Abstract
Rationale:
Osteopetrosis is a rare disease that predominantly occurs in descendants of inbreeding families. In the case of fractures happen in patients with osteopetrosis, the choice between operative or conservative treatment is still controversial. Open reduction and internal fixation (ORIF) is a conventional treatment for fractures, and it possesses more applicability than conservative treatment. During this surgical treatment, ensure that bone union in the right way is pivotal to success and simultaneously prevents refracture and displacement after the operation. Herein, we present a case of femoral fracture of a patient with osteopetrosis via open reduction and internal fixation. To illustrate successful factors during the treatment process, we discuss experience combined with literature review following case report.
Patient concerns:
A 67-year-old man who has diagnosed with osteopetrosis over 20 years ago suffered from pain in the left hip last for more than 1 month and he was incapable of walking recently. Before this incident, he had sustained 4 femoral fractures that treated insufficiently by open reduction surgery.
Diagnosis:
Physical, radiological, and biological examinations indicated a femoral subtrochanteric fracture that was overlapping displacement between fracture ends.
Interventions and outcomes:
Treated with surgery by open reduction with internal fixation and osteotomy, the fracture united in 12 months, and he returned to walk with full weight bearing, during which no complication occurred.
Lessons:
Open reduction and internal fixation is also suitable for the patient with osteopetrosis, and they have similar union ability to the normal. To guarantee successful treatment, specific strategies of operation and rehabilitation program are necessary.
Keywords: femoral fracture, internal fixation, osteopetrosis, rehabilitation, surgical treatment
1. Introduction
Osteopetrosis also known as “marble bone disease” or “Albers-Schonberg disease” is a heterogeneously hereditary disease. Based on clinical manifestations and genetic phenotypes, it classifies osteopetrosis in 3 forms: autosomal dominant (ADO), autosomal recessive (ARO), and X-linked (IRO). Frequently encountered in orthopedics, the ADO form manifests as diffused sclerosis of bone, or alternative band of metaphysis, or thickened skull. What is more, this condition has a “bone in bone” or “sandwich vertebrae” feature observed in the x-ray film.[1] The ADO form usually has a benign course and its onset is generally in adulthood; however, it is heterogeneous that may appear from symptomless to severe syndrome.
In cytopathology, the primary manifestation of dysfunctional osteoclasts is either impaired acidification or generation failure. The former is predominantly associated with mutant gene ClCN7 or TCIRG1, which accordingly compromise chloride channel and proton pump, subsequently resulting in insufficient acid secretion and abnormal bone reabsorption. However, the latter situation involves the absence of “receptor activator of nuclear factor-κB ligand” (RANKL) on osteoblasts. RANKL conjugates to RANK that on osteoclast precursors and generates signals to stimulate differentiation to osteoclasts.[2,3] Attributed to dysfunctional osteoclasts, the resorption of calcified cartilage and primary trabecular weakens or even disappears, inhibiting secondary lamellar bone to replace the primary structure. Thus, newborn bone inadequately withstands stress since its weak mechanical-property,[1,4] and not surprisingly, reduplicative fracture exists in the course of osteopetrosis.
Facing to these handicaps, surgeons have long worried about challenges caused by excessive bone mineralization in surgery and the ability of patient to heal. Therefore, some surgeons advocate conservative treatment rather than operative treatment, even for adults. However, a number of clinical reports have certified that osteocytes of osteopetrosis patients possess similar healing capability to the normal (this will discuss in the part of “Union of bone”). In this case, we report a case relating to a displaced femoral fracture in a patient with benign osteopetrosis, who successfully treated by surgery with open reduction and internal fixation (ORIF). ORIF is a major process for managing acute fractures and osteopetrotic fractures since the last decade. Nevertheless, treatment reports for osteopetrosis have been published, few presentations as complicated as this case have been subjected to peer review. Given this, we summarized several points for attention in the surgical procedure via ORIF in patients with osteopetrosis in the article. We obtained consent from the patient who participated in this study.
