When people with life threatening illnesses and their carers ask about prognosis (“How long have I got?”), they are often doing more than simply inquiring about life expectancy. Within this question is another, often unspoken, question about likely patterns of decline (“What will happen?”). One aid to answering both questions may be through the use of typical illness trajectories. Thinking in terms of these trajectories provides a broad timeframe and patterns of probable needs and interactions with health and social services that can, conceptually at least, be mapped out towards death.
Such frameworks may help clinicians plan and deliver appropriate care that integrates active and palliative management. If patients and their carers gain a better understanding by considering illness trajectories this may help them feel in greater control of their situation and empower them to cope with its demands. An important implication for service planners is that different models of care will be appropriate for people with different illness trajectories. We review the main currently described illness trajectories at the end of life and draw out key clinical implications.
Methods
We searched our own database of papers, conducted a Medline search, and approached experts for additional published references (further details available from SAM). We also re-examined primary data relating to illness trajectories from our previous studies investigating the palliative care needs of people with advanced lung cancer and heart failure.1
Different trajectories for different diseases
A century ago, death was typically quite sudden, and the leading causes were infections, accidents, and childbirth. Today sudden death is less common, particularly in Western, economically developed, societies. Towards the end of life, most people acquire a serious progressive illness—cardiovascular disease, cancer, and respiratory disorders are the three leading causes—that increasingly interferes with their usual activities until death.
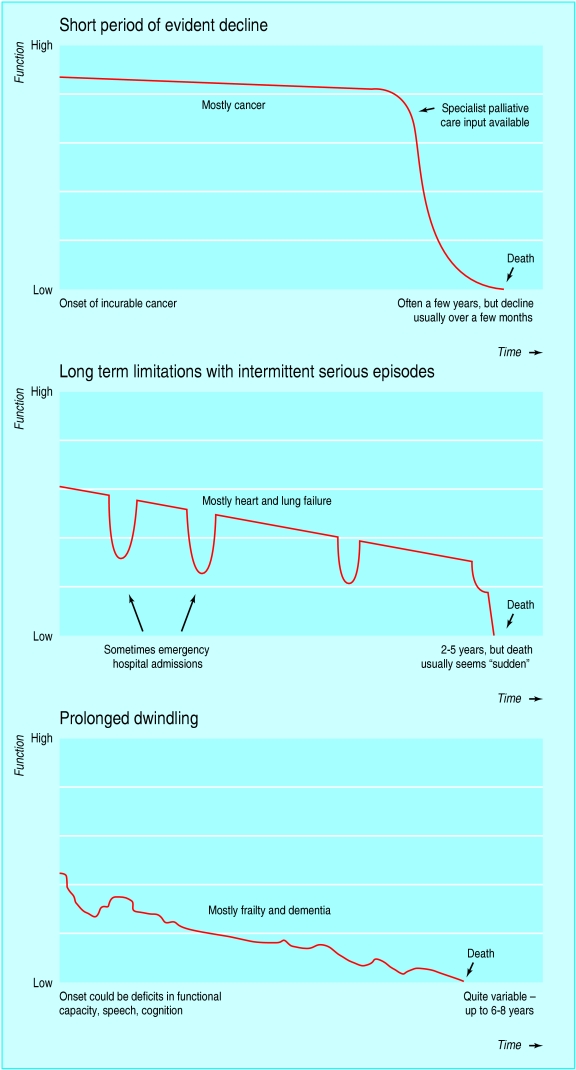
Three distinct illness trajectories have been described so far for people with progressive chronic illnesses (fig 1)2-6: a trajectory with steady progression and usually a clear terminal phase, mostly cancer; a trajectory (for example, respiratory and heart failure) with gradual decline, punctuated by episodes of acute deterioration and some recovery, with more sudden, seemingly unexpected death; and a trajectory with prolonged gradual decline (typical of frail elderly people or people with dementia).
Fig 1.
Typical illness trajectories for people with progressive chronic illness. Adapted from Lynn and Adamson, 2003.7 With permission from RAND Corporation, Santa Monica, California, USA.
