Abstract
This study aimed to evaluate the self-reported prevalence of burnout and psychological morbidity among radiation oncologists members of the Kyoto Radiation Oncology Study Group (KROSG) and to identify factors contributing to burnout. We mailed an anonymous survey to 125 radiation oncologists members of the KROSG. The survey included; the demographic data, the Maslach Burnout Inventory – Human Services Survey (MBI-HSS) and the 12-item General Health Questionnaire (GHQ-12). There were 87 responses out of 125 eligible respondents (69.6% response rate). In terms of burnout, three participants (3.4%) fulfilled the MBI-HSS criteria of having simultaneously high emotional exhaustion (EE), high depersonalization (DP) and low sense of personal accomplishment (PA). Eighteen (20.6%) reported a high score for either EE or DP meeting the alternative criteria for burnout with three of these simultaneously having high EE and high DP. The prevalence of psychological morbidity estimated using GHQ-12 was 32%. A high level of EE and low level of PA significantly correlated with high level of psychological morbidity with P < 0.001 and <0.01 respectively. Having palliative care activities other than radiotherapy and number of patients treated per year were the only factors associated with burnout. This is the first study investigating the prevalence of burnout and psychological morbidity among radiation oncologists in Japan. Compared with other studies involving radiation oncologists, the prevalence of low personal accomplishment was particularly high in the present study. The prevalence of psychological morbidity was almost the double that of the Japanese general population and was significantly associated with low PA and high EE.
Keywords: burnout, depression, radiation oncologists, Japan
INTRODUCTION
Burnout is a stress-induced syndrome defined by three dimensions: emotional exhaustion (EE; a loss of enthusiasm for work), depersonalization (DP; a feeling of cynicism) and low sense of personal accomplishment (PA; perspective that work is meaningful). Burnout is frequently observed in workers that spend considerable time in intense involvement with other people. This is the case for physicians in general, and oncologists in particular [1, 2]. Burnout has been linked to job turnover, absenteeism and low morale; in physicians it has also been linked to poor quality of life, increased suicidal ideation, poorer quality of care, increased medical errors and lawsuits, and decreased empathy [1, 3–5].
The practice of oncology, although rewarding, is by nature one of the most demanding and stressful areas in medicine, since the oncologist needs to face life-and-death decisions, deal with patients’ existential questions, and deal with the conflict between the curative goals (on which most training is based) and the palliative goals (of much cancer care) on a daily basis [2, 6]. This probably explains the high level of burnout reported among oncologists. In a survey of 1000 randomly selected physician subscribers to the Journal of Clinical Oncology, 56% reported to be suffering burnout [7]. Trufelli et al. (in a systematic review and meta-analysis including 10 observational studies) reported a prevalence of 36% [95% confidence interval (CI) (31–41)], 34% [95% CI (30–39)] and 25% [95% CI (0.16–34)], respectively, for EE, DP and PA. Severe involvement by any one of the three dimensions ranged from 8% to 51%, revealing the heterogeneity of the different studies. This heterogeneity may result from differences in culture, national labor policies, personal philosophic background and the manner of facing difficult issues such as death and suffering [8, 9]. Hence, there is a need to investigate the prevalence of and factors associated with burnout in various contexts in order to better define the most appropriate strategies to be implemented.
Several studies on burnout in oncology professionals have been recently published [10–14]. In Japan, research on burnout in healthcare professionals has been mostly carried out on nurses; few studies have involved physicians in general, and even fewer have involved oncology professionals [15–20]. Asai et al. reported a prevalence of 22% for EE, 11% for DP and 62% for low PA among clinical oncologists and palliative care physicians involved in end-of-life care of cancer patients in Japan. However, no study has been conducted in Japan to evaluate the prevalence of burnout and its characteristics in Japanese radiation oncologists. In a survey investigating the burden on radiation oncologists working either alone or with only one colleague in community hospitals in Japan, 60% of the 51 respondents (out of 250 surveyed) reported to be satisfied with their work. However, they also reported insufficient vacation time, the difficulty of getting other colleagues’ opinions about a case, insufficient time for continued medical education, and a need for more part-time radiation oncologists, radiation oncology nurses and paramedical staff to reduce their heavy workload. Job satisfaction has also been reported in many studies investigating burnout among physicians; yet in those studies, insufficient personal and/or vacation time and heavy workload were frequently reported as reasons explaining the existence of burnout [7].
