Abstract
Objectives: The objective of the study was to investigate the association between predialysis chronic kidney disease and contracting pneumonia in Taiwan.
Methods: We employed a population-based, retrospective cohort design using the database of the Taiwan National Health Insurance (NHI) Program. There were 18807 subjects aged 20-84 years who were newly diagnosed with predialysis chronic kidney disease between 2000 to 2012 as the predialysis chronic kidney disease group and 18807 randomly selected subjects without chronic kidney disease as the non-chronic kidney disease group. The predialysis chronic kidney disease and non-chronic kidney disease groups were matched according to sex, age, comorbidities, and the year of index date. The incidence of contracting pneumonia among both groups at the end of 2013 was calculated. The multivariable Cox proportional hazards regression model was used to calculate the hazard ratio (HR) and 95% confidence interval (CI) for contracting pneumonia being associated with predialysis chronic kidney disease.
Results: The overall incidence of contracting pneumonia was 1.47-fold higher in the predialysis chronic kidney disease group than that in the non-chronic kidney disease group (24.6 vs. 16.7 per 1, 000 person-years, 95% CI 1.40, 1.55). After adjusting for co-variables, the HR of contracting pneumonia became 1.52 for subjects with predialysis chronic kidney disease (95% CI 1.43, 1.60) compared to subjects without chronic kidney disease. With even further analysis, in the absence of any comorbidity, the adjusted HR of contracting pneumonia was 1.53 for subjects with predialysis chronic kidney disease alone (95% CI 1.32, 1.76).
Conclusions: Patients with predialysis chronic kidney disease have a 1.52-fold increased risk of contracting pneumonia as compared to those with non-chronic kidney disease. Even in the absence of any comorbidity, a greater than average risk of contracting pneumonia remains present.
Keywords: Pneumonia, Predialysis chronic kidney disease, Taiwan National Health Insurance Program
1. Introduction
Pneumonia continues to be a major public health problem due to the substantial number of deaths it causes as well as the high economic cost to treat it globally. Pneumonia has been ranked as the third leading cause of death in the world.[1] In addition, pneumonia was the fourth most common cause of death in Taiwan in 2015.[2] Lin et al’s study showed that patients with pneumonia needed longer lengths of hospital stays than average to recover and higher health care expenditures, both of which have placed a significant economic burden on Taiwan. [3]
Meanwhile, chronic kidney disease was the ninth most common cause of death in Taiwan in 2015.[2] Much evidence has already shown that pneumonia is a common comorbidity among patients with chronic kidney disease.[4, 5] Thus, we made a rational hypothesis that there could be a potential link between predialysis chronic kidney disease and pneumonia in Taiwan. If the link can be made, from a view of preventive medicine, vaccination for pneumonia might be something to take into account among patients with predialysis chronic kidney disease. With the above in mind, our study employed apopulation-based cohort design using the database of the Taiwan National Health Insurance (NHI) Program to investigate the association between predialysis chronic kidney disease and pneumonia.
2. Methods
2.1. Study design and data source
For this study, a population-based, retrospective cohort design was employed using the database from the Taiwan National Health Insurance Program. Taiwan is an independent country with more than 23 million persons. The NHI Program was launched in March 1, 1995, and it now covers about 99% of the said 23 million persons living in Taiwan.[6] The details of the insurance program will not be discussed here, but they have been thoroughly written about in previous studies.[7–11] Our study was approved by the Research Ethics Committee of China Medical University and Hospital in Taiwan (CMUH-104-REC2-115).
2.2. Selection of subjects
Subjects aged 20-84 who had been newly diagnosed with predialysis chronic kidney disease (International Classification of Diseases, Ninth Revision, Clinical Modification, ICD-9 codes 581-583, 585-587, and 588.8-588.9) between 2000 to 2012 were assigned as our predialysis chronic kidney disease group. The date for subjects being diagnosed with predialysis chronic kidney disease was defined as the index date. For each subject with predialysis chronic kidney disease, one subject without chronic kidney disease was randomly selected from the same database and was assigned to the non-chronic kidney disease group. The predialysis chronic kidney disease group and the non-chronic kidney disease group were matched in terms of sex, age (every 5-year interval), comorbidities, and the year of the former’s index date.