2. Case report
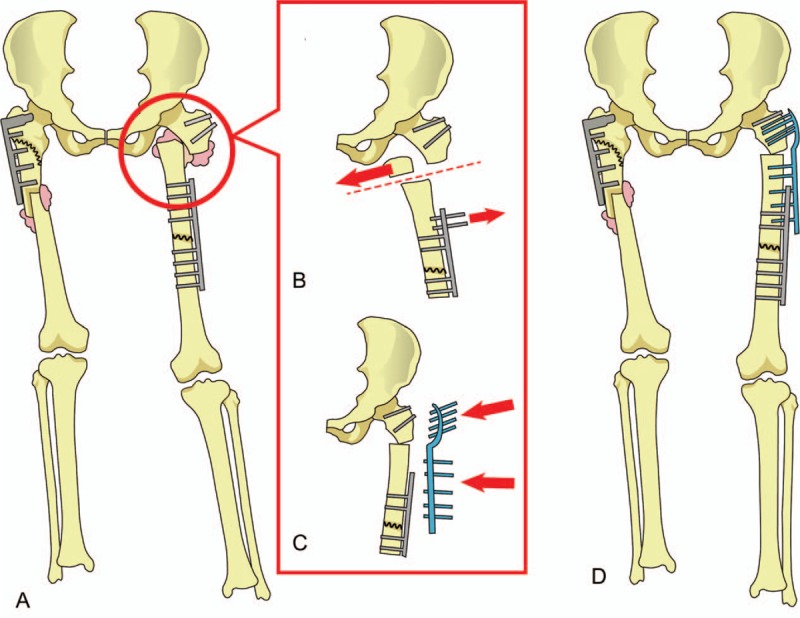
A 67-year-old man who was diagnosed with osteopetrosis more than 20 years ago was admitted to our hospital for systematic treatment on 25 August 2014. Over 1 month ago, persistent pain emerged with no obvious injury in his left hip but did not influence his walk. Thus, he not only ignored this symptom but also rejected any treatment. After suffering from aggravating pain, he was unable to ambulate and sought medical advice in the hospital. Before this incident, 4 femoral fractures occurred respectively in 1986, 1993, 2002, and 2011, which explicated in Table 1. The patient denied both consanguineous marriage on his parental side and familial genetic disease. None of his family members (3 paternal and 2 maternal uncles, 2 sisters, and his daughter) had a condition as this patient.
Table 1.
Former femoral fractures and treatments.
The physical examination revealed that tumefaction appeared in his left hip and restricted his range of motion; additionally, pressing pain existed in the upper part of the left thigh. The lever force disappeared and deformity appeared during adduction and abduction. It was no distinct tenderness in the right hip and knee, but restriction of movement was the same as the left hip within the angle ranging from 0 to 30 degrees. In addition, lower extremities had unequal length in appearance.
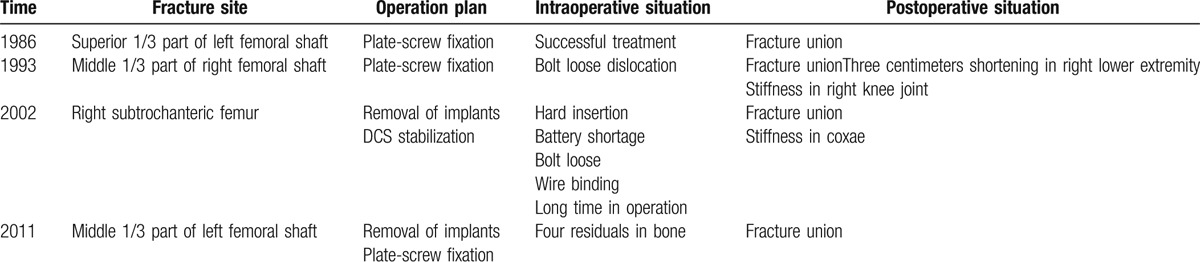
A radiological examination was carried out simultaneously through x-ray check. Radiographs proved that bones had calcified variously in pelvis, diaphysis, metaphysis, which characteristically identified osteopetrosis. Besides, a left subtrochanteric femoral fracture was observed in the film, along with a bilateral fracture formerly treated by internal fixation. In the meantime, we found that overlap extent of fracture was about 3 centimeters that surrounded some callus. (Fig. 1A–C). It was in sore need of reduction for femoral subtrochanteric fracture.
Figure 1.
The orthophoric position of x-ray plain film. (A, B) A typical indication of osteopetrosis showed in these situations: expansion and densification in ribs, representative concentric rings in the pelvis, and constriction of medullary cavity in the long bone. (C) Five fractures in femur (Arrows). Displaced fracture before the operation. (D) Six months after the operation. (E, F) Twelve months after operation and bone union.