The present study is the first aiming to determine the prevalence of burnout and depression among radiation oncologists and to reveal the various associated factors. This study targeted radiation oncologist members of the Kyoto Radiation Oncology Study Group (KROSG).
METHODS
The study received the approval of the board members of the KROSG. In December 2015, a cross-sectional survey was mailed to all board-certified and in-training radiation oncologists registered in the KROSG membership list (see supplemental material). Non-respondents were reminded to complete the survey on a subsequent meeting of the association held early January 2016. The study questionnaire consisted of the following instruments:
Demographic parameters
The demographic data, including sex, age, current marital status and professional status, number of children <22 years old, years in practice, as well as variables related to practice patterns (Table 1).
Table 1.
Description of the study population (N = 87)
| Variables | N | % |
|---|---|---|
| Sex | ||
| Male | 70 | 80 |
| Female | 17 | 20 |
| Age | ||
| 20–29 | 10 | 12 |
| 30–39 | 27 | 31 |
| 40–49 | 23 | 26 |
| 50–59 | 20 | 23 |
| 60–69 | 6 | 7 |
| ≥70 | 1 | 1 |
| Marital status | ||
| Married | 77 | 89 |
| Single | 10 | 11 |
| Children <22 years old | ||
| Yes | 58 | 67 |
| No | 29 | 33 |
| No. of years of experience | ||
| ≤5 | 17 | 19 |
| 6–10 | 20 | 23 |
| 11–20 | 24 | 28 |
| 21–30 | 20 | 23 |
| ≥31 | 6 | 7 |
| Board certification | ||
| Yes | 63 | 73 |
| No | 23 | 27 |
| Data missing | 1 | |
| Work sector | ||
| University hospital | 38 | 44 |
| Research institute | 4 | 5 |
| Public medical institution | 27 | 31 |
| General hospital | 18 | 20 |
| Working days/week | ||
| ≤2 | 5 | 6 |
| 3 | 2 | 2 |
| 4 | 4 | 5 |
| ≥5 | 76 | 87 |
| Hours worked/week | ||
| <32 | 8 | 9 |
| 32–40 | 9 | 10 |
| 41–50 | 23 | 26 |
| 51–60 | 31 | 36 |
| ≥61 | 16 | 18 |
| Dedicated time for CME | ||
| Yes | 67 | 78 |
| No | 19 | 22 |
| Data missing | 1 | |
| Research activities | ||
| Yes | 47 | 54 |
| No | 40 | 46 |
| Practice of pediatric oncology | ||
| Yes | 27 | 31 |
| No | 60 | 69 |
| Practice of diagnostic radiology | ||
| Yes | 25 | 29 |
| No | 62 | 71 |
| Practice of chemotherapy | ||
| Yes | 14 | 16 |
| No | 72 | 84 |
| Data missing | 1 | |
| Palliative care activities other than RT | ||
| Yes | 16 | 18 |
| No | 71 | 82 |
| Number of patients treated/year | ||
| <120 | 22 | 25 |
| 120–250 | 48 | 55 |
| >250 | 17 | 20 |
CME = continuing medical education, RT = radiotherapy.
Burnout
Among the psychometric instruments used to measure burnout, the Maslach Burnout Inventory (MBI) has shown to be the most widely used standardized measure of burnout. The MBI-HSS is comprised of a 22-item questionnaire that evaluates all of the three dimensions of burnout (EE, DP and PA) and has been validated in several languages, including Japanese [21]. The MBI-HSS uses a 7-point Likert scale ranging from 0 (never) to 6 (every day). The total score for each subscale was categorized as low, medium or high. Based on normative data from 1104 medical professionals, a high level of burnout is considered to be indicated by a score ≥27 in the EE subscale, ≥10 in the DP subscale and ≤33 in the PA subscale [22]. Although the classic definition of burnout implies the combination of high EE, high DP and low PA, an alternative definition of burnout commonly found in the literature only requires a high score in the EE and DP subscales, defined as the core burnout dimensions [3, 12, 23, 24].
