Abstract
Objective
Goal setting is a common element of self-management support programs; however, little is known about the nature of patients' goals or how goals change during pain self-management. The purpose of the current study is to explore how patients' goals and views of goal setting change over the course of a peer-led pain self-management program.
Methods
Veterans (n = 16) completing a 4-month peer-led pain self-management program completed semi-structured interviews at baseline and follow-up regarding their goals for their pain. Interviews were analyzed using immersion/crystallization.
Results
Analyses revealed six themes: motivation to do something for their pain, more goal-oriented, actually setting goals, clarity of goal importance, more specific/measurable goal criteria, and more specific/measurable strategies.
Conclusion
The current analyses illustrate how participants' goals can evolve over the course of a peer-led pain self-management program. Specifically, increased motivation, more openness to using goals, greater clarity of goal importance, more specific and measurable goals and strategies, and the influence of the peer coach relationship were described by participants.
Practice implications
Pain self-management interventions should emphasize goal setting, and development of specific, measurable goals and plans. Trainings for providers should address the potential for the provider-patient relationship, particularly peer providers, to facilitate motivation and goal setting.
Keywords: Pain self-management, Goal setting, Working alliance
1. Introduction
Chronic pain is a pervasive and costly condition. Nationwide, over 100 million Americans are affected by pain, with annual costs exceeding $600 billion [1]. The presence of chronic pain among Veterans is especially high, with 50-60% of Veterans reporting that they experience chronic pain [2, 3]. Moreover, as the population of older Veterans grows, the presence and cost of chronic pain is expected to increase [3, 4]. Beyond fiscal costs, chronic pain is associated with reduced quality of life, poor overall health, psychological distress, limitation of activities, poor sleep, and increased disability [3, 5-8].
In 2009, the Department of Veterans Affairs recommended the use of self-management programs in their directive on pain management [9]. Pain self-management is an inter-disciplinary intervention rooted in patient education that utilizes an individualized approach to strengthen a patient's capability to manage the day-to-day physical and psychological demands of their chronic condition [4]. Pain self-management programs have been effective in ameliorating various effects of chronic pain [10], including decreases in pain-related disability, pain severity, negative cognitions and beliefs, depressive symptoms, and number of physicians' visits [11-14]. Similarly, pain self-management programs have been shown to increase self-confidence and self-efficacy, improve mental function, and result in more favorable self-reports of overall health [4, 6, 15, 16].
An important component of many self-management programs is goal setting [17]. Specifically, goal setting can facilitate the effective use of pain self-management strategies [18] and lead to improved patient outcomes and enhanced patient autonomy. For instance, in a self-management program for individuals with polyarthritis, the use of goal-management strategies, particularly adjusting one's goals to one's personal abilities, was positively associated with positive affect and purpose in life, and negatively associated with depression and anxiety [19]. Additionally, Lorig's Chronic Disease Self-Management program, which utilizes patient-set goals and action plans, has resulted in greater self-efficacy as well as more favorable health outcomes and fewer hospitalizations when compared to baseline [20] and when compared to those receiving care as usual [21]. Relevant to this work is Goal Setting Theory [22], which empirically demonstrates the role of goal setting and factors affecting its success. Fundamentally, setting a specific goal is associated with greater progress than setting a more general goal (e.g., “to do my best”). Additionally, several factors, such as the perceived importance of the goal, self-efficacy, and the effectiveness of goal-related strategies, moderate the effects of goal setting on goal success [22].
Despite the importance of goal setting within pain self-management [13, 23, 24], little is known about the nature of patients' goals for pain self-management, how patients use goals in the context of pain self-management, or how these goals change over time. Such knowledge can facilitate goal setting discussions between patients and their providers and be used to refine and bolster the goal setting component of self-management programs. Consequently, the purpose of the current study is to explore the nature of patients' pain self-management goals and how patients' goals and their views of goal setting change in the context of a peer-led pain self-management intervention.