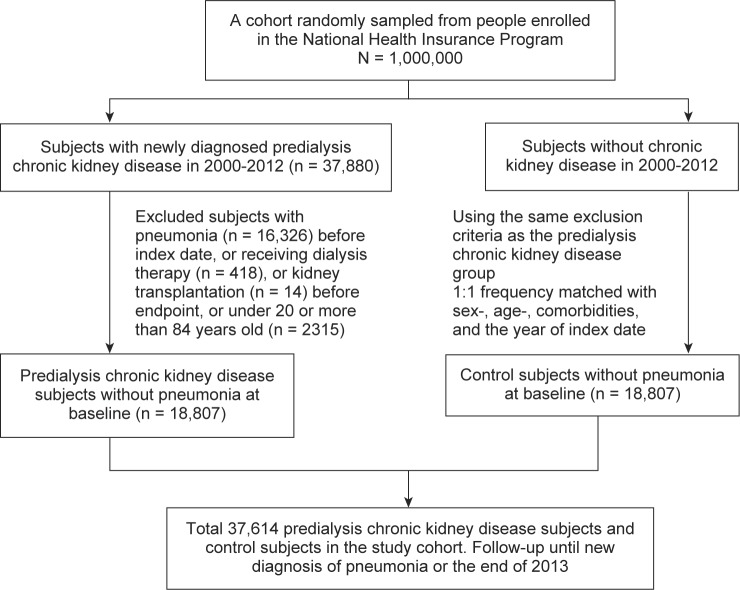
Subjects who had a history of pneumonia (ICD-9 codes 480-486) before the index date were excluded from the study. Subjects who were currently receiving dialysis therapy or had received renal transplantation before the major endpoint were excluded from the study (Fig. 1).
Fig. 1.
Flow chart for selecting the study’s subjects.
2.3. Major endpoint
The major endpoint was a new diagnosis of pneumonia during the follow-up period. Each subject was followed-up with until they were diagnosed with pneumonia, or until the end of 2013.
2.4. Comorbid conditions
The comorbid conditions potentially related to contracting pneumonia that were included were as follows: alcohol-related disease, cancer, cardiovascular disease (including coronary artery disease, heart failure, cerebrovascular disease, and peripheral atherosclerosis), chronic liver disease (including cirrhosis, hepatitis B, hepatitis C, and other chronic hepatitis), chronic obstructive pulmonary disease, hyperlipidemia, hypertension, and diabetes mellitus. All comorbidities in the study were diagnosed with ICD-9 codes, which have been well examined in previous studies.[12–21]
2.5. Statistical analysis
The differences in the sex, age, and comorbidities between the predialysis chronic kidney disease group and the non-chronic kidney disease group were compared via a Chi-square test for categorical variables and a t-test for continuous variables. The incidence of contracting pneumonia was calculated as the number of pneumonia cases identified during the follow-up period, divided by the total number of follow-up person-years for each group. In the beginning, all variables were included in a univariable model. Then, variables found to be statistically significant in the univariable model were further included in the multivariable model. The multivariable Cox proportional hazards regression model was used to calculate the hazard ratio (HR) with 95% confidence interval (CI) of contracting pneumonia associated with predialysis chronic kidney disease along with other comorbidities. All statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina, USA). Two-tailed P < 0.05 was considered statistically significant.