Summary points
Three typical illness trajectories have been described for patients with progressive chronic illness: cancer, organ failure, and the frail elderly or dementia trajectory
Physical, social, psychological, and spiritual needs of patients and their carers are likely to vary according to the trajectory they are following
Being aware of these trajectories may help clinicians plan care to meet their patient's multidimensional needs better, and help patients and carers cope with their situation
Different models of care may be necessary that reflect and tackle patients' different experiences and needs
We now consider each of these three trajectories in more detail.
Trajectory 1: short period of evident decline, typically cancer
This entails a reasonably predictable decline in physical health over a period of weeks, months, or, in some cases, years. This course may be punctuated by the positive or negative effects of palliative oncological treatment. Most weight loss, reduction in performance status, and impaired ability for self care occurs in patients' last few months. With the trend towards earlier diagnosis and greater openness about discussing prognosis, there is generally time to anticipate palliative needs and plan for end of life care. This trajectory enmeshes well with traditional specialist palliative care services, such as hospices and their associated community palliative care programmes, which concentrate on providing comprehensive services in the last weeks or months of life for people with cancer. Resource constraints on hospices and their community teams, plus their association with dying, can limit their availability and acceptability. Box 1 illustrates this trajectory.
Trajectory 2: long term limitations with intermittent serious episodes
With conditions such as heart failure and chronic obstructive pulmonary disease, patients are usually ill for many months or years with occasional acute, often severe, exacerbations. Deteriorations are generally associated with admission to hospital and intensive treatment. This clinically intuitive trajectory has sharper dips than are revealed by pooling quantitative data concerning activities of daily living.4 Each exacerbation may result in death, and although the patient usually survives many such episodes, a gradual deterioration in health and functional status is typical. The timing of death, however, remains uncertain. In one large study, most patients with advanced heart failure died when expected to live for at least a further six months.8 Many people with end stage heart failure and chronic obstructive pulmonary disease follow this trajectory, but this may not be the case for some other organ system failures. Box 2 illustrates this trajectory.
Trajectory 3: prolonged dwindling
People who escape cancer and organ system failure are likely to die at an older age of either brain failure (such as Alzheimer's or other dementia) or generalised frailty of multiple body systems.7
This third trajectory is of progressive disability from an already low baseline of cognitive or physical functioning. Such patients may lose weight and functional capacity and then succumb to minor physical events or daily social “hassles” that may in themselves seem trivial but, occurring in combination with declining reserves, can prove fatal.9,10 This trajectory may be cut short by death after an acute event such as a fractured neck of femur or pneumonia. Box 3 illustrates this trajectory.
Clinical implications
Trajectories allow us to appreciate that “doing everything that can be done for a possible cure” may be misdirected.
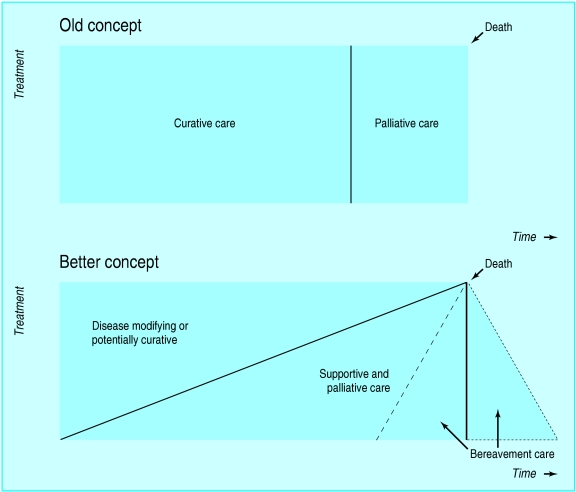
Optimising quality of life before a timely, dignified, and peaceful death are the primary aims of palliative care. Understanding and considering trajectories may help professionals take on board, at an earlier stage than would otherwise be the case, that progressive deterioration and death are inevitable. Before the terminal stages of a disease, some health professionals may allow the reality of the prognosis to remain unconsidered or unspoken, unwittingly colluding with patients and relatives in fighting death to the bitter end.11 Patients often want palliative oncological treatment even if it is extremely unlikely to benefit them, and doctors usually offer it to maintain hope as well as to treat disease.12 An outlook on death and expectations that are more acquiescent to reality may moderate the “technological imperative,” preventing unnecessary admissions to hospital or aggressive treatments. A realistic dialogue about the illness trajectory between patient, family, and professionals can allow the option of supportive care, focusing on quality of life and symptom control to be grasped earlier and more frequently. Figure 2 illustrates how the idea that palliative care is relevant only to the last few weeks of life is being replaced with the concept that the palliative care approach should be offered increasingly alongside curative treatment, to support people with chronic progressive illnesses over many years.