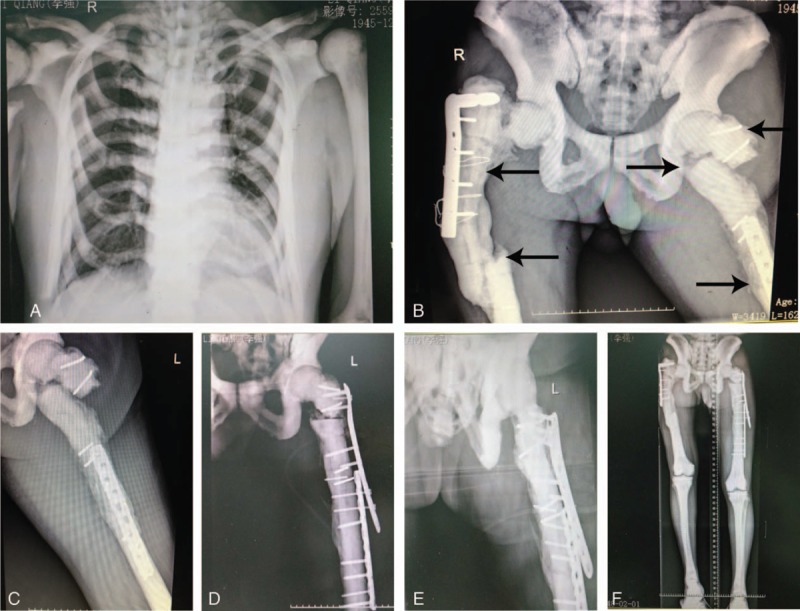
Biochemical examination parameters were illustrated in Table 2, in which could find out abnormity of hepatic and hematopoietic function. Osteopetrosis could be further confirmed by hematological indices about liver, hemocytes, and bone calcium metabolism. Excessively high alkaline phosphatase (ALP) implies that osteal diseases have been progressing. However, low red blood cell count (RBC) and red blood cell distribution width (RDW), as well as decreased hemoglobin (Hb), mainly relate to anemia that probably is an accompanying sign with osteopetrosis. Besides, hepatosplenomegaly sometimes seen in the disease could arouse increase in alanine aminotransferase (ALT), aspartic acid transaminase (AST), and γ-glutamyltransferase ggt (γ-GGT). For comparison easily, we list associated data in Table 2.
Table 2.
Abnormal parameters of biological examination.
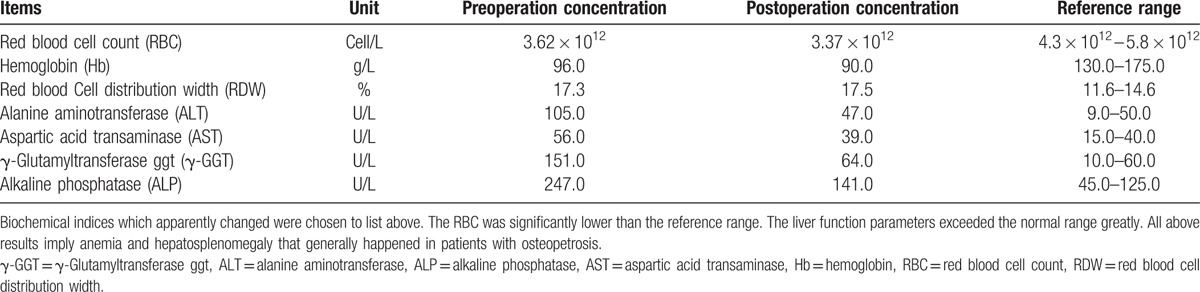
On 28 August 2014, ORIF (with LISS plate-screw fixation) was conducted for this patient. Epidural anesthesia was chosen for the subject during surgery. As expected, it was a great quantity of callus surrounding the fracture and seemed to be tough to resume their position ascribed to soft tissue contracture and malunion. As a result, we took amputation by 3 centimeters in the distal part of fracture ends as planned, which made fragments return to appropriate position smoothly and equilibrated length between lower extremities. As to fixing the fracture, LISS plate partly covered on the previous plate after removing 2 screws from the former fixture (Fig. 2). In spite of one drill bit unavoidably broke in the process of digging cannelure, the operation completed ultimately. After this surgery, cephalosporin was appropriately used to prevent infection. Since the date he was discharged from the hospital, a long-term follow-up had been implemented with return visit every 2 weeks and 1, 3, 6, and 12 months. During a 12-month nursing, the patient is capable of walking and bearing weight without pain. Moreover, radiographs displayed as below also reflected recovery stage of the fracture (Fig. 1D–F). Unfortunately, we eventually lost contact with the patient when an inspection was carried on the 13th month.