2. Methods
2.1 Study Setting and Participants
The current study involves participants from IMPPRESS (Improving Pain using Peer-REinforced Self-Management Strategies, NCT01748227), a pilot study designed to test the effects of peer-supported pain self-management on Veterans with chronic pain. Recruitment for this parent study has been described elsewhere [25]. Briefly, participants were recruited from one Veterans Affairs (VA) Medical Center in the Midwestern United States. Eligibility requirements included musculoskeletal pain of at least moderate severity (i.e., rated 5 or more on a scale of 0 to 10), lasting at least 6 months. Patients were excluded if they had been hospitalized for psychiatric or substance abuse reasons in the past six months, had current suicidal ideation, prior or pending back surgery, speech or hearing impairment, or had a severe medical condition that would prevent participation (e.g., advanced heart failure). For the current study, 16 of the 17 patients who completed the parent study completed two additional interviews regarding their goals for pain self-management (see Sec. 2.3). These additional interviews are the focus of the current analysis. Ethical approval was granted by the local IRB and informed consent was obtained from all participants.
2.2 Intervention
Participants were paired with a peer coach, who was assigned two patients each and instructed to contact each patient twice per month for four months, resulting in eight contacts with each patient. Coach-patient pairs met in person and/or over the telephone per individual preferences and needs. All coaches and patients received a pain self-management manual consisting of eight sections: 1) Introduction to Pain Self-Management; 2) Pain Education; 3) Activity Pacing; 4) Relaxation Skills; 5) Self-Care Skills; 6) Interpersonal Skills; 7) Relapse Prevention; and 8) Informational Resources. Peer coaches' manuals contained an additional section, “How to Be a Peer.” Peer coaches completed a three-hour training prior to being assigned patients and received regular supervision from the study psychologist who encouraged implementation of various techniques, including focusing on the patients' goals.
2.3 Procedures
In addition to the data collection for the parent study, patients were invited to participate in two additional interviews focused on their pain self-management goals. These interviews were conducted at baseline and at the end of the four-month intervention. Patients were financially compensated for their participation in each of these interviews. Study research assistants, experienced in qualitative interviewing conducted all interviews. All interviews were audio recorded, transcribed, checked for accuracy, and de-identified.
2.4 Interviews
During both interviews, patients were asked to list all of their goals related to their pain, and then to pick their two most important goals to discuss further. The interview protocol was guided by questions about goal quality, as described by Goal Setting Theory [22]. Questions focused on how the patient operationalized their goal (“goal criteria”), their plan for reaching each goal (“goal strategy”), why each goal was important, how their goals emerged, and their general view of goal setting (see Appendix for full list of interview questions). Baseline and follow-up questions differed minimally; at baseline patients were asked if and how the baseline interview had affected their thoughts about goals and at follow-up patients were asked about the impact of the intervention on their goals and use of goal setting.
2.5 Data Analysis
Data analysis began after all data collection was complete, and was conducted by the first author using immersion/crystallization methodology [26]. First, recordings and transcripts were reviewed to foster familiarity with the data, case notes were generated and salient quotes were recorded. Second, baseline and follow-up interviews for each patient were reviewed and compared; a list of changes and differences between the content of the baseline and follow-up interviews for each participant was compiled. Third, a list of preliminary themes and possible codes was generated. Preliminary codes were applied to both transcripts and notes regarding changes, and additional quotes of interest were identified. Iterative code lists were discussed with the second author and a final code list was established. After final coding was completed, data were grouped into conceptual themes and coauthors reviewed findings for veracity and alternative interpretations. Coding and analyses were facilitated by ATLAS.ti 7.
Analyses of the goals set by patients followed an inductive emergent qualitative approach. After all text had been coded using the emergent approach, and baseline and follow-up goals were compared, it was evident that goals changed in how strongly they reflected SMART goal principles, i.e., specific, measurable, action-focused, realistic, and time-specific [27, 28]. In the current study, changes in the SMART principles of “specific” and “measurable” were most prevalent, and thus, considered in analyses. Patients' answers to two questions were particularly examined in light of these SMART principles: 1) How would you know you had met your goal (goal criteria)? and 2) What are your plans to meet this goal (goal strategy)? For each patient, the first author determined whether goal criteria and strategies became more or less specific and measurable or were unchanged at follow-up.
3. Results
Patients ranged in age from 34 to 66 years (M = 57.38, SD = 8.25), 8 were White and 8 were Black, and all were male Veterans. Analyses revealed six themes describing how patients' goals and/or views of goal setting changed during the IMPPRESS intervention.