Fig 2.
Appropriate care near the end of life. Adapted from Lynn and Adamson, 2003.7 With permission from RAND Corporation, Santa Monica, California, USA
Box 1: Example of a cancer trajectory
CC, a 51 year old male shop assistant, complained of night sweats, weight loss, and a cough. An x ray initially suggested a diagnosis of tuberculosis, but bronchoscopy and a computed tomography scan revealed an inoperable, non-small cell lung cancer. He was offered and accepted palliative chemotherapy when he had already lost considerable weight (too much to allow him to enter a trial). The chemotherapy may have helped control his breathlessness, but he was subsequently admitted owing to vomiting. Looking back, CC (like several other patients in our study) expressed regret that he had received chemotherapy: “If I had known I was going to be like this....” His wife felt they had lost valuable time together when he had been relatively well.
CC feared a lingering death:
“I'd love to be able to have a wee turn-off switch, because the way I've felt, there's some poor souls go on for years and years like this, and they never get cured, I wouldn't like to do that.”
CC's wife, in contrast, worried that her husband might die suddenly: “When he's sleeping, I keep waking him up, I am so stupid. He'll say, `Will you leave me alone, I'm sleeping.'... He's not just going to go there and then, I know, but I've got to reassure myself.”
CC died at home three months after diagnosis, cared for by the primary care team, night nurses, and specialist palliative care services. His death had been discussed openly. He and his wife were confident that nursing, medical, and support staff would be available.
Box 2: Example of an organ failure trajectory
Mrs HH, a 65 year old retired bookkeeper (photo), had been admitted to hospital several times with cardiac failure. She was housebound in her third floor flat and cared for by a devoted husband who accepted little help from social work or community nursing. Previously she had been very outgoing, but she then became increasingly isolated. Her major concern was that her rapidly deteriorating vision because of diabetes prevented her completing crosswords, not that she had stage IV heart failure. Her treatment included high dose diuretics and long term oxygen therapy. She required frequent blood tests.
Figure 2.
She had raised her prognosis indirectly with her general practitioner, by mentioning to him that her grandson had asked her if she would be around at Christmas. Prognostic uncertainty was a key issue for many heart failure patients and their carers in our study, as illustrated by the following quotations.
“I take one step forward, then two steps back.” 84 year old, male, retired engineer, living alone, several recent admissions to hospital.
“I'd like to get better, but I keep getting worse.” 72 year old widow, living alone, psoriasis and arthritis.
“Things I used to take for granted are now an impossible dream.” 75 year old man, large family nearby, recently celebrated 50th wedding anniversary.
“There were times last year, when I thought I was going to die.” 77 year old woman, living alone, several periods in hospital with acute breathlessness.
“It could happen at any time.” Wife of 62 year old former footballer and taxi driver.
“I know he won't get better, but don't know how long he's got.” Wife of 77 year old retired flour mill worker with severe asthma.
Mrs HH died on the way home from a hospital admission due to a nosebleed. She had had these occasionally as she had hypertension and a perforated nasal septum. Attempted resuscitation took place in the ambulance. Her husband later expressed deep regret that his wife's clear wish not to have her life prolonged was not respected.
Box 3: Example of frailty trajectory
Mrs LC, a 92 year old widow, lives alone in a ground floor flat in central Edinburgh.
Figure 3.

Bereaved 12 years ago, she is now housebound due to arthritis and general physical frailty.