3. Results
3.1. Demorgraphic information and comorbidities of the study population
Table 1 shows the distributions of sex, age, and comorbidities between the predialysis chronic kidney disease and non-chronic kidney disease groups. There were 18807 subjects in the predialysis chronic kidney disease group and likewise 18807 subjects in the non-chronic kidney disease group, with similar distributions of sex and age. The mean ages (standard deviation) of the study’s subjects were 58.5 (15.0) years in the predialysis chronic kidney disease group and 58.2 (15.0) years in the non-chronic kidney disease group (t-test, P = 0.05). The comorbidities were equally distributed in the predialysis chronic kidney disease group and the non-chronic kidney disease group (Chi-square test, P > 0.05 for all).
Table 1.
Demographic information and comorbidities between predialysis chronic kidney disease group and non-chronic kidney disease group.
| Non-chronic kidney disease N=18807 |
Predialysis chronic kidney disease N=18807 |
||||
|---|---|---|---|---|---|
| Variable | n | (%) | n | (%) | P value* |
| Sex | 0.99 | ||||
| Female | 7655 | (40.7) | 7655 | (40.7) | |
| Male | 11152 | (59.3) | 11152 | (59.3) | |
| Age group (years) | 0.99 | ||||
| 20-39 | 5367 | (28.5) | 5367 | (28.5) | |
| 40-64 | 6243 | (33.2) | 6243 | (33.2) | |
| 65-84 | 7197 | (38.3) | 7197 | (38.3) | |
| Age (years), mean (standard deviation)† | 58.2 | (15.0) | 58.5 | (15.0) | 0.05 |
| Baseline comorbidities | |||||
| Alcohol-related disease | 885 | (4.71) | 885 | (4.71) | 0.99 |
| Cancer | 749 | (3.98) | 749 | (3.98) | 0.99 |
| Cardiovascular disease | 7604 | (40.4) | 7604 | (40.4) | 0.99 |
| Chronic liver disease | 4188 | (22.3) | 4188 | (22.3) | 0.99 |
| Chronic obstructive pulmonary disease | 2468 | (13.1) | 2468 | (13.1) | 0.99 |
| Hyperlipidemia | 8322 | (44.3) | 8322 | (44.3) | 0.99 |
| Hypertension | 11699 | (62.2) | 11699 | (62.2) | 0.99 |
| Diabetes mellitus | 3836 | (20.4) | 3836 | (20.4) | 0.99 |
Data are presented as the number of subjects in each group, with percentages given in parentheses, or the mean with standard deviation given in parentheses.
Chi-square test, and
t-test comparing subjects with predialysis chronic kidney disease and without chronic kidney disease.
3.2. Incidence of contracting pneumonia in the study population stratified by sex and age
Table 2 shows that the overall incidence of contracting pneumonia was 1.47-fold higher in the predialysis chronic kidney disease group than that in the non-chronic kidney disease group (24.6 vs. 16.7 per 1, 000 person-years, 95% CI 1.40, 1.55). As stratified by sex and age, the incidences of contracting pneumonia were all higher in the predialysis chronic kidney disease group than those in the non-chronic kidney disease group. The incidences of contracting pneumonia increased with age in both groups, with the highest incidence rate being in the predialysis chronic kidney disease group aged 65-84 years (45.2 per 1, 000 person-years).
Table 2.
Incidence of pneumonia stratified by sex and age between predialysis chronic kidney disease group and non-chronic kidney disease group.
| Non-chronic kidney disease |
Predialysis chronic kidney disease |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | N | Event | Person- years | Incidence† | N | Event | Person- years | Incidence† | IRR# | (95% CI) |
| All | 18807 | 2113 | 126622 | 16.7 | 18807 | 2821 | 114713 | 24.6 | 1.47 | (1.40, 1.55) |
| Sex | ||||||||||
| Female | 7655 | 748 | 54399 | 13.8 | 7655 | 1035 | 48472 | 21.4 | 1.55 | (1.43, 1.68) |
| Male | 11152 | 1365 | 72223 | 18.9 | 11152 | 1786 | 66241 | 27.0 | 1.43 | (1.34, 1.52) |
| Age group (years) | ||||||||||
| 20-39 | 5367 | 292 | 43624 | 6.69 | 5367 | 473 | 41350 | 11.4 | 1.71 | (1.53, 1.90) |
| 40-64 | 6243 | 569 | 42385 | 13.4 | 6243 | 794 | 38994 | 20.4 | 1.52 | (1.38, 1.66) |
| 65-84 | 7197 | 1252 | 40613 | 30.8 | 7197 | 1554 | 34369 | 45.2 | 1.47 | (1.36, 1.58) |
Incidence: per 1, 000 person-years.
