. In 12 to 24 months old children, mean dft scores were found to be 0.25 ± 1.030 and mean dft scores in 25 to 36 months old children were found to be 1.41 ± 0.750; mean decayed, filled surfaces (dfs) score in the study population was found to be 1.36 ± 3.998. Mean dfs score for 12 to 24 months old children in the study population was found to be 0.47 ± 2.286. Mean dfs score for 24 to 36 months old children in the study population was found to be 1.83 ± 4.583 (Table 2).
Table 2: Age groupwise distribution of mean dft and mean dfs in 510 children
|
Age group (months) |
N |
Mean dft ± Std. deviation |
Mean dfs ± Std. deviation |
||||
| 12-24 | 175 | 0.25 ± 1.030 | 0.47 ± 2.286 | ||||
| 25-36 | 335 | 1.41 ± 0.750 | 1.83 ± 4.583 | ||||
| Total | 510 | 1.01 ± 2.373 | 1.36 ± 3.998 |
Multivariate analysis was carried out using a stepwise multiple logistic regression to determine the strongest factors that were independently related to S-ECC when other variables were held constant. All variables were included in the start and those failing to show a significant relationship to S-ECC were subsequently removed in a step-wise manner. After logistic regression, which analyzes the effect of each factor when controlled across all other factors, many of the early significant relationships disappeared (Table 3).
Table 3: Factors related to S-ECC explained by logistic regression model
| 95% confidence interval | |||||||||
| S-ECC logistic regression model Variables | Significance | Odds ratio | Lower | Upper | |||||
| Age group | <.0001** | 7.059 | 3.219 | 15.476 | |||||
| Mother working or nonworking | 0.312 | 1.401 | 0.729 | 2.693 | |||||
| Income | 0.494 | 1.049 | 0.914 | 1.204 | |||||
| Mother’s education level | 0.001** | 0.571 | 0.405 | 0.806 | |||||
| Father’s education level | 0.083 | 1.347 | 0.962 | 1.886 | |||||
| Socioeconomic status | 0.885 | 1.042 | 0.595 | 1.825 | |||||
| Bottle-feeding done on demand | 0.510 | 2.347 | 0.186 | 29.686 | |||||
| Bottle sipping during the day | 0.237 | 4.043 | 0.399 | 40.937 | |||||
| Bottle fed to sleep | 0.702 | 1.901 | 0.071 | 50.781 | |||||
| Duration of bottle-feeding | 0.018* | 0.508 | 0.289 | 0.892 | |||||
| Contents of bottle-feeding | 0.992 | 0.998 | 0.712 | 1.399 | |||||
| Any sugar added to milk | 0.289 | 1.609 | 0.668 | 3.879 | |||||
| Age of commencement of solids | 0.873 | 0.964 | 0.617 | 1.508 | |||||
| Current adult supervision of toothbrushing | 0.003** | 0.367 | 0.189 | 0.710 | |||||
| Frequency of consumption of sweet and sticky food | 0.010* | 1.552 | 1.110 | 2.170 | |||||
| Whether sweets are given as reward to the child | 0.737 | 0.833 | 0.286 | 2.423 | |||||
| Constant | 0.000 | 0.011 | |||||||
*Stands for statistically significant as p ≤0.005; **Stands for statistically highly significant as p ≤ 0.001
The factors remaining statistically significant were:
Age group of the child
Mother’s level of education
Duration of bottle-feeding
Current adult supervision of toothbrushing
Frequency of consumption of sweet and sticky foods
Mothers educated up to high school level showed higher percentage of children with S-ECC.
About 60.7% (65) children with S-ECC were bottle-fed up to 13 to 36 months. Thus, more number of children with S-ECC were bottle-fed for prolonged duration.
In 37.4% (40) children with S-ECC, adults supervised their toothbrushing and in 62.6% (67) children, adults did not supervise their toothbrushing.
In 31.8% (34) children, frequency of consumption of sweet and sticky food was twice. Thus, more the number of times sweet and sticky food is consumed by children, more are the children affected by S-ECC.
DISCUSSION
The measurement of oral health is important for understanding normal biological processes and the natural history of disease and for planning and evaluating health services.8 India is a developing country, facing many challenges in rendering oral health care to masses. Dental caries is highly prevalent in India, which is influenced by the lack of awareness among the public. There is a dearth of awareness and information about the oral health of preschool children in India.9
In the present study, S-ECC was found in 21% of 510, 12 to 36 months old children of Sirmaur district, Himachal Pradesh. The mean dft score was 1.01 ± 2.373 and the mean dfs score was found to be 1.36 ± 3.998. Azevedo et al3 in 2005 reported S-ECC in 36% of the 36 to 71 months old children examined. Jin et al10 found S-ECC in 47% of children aged 6 to 59 months with a mean decayed, missing, filled teeth (dmft) score of 1.93 ± 0.27. The difference in the present study may be due to the inclusion of higher age groups in other studies.