3.1 Motivation to Do Something
Seven patients mentioned that the intervention helped them to become motivated or “fired up” (P219) to do something more regarding their pain self-management.
The study has opened my eyes more. I've gotten more serious about this. Hearing and seeing what other people have accomplished gives me the encouragement to want to do better. (P211)
Before, I'd take my medicine and that would be it, but by talking with [my peer coach] it was like, this is not a give-up time, you know, you've got to keep going, and that was great. That was great. (P214)
Notably, in many cases (such as those quoted above), participants attributed this change to interactions with their peer coach and, to a lesser extent, other participants.
3.2 More Oriented Toward Using Goals (or) More Goal-Oriented
When asked how the baseline interview affected their thoughts about goals, 12 patients reported that they had experienced some change in their thoughts, seven of whom indicated they had not considered goals for pain management prior to the baseline interview: “[The baseline interview] brought [goals and pain management] up towards the top where I can actually see and think about it” (P203), “I really haven't concentrated on my pain that much, on what to do or what direction I'm going in with it” (P217).
Seven patients were more goal-oriented at follow-up than at baseline. For example, one patient saw goals as irrelevant for him at baseline: “[I'm] less [goal-oriented] now than I was before…I retired in '03…I went on physical disability…I've had really no need to set goals” (P208). At follow-up he expressed a relatively stronger goal orientation, “somewhat [goal oriented]…If I set a goal I try to get it accomplished one way or the other.” Five patients maintained a positive orientation toward goals; for example, answers shifted from “extremely” goal-oriented at baseline to “100%” at follow-up (P213). For the remaining four, it was not always clear how goal oriented they considered themselves; their answers at baseline and/or follow-up were unclear or unable to be compared. Additionally, participants generally expressed greater or equal agreement with statements about using goals to help with pain management (see Table; see items 10a & 10b in Appendix).
Table. Agreement with statements of goal use.
| Question | Time | Strongly Agree | Agree | Disagree | Strongly Disagree | ||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Frequency | % | Frequency | % | Frequency | % | Frequency | % | ||
|
|
|
|
|
||||||
| I use goals to help relieve my pain* | Baseline | 6 | 37.5% | 2 | 12.5% | 6 | 37.5% | 2 | 12.5% |
|
| |||||||||
| Follow-up | 6 | 37.5% | 6 | 37.5% | 4 | 25.0% | 0 | 0.0% | |
|
|
|||||||||
| I use goals to be more active despite my pain** | Baseline | 10 | 62.5% | 4 | 25.0% | 1 | 6.2% | 0 | 0.0% |
|
| |||||||||
| Follow-up | 7 | 43.7% | 2 | 12.5% | 5 | 31.2% | 2 | 12.5% | |
Wilcoxin signed‐rank:
z = -1.261, p = .207
z = -1.897, p = .058
3.3 Setting Goals
Five patients stated that the intervention helped them to set goals. One patient simply stated, “[the intervention's] given me goals” (P214), and another that he restarted old goals (P210). Moreover, many patients described some of the ways that the intervention facilitated goal setting. Some found that the intervention gave them the support they needed to begin pursuing goals:
Before I started the program I didn't set very many [goals] because before the program I was feeling pretty bad. And I wasn't able to physically- I didn't have the support that I needed. I wasn't able to set goals because I wasn't able to, much- I didn't have much of a measuring line. But since the program I've been able to set quite a few. (P213)