IRR (incidence rate ratio): predialysis chronic kidney disease vs. non-chronic kidney disease (95% confidence interval)
Using the Kaplan-Meier model, we have shown that the cumulative incidence of contracting pneumonia was higher in the predialysis chronic kidney disease group than that in the nonchronic kidney disease group (23.0% vs. 16.8% at the end of follow-up; P < 0.001, Fig. 2).
Fig. 2.
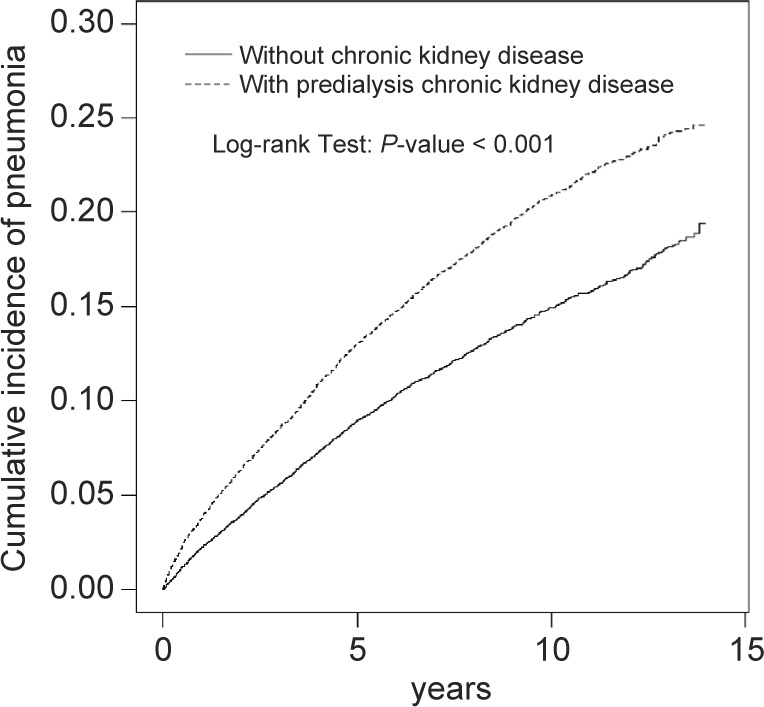
Kaplan–Meier curves showing a significant difference in cumulative incidences of pneumonia among patients with predialysis chronic kidney disease and without chronic kidney disease. (23.0% vs. 16.8% at the end of follow-up; P < 0.001)
3.3. Hazard ratio of contracting pneumonia associated with predialysis chronic kidney disease and comorbidities
Table 3 shows the hazard ratio (HR) of contracting pneumonia associated with predialysis chronic kidney disease and other comorbidities. After adjusting for co-variables, a multivariable Cox proportional hazards regression model showed that the adjusted HR of contracting pneumonia was 1.52 for subjects with predialysis chronic kidney disease (95% CI 1.43, 1.60), compared to subjects without chronic kidney disease. In addition, being male (adjusted HR 1.33, 95% CI 1.25, 1.41), having an alcohol- related disease (adjusted HR 1.35, 95% CI 1.18, 1.55), having cancer (adjusted HR 1.30, 95% CI 1.12, 1.49), having a cardiovascular disease (adjusted HR 1.24, 95% CI 1.17, 1.33), having chronic obstructive pulmonary disease (adjusted HR 1.40, 95% CI 1.31, 1.51), and having diabetes mellitus (adjusted HR 1.59, 95% CI 1.49, 1.69) were other factors associated with contracting pneumonia. Every one-year increase in age was associated with a 1.04-fold increased hazard of contracting pneumonia (95% CI 1.03, 1.04).