The multivariate logistic regression model showed that older age of the child was a major risk factor that affects S-ECC. The severity of caries, as reflected by mean dft and dfs, was seen to increase with age. Chi-square test reveals that a significant correlation exists between the mean dft and age of children. Similar increase in caries experience has been found by other investigators.11-14 This may be explained by the fact that if caries-inducing factors are persistently present in affected children, the accumulative effect results in an increase in the severity of caries with age.15
Also, mother’s low level of education was found to be an important risk factor. In this study, children with S-ECC belonged to more of mothers with low level of education up to high school or primary school. The difference between S-ECC experience among children with regard to mother’s educational level could be attributed to lack of knowledge and awareness of mothers regarding dental health, oral hygiene practices, and feeding habits. Mothers completing higher level of education are more informed in health questions, and these influence various behaviors related to health as to maintain good dietary and hygiene behaviours.16 Similar results have been reported in most studies.15,17-19
In addition, S-ECC was also more likely to occur if the toothbrushing was not supervised as there were significantly more children with S-ECC in whom the brushing was not supervised and they brushed alone rather than being assisted. Similar findings were observed by Mahejabeen et al.20
Prolonged duration of bottle-feeding was the next major contributing risk factor for S-ECC. Bottle-fed children in this study were more likely to have S-ECC than those whose caregivers reported that they did not receive a bottle. However, prolonged duration of bottle-feeding was found to be a major risk factor in S-ECC, according to the multiple regression analysis. Nonetheless, mothers and other caregivers should be informed of how they can reduce the probability of S-ECC by avoiding inappropriate bottle use and contents, discouraging breastfeeding on demand, transitioning to the use of a regular cup at 12 months of age, and cleaning the child’s mouth regularly, once the first primary tooth has erupted. Improper feeding habits were found to be important attributive factors for S-ECC.
Severe early childhood caries was found to be higher in children consuming sweet and sticky snacks more frequently. Statistically significant positive correlations were found between S-ECC and frequency of consumption of sweet and sticky snacks in other studies also.17,21,22
This calls for improvement in children’s oral health maintenance among all those who serve as dominant primary caregivers of the children. There is a need to inform parents about necessary prevention, education, and dental care at early stages of development. Oral health promotion programs should be extended to all health care facilities where children from all socioeconomic levels are visiting from infancy onward.
Parents of children in India usually do not realize the importance of primary dentition considering that permanent teeth would soon erupt even if the primary teeth are decayed. Their lack of knowledge about the importance of oral health of their wards is a contributory factor for oral health decline in the very young.
The early caries development seen in these young children reinforces the need for early caries examinations and initiation of prevention programs before, or soon after, tooth eruption.
CONCLUSION
Occurrence of S-ECC was found to be 21% among 12 to 36 months old children of Sirmaur district, Himachal Pradesh, with a mean dft score of 1.01 ± 2.373 and mean dfs score of 1.36 ± 3.998. Evaluating the relationship of S-ECC with various associated risk factors, the factors found to have highly significant correlation value, in decreasing order were as follows:
Age group (mean dft score in 25-36 months age group was found to 1.41 ± 0.750 and mean dft score of 0.25 ± 1.030 in 12-24 months old children)
Mother’s low level of education
Prolonged duration of bottle-feeding
Current adult supervision of toothbrushing.
Frequency of consumption of sweet and sticky food
Providing anticipatory guidance and education to parents is essential for the promotion of optimal oral health of their children. Young children constitute a vulnerable population because of their dependence and inability to communicate their needs. Oral health disparities continue to pose challenges as dental caries is the most common chronic disease of childhood. Therefore, there is a need for moving upstream to propose and implement policies and programs to improve the oral health of the very young, especially in a developing country like India, which lacks much data on S-ECC.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Reisine S, Douglass JM. Psychosocial and behavioral issues in early childhood caries. Community Dent Oral Epidemiol. 1998;26(1 Suppl):32–44. doi: 10.1111/j.1600-0528.1998.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 2.Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2009;31(6):44–46. [PubMed] [Google Scholar]