Psychological morbidity
The 12-item General Health Questionnaire (GHQ-12) is a self-administered screening questionnaire, designed for use in consulting settings and aimed at either detecting individuals with a diagnosable psychiatric disorder or as a general measure of psychiatric well-being [25]. We used the validated Japanese version to assess depression and general psychiatric well-being [26–28]. We used the bimodal scaling system, in which the four options for each question were scored 0, 0, 1 and 1, respectively. This scaling has been reported to agree better with the 12-item version of the GHQ than the other two scaling systems, namely the Likert scoring system and the C-GHQ. Psychological morbidity was defined as a score of 4 or more on the GHQ-12 [25].
Statistical analysis
Correlation between the GHQ-12 and MBI-HSS scores was evaluated using multiple linear regression instead of logistic regression, following the recommendation by Maslach to use the individual domain score as continuous data when comparing symptoms of burnout and other outcomes [12, 22, 29].
We also performed multivariate linear regression analysis to identify patient characteristics associated with burnout and psychological morbidity.
All statistical analysis was undertaken using SPSS v.20.0 (SPSS Inc., 2003, Chicago, USA). P values < 0.05 were considered significant.
RESULTS
Demographic parameters
Of the 125 board-certified and in-training radiation oncologists to whom the questionnaire was mailed, 86 responded within 3 weeks, and 2 after a reminder. One response didn't meet the criteria for analysis, so 87 responses were analyzed, representing an overall response rate of 69.6%. Eighty percent of the participants were male, and there was a median age of 43 years. They were mostly board certified (73%), with 44% working in university hospitals and 31% in public medical institutions. The average weekly working time was 49 h, with 55% treating between 120 and 250 patients per year. Other relevant demographic parameters are summarized in Table 1.
Prevalence of burnout and psychological morbidity
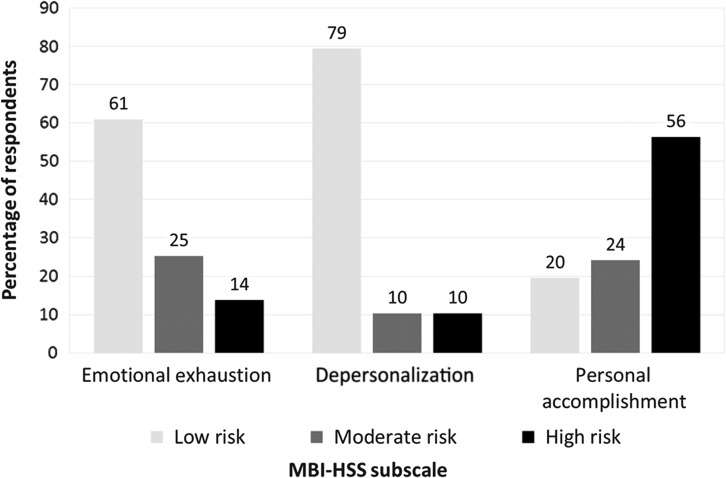
The prevalence of burnout is shown in Fig. 1. Three participants (3.4%) fulfilled the MBI-HSS criteria of having simultaneously high EE, high DP and low PA. Eighteen (20.6%) reported a high score for either EE or DP, meeting the alternative criteria for burnout, with three of these simultaneously having high EE and high DP. A simultaneous high score in EE and DP was always associated with a low score in the PA subscale (100%). Forty-nine (56%) of the respondents scored low in the PA subscale, while 10 respondents (11%) scored low in all three subscales of the MBI-HSS.
Fig. 1.
Percentage of respondents in each MBI-HSS subscale score.