Peer coaches had a significant influence on the formulation of patients' goals. Although interviewers did not specifically ask about the impact of the peer coach, eight patients spontaneously explained how their peer coach influenced their goals. This influence was seen in one patient's goal to have a better quality of life:
[The goal] came about with [my peer coach's] input. Even though I was repeating the same things, which he could have looked at as negative, he was coming up with different ways I could interact. Like getting me help with the Boy Scouts. Oh, call this person. What about an electric [wheel] chair? Then you could get around and you wouldn't have to be dependent. (P201)
This patient's peer coach suggested different strategies for interacting with people, which the patient says helped him realize his goal. For another patient, conversing with his peer coach changed his perspective about his abilities and influenced his goal of not letting pain control his life:
Since I've started this program, since I've talked to my peer, I've got to the point where I have a lot more confidence in myself. I'm not relying on medication…The goal came about when I realized for the first time in years that I am in control of [the pain] if I want to be. And it was just a matter of this program helped me to become aware of that. The program with my peer. (P213)
3.4 Clarity of Goal Importance
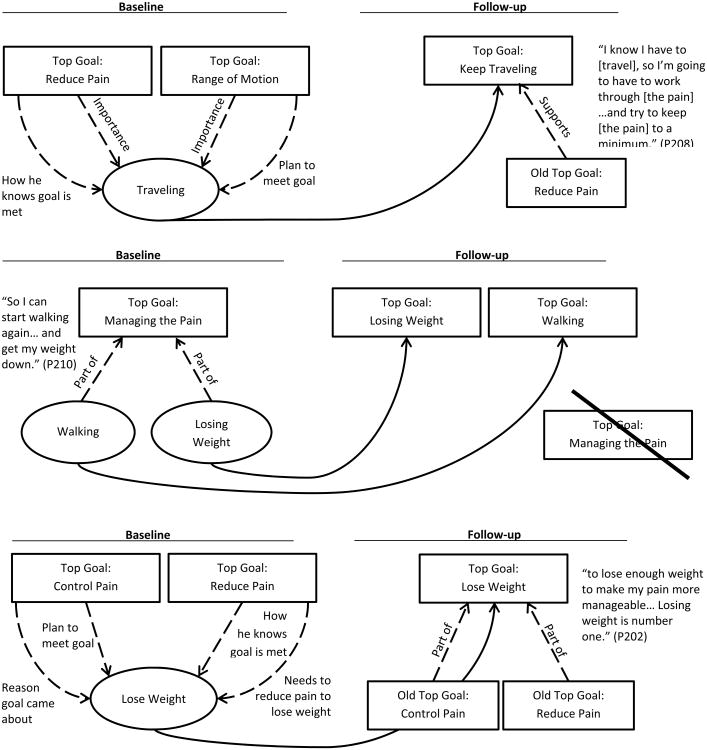
It was common for patients to express multiple goals and desires in addition to their two most important goals. For seven patients, these additional goals were predominant in the baseline interview, sometimes overshadowing the goals they stated were “most important.” In the follow-up interview these goals were identified as one of the patient's two most important goals. This was interpreted as the patient gaining more clarity regarding their most important goals.
This increased clarity was evident for P208's goal of continuing to travel. At baseline, his top two goals were to reduce his pain and increase his range of motion. He did not mention travel in his full list of goals at baseline; however, throughout his baseline interview, it was clear that travel was extremely important to this patient and played a significant role in his top two goals:
(Goal Criterion: Reducing pain) If I could be able to enjoy getting on a cruise ship and going through all the rigmarole and getting in and getting documented and everything…to get on and off the boat without much effort, and not tripping and losing my balance.
(Goal Strategy: Range of motion) We go to the Grand Ole Opry in Nashville, and that's not too bad. I can get by because they have a golf cart to take you from the busses to the entrance and back…but…it's how much longer I'm going to be able to do it until I get things where I can learn how to cope with [the lack of mobility/range of motion].
This patient also mentioned travel when discussing why his goals were important and how they came about. At follow-up, he explicitly stated that travel was his most important goal; it appears that over the course of the intervention, the importance of the goal to keep traveling became clearer to this patient (see Figure for additional examples).
Figure. Illustration and further examples of change in goal importance.
In some cases, patients who presented this progression also expressed that the intervention helped them consider what was important to them, “[the intervention] helped me organize my thinking and that type of organization is helpful, because I can put things that are really important in front of the things that I like to be important” (P202).
3.5 More Specific & Measurable Goal Criteria
Goal criteria became more specific and measurable for seven patients. For example, one patient had a baseline goal to lose weight, but his criteria were vague, “[I'd know] by the scale… I'd get on the scale and…watch the scale” (P221). At follow-up, the patient had set specific goal criteria—to lose 150-160 pounds.
