Abstract
Background:
The aim of management of Achilles tendon rupture is to reduce tendon lengthening and maximize function while reducing the rerupture rate and minimizing other complications.
Purpose:
To determine changes in Achilles tendon resting angle (ATRA), heel-rise height, patient-reported outcomes, return to play, and occurrence of complications after minimally invasive repair of Achilles tendon ruptures using nonabsorbable sutures.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Between March 2013 and August 2015, a total of 70 patients (58 males, 12 females) with a mean age of 42 ± 8 years were included and evaluated at 6 weeks and 3, 6, 9, and 12 months after repair of an Achilles tendon rupture. Surgical repair was performed using either 4-strand or 6-strand nonabsorbable sutures. After surgery, patients were mobilized, fully weightbearing using a functional brace. Early active movement was permitted starting at 2 weeks.
Results:
There were no significant differences in the ATRA, Achilles Tendon Total Rupture Score (ATRS), and Heel-Rise Height Index (HRHI) between the 4- and 6-strand repairs. The mean (SD) relative ATRA was –13.1° (6.6°) (dorsiflexion) following injury; this was reduced to 7.6° (4.8°) (plantar flexion) directly after surgery. During initial rehabilitation at 6 weeks, the relative ATRA was 0.6° (7.4°) (neutral) and –7.0° (5.3°) (dorsiflexion) at 3 months, after which ATRA improved significantly with time to 12 months (P = .005). At 12 months, the median ATRS was 93 (range, 35-100), and the mean (SD) HRHI and Heel-Rise Repetition Index were 81% (0.22%) and 82.9% (0.17%), respectively. The relative ATRA at 3 and 12 months correlated with HRHI (r = 0.617, P < .001 and r = 0.535, P < .001, respectively).
Conclusion:
Increasing the number of suture strands from 4 to 6 does not alter the ATRA or HRHI after minimally invasive Achilles tendon repair. The use of a nonabsorbable suture during minimally invasive repair when used together with accelerated rehabilitation did not prevent the development of an increased relative ATRA. The ATRA at 3 months after surgery correlated with heel-rise height at 12 months.
Keywords: Achilles tendon, ankle, lengthening, outcome
The aim of modern management of Achilles tendon rupture is to reduce tendon lengthening and maximize function while reducing the rerupture rate and minimizing other complications.16,33 A rupture of the Achilles tendon has a prolonged recovery, leaving a 10% to 30% reduction in functional calf strength19,32,33,38,42 and endurance2 despite increased muscle activity.20,40 The injury produces long-term limitations,19,20,22,29 and many patients fail to return to sports activities at the same level of performance as that before injury.43
Minimally invasive repair of the Achilles tendon allows the restoration of tendon length and optimizes early tendon tension without an increased risk of wound breakdown.13 Repairs have adequate stability to permit immediate weightbearing with a protective brace and early movement.3,12 The use of a modified Bunnell suture proximally and a modified Kessler suture distally is an established technique,4 producing good functional outcomes when combined with accelerated rehabilitation.1,6,17,26–28
Recent research has focused on how the biomechanical properties of the healing tendon relate to functional performance after treatment, using different treatment methods with the aim of reducing tendon elongation and optimizing stiffness.36–38 In cadaveric studies, Costa et al10 determined that 1 cm of tenotomized tendon-end separation corresponded to a 12° increase in ankle dorsiflexion, and it is reasonable to compare this to the lengthening of the Achilles tendon. With nonoperative management consisting of cast immobilization and early weightbearing, the resting flexion angle has been shown to correlate with muscle strength (r = –0.3).15 Minimally invasive repair, using an absorbable suture, and accelerated rehabilitation have been shown to lead to 5° increased dorsiflexion at rest, indicating less tension and/or increased elongation of the muscle-tendon unit.
The Achilles tendon resting angle (ATRA) is a reliable measurement determined by the angle between the long axis of the fibula and the line from the tip of the fibula to the center of the head of the fifth metatarsal.5,7,18 Carmont et al5 found that, at 12 months following repair, the absolute ATRA correlated with heel-rise height, with a greater ATRA leading to a lower heel-rise height relative to the noninjured side. It is possible that the degradation of the suture material may have allowed tendon elongation. Whether use of a nonabsorbable suture would lead to a more symmetrical ATRA has yet to be determined.