Overall, the psychological morbidity rate was 32% among all the respondents. The three respondents who scored high in the EE and DP subscales and low in the PA subscale all had a GHQ-12 score ≥4. Table 2 shows the association between high level of burnout and psychological morbidity. A high level of EE and a low level of PA were significantly associated with a high level of psychological morbidity, with P < 0.001 and <0.01, respectively. On the other hand, without being statistically significant, the DP score tended to be negatively associated with the GHQ-12 score (P = 0.48).
Table 2.
Association between MBI-HSS scores and psychological morbidity
| Psychological morbidity | |||
|---|---|---|---|
| Coefficient (SD) | 95% CI | P value | |
| EE score | 0.16 (0.04) | 0.08–0.24 | <0.001 |
| DP score | −0.05 (0.08) | −0.22–0.10 | 0.48 |
| PA score | −0.1 (0.03) | −0.18− −0.03 | <0.01 |
EE = emotional exhaustion, DP = depersonalization, PA = sense of personal accomplishment.
Factors associated with burnout and psychological morbidity
Table 3 shows the association between participants’ characteristics and burnout level/psychological morbidity. Having palliative care activities other than radiotherapy and a high number of patients treated per year were significantly associated with a high level of EE (P = 0.04 and P = 0.01 respectively), while having palliative care activities other than radiotherapy was the only factor that was significantly associated with a high level of DP (P = 0.01). On the other hand, none of the factors investigated were significantly associated with a low PA.
Table 3.
Factors associated with burnout and psychological morbidity
| Emotional exhaustion | Depersonalization | Personal accomplishment | Psychological morbidity | |
|---|---|---|---|---|
| β (P value) | β (P value) | β (P value) | β (P value) | |
| Sex | −0.03 (0.84) | 0.07 (0.58) | −0.08 (0.55) | −0.10 (0.48) |
| Age (<40 vs ≥40) | 0.01 (0.97) | −0.08 (0.60) | 0.13 (0.41) | −0.15 (0.35) |
| Marital status | 0.00 (0.98) | 0.06 (0.64) | −0.20 (0.17) | 0.16 (0.29) |
| Children <22 years old | −0.08 (0.53) | 0.11 (0.40) | 0.16 (0.26) | −0.06 (0.66) |
| Years of experience (≤5 vs >5) | 0.14 (0.52) | 0.23 (0.31) | 0.10 (0.67) | 0.21 (0.37) |
| Board certification | −0.21 (0.33) | −0.32 (0.14) | −0.04 (0.85) | −0.10 (0.68) |
| Work sectora | 0.03 (0.83) | 0.24 (0.14) | −0.02 (0.89) | 0.02 (0.90) |
| Working days/week (<5 vs ≥5) | 0.04 (0.74) | −0.04 (0.75) | 0.17 (0.22) | −0.09 (0.55) |
| Hours worked/week (≤50 vs >50) | −0.14 (0.28) | −0.01 (0.96) | −0.06 (0.68) | 0.19 (0.20) |
| Dedicated time for CME | −0.12 (0.31) | 0.12 (0.35) | 0.03 (0.83) | −0.08 (0.56) |
| Research activities | 0.08 (0.59) | −0.07 (0.62) | 0.00 (0.99) | 0.14 (0.38) |
| Practice of pediatric oncology | 0.04 (0.75) | 0.02 (0.89) | 0.00 (0.98) | 0.02 (0.86) |
| Practice of diagnostic radiology | −0.15 (0.22) | −0.17 (0.17) | −0.02 (0.88) | −0.05 (0.73) |
| Practice of chemotherapy | 0.04 (0.74) | −0.04 (0.77) | 0.17 (0.23) | −0.15 (0.30) |
| Palliative care activities other than radiotherapy | 0.26 (0.04)b | 0.35 (0.01)b | 0.02 (0.87) | 0.01 (0.95) |
| Number of patients treated/yearc | 0.35 (0.01)b | 0.18 (0.22) | 0.16 (0.27) | 0.10 (0.49) |
β = standardized coefficient, CME = continued medical education.
a Coded as: 0 = public medical institution,1 = general hospital, 2 = university hospital or research institutions.
b Statistically significant variable (P < 0.05).
c Coded as: 0 = < 120, 1= between 120 and 250, 2 = >250.