Figure 2.
The surgical solution for the patient. (A) Before surgery, callus encompassing broken bone had formed (pink cloud form). (B) Malunion part in subtrochanteric femur was removed, and 2 former screws in the upper part of homolateral plate were taken away as well. (C) The rest fracture ends were fixed at a suitable angle and reinforced by locking plate with screws. (D) Condition after open reduction and internal fixation.
3. Discussion
In this case, the phenotype of osteopetrosis probably belongs to ADO form, which has characteristics as distinctly sclerous cortex and reduplicative fractures. In most cases, fractures appear mostly in the diaphysis of lower extremities, especially in proximal femur,[5–8] for example, Bénichou et al[6] had reported in 42 osteopetrotic patients. Intriguingly, some patients are unaware of cataclasis. Here, the patient experienced 5 fractures, in which only 2 were correlated with accidents and the rest were stress fractures.
4. Union of bone in benign osteopetrosis
After ORIF for every fracture in the patient, injured site all cicatrized, despite 1 dislocation took place in 1993. Early in the 1980s, De Palma et al[7] proposed that the early healing process of bone tissue in benign osteopetrosis is no significant difference from the normal, but it lacks a remodeling phase because of afunctional osteoclasts. In the process of fracture union, every step runs well except bone reconstruction when osteoclasts are required to eliminate woven bone for consolidation in the creating area. Furthermore, some studies indicate that defective osteoclasts still produce metabolites to promote the activity of osteoblasts whereafter accelerates bone formation. This case demonstrates that the time of fracture healing is about 12 months in benign osteopetrosis, by observing whether fracture line goes indistinctly via radiograph.
5. Treatment of fracture in osteopetrosis
5.1. Choice for surgical approach
As shown by antecedent reports, conservative treatment is generally utilized for children or nondisplaced fractures chiefly applied plaster immobilization. But nowadays, it is limited to few patients with anesthetic contraindication[9] due to its adverse effects as long-term decubitus, secondary infection, delayed union, deformity and high mortality rate. Patrick and Kathleen[10] reported a nonsurgical management of femoral neck fracture (a 56-year-old man suffered osteopetrosis) with a hip spica cast and it progressed to coxa vara in the end. Recently, surgical treatment is the rule for trochanteric fracture in adults, yet there is a consensus that geriatrics would have a poor prognosis. Just the opposite, a retrospective study[11] suggested ORIF for geriatric open fracture appears to be at low risk of complications. Perhaps it is a certain extent of exaggeration, although some research affirmed ORIF potentially causes a high rate of reoperation, malunion, nonunion, or infection.[12,13] By far, we choose surgical treatment for patients as long as they have stable vital signs according to successful cases. In this case, the femoral fracture dislocated and callus formulated; hence, ORIF was urgently in need although in osteopetrosis.
During surgery, we performed transverse osteotomy to set abutting ends of fracture at a proper angle. Regarding osteotomy, James et al.[14] had clarified its effect on pain relief, and it needs 6 months in the average time to union. In our experience, transverse osteotomy, which has been accomplished in normal patients, demands for fewer techniques and operative time. Thus, multiple risks would be reduced.
On the other side, an appropriate fixture is another guarantee for treatment success. Though some instances demonstrated the intramedullary nail fixation is practicable,[4,9] bicortical nail provides dependable stability in femoral fracture.[15] Screw-plate fixation is a priority selection due to avoiding borehole in non-medullated bone, but some limitation still disturbs surgeons, such as refracture, accumulative stress to newborn site.[4] Even a later retrospective study[16] illuminated that fixation with a cable leads to an earlier union than that with plate and screw in the osteotomy. In this case, we utilized a locked plate system (LISS) to enhance stability in the osteopetrotic patient.