Table 3.
Hazard ratio (HR) and 95% confidence interval of contracting pneumonia associated with predialysis chronic kidney disease and certain comorbidities.
| Crude |
Adjusted†
|
|||
|---|---|---|---|---|
| Variable | HR | (95% CI) | HR | (95% CI) |
| Sex (male vs. female) | 1.29 | (1.22, 1.37) | 1.33 | (1.25, 1.41) |
| Age (per one year) | 1.04 | (1.04, 1.05) | 1.04 | (1.03, 1.04) |
| Predialysis chronic kidney disease | 1.46 | (1.38, 1.55) | 1.52 | (1.43, 1.60) |
| Baseline comorbidities (yes vs. no) | ||||
| Alcohol-related disease | 1.27 | (1.11, 1.45) | 1.35 | (1.18, 1.55) |
| Cancer | 1.57 | (1.36, 1.80) | 1.30 | (1.12, 1.49) |
| Cardiovascular disease | 2.15 | (2.03, 2.28) | 1.24 | (1.17, 1.33) |
| Chronic liver disease | 0.93 | (0.87, 1.00) | - | - |
| Chronic obstructive pulmonary disease | 2.12 | (1.98, 2.26) | 1.40 | (1.31, 1.51) |
| Hyperlipidemia | 0.96 | (0.91, 1.02) | - | - |
| Hypertension | 2.01 | (1.89, 2.14) | 1.03 | (0.96, 1.11) |
| Diabetes mellitus | 1.99 | (1.87, 2.11) | 1.59 | (1.49, 1.69) |
Variables found to be statistically significant in a univariable model were further examined in a multivariable model. Adjustments for sex, age, alcohol-related disease, cancer, cardiovascular disease, chronic obstructive pulmonary disease, hypertension, and diabetes mellitus.
3.4. Association of contracting pneumonia stratified by predialysis chronic kidney disease and comorbidities
As a reference of subjects in the study without predialysis chronic kidney disease and without any comorbidity, the adjusted HR of contracting pneumonia was 1.53 for subjects with predialysis chronic kidney disease alone and without any comorbidity (95% CI 1.32, 1.76). The adjusted HR markedly increased to 2.16 for those with predialysis chronic kidney disease and with any comorbidity (95% CI 1.91, 2.43) (Table 4).
Table 4.
Association of contracting pneumonia stratified by predialysis chronic kidney disease and comorbidities.
| Variable |
|
Event | Incidence† | Adjusted HR# (95% CI) |
|---|---|---|---|---|
| Predialysis chronic kidney disease | Any comorbidity* | |||
| No | No | 321 | 7.82 | (Reference) |
| No | Yes | 1792 | 20.9 | 1.45 (1.28, 1.64) |
| Yes | No | 468 | 11.9 | 1.53 (1.32, 1.76) |
| Yes | Yes | 2353 | 31.2 | 2.16 (1.91, 2.43) |
Incidence: per 1, 000 person-years
Adjusted for sex and age
Comorbidities include alcohol-related disease, cancer, cardiovascular disease, chronic obstructive pulmonary disease, hypertension, and diabetes mellitus
4. Discussion
In the study, we noted that the overall incidence of contracting pneumonia was 1.47-fold higher in the predialysis chronic kidney disease group than in the non-chronic kidney disease group, particularly among the predialysis chronic kidney disease group aged 65-84, who had the highest incidence of contracting pneumonia (45.2 per 1, 000 person-years). Of note, the incidence of contracting pneumonia in patients with predialysis chronic kidney disease appears to be much higher than that in patients with sleep apnea (24.6 vs. 20.9 per 1, 000 person-years), [22] but much lower than that in patients with pulmonary tuberculosis in Taiwan (24.6 vs. 51.6 per 1, 000 person-years).[23] From a preventive medicine view, therefore, it is suggested that vaccination for pneumonia might be worth taking into account as an option among patients with predialysis chronic kidney disease, particularly for those with predialysis chronic kidney disease who are aged 65-84 due to their having the highest observed incidence of contracting pneumonia.