She used to venture out occasionally to the shops but over the years has felt less able and confident, largely because of a fear of falling. She appreciates the chair and walking aids supplied by the occupational therapist as these provide support and a sense of security at home. Since a “little fright” she had before Christmas when her legs gave way, she retires to bed earlier than before.
She receives regular visits from friends and the local church and is undemanding of services. Current medications are paracetamol, thyroxin, and bendrofluazide (for hypertension) and an annual influenza vaccine.
Mrs LC understands her current trajectory in terms of gradual decline in activities that she is able to do, and she is concerned that she might one day lose her independence. She has no relatives but is supported by her trust in God, who has “given me a good while on the planet, and should be sending for me now.”
Trajectories allow practical planning for a “good death”
Dying at home is the expressed wish of around 65% of people at the beginning of the cancer and organ failure trajectories.13 An appreciation that all trajectories lead to death, but that death may be sudden (particularly in patients following trajectory 2), makes it evident that advanced planning is sensible. Eliciting the “preferred place of care” is now standard in some palliative care frameworks and helps general practitioners plan for terminal care where the patient and family wish. This may increase the likelihood of patients dying in the place of their choice, as was the case for CC (see box 1).
Sensitive exploration is needed and can allow issues such as resuscitation status to be clarified and “unfinished business” to be completed for patients on all these trajectories. However, advance directives may be ignored in the heat of the moment.14 Mrs HH's death had (unusually in people with heart failure) been planned, but an emergency overtook the situation and she received inappropriate resuscitation as documentation was not at hand. Living wills (advance directives) may be becoming more popular with patients, but most primary care professionals still have relatively little experience with these (Polack C, personal communication, 2004). Such planning may be particularly relevant to people in the third trajectory, where progressive cognitive decline is common.
Understanding the likely trajectory may be empowering for patient and carer
Some patients attempt to gain control over their illness by acquiring knowledge about how it is likely to progress.15,16 Had CC (box 1), who had lung cancer, been aware of his likely course of decline he might have been less worried about a very protracted death. Similarly, his wife might have been less worried about a sudden death. Both gave clear cues in the research interviews that they were concerned about the possible nature of the death and would have welcomed sensitive discussion of this with health professionals.
Limitations of the trajectory approach
The trajectory approach gives a conceptual overview, but patients must not be simply slotted into a set category without regular review. Individual patients will die at different stages along each trajectory, and the rate of progression may vary. Other diseases or social and family circumstances may intervene, so that priorities and needs change. Some people cope by denial or disavowal, making open communication less appropriate in the earlier stages.17
Some illnesses might follow none, any, or all of the trajectories: a severe stroke could, for example, result in sudden death or a fairly acute decline as in trajectory 1; a series of smaller strokes and recovery could mimic trajectory 2; while a gradual decline with progressive disability could parallel trajectory 3. Renal failure might represent a fourth trajectory consisting of a steady decline, with the rate of decline dependent on the underlying pathology and other patient related factors such as comorbidity.2 Patients with multiple disorders may have two trajectories running concurrently, with the more rapidly progressing trajectory typically taking centre stage. This is not uncommon in older patients with slowly progressive cancers.
Other dimensions of needs may have different trajectories
The trajectories we have considered relate to physical wellbeing. Other trajectories may exist regarding dimensions such as the spiritual or existential domain. In cancer patients, we have noted that spiritual distress and questioning may peak at diagnosis, again at the time of recurrence, and then later during the terminal stage. Spiritual distress in people with heart failure may, in contrast, be evident more uniformly throughout the trajectory, reflecting the gradual loss of identity and growing dependence.18 Psychological and social trajectories may also potentially be mapped. In dementia, the loss of cognitive function may cause parallel loss in activities of daily living, social withdrawal, and emotional distress.
Implications for service planning and development
One size may not fit all
Different models of care will be appropriate for people with different illness trajectories. The typical model of cancer palliative care might not suit people who have a gradual, progressive decline with unpredictable exacerbations.
People with non-malignant disease may have more prolonged needs, but these are as pressing as those of people with cancer. Uncertainty about prognosis should not result in these patients, and their families, being relatively neglected by health and social services.3,4 A strategic overview of the needs of and services available to people on the main trajectories may help policies and services to be better conceptualised, formulated, and developed to consider all people with serious chronic illnesses.