Another patient had a baseline goal to learn new things to help control his pain. His criteria lacked specificity and were not measurable, “when I see myself doing more, or feel good enough to do more, and start enjoying life a lot more” (P219). At follow-up, one of his goals was to talk to his doctor about how his pain medication affected him. He stated he would know this goal was met when he had talked to his doctor at his next appointment, “[I'll know] when I meet with him this month and we sit down….I'm pretty sure he'll listen to me. I'm going to kind of demand he does.”
3.6 More Specific & Measurable Strategies
Strategies became more specific and measurable for nine patients. For example, one patient had a baseline goal to quit smoking. He reasoned that smoking cessation would improve his respiration so he could exercise and improve his pain. At baseline, he was not able to describe a specific or measurable plan to meet his goal:
Well, I've got a couple things to finish up at the VA and then I'm going to work on my weight loss first and then try to stop smoking…right now I'm just trying not smoking as much…I've not started it, but I've planned it (P211).
At follow-up, he mentioned that he had achieved his goal to quit smoking, and described a plan to maintain a smoke-free lifestyle, “I did that. I went through all the steps, you know, I'm on my last step, step three…my goal is to keep telling people that I haven't had a cigarette each week until a year goes by.” Over the course of the study, not only did his strategy to quit smoking become specific and measurable, but he had also achieved his goal.
Another patient stated that he had no plan to meet either of his baseline goals. At follow-up he was able to articulate a plan for his goal to exercise, “Get up and do it, get up in the morning and do my exercises” (P214). This patient went from having no strategies to meet his goals to having a plan to exercise at a regular time, showing a relative improvement in the specificity and measurability of his strategies.
Not all patients' strategies or criteria became more specific and measurable over time. For five patients, both goal criteria and strategies became less specific and measurable at follow-up (declined) and/or were not specific or measurable at baseline and follow-up (stagnant). Most commonly, goal criteria declined and plans remained stagnant.
For example, at baseline, P207 had specific and measurable criteria to walk and bike in order to lose 5 pounds and meet his goal of exercising, but at follow-up he was not able to articulate measurable and specific criteria for his goal to not let pain control his life, “I'd enjoy the things around me more. I'd appreciate the things I can do,” showing a decline in goal criteria. In contrast, P215 showed stagnation in his strategies. His plan to lose weight at baseline was specific, “Get a job. Join the gym again, start swimming;” however, he had no plan for his second goal of getting control of his life. Similarly, at follow-up he planned to move to a safer neighborhood so he could meet his goal of riding his bike, but was again unable to articulate a plan for his second goal of finding time to exercise.
4. Discussion and Conclusion
4.1 Discussion
The current study explored how patients' pain self-management goals and their views of goal setting changed over the course of a peer-led pain self-management intervention. Six themes emerged from patients' responses: increased motivation to do something regarding their pain, an increased openness to using goals, actual setting of goals, clarifying the relative importance of their goals, and more specific goal criteria and strategies. These themes are consistent with literature from other fields regarding the effects of goal setting [22], and point to multiple junctures at which pain self-management programs may exact positive effects on patients.
The first theme, that patients were motivated toward action, is a precursor toward goal setting. Goal setting is action-oriented and best suited for patients in the action phase [29]. At follow-up, patients were more oriented toward action. This progression into action appears to have been driven substantially by the influence of and relationship with the peer coach, which is consistent with previous research [30-32]; patients voluntarily reported that the supportive and dynamic relationship with their peer coach helped them explore their goals for pain self-management and increased their motivation.
Notably, patients reported having given little thought to setting goals, either as a general strategy or for their specific pain self-management goals, prior to the intervention. Through the course of the program, patients set goals. This act, in and of itself, is important, because simply setting goals has been linked with increased progress and motivation [22, 33]. Although goal setting is almost universally considered a critical element of self-management programs [13, 23, 24], little empirical data have demonstrated that patients actually engage in the activity, nor has it been described sufficiently. Beyond merely setting a goal, the themes emerging from the current study suggest that participating in a pain self-management intervention may be associated with changes in goal dimensions [34] (e.g., importance, specificity) as well as planning (i.e., development of alternative strategies). More optimal planning [35-37] and greater specificity [38] have been associated with greater likelihood of progress, and increased goal importance has been associated with perseverance in the face of difficulties [39, 40].