5.2. Preparation before operation
Surgery for osteopetrotic fracture is a challenge for surgeons, wherein they must have a thorough a surgical plan. Primarily we searched databases of Medline, Embase, and Cochrane for treatment strategies, notwithstanding we had routine procedures for femoral subtrochanteric fracture of the normal. Indispensability we took an adequate assessment to difficulties (mission time, unexpected incident, complications, and so on), and gave attention to examination results. It is worth monitoring serum biochemical indices, including blood cell counts, lactic dehydrogenase, acid phosphatase, creatine kinase, with which reflect real-time pathological state of osteopetrosis.[18–20] Because of limitation in our hospital, we just obtained blood routine and liver function record. Second, implants and placement in vivo have to coordinate with reality, for example, the location of former fixations, uniformity of bilateral limbs and effect on redintegration. Third, sufficient drills and batteries are necessary. In the case above, the fracture had some characteristics as follows: (i) subtrochanteric fracture was procrastinated on therapy and overlapped; (ii) ipsilateral screw fixation obstructed subsequent implants; (iii) the contralateral limb was shorter than the affected one. In conclusion, we conducted ORIF with LISS, and lay implant on the initial fixation rather than removed it, which avoided the risk of refracture.
5.3. Attention for the intraoperative period
Anomalous rigidity of bone enhances more arduousness in drilling holes. However, a high-speed drill works, overheat probably causes bone necrosis.[4,17] The validity of several prevention measures had been confirmed in this surgery: Replace frequently with high-speed aiguille; apply tapping drilling screw; ensure insertion perpendicular to bone surface; alternate speed in perforating; cool down with cold saline; do not utilize hammer to decrease risk of iatrogenic fracture.[17,21,22] It is also important to note that autologous bone is not available for autograft since osteoclasts of patient with osteopetrosis are dysfunctional. Furthermore, some scholars[4,17] had suggested that use a metal drill to perform a canal, and then carry on by 3.2 mm drill for reducing osteonecrosis, infection, and looseness of screws.
5.4. Postoperative management
Multiple essays reported complications marked an increase in osteopetrotic patients after ORIF, such as fixation loosening, nonunion or malunion, refracture, infection. To prevent these problems, we propose management schemes as below. Close follow-up visit: Excluding time interval of 1 week, the patient should accept a routine examination every 6 months until death to discover complications in time. Progressive rehabilitation: During extend treatment, antibiotics are commonly adopted to protect body away from microbial infection.[5,19,20] Defer full-weight bearing walk for reducing the risk of delayed union. Retain internal fixation: This is extremely suitable for multiple fractures in the gerontal patient.
5.5. Limitations
In this report, several deficiencies exist and further research is necessary. To diagnose specific form of osteopetrosis and to identify effective genes, we should perform a gene screening with new generation sequence in subsequent cases. The time of follow-up is not long enough to estimate whether ORIF is the best treatment for the patient with benign osteopetrosis. Finally, more subjects should be recruited to supply adequate data that should be analyzed systematically. Only in this way, we can expand our understanding of disease mechanism.
6. Conclusion
ORIF is appropriate for fractures in patients with osteopetrosis, especially for severely displaced fractures, yet conservative treatment is suitable for nondisplaced fractures. Although various difficulties emerged in the therapeutic process, we still handled the surgery with ORIF and controlled treatment risks with good treatment programs. In future, we expect to apply this operation method for conventional management in osteopetrotic fractures, synchronously combining with gene diagnose or gene therapy.