Planning care in advance may prevent admissions
Planning care and providing resources in advance on the basis of these trajectories might help more people die where they prefer. For example, many frail elderly and patients with dementia are currently admitted to hospital to die when terminally ill. The use of end of life care pathways in nursing homes is proving increasingly effective in preventing such admissions.13
Transferable lessons
Models of care for one trajectory may inform another. For example, cancer care can learn from the health promotion paradigm already established in the management of chronic diseases. Improving living while near death in North America19 and “health promoting palliative care” in Australia are two such examples. These have the potential to destigmatise death and maximise cancer patients' quality of life right up to death. Conversely, patients with organ failure could benefit from ideas developed in cancer care, such as advanced care planning frameworks and end of life pathways.20,21
There are striking similarities between the burden of symptoms at any time of patients dying of cancer and those dying of non-malignant cardiorespiratory disease.22 Hospital palliative care teams, through offering specialist advice and sharing care with other specialists, can improve the care of many non-cancer patients.23
Conclusions
The key to caring well for people who will die in the (relatively) near future is to understand how they may die, and then plan appropriately. Since diseases affect individuals in different ways, prognosis is often difficult to estimate. None the less, it seems that patients with specific diseases and their carers often have common patterns of experiences, symptoms, and needs as the illness progresses. The notion of typical or characteristic trajectories is therefore conceptually sustainable and borne out in our longitudinal qualitative studies. Three typical trajectories have been described so far, and others may be characterised soon. More research is now needed to help understand how the insights offered by these trajectories can be translated into improvements in outcomes for patients and their families.
In Hippocrates' day, the physician who could fore-tell the course of the illness was most highly esteemed, even if he could not alter it.24 Nowadays we can cure some diseases and manage others effectively. Where we cannot alter the course of events we must at least (when the patient so wishes) predict sensitively and together plan care, for better or for worse.
Additional educational resources
For clinicians
Lynn J, Schuster JL, Kabcenell A. Improving care for the end of life: a sourcebook for health care managers and clinicians. New York: Oxford University Press, 2000.
WHO Europe. Better palliative care for older people. Copenhagen: WHO, 2004.
Thomas K. Caring for the dying at home. Companions on a journey. Oxford: Radcliffe Medical Press, 2003.
Macmillan Cancer Relief. Our principles of patient-centred care. London: Macmillan Cancer Relief, 2004. www.professionalresources.org.uk/Macmillan
NHS Modernisation Agency. Liverpool care pathway. Promoting best practice for the care of the dying. User Guide. Liverpool: NHS Modernisation Agency, 2004. www.lcp-mariecurie.org.uk
Lynn J. Sick to death and not going to take it any more. Reforming health care for the last years of life. Berkeley, Ca: University of California Press, 2004.
For patients and carers
DIPEx. Personal experiences of health and illness (www.dipex.org)—allows patients and carers to learn about cancer and other illnesses through sharing other people's personal experiences.
BBC Online. Health (www.bbc.co.uk/health)—gives information on a range of illnesses and conditions.
Growth House Inc (www.growthhouse.org)—provides patients and professional resources for life-threatening illness and end of life care.
UK Self Help (www.ukselfhelp.info)—provides a list of UK self help websites.
Lynn J, Harrold J. Handbook for mortals: guidance for people facing serious illness. New York: Oxford University Press, 1999.
We would like to acknowledge the pioneering work of Joanne Lynn and colleagues at the Washington Home Centre for Palliative Care Studies, and June Lunney and colleagues at the National Institute of Aging, National Institutes of Health, Bethesda, USA, in the area of illness trajectories.
Contributors: All authors wrote the paper. MK provided the research data. SAM is the guarantor.
Funding: The Chief Scientist Office, Scottish Executive, funded the original research.
Competing interests: None declared.
Ethical approval: The local ethics committee and primary care and hospital trusts granted ethical approval.