After adjusting for co-variables, we noted that patients with predialysis chronic kidney disease demonstrated a 1.52-fold increased hazard of contracting pneumonia, compared with subjects without chronic kidney disease (Table 3). Upon further analysis, patients with predialysis chronic kidney disease alone still had an increased risk of contracting pneumonia (adjusted HR 1.53, Table 4). This finding indicates that patients with predialysis chronic kidney disease alone are at a substantially increased risk for contracting pneumonia even in the absence of any comorbidity. In addition, we noted that if patients were comorbid with predialysis chronic kidney disease and any of the comorbidities studied, the adjusted HR of contracting pneumonia markedly increased to 2.16. This finding indicates that there might be a synergistic effect on the risk of contracting pneumonia between predialysis chronic kidney disease and any of the comorbidities studied.
We can conclude that patients with predialysis chronic kidney disease have a 1.52-fold increased risk of contracting pneumonia as compared to those with non-chronic kidney disease. Thus, even in the absence of any comorbidity, the risk of contracting pneumonia can be said to be high among patients with predialysis chronic kidney disease.
Acknowledgments
This study was supported in part by Taiwan’s Ministry of Health and Welfare Clinical Trial Center (M0HW106-TDU-B-212-113004), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10501010037), the National Research Program for Biopharmaceuticals (NRPB) Stroke Clinical Trial Consortium (MOST 105-2325-B-039-003), Tseng-Lien Lin Foundation in Taichung in Taiwan, Taiwan Brain Disease Foundation in Taipei in Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds in Japan. These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Specific author contributions
Shih-Wei Lai planned and conducted this study. He substantially contributed to the conception of the article, initiated the first draft of the article, and critically revised the article.
Cheng-Li Lin conducted the data analysis and critically reviewed the article.
Kuan-Fu Liao planned and conducted this study. He participated in the data interpretation and also critically revised the article.
Conflicts of Interest Statement
The authors wish to disclose they have no conflicts of interest.
References
- 1. Wiemken TL, Peyrani P, Ramirez JA. Global changes in the epidemiology of community-acquired pneumonia. Semin Respir Crit Care Med. 2012; 33: 213–9. [DOI] [PubMed] [Google Scholar]
- 2. Ministry of Helath and Welfare, Taiwan. 2015 statistics of causes of death. http://www.mohw.gov.tw/ [cited in May 1, 2017, English version].
- 3. Lin CY, Ma T, Lin CC, Kao CH. The impact of global budgeting on health service utilization, health care expenditures, and quality of care among patients with pneumonia in Taiwan. Eur J Clin Microbiol Infect Dis. 2016; 35: 219–25. [DOI] [PubMed] [Google Scholar]
- 4. McDonald HI, Thomas SL, Nitsch D. Chronic kidney disease as a risk factor for acute community-acquired infections in high-income countries: a systematic review. BMJ Open. 2014; 4: 2013–004100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Viasus D, Garcia-Vidal C, Cruzado JM, Adamuz J, Verdaguer R, Manresa F, et al Epidemiology, clinical features and outcomes of pneumonia in patients with chronic kidney disease. Nephrol Dial Transplant. 2011; 26: 2899–906. [DOI] [PubMed] [Google Scholar]
- 6. National Health Insurance Research Database. Taiwan. http://nhird.nhri.org.tw/en/index.html [cited in May 1, 2017, English version].