DISCUSSION
Several studies have recently been published on burnout in oncology professionals [2, 6–8, 18]. However, only a few of them specifically deal with burnout in radiation oncologists. Table 4 summarizes some of the studies that used the MBI as a tool for evaluation of burnout, for better comparison with the present study. Our study, to the best of our knowledge, is the first study to investigate the prevalence of burnout and psychological morbidity in radiation oncology professionals in Japan. Our results show that 14% of the respondents had a high level of EE, 10% had a high level of DP, and 56% had a low level of PA. In comparison with previous studies carried out in Western countries, our study shows a lower level of EE and DP and a higher level of low PA [12, 13, 30–32]. However, our results are consistent with those of another study carried out among palliative care physicians and clinical oncologists in Japan by Asai et al., in which the rate of EE, DP and low PA were 22%, 11% and 62%, respectively [18]. It is notable that a particularly high rate of low PA is reported in most Japanese studies compared with the rates reported in studies in Western countries [18, 19, 33]. This may be due to cultural differences from the West regarding work attitude [19]. In our study, participants who were not board-certified (in-training) had a high level of DP (17% vs 8%) and low PA (61% vs 54%) compared with those who were board certified, while the latter had a higher level of EE (14% vs 13%). Very few studies have directly compared burnout patterns between radiation oncology residents and specialists, but it is well documented that the risk factors associated with burnout differ between residents and specialists [32, 34]. Panagopoulou et al. reported a higher level of EE and DP in internal medicine residents compared with specialists. In their study, medical residents reported working more hours per week (which strongly correlated with DP) and perceived their job as more demanding in terms of time pressure and mental effort than medical specialists [34]. Working hours and lack of control, probably due to inexperience, have also been identified as factors contributing to residents’ burnout in a systematic review [35]. In our study, respectively 35% and 11% of in-training and board-certified radiation oncologists reported to work ≥61 h per week. This might be a possible explanation for the difference observed between in-training and board-certified radiation oncologists in this study (especially for DP rate), although the difference between the two groups did not reach statistical significance. Blanchard et al. reported an overall burnout rate of 46% among French radiation oncology residents, with EE and DP rates of 25% and 41%, respectively [12]. They did not report the PA rate, but their EE and DP rates were higher than that of in-training radiation oncologists in our study, confirming the overall tendency discussed above.
Table 4.
Recent studies on burnout evaluated with the MBI among radiation oncologists
| Authors and year of publication | Country | Type of interview | Total number of surveyed (response rate) | Type of oncology professional who participated in the survey | GHQ-12 (%) | EE (%) | DP (%) | PA (%) |
|---|---|---|---|---|---|---|---|---|
| Leung et al. (2014) [30] | Australia and New Zealand | Online survey | 348 (63.2%) | Radiation oncologists | Not applied | 21.8 | 19.2 | 24.1 |
| Kusano et al. (2014) [13] | United states | Online survey | 87 (76%) | Academic chairs of radiation oncology programs | Not applied | 25 | 10 | 15 |
| Aggarwal et al. (2015) [31] | United states | Online survey | 88 (53%) | Radiation oncology residency program directors | Not applied | 28 | 15 | 32 |
| Ciammella et al. (2013) [32] | Italia | Mailed survey | 400 (28%) | Radiation oncologist aged < 40 years old | Not applied | 9 | 26 | 8 |
| Blanchard et al. (2010) [12] | France | Handed/mailed survey | 340 (60%) | Medical, radiation and hemato-oncology residents | Not applied | 25a | 41a | |
| Our study | Japan | Mailed survey | 125 (69.6%) | Board-certified and in-training radiation oncologists | 32 | 14 | 10 | 56 |
aMBI = Maslach Burnout Inventory, EE = emotional exhaustion, DP = depersonalization, PA = low sense of personal accomplishment, GHQ-12 = 12-item general health questionnaire.