References
- 1.Murray SA, Boyd K, Kendall M, Worth A, Benton TF. Dying of lung cancer or cardiac failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325: 929-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murtagh FEM, Preston M, Higginson I. Patterns of dying: palliative care for non-malignant disease. Clin Med 2004;4: 39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Palliative care: the solid facts. Europe: WHO, 2004.
- 4.Lunney JR, Lynn J, Foley DS, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA 2003;289: 2387-92. [DOI] [PubMed] [Google Scholar]
- 5.Lehman R. How long can I go on like this? Dying from cardiorespiratory disease. Br J Gen Pract 2004;54: 892-3. [PMC free article] [PubMed] [Google Scholar]
- 6.Glare PA, Christakis NA. Predicting survival in patients with advanced disease. In Doyle D, Hanks G, Cherny N, Calman K, eds. Oxford textbook of palliative medicine. Oxford: Oxford University Press, 2004.
- 7.Lynn J, Adamson DM. Living well at the end of life. Adapting health care to serious chronic illness in old age. Washington: Rand Health, 2003.
- 8.Levenson JW, McCarthy EP, Lynn J. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc 2000;48: S101-9. [DOI] [PubMed] [Google Scholar]
- 9.Ballam M, Porter M, Bagely SD, Hockey L, Murray SA. Cumulative trivia: exploratory focus group work. Edinburgh: Edinburgh University, 2001.
- 10.Williams R, Zyzanski SJ, Wright A. Life events and daily hassles and uplifts as predictors of hospitalisation and out patient visitation. Soc Sci Med 1992;34: 763-8. [DOI] [PubMed] [Google Scholar]
- 11.Higgs R. The diagnosis of dying. J R Coll Physicians Lond 1999;33: 110-2. [PMC free article] [PubMed] [Google Scholar]
- 12.Slevin ML, Stubbs L, Plant HJ, Wilson P, Gregory WM, Armes PJ. Attitudes to chemotherapy: comparing views of patients with those of doctors, nurses and general public. BMJ 1990;300: 1458-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higginson I,.Sen-Gupta GJA. Place of care in advanced cancer. J Palliat Med 2004;3: 287-300. [DOI] [PubMed] [Google Scholar]
- 14.Hardin SB, Yusufaly YA. Difficult end-of-life treatment decisions: do other factors trump advance directives? Arch Intern Med 2004;164: 1531-3. [DOI] [PubMed] [Google Scholar]
- 15.Asbring P, Narvanen AL. Patient power and control: a study of women with uncertain illness trajectories. Qual Health Res 2004;14: 226-40. [DOI] [PubMed] [Google Scholar]
- 16.Burke SO, Kauffmann E, LaSalle J, Harrison MB, Wong C. Parents' perceptions of chronic illness trajectories. Canadian J Nurs 2000;32: 19-36. [PubMed] [Google Scholar]
- 17.Buetow S, Coster G. Do general practice patients with heart failure understand its nature and seriousness, and want improved information? Patient Educ Couns 2001;45: 181-5. [DOI] [PubMed] [Google Scholar]
- 18.Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliat Med 2004;18: 39-45. [DOI] [PubMed] [Google Scholar]
- 19.Lynn J. Learning to care for people with chronic illness facing the end of life. JAMA 2000;284: 2508-11. [DOI] [PubMed] [Google Scholar]
- 20.Thomas K. Caring for the dying at home. Companions on a journey. Oxford: Radcliffe Medical Press, 2003.
- 21.Ellershaw JE, Wilkinson S. Care of the dying: A pathway to excellence. Oxford: Oxford University Press, 2003.
- 22.McKinley RK, Stokes T, Exley C, Field D. Care of people dying with malignant and cardiorespiratory disease in general practice. Br J Gen Pract 2004;54: 909-13. [PMC free article] [PubMed] [Google Scholar]
- 23.Kite S, Jones K, Tookman A. Specialist palliative care and patients with non-cancer diagnosis: the experience of a service. Palliat Med 2001;15: 413-8. [DOI] [PubMed] [Google Scholar]
- 24.Cassell E. The nature of suffering. New York: Oxford University Press, 1991.