- 7. Tsai TY, Lin CC, Peng CY, Huang WH, Su WP, Lai SW, et al The association between biliary tract inflammation and risk of digestive system cancers: A population-based cohort study. Medicine. 2016; 95: e4427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen HY, Lin CL, Lai SW, Kao CH. Association of Selective Serotonin Reuptake Inhibitor Use and Acute Angle-Closure Glaucoma. J Clin Psychiatry. 2016; 77: e692–6. [DOI] [PubMed] [Google Scholar]
- 9. Yang SP, Muo CH, Wang IK, Chang YJ, Lai SW, Lee CW, et al Risk of type 2 diabetes mellitus in female breast cancer patients treated with morphine: A retrospective population-based time-dependent cohort study. Diabetes Res Clin Pract. 2015; 110: 285–90. [DOI] [PubMed] [Google Scholar]
- 10. Kuo SC, Lai SW, Hung HC, Muo CH, Hung SC, Liu LL, et al Association between comorbidities and dementia in diabetes mellitus patients: population-based retrospective cohort study. J Diabetes Complications. 2015; 29: 1071–6. [DOI] [PubMed] [Google Scholar]
- 11. Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC. Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine. 2010; 89: 295–9. [DOI] [PubMed] [Google Scholar]
- 12. Liao KF, Huang PT, Lin CC, Lin CL, Lai SW. Fluvastatin use and risk of acute pancreatitis:a population-based case-control study in Taiwan. Biomedicine-Taiwan. 2017; 7: 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liao KF, Cheng KC, Lin CL, Lai SW. Etodolac and the risk of acute pancreatitis. Biomedicine-Taiwan. 2017; 7: 25–9 (in English). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lai SW, Lin CL, Liao KF. Digoxin use may increase the relative risk of acute pancreatitis: A population-based case-control study in Taiwan. Int J Cardiol. 2015; 181: 235–8. [DOI] [PubMed] [Google Scholar]
- 15. Shen ML, Liao KF, Tsai SM, Lin CL, Lai SW. Herpes zoster correlates with pyogenic liver abscesses in Taiwan. Biomedicine-Taiwan. 2016; 6: 24–9. (in English). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hsu F-G, Sheu M-J, Lin C-L, Hsieh Y-W, Lai S-W. Use of Zolpidem and Risk of Acute Pyelonephritis in Women: A Population-Based Case-Control Study in Taiwan. J Clin Pharmacol. 2017; 57: 376–81. [DOI] [PubMed] [Google Scholar]
- 17. Lai SW, Lai HC, Lin CL, Liao KF. Zopiclone use associated with increased risk of acute pancreatitis: a case-control study in Taiwan. Int J Clin Pract. 2015; 69: 1275–80. [DOI] [PubMed] [Google Scholar]
- 18. Wong TS, Liao KF, Lin CM, Lin CL, Chen WC, Lai SW. Chronic Pancreatitis Correlates With Increased Risk of Cerebrovascular Disease: A Retrospective Population-Based Cohort Study in Taiwan. Medicine. 2016; 95: e3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lai SW, Lin CL, Liao KF. Rheumatoid Arthritis and Risk of Pyogenic Liver Abscess in Taiwan. Int Med J. 2016; 23: 267–8. [Google Scholar]
- 20. Liao KF, Lin CL, Lai SW. Schizophrenia Correlates with Increased Risk of Hepatocellular Carcinoma in Men: A Cohort Study in Taiwan. Int Med J. 2015; 22: 273–6. [Google Scholar]
- 21. Lai SW, Lin CL, Liao KF, Lin CY. Amiodarone use and risk of acute pancreatitis: A population-based case-control study. Heart Rhythm. 2015; 12: 163–6. [DOI] [PubMed] [Google Scholar]
- 22. Su VY, Liu CJ, Wang HK, Wu LA, Chang SC, Perng DW, etal Sleep apnea and risk of pneumonia: a nationwide population-based study. Cmaj. 2014; 186: 415–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chang TM, Mou CH, Shen TC, Yang CL, Yang MH, Wu FY, et al Retrospective cohort evaluation on risk of pneumonia in patients with pulmonary tuberculosis. Medicine. 2016; 95: e4000. [DOI] [PMC free article] [PubMed] [Google Scholar]