Several definitions of clinical burnout have been proposed in the literature [12, 22, 23, 36]. In this study, participants were considered as suffering clinical burnout if they had a coexistence of high EE, high DP and low PA scores in the three subscales of the MBI-HSS (classic definition) or they scored high in the core components of the MBI-HSS, that is EE or DP subscales (alternative criteria). Based on the classic definition and the alternative criteria for the existence of burnout, 3.5% and 20.6% of the respondents were, respectively, suffering clinical burnout. Considering the classic definition, our result was comparable with the results of other studies that reported 3%, 0% and 6% among Australian and New Zealand radiation oncologists, the chairs of radiation oncology programs, and radiation oncology residency program directors in the USA, respectively [13, 30, 31]. However, based on the alternative definition, our study shows a relatively lower level of burnout (20.6%) than that reported in the literature among radiation oncologists (>30%). Despite that, we would like to emphasis that one out of five respondents in this study reported to be suffering clinical burnout, and 35% of respondents met the criteria for moderate burnout. Additionally, a significant number of respondents had at least one manifestation of burnout. These are grounds for concern.
The prevalence of psychological morbidity was 32% in this study. This was higher than that among Japanese clinical oncologists and palliative care physicians reported by Asai et al. (20%) and almost the double of that of the general population of Japan [18, 37]. Studies using the GHQ-12 among radiation oncologists are scarce; however, the prevalence in this study (Fig. 1) compared well with that reported among oncology professionals in general (25–32%). In Asai's study, high level of EE and low level of PA were significantly associated with psychological morbidity. A significant association was also found between high level of EE and low level of PA with psychological morbidity in the present study (P < 0.001 and P < 0.01, respectively). This suggests that an increased sense of PA and low level of EE may reduce the risk of psychological morbidity.
Having palliative care activities other than radiotherapy, and the number of patients treated per year were the only factors associated with EE, while having palliative care activities other than radiotherapy was the only factor associated with DP. However, no associations were found between the participants’ characteristics and PA or psychological morbidity. Among the 16 radiation oncologists doing palliative care other than radiotherapy, 8 were working at university hospitals and 8 (50%) reported chemotherapy as part of their practice. Thirteen treated >120 patients per year, and 4 (25%) treated >250 patients per year.. Treating more patients can result in excess workload, which has been reported to be one of the central factors contributing to burnout among physicians [2]. Palliative care physicians have been reported to have a lower burnout level compared with other oncology physicians [6, 18]. The association with EE and DP found in the present study may then be due to a lack of sufficient training of radiation oncologists regarding the administration of palliative care not related to radiotherapy (probably chemotherapy-related). However, a more complex interaction between several risk factors is highly probable and should be addressed in future research with a larger sample.
Our findings should be interpreted with caution due to several limitations. First of all, the cross-sectional nature of the study does not allow the establishment of a causal relationship between burnout and psychological morbidity, or between the respondents’ characteristics and burnout or psychological morbidity. Second, like most studies evaluating burnout and psychological morbidity, the standardized questionnaire used relies on self-reporting and might not correspond to reality. Third, the limited number of participants recruited from one hospital network, even though geographically dispersed, limited the possibility of performing more subclass analysis and compromised our ability to generalize our results. Finally, since radiation oncology is a multidisciplinary field, including radiation therapists, nurses, physicists and dosimetrists might allow for a broader-based definition of factors associated with burnout in radiation oncology professionals.
Our study has several important strengths. First, to our knowledge, our study is the first to evaluate burnout among radiation oncologists in Japan, and achieved a good survey response rate. Second, the prevalence of burnout and psychological morbidity, and the trends in the various components of burnout in our study, are similar to those of other studies involving oncology professionals in Japan, which suggests that our results reflects the typical trends observed among oncologists in Japan [18]. Last but not least, we used validated metrics to measure burnout and psychological morbidity, which allowed comparison with other studies involving radiation oncologists and the general population.