These results suggest a dynamic relationship between goal setting and other elements of the pain self-management intervention. The interpersonal relationship between the patient and program provider (peer coach) facilitates action, while goal setting provides direction and a sense of a common agenda for treatment [41].
4.2 Limitations and Directions for Future Research
Our study examined how goals changed over the course of a peer-led pain self-management intervention. A substantial limitation was that, although participants described changes in their attitudes and goals, they were not invited to explain why or how these changes took place. Additionally, many of the changes observed were likely to have an effect on goal achievement; however, patients were not asked if they had completed their goals, although a very small number of patients voluntarily reported they had completed a goal in the course of the intervention. In addition, although patients were asked how the baseline interview and the intervention as a whole affected their goals and attitudes about goals, it remains unclear if the changes that occurred are due to the intervention, the interviews, or both. Even in cases where patients specifically attribute changes to the intervention, it is possible that the baseline interview may have influenced their thinking about goals prior to the start of the intervention. Finally, this study is a small qualitative study conducted at one VA medical center with Veterans who are all male. Thus, the results should be taken as preliminary; additional research is needed in other populations and settings to continue to refine our understanding of how patients experience goal setting in pain self-management.
Future research should explore goal setting in larger, more diverse samples. Additionally, further examination is needed regarding how and why participants' goals change, and whether the changes observed in this study are associated with goal attainment and other patient outcomes. Changes should be compared between patients participating in a self-management support program and those who are not. The effects of other factors (e.g., interactions with providers) should also be examined. Moreover, additional research should explore how the goal setting and motivational dynamic may differ when the provider is a peer versus a non-peer. Finally, although the current study suggests self-management programs may bolster several aspects of goal setting, additional research is needed to explore which aspects should be targeted, for whom, and when.
4.3 Conclusion
Participation in a peer-led pain self-management intervention may facilitate patients' goal setting, including actively developing goals, prioritizing their most important goals, articulating goals that are more specific and measurable, and developing concrete strategies for goal attainment. Many participants reported that their relationship with their peer coach influenced their goal setting process and motivation; the promising role of peers in goal setting warrants further exploration. The current analysis suggests that a peer-led pain self-management program may help facilitate goal development that enhances goal quality, bolsters patient motivation, clarifies the importance of goals, and increases the likelihood of goal success.
4.4 Practice Implications
Self-management interventions should continue to emphasize goal setting as a self-management strategy. Moreover, trainings for program facilitators should emphasize the working relationship as a facilitator to action-oriented tasks such as goal setting. Finally, curricula should provide information to guide patients' development of more specific and personally meaningful goals, as well as establishment of viable strategies.
I confirm that all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Highlights.
Explores how goals & views change during a peer-led pain self-management program.
Patients reported more motivation & goal-setting, and stronger goal-orientation.
Patients clarified goal importance and had more measurable & specific goals.
The peer-coach relationship influenced increased motivation & goal setting.
Trainings should explore effect of provider-patient relationship on motivation.
Acknowledgments
The project reported here was supported by the Department of Veterans Affairs, Veterans Health administration, Quality Enhancement Research Initiative (QUERI) and Health Services Research and Development (HSR&D; RRP 12-483, CDA 10-034, and D0712W). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs of the United States Government.
Appendix
Interview Questions
How goal-oriented do you see yourself as being?
What are your goals regarding your pain? (repeat back goals)
-
What would you say are your two most important goals?
For each of the two most important goals:- How did this goal come about?
- How important is this goal to you? What is important about it?
- How would you know you had met this goal?
- What might happen with this goal in the next few weeks?
- Is this a short-term or long term goal?
- What are the chances that you will meet this goal?
Have you talked to your doctor about your goals regarding your pain? Tell me about that.
Specifically, have you talked with your doctor about desired lifestyle goals/changes you feel will result from reduced pain?
How would you like to see your relationship with your doctor improve?
Would you like your doctor to focus on your lifestyle goals regarding your pain as well as your physical pain goals? Why or why not?
Have you thought about and/or shared strategies you might use in order to achieve your lifestyle or physical goals with your doctor?
You've mentioned several goal you have regarding your pain treatment. Are these goals related in some way to each other?