The use of nonabsorbable suture material during Achilles tendon repair is common.21,33 Although the suture does not degrade, biomechanical models have shown that failure at the tendon-suture interface can lead to elongation by “suture cut out or pull through.”11,14,24,34 An increased number of suture strands has been shown to increase the strength of repair in an Achilles tendon repair model.31
A prospective cohort study was performed to determine the functional outcomes of patients after Achilles tendon minimally invasive repair using a nonabsorbable suture; assessments were based on ATRA, heel-rise height, patient-reported functional outcome, return to sports activity, and occurrence of complications. The effect on ATRA and outcome was compared between 4-strand and 6-strand suture repairs. An ATRA of ≥–12° (ie, 12° of dorsiflexion relative to the noninjured side), was chosen as the threshold for comparison of predictability of repair.
Methods
Between March 2013 and August 2015, a total of 70 patients (58 males), with a mean (SD) age of 42 (8) years and all with midportion ruptures of the Achilles tendon, were evaluated. All patients demonstrated the triad of a palpable gap, the absence of plantar flexion with the calf-squeeze test, and an increased relative ATRA7 confirming the diagnosis of Achilles tendon rupture.25,39 All patients consented to be included in the study, and the National Research Ethics Service confirmed that formal ethical review was not required. Patients were included if they received surgery within 14 days from the injury (Table 1). Five patients were excluded from comparative analysis (Table 1). The incidence of rupture-related sural nerve injury was determined by comparing digital tactile sensation of the injured and noninjured sides.
TABLE 1.
Patients Evaluated for Inclusion and Exclusion From the Study
| Evaluated | Acute midsubstance ruptures of the Achilles tendon having operative repair within 14 days of injury (N = 70) |
|---|---|
| Exclusion | Acute-on-chronic and chronic ruptures, defined as longer than 14 and 28 days following injury, respectively Reruptures (2.9%, n = 2) Failed surgery (1.5%, n = 1) Prolapsed intervertebral disc causing calf weakness (1.5%, n = 1) Unavailability for follow-up (1.5%, n = 1) |
| Relative exclusion | Patients with deep vein thrombosis (9%, n = 6) were excluded from calf circumference analysis 1 patient was excluded from calf circumference, heel-rise height, and endurance analysis at 12 months due to pregnancy (1.5%, n = 1) Previous contralateral rupture (1.5%, n = 1) |
This study was originally planned as a prospective outcome evaluation following a 4-strand suture technique using nonabsorbable sutures. At the 3-month evaluation, 5 of 12 patients were noted to have sustained an increase in relative ATRA of ≥–12° after mobilizing following brace discontinuation. By this time point, 19 patients had received 4-strand repairs. Due to the concern that a large number of patients had a large increment in ATRA, a clinical decision was made to increase the number of suture strands and thickness of the repair material. This presented the opportunity to develop the case series into a cohort comparison study, with group 1 patients having received a 4-strand repair and group 2 patients receiving a 6-strand repair.
Surgical Technique
Patients underwent Achilles tendon rupture repair using a minimally invasive technique5 modified from a previous percutaneous technique.4 A 2-cm midline longitudinal incision just proximal to the rupture site allowed visualization of the tendon ends’ apposition following repair. A second 2-cm longitudinal midlateral incision at 8 to 10 cm from the insertion was made to visualize and protect the sural nerve (Figure 1A). Repairs were performed using a No. 2 nonabsorbable polytetrafluoroethylene-coated polyester suture (FiberWire) using a Bunnell configuration proximally and a modified Kessler suture distally, using either 4 strands (group 1) or 6 strands (group 2) instituted at different time periods (Figure 1B). These intratendinous sutures were tied with the ankle and foot held in maximal plantar flexion or reduced ATRA to the nonaffected side (Figure 1C). Knots were buried within the tendon substance or placed anteriorly to the tendon, and the fascia cruris was closed using absorbable detensioning sutures.
Figure 1.
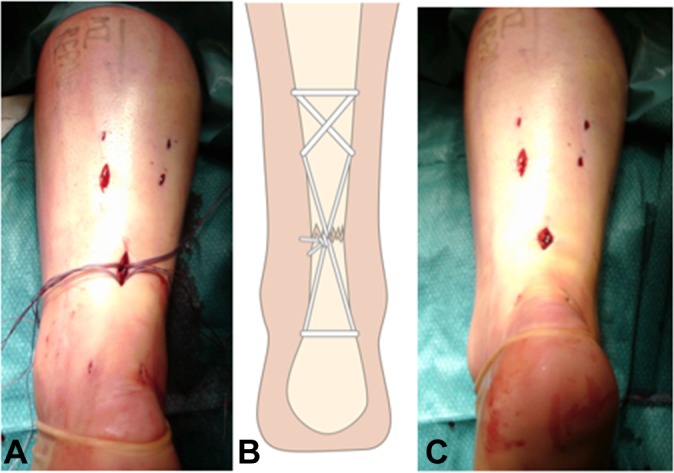
Minimally invasive Achilles tendon rupture repair. (A) Two longitudinal incisions are made: one on the midline just proximal to the palpable tendon defect, and the second at 10 cm from the insertion. These enable visual inspection of the tendon ends and the sural nerve. The nerve can be visualized and mobilized to help prevent iatrogenic injury. (B) Through skin and fascia cruris stab incisions, a needle is used to form modified Bunnell and modified Kessler sutures. (C) With the ankle held in plantar flexion, the sutures are tied off, to ensure end-to-end apposition of the tendon end. The knots are buried deep into the substance of the repair and the overlying fascia cruris closed.