We believe that additional studies are needed to address the above-mentioned limitations, but this work, as a preliminary study, provides a basis for future research to help improve not only the professionals’ well-being, but also quality of care for the patients.
In conclusion, this is the first study investigating the prevalence of burnout and depression among radiation oncologists in Japan. Compared with other studies involving radiation oncologists, the prevalence of low PA was found to be particularly high in the present study. The prevalence of psychological morbidity was almost the double that of the Japanese general population and was significantly associated with low PA and high EE.
SUPPLEMENTARY DATA
Supplementary data are available at Journal of Radiation Research online.
Supplementary Material
ACKNOWLEDGEMENTS
We are grateful to all the members of the Kyoto Radiation Oncology Study Group who kindly responded to our survey. This work will be presented in part at the 58th Annual Meeting of the American Society for Radiation Oncology in Boston, 25–28 September 2016.
FUNDING
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI [Grant Number 15K09992].
CONFLICT OF INTEREST
The authors have declared that there are no conflicts of interest.
REFERENCES
- 1. Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav 1981;2:99–113. [Google Scholar]
- 2. Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol 2015;30:1235–41. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67. [DOI] [PubMed] [Google Scholar]
- 4. Olkinuora M, Asp S, Juntunen J, et al. Stress symptoms, burnout and suicidal thoughts of Finnish physicians. Scand J Work Environ Health 1992;18:110–2. [PubMed] [Google Scholar]
- 5. Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med 1995;18:581–99. [DOI] [PubMed] [Google Scholar]
- 6. Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer 1995;71:1263–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whippen DA, Canellos GP. Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol 1991;9:1916–20. [DOI] [PubMed] [Google Scholar]
- 8. Trufelli DC, Bensi CG, Garcia JB, et al. Burnout in cancer professionals: a systematic review and meta-analysis. Eur J Cancer Care (Engl) 2008;17:524–31. [DOI] [PubMed] [Google Scholar]
- 9. Purvanova RK, Muros JP. Gender differences in burnout: a meta-analysis. J Vocat Behav 2010;77:168–85. [Google Scholar]
- 10. Ruggieri V, Zeppegno P, Gramaglia C, et al. A survey of Italian radiation oncologists: job satisfaction and burnout. Tumori 2014;100:307–14. [DOI] [PubMed] [Google Scholar]
- 11. Jasperse M, Herst P, Dungey G. Evaluating stress, burnout and job satisfaction in New Zealand radiation oncology departments. Eur J Cancer Care (Engl) 2014;23:82–8. [DOI] [PubMed] [Google Scholar]
- 12. Blanchard P, Truchot D, Albiges-Sauvin L, et al. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer 2010;46:2708–15. [DOI] [PubMed] [Google Scholar]
- 13. Kusano AS, Thomas CR, Bonner JA, et al. Burnout in United States academic chairs of radiation oncology programs. Int J Radiat Oncol Biol Phys 2014;88:363–8. [DOI] [PubMed] [Google Scholar]
- 14. Lyckholm L. Dealing with stress, burnout, and grief in the practice of oncology. Lancet Oncol 2001;2:750–2. [DOI] [PubMed] [Google Scholar]
- 15. Kitaoka-Higashiguchi K, Nakagawa H. Job strain, coping, and burnout among Japanese nurses. Japanese J Health Hum Ecol 2003;69:66–79. [Google Scholar]
- 16. Nishimura K, Nakamura F, Takegami M, et al. Cross-sectional survey of workload and burnout among Japanese physicians working in stroke care: the nationwide survey of acute stroke care capacity for proper designation of comprehensive stroke center in Japan (J-ASPECT) study. Circ Cardiovasc Qual Outcomes 2014;7:414–22. [DOI] [PubMed] [Google Scholar]