- 3.Azevedo TD, Bezerra AC, de Toledo OA. Feeding habits and severe early childhood caries in Brazilian preschool children. Pediatr Dent. 2005 Jan-Feb;27(1):28–33. [PubMed] [Google Scholar]
- 4.Bonecker M, Marcenes W, Sheiham A. Caries reductions between 1995, 1997 and 1999 in preschool children in Diadema, Brazil. Int J Paediatr Dent. 2002 May;12(3):183–188. doi: 10.1046/j.1365-263x.2002.00352.x. [DOI] [PubMed] [Google Scholar]
- 5.Horowitz HS. Research issues in early childhood caries. Community Dent Oral Epidemiol. 1998;26(1 Suppl):67–81. doi: 10.1111/j.1600-0528.1998.tb02096.x. [DOI] [PubMed] [Google Scholar]
- 6.Fact file, District statistical office, Nahan. Available from: http://hpsirmaur.nic.in//fact file(general parameters). [Accessed date 9th May 2013];
- 7.WHO. Oral health surveys - basic methods. Geneva: WHO; 1997. [Google Scholar]
- 8.Lang WP, Borgnakke WS, Taylor GW, Woolfolk MW, Ronis DL, Nyquist LV. Evaluation and use of an index of oral health status. J Public Health Dent. 1997 Fall;57(4):233–242. doi: 10.1111/j.1752-7325.1997.tb02980.x. [DOI] [PubMed] [Google Scholar]
- 9.Suresh BS, Ravishankar TL, Chaitra TR, Mohapatra AK, Gupta V. Mother’s knowledge about pre-school child’s oral health. J Indian Soc Pedod Prev Dent. 2010 Oct-Dec;28(4):282–287. doi: 10.4103/0970-4388.76159. [DOI] [PubMed] [Google Scholar]
- 10.Jin BH, Ma DS, Moon HS, Paik DI, Hahn SH, Horowitz AM. Early childhood caries: prevalence and risk factors in Seoul, Korea. J Public Health Dent. 2003 Summer;63(3):183–188. doi: 10.1111/j.1752-7325.2003.tb03497.x. [DOI] [PubMed] [Google Scholar]
- 11.Warren JJ, Weber-Gasparoni K, Marshall TA, Drake DR, Dehkordi-Vakil F, Kolker JL, Dawson DV. Factors associated with dental caries experience in 1-year-old children. J Public Health Dent. 2008 Spring;68(2):70–75. doi: 10.1111/j.1752-7325.2007.00068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang JM, Altman DS, Robertson DC, O’Sullivan DM, Douglass JM, Tinanoff N. Dental caries prevalence and treatment levels in Arizona preschool children. Public Health Rep. 1997 Jul-Aug;112(4):319–329; 330-331. [PMC free article] [PubMed] [Google Scholar]
- 13.Tsai AI, Chen CY, Li LA, Hsiang CL, Hsu KH. Risk indicators for early childhood caries in Taiwan. Community Dent Oral Epidemiol. 2006 Dec;34(6):437–445. doi: 10.1111/j.1600-0528.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- 14.Jones DB, Schlife CM, Phipps KR. An oral health survey of Head Start children in Alaska: oral health status, treatment needs, and cost of treatment. J Public Health Dent. 1992 Winter;52(2):86–93. doi: 10.1111/j.1752-7325.1992.tb02249.x. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira SH, Beria JU, Kramer PF, Feldens EG, Feldens CA. Dental caries in 0- to 5-year-old Brazilian children: prevalence, severity, and associated factors. Int J Paediatr Dent. 2007 Jul;17(4):289–296. doi: 10.1111/j.1365-263X.2007.00831.x. [DOI] [PubMed] [Google Scholar]
- 16.Piovesan C, Mendes FM, Ferreira FV, Guedes RS, Ardenghi TM. Socioeconomic inequalities in the distribution of dental caries in Brazilian preschool children. J Public Health Dent. 2010 Fall;70(4):319–326. doi: 10.1111/j.1752-7325.2010.00191.x. [DOI] [PubMed] [Google Scholar]
- 17.Dini EL, Holt RD, Bedi R. Caries and its association with infant feeding and oral health-related behaviours in 3-4-year-old Brazilian children. Community Dent Oral Epidemiol. 2000 Aug;28(4):241–248. doi: 10.1034/j.1600-0528.2000.280401.x. [DOI] [PubMed] [Google Scholar]
- 18.Namal N, Vehit HE, Can G. Risk factors for dental caries in Turkish preschool children. J Indian Soc Pedod Prev Dent. 2005 Sep;23(3):115–118. doi: 10.4103/0970-4388.16881. [DOI] [PubMed] [Google Scholar]
- 19.Qin M, Li J, Zhang S, Ma W. Risk factors for severe early childhood caries in children younger than 4 years old in Beijing, China. Pediatr Dent. 2008 Mar-Apr;30(2):122–128. [PubMed] [Google Scholar]
- 20.Mahejabeen R, Sudha P, Kulkarni SS, Anegundi R. Dental caries prevalence among preschool children of Hubli: Dharwad city. J Indian Soc Pedod Prev Dent. 2006 Mar;24(1):19–22. doi: 10.4103/0970-4388.22829. [DOI] [PubMed] [Google Scholar]
- 21.Jose B, King NM. Early childhood caries lesions in preschool children in Kerala, India. Pediatr Dent. 2003 Nov-Dec;25(6):594–600. [PubMed] [Google Scholar]
- 22.Hallett KB, O’Rourke PK. Social and behavioural determinants of early childhood caries. Aust Dent J. 2003 Mar;48(1):27–33. doi: 10.1111/j.1834-7819.2003.tb00005.x. [DOI] [PubMed] [Google Scholar]