Preoperative flucloxacillin 1 g and 2 weeks of low-molecular-weight heparin (Tinzaparin 4500 IU once daily; Leo Pharma) were administered. After surgery, patients underwent accelerated rehabilitation. Once the local anesthetic wore off and protective pain sensation was restored, patients were encouraged to bear weight on their metatarsal heads as tolerated by pain. The patients used axillary crutches and a protective synthetic equinus split cast for 2 weeks. After this period, the split cast was removed, and patients commenced early active-movement exercises consisting of plantar flexion, inversion, and eversion contractions for 10 seconds performed for 10 repetitions, 3 times per day. Dorsiflexion was not permitted until 6 weeks. Weightbearing continued using the anterior protective shell alone, secured in place using elasticated Velcro straps. Formal physical therapy was commenced at the 6-week time point, consisting of gait retraining and strengthening with double-heel rises progressing to single-heel rises. Stretching and plyometric exercises were avoided until the 3-month time point. Running was permitted earliest at 3 months but was dependent on the individual patient’s recovery. No formal restrictions were given with regard to return to play; however, most patients held off returning to play until they felt comfortable to do so.
Follow-up Evaluation
Patients were reviewed at 6 weeks and at 3, 6, 9, and 12 months after surgery. Symptoms and physical activity were evaluated using the Achilles Tendon Total Rupture Score (ATRS)8,30 and the Tegner activity score.41 The preinjury level of physical activity/patient perception of performance (PPP) was determined at the 3-month time point. At each follow-up, the patients were asked, “Do you think you have reached the same level of physical activity and performance as before your injury?” They were asked to categorize their response as not yet attained, the same, or greater/improved.
Patients were examined for palpable tendon gaps and tendon continuity using the calf-squeeze test. The ATRA7 was measured after rupture, after surgery, at 6 weeks, and at all subsequent evaluations (Figure 2). A maximal single-leg Limb Symmetry Index (LSI) for heel-rise height37 and calf circumference was compared with the nonaffected side at 3, 6, 9, and 12 months. The calf circumference was measured using a tape measure at 15 cm below the medial knee joint line.7 Heel-rise repetition was assessed by counting the number of single-leg heel-rises performed by the patient to exhaustion at the 12-month point. Fingertip contact with the wall was permitted for balance. LSIs for the Heel-Rise Height Index (HRHI) and the Heel-Rise Repetition Index (HRRI) were determined as follows: The HRHI was calculated as the maximal height of a single heel-rise on the injured side/the maximal height of a single heel-rise on the uninjured side ×100. The HRRI was calculated as the number of repetitions performed on the repaired side/number of repetitions on the uninjured side ×100.
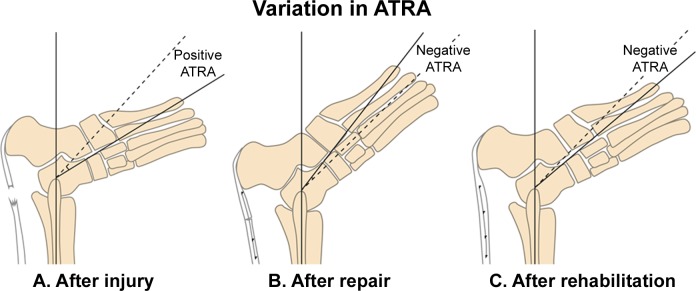
Figure 2.
The relative Achilles tendon resting angle (ATRA) following rupture, after operative repair, and after rehabilitation. The ATRA is the angle between the long axis of the fibula and the line from the tip of the fibula to the center of the head of the fifth metatarsal. (A) Following rupture, the ankle adopts a relatively dorsiflexed position5,7; the ATRA of the injured side (solid line) and is compared with the ATRA of the noninjured side (dashed line). This increment in angle would lead to the Achilles healing with elongation and the patient to have weak active plantar flexion, and so it is termed a negative ATRA. (B) Following repair, the ankle is relatively plantar flexed compared to the noninjured side. The ATRA is described/defined as positive, as the Achilles is relatively tight. (C) Following brace removal, increased mobilization, and rehabilitation, the injured tendon elongates, so the ATRA increases and is described/defined as negative.