- 17. Shimizu T, Mizoue T, Kubota S, et al. Relationship between burnout and communication skill training among Japanese hospital nurses: a pilot study. J Occup Health 2003;45:185–90. [DOI] [PubMed] [Google Scholar]
- 18. Asai M, Morita T, Akechi T, et al. Burnout and psychiatric morbidity among physicians engaged in end-of-life care for cancer patients: a cross-sectional nationwide survey in Japan. Psycho-oncology 2007;16:421–8. [DOI] [PubMed] [Google Scholar]
- 19. Fujitani K, Carroll M, Yanagisawa R, et al. Burnout and psychiatric distress in local caregivers two years after the 2011 Great East Japan Earthquake and Fukushima Nuclear Radiation Disaster. Community Ment Health J 2016;52:39–45. [DOI] [PubMed] [Google Scholar]
- 20. Saijo Y, Chiba S, Yoshioka E, et al. Job stress and burnout among urban and rural hospital physicians in Japan. Aust J Rural Health 2013;21:225–31. [DOI] [PubMed] [Google Scholar]
- 21. Higashiguchi K, Morikawa Y, Miura K, et al. The development of the Japanese version of the Maslach Burnout Inventory and the examination of the factor structure. Jpn J Hyg 1998;53:447–55. [DOI] [PubMed] [Google Scholar]
- 22. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual (3rd edn). Palo Alto, CA:Consulting Psychologists Press, 1996. [Google Scholar]
- 23. Grunfeld E, Whelan TJ, Zitzelsberger L, et al. Cancer care workers in Ontario: prevalence of burnout, job stress and job satisfaction. CMAJ 2000;163:166–9. [PMC free article] [PubMed] [Google Scholar]
- 24. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work–life balance among US physicians relative to the general US population. Arch Intern Med 2012;172:1377–85. [DOI] [PubMed] [Google Scholar]
- 25. Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191–7. [DOI] [PubMed] [Google Scholar]
- 26. Doi Y, Minowa M. Factor structure of the 12-item General Health Questionnaire in the Japanese general adult population. Psychiatry Clin Neurosci 2003;57:379–83. [DOI] [PubMed] [Google Scholar]
- 27. Fukunishi I. The assessment of cut-off point of the General Health Questionnaire (GHQ) in the Japanese version. J Clin Psychol 1990;3:228–34. [Google Scholar]
- 28. Nakagawa Y, Daibou I. Manual of the Japanese version of the General Health Questionnaire Tokyo: Nihon Bunka Kagakusha, 1985. (in Japanese). [Google Scholar]
- 29. Dyrbye LN, West CP, Shanafelt TD. Defining burnout as a dichotomous variable. J Gen Intern Med 2009;24:440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leung J, Rioseco P, Munro P. Stress, satisfaction and burnout amongst Australian and New Zealand radiation oncologists. J Med Imaging Radiat Oncol 2015;59:115–24. [DOI] [PubMed] [Google Scholar]
- 31. Aggarwal S, Kusano AS, Carter JN, et al. Stress and burnout among residency program directors in United States radiation oncology programs. Int J Radiat Oncol 2015;93:746–53. [DOI] [PubMed] [Google Scholar]
- 32. Ciammella P, De Bari B, Fiorentino A, et al. The ‘BUONGIORNO’ project: burnout syndrome among young Italian radiation oncologists. Cancer Invest 2013;31:522–8. [DOI] [PubMed] [Google Scholar]
- 33. Umene-Nakano W, Kato TA, Kikuchi S, et al. Nationwide survey of work environment, work–life balance and burnout among psychiatrists in Japan. PLoS One 2013;8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Panagopoulou E, Montgomery A, Benos A.. Burnout in internal medicine physicians: differences between residents and specialists. Eur J Intern Med 2006;17:195–200. [DOI] [PubMed] [Google Scholar]
- 35. IsHak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ 2009;1:236–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA 2011;305:2009–10. [DOI] [PubMed] [Google Scholar]
- 37. Nakane Y, Tazaki M, Miyaoka E.. WHOQOL-BREF survey of general population. Iryo to Shakai 1999;9:123–31. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.