Footnotes
Abbreviations: γ-GGT = γ-glutamyltransferase ggt, ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartic acid transaminase, DCS = dynamic hip screw, Hb = hemoglobin, LISS = less invasive stabilization system, ORIF = open reduction and internal fixation, RBC = red blood cell count, RDW = red blood cell distribution width.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Andrea DF, Alfredo C, Anna T. Genetics, pathogenesis and complications of osteopetrosis. Bone 2008;42:19–29. [DOI] [PubMed] [Google Scholar]
- [2].Jens B, Kim H, Morten FN, et al. Autosomal dominant osteopetrosis revisited: lessons from recent studies. Eur J Endocrinol 2013;169:R39–57. [DOI] [PubMed] [Google Scholar]
- [3].Tolar J, Teitelbaum SL, Orchard PJ. Mechanisms of disease: osteopetrosis. N Engl J Med 2004;351:2839–49. [DOI] [PubMed] [Google Scholar]
- [4].Joshua L, Nathaniel M, Paul DC. Orthopaedic management of the patient with osteopetrosis. J Am Acad Orthop Surg 2007;15:654–62. [DOI] [PubMed] [Google Scholar]
- [5].Miguel AF, Carlos MO, Rodrigo FP. Recommendations for fracture management in patients with osteopetrosis: case report. Arch Orthop Trauma Surg 2015;135:351–6. [DOI] [PubMed] [Google Scholar]
- [6].Bénichou OD, Laredo JD, de Vernejoul MC. Type II autosomal dominant osteopetrosis (Albers-Schonberg disease): clinical and radiological manifestations in 42 patients. Bone 2000;26:87–93. [DOI] [PubMed] [Google Scholar]
- [7].De Palma L, Tulli A, Maccauro G, et al. Fracture callus in osteopetrosis. Clin Orthop Rel Res 1994;308:85–9. [PubMed] [Google Scholar]
- [8].Mariana A, Maria CAC, Aline BM, et al. Bone mineral density and microarchitecture in patients with autosomal dominant osteopetrosis: a report of two cases. J Bone Miner Res 2016;31:657–62. [DOI] [PubMed] [Google Scholar]
- [9].Adam P. Treatment of recent trochanteric fracture in adults. Orthop Traumatol Surg Res 2014;100:S75–83. [DOI] [PubMed] [Google Scholar]
- [10].Patrick B, Kathleen AM. Treatment of subtrochanteric and ipsilateral femoral neck fractures in an adult with osteopetrosis. Clin Orthop Rel Res 2008;466:2002–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Adam MK, Raymond AP, Robert VO, et al. Safety of immediate open reduction and internal fixation of geriatric open fractures of the distal radius. Injury 2014;45:534–9. [DOI] [PubMed] [Google Scholar]
- [12].Timothy L, David W, Patrick, et al. Rate of and risk factors for reoperations after open reduction and internal fixation of midshaft clavicle fractures. J Bone Joint Surg 2014;96:1119–25. [DOI] [PubMed] [Google Scholar]
- [13].Stein JJ, Teun T, Francis JH, et al. Outcome after fixation of metastatic proximal femoral fractures: a systematic review of 40 studies. J Surg Oncol 2016;114:507–19. [DOI] [PubMed] [Google Scholar]
- [14].James IC, Julie MC, Arash YK, et al. Lateral opening-wedge distal femoral osteotomy: pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res 2015;473:2009–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Clemens G, Sven M, Tobias D, et al. Bicortical screw fixation provides superior biomechanical stability but devastating failure modes in periprosthetic femur fracture care using locking plates. Int Orthop 2015;39:1749–55. [DOI] [PubMed] [Google Scholar]
- [16].Mehmet FC, Serhan Ü, Alper Ö, et al. Femoral shortening osteotomy in total hip arthroplasty for severe dysplasia: a comparison of two fixation techniques. Int Orthop 2016;40:2271–6. [DOI] [PubMed] [Google Scholar]
- [17].Sen RK, Gopinathan NR, Kumar R, et al. Simple reproducible technique in treatment for osteopetrotic fractures. Musculoskelet Surg 2013;97:117–21. [DOI] [PubMed] [Google Scholar]
- [18].Ihde LL, Forrester DM, Gottsegen CJ, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics 2011;31:1865–82. [DOI] [PubMed] [Google Scholar]
- [19].Michael PW, Deborah W, Karen LC, et al. Bisphosphonate-induced osteopetrosis. N Engl J Med 2003;349:457–63. [DOI] [PubMed] [Google Scholar]
- [20].Nilika W, Kay WC, Lu ZX, et al. A girl with bone sclerosis and fracture. Clin Chem 2016;62:684–7. [DOI] [PubMed] [Google Scholar]
- [21].Kumbaraci M, Karapinar L, Incesu M, et al. Treatment of bilateral simultaneous subtrochanteric femur fractures with proximal femoral nail antirotation (PFNA) in a patient with osteopetrosis: case report and review of the literature. J Orthop Sci 2013;18:486–9. [DOI] [PubMed] [Google Scholar]
- [22].Ahmet A, Yakup BB, Emin US. Surgical treatment of osteopetrosis-related femoral fractures: two case reports and literature review. Case Rep Orthop 2014;2014:891–963. [DOI] [PMC free article] [PubMed] [Google Scholar]