- Please tell me how much you agree or disagree with the following statements:
- I use goals to help relieve my pain. Do you strongly disagree, disagree, agree, or stronglyagree? OK, tell me about that.
- I use goals to be more active despite my pain. Do you strongly disagree, disagree, agree,or strongly agree? OK, tell me about that.
Imagine a hypothetical day where you woke up pain-free. Can you walk me through that day, what would you do? How would it differ from a typical day that you presently experience?
(At baseline) Do you think that doing this interview changed the way that you think about your goals or about your pain management in general? (if change)OK, can you explain?
(At follow-up) In what way, if at all, has being in the peer program changed your goals regarding your pain?
(At follow-up) Has being in the peer program changed the way you use goals or set goals?
Anything else you would like to add regarding your goals and your pain?
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.IoM, C.a.E.C.o.A.P.R. Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Kerns RD, et al. Veterans' reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. Journal of Rehabilitation Research and Development. 2003;40:371–80. doi: 10.1682/jrrd.2003.09.0371. [DOI] [PubMed] [Google Scholar]
- 3.Butchart A, et al. Experience and management of chronic pain among patients with other complex chronic conditions. Clin J Pain. 2009;25:293–8. doi: 10.1097/AJP.0b013e31818bf574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barlow JH, et al. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling. 2010;48:177–87. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 5.Leadly RM, et al. Healthy aging in relation to chronic pain and quality of life in Europe. Pain Practice. 2014;14:547–58. doi: 10.1111/papr.12125. [DOI] [PubMed] [Google Scholar]
- 6.von Korff M, et al. A randomized trial of a lay person-led self-management group intervention for back pain patients in primary care. Spine. 1998;23:2608–15. doi: 10.1097/00007632-199812010-00016. [DOI] [PubMed] [Google Scholar]
- 7.Stefane T, et al. Chronic low back pain: Pain intensity, disability and quality of life. Acta Paul Enferm. 2013;26:14–20. [Google Scholar]
- 8.Sezgin M, et al. Sleep quality in patients with chronic low back pain: A cross-sectional study assessing its relations with pain, functional status and quality of life. Journal of Back & Musculoskeletal Rehabilitation. 2015;28:433–42. doi: 10.3233/BMR-140537. [DOI] [PubMed] [Google Scholar]
- 9.Affairs, D.o.V. VHA Directive 2009-053: Pain Management. Washington, D.C: 2009. [Google Scholar]
- 10.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–37. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 11.Bair MJ, et al. Evaluation of steped care for chronic pain (ESCAPE) in Veteran's of the Iraq and Afghanistan conflicts. J Amer Med Assoc Intern Med. 2015;175:682–89. doi: 10.1001/jamainternmed.2015.97. [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, et al. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: A randomized control trail. The Journal of the American Medical Association. 2009;301:2099–110. doi: 10.1001/jama.2009.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lorig K, Laurin J, Holman HR. Arthritis self-management: A study of the effectiveness of patient education for the elderly. The Gerontologist. 1984;24:455–7. doi: 10.1093/geront/24.5.455. [DOI] [PubMed] [Google Scholar]
- 14.Nicholas MK, et al. Is adherence to pain self-management strategies associated with improved pain, depression and disability in those with disabling chronic pain? European Journal of Pain. 2012;16:93–104. doi: 10.1016/j.ejpain.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Damush TM, et al. The long-term effects of a self-management program for inner-city primary care patients with acute low back pain. Arch Intern Med. 2003;163:2632–8. doi: 10.1001/archinte.163.21.2632. [DOI] [PubMed] [Google Scholar]
- 16.Mendelson AD, McCullough C, Chan A. Integrating self-management and exercise for people living with arthritis. Health Education Research. 2011;26:167–77. doi: 10.1093/her/cyq077. [DOI] [PubMed] [Google Scholar]
- 17.Caudill MA. Managing pain before it manages you. Revised. New York: Guilford; 2002. [Google Scholar]
- 18.Bair MJ, et al. Barriers and facilitators to chronic pain self-management: A qualitative study of primary care patients with comorbid muscoskeletal pain and depression. Pain Medicine. 2009;10:1280–90. doi: 10.1111/j.1526-4637.2009.00707.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arends RY, et al. The role of goal management for successful adoption to arthritis. Patient Education and Counseling. 2013;93:130–8. doi: 10.1016/j.pec.2013.04.022. [DOI] [PubMed] [Google Scholar]
- 20.Lorig K, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Lorig K, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization. Medical Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. American Psychologist. 2002;57(9):705–717. doi: 10.1037//0003-066x.57.9.705. [DOI] [PubMed] [Google Scholar]
- 23.Levack WM, et al. Is goal planning in rehabilitation effective? Clinical Rehabilitation. 2006;20:739–55. doi: 10.1177/0269215506070791. [DOI] [PubMed] [Google Scholar]
- 24.McGuire AB, et al. The “critical” elements of Illness Management and Recovery: Comparing methodological approaches. Administration and Policy in Mental Health and Mental Health Services Research. 2014:1–10. doi: 10.1007/s10488-014-0614-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthias MS, et al. A brief peer support intervention for veterans with chronic musculoskeletal pain: A pilot study of feasability and effectiveness. Pain Medicine. 2015;16:81–7. doi: 10.1111/pme.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borkan J. Immersion/Crystallization. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. 1999. pp. 179–94. [Google Scholar]
- 27.Adams N, Grieder D. Treatment planning for person-centered care. Amsterdam: Elsiver Academic Press; 2005. [Google Scholar]
- 28.Nicolaidis C. Police officer, deal-maker, or health care provider? Moving to a patient-centered framework for chronic opioid management. Pain Medicine. 2011;12:890–7. doi: 10.1111/j.1526-4637.2011.01117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prochaska JO, DiClemente CC. The transtheoretical approach: Crossing traditional boundaries of change. Homewood, IL: Dorsey Press; 1984. [Google Scholar]
- 30.Cohen S, Gottlieb B, Underwood LG. Social relationships and health. In: Cohen S, Underwood LG, Gottlieb B, editors. Social Support Measurement and Intervention: A Guide for Health and Social Scientists. Oxford University Press; Toronto: 2000. [Google Scholar]
- 31.Matthias MS, et al. An expanded view of self-managment: Patients' perceptions of education and support in an intervention for chronic pain. Pain Medicine. 2012;13:1018–28. doi: 10.1111/j.1526-4637.2012.01433.x. [DOI] [PubMed] [Google Scholar]
- 32.Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64:527–37. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Siegert RJ, McPherson KM, Taylor WJ. Toward a cognitive-affective model of goal-setting in rehabilitation: Is self-regulation theory a key step? Disability and Rehabilitation. 2004;26:1175–83. doi: 10.1080/09638280410001724834. [DOI] [PubMed] [Google Scholar]
- 34.Austin JT, Vancouver JB. Goal constructs in psychology: Structure, Process, and Content. Psychological Bulletin. 1996;120:338–375. [Google Scholar]
- 35.Gollwitzer PM. Implementation intentions: strong effects of simple plans. American Psychologist. 1999;54:493–503. [Google Scholar]
- 36.Gollwitzer PM, Brandstatter V. Implementation intentions and effective goal pursuit. Journal of Personality and Social Psychology. 1997;73:186–99. doi: 10.1037//0022-3514.81.5.946. [DOI] [PubMed] [Google Scholar]
- 37.Wood RE, Locke EA. Goal setting and stratgy effects on comples tasks. Research in Organizational Behavior. 1990;12:73–109. [Google Scholar]
- 38.Diefendorff JM, Lord RG. The volitional and strategic effects of planning on task performance and goal commitment. Human Performance. 2003;16:365–87. [Google Scholar]
- 39.Bandura A, Locke EA. Negative self-efficacy and goal effects revisited. Journal of Applied Psychology. 2003;88:87–99. doi: 10.1037/0021-9010.88.1.87. [DOI] [PubMed] [Google Scholar]
- 40.Bandura A. The role of self-efficacy in goal based motivation. In: Locke EA, Latham GP, editors. New developments in goal setting and task performance. Routledge/Taylor & Francis Group; New York: 2013. pp. 147–57. [Google Scholar]
- 41.Horvath A, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36(2):223–233. [Google Scholar]