The primary outcome of the study was the change in ATRA over time. Secondary outcomes were the ATRS, Tegner, PPP, calf circumference, HRHI, and HRRI.5,30,37,41
Statistical Analysis
All data were analyzed using IBM SPSS Statistics version 24 (IBM Corp). Descriptive statistics for ATRS were reported using median (range) and mean (SD). A sample-size calculation performed using a population mean with relative ATRA of 0° was compared to the sample mean of –6.5° (6.5°) at 12 months5 using a beta of 0.8. A sample size of 8 patients per group would be required to compare the difference in ATRA at 12 months between the 4- and 6-strand repairs. Patients who sustained complications were pragmatically included and excluded from analysis (Table 1). The level of significance was set at P < .05. A 2-way mixed analysis of variance for repeated measures using Bonferroni correction for pairwise analysis was used to evaluate changes over time between groups. The Mauchly test for sphericity was significant for ATRA and ATRS, and significance levels are reported for Greenhouse-Geisser. Pearson correlation was used for analyzing the correlations between the relative ATRA and HRHI and between relative ATRA and calf circumference.
The proportion of patients with an ATRA of ≥–12° was also determined at each time point. Chi-square and Fisher exact tests were performed for descriptive analysis using cross-tabulations for these binomial outcome measures.
Results
Seventy patients with a midportion rupture of the Achilles tendon were evaluated after injury and received surgical repair (Table 1). The activities during which ruptures were sustained included football (20%, n = 13), badminton (10.8%, n = 7), children’s sports (9.2%, n = 6), stepping in a hole or falling on an uneven surface (7.7%, n = 5), cricket (6.2%, n = 4), netball (6.2%, n = 4), squash (6.2%, n = 4), pushing a vehicle (6.2%, n = 4), slipping on the stairs (6.2%, n = 4), and other activities (n = 8); notably, 4 patients were injured participating in cross-fit (3.1%, n = 2) activities and rural activities (3.1%, n = 2).
Two patients sustained reruptures; both had been repaired using 6-strand repairs. One slipped on a wet surface and another stumbled while intoxicated at 4 and 5 weeks following repair, respectively. Neither patient was wearing a protective brace as advised. Additional surgical complications were cellulitis, suture sinus, second-site rupture managed nonoperatively, and failed surgery with inability to appose tendon ends (all 1.5%, n = 1) (Table 1). Sixty-five patients formed 2 comparative groups (Table 2). Other than the number of patients, there were no significant differences in the demographic characteristics between the 2 groups.
TABLE 2.
Patient Demographicsa
| Overall | Group 1 (4-Strand) | Group 2 (6-Strand) | |
|---|---|---|---|
| No. of patients | 65 | 19 | 46 |
| Age (range), y | 45 (28-77) | 44 (29-64) | 47.6 (28-77) |
| Side, left:right | 31:34 | 10:9 | 21:25 |
| Gender, male:female | 53:12 | 15:4 | 38:8 |
| Tegner preinjury median (range) | 7 (2-9) | 7 (3-8) | 7 (2-9) |
| Time elapsed from injury to surgery (range), d | 6 (1-14) | 4 (2-13) | 6 (1-14) |
aThere were no significant differences in demographic characteristics between the 2 groups.
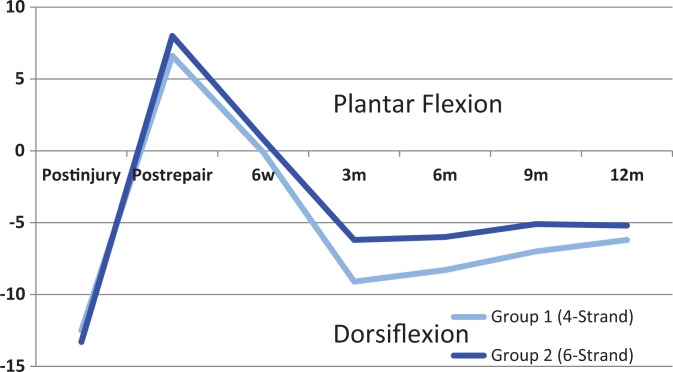
The changes in the relative ATRA are shown in Table 3 and Figure 3. There was no difference in ATRA between the groups (P = .469) (Table 3). The relative ATRA increased significantly until the 3-month time point, after which the angle increased significantly at 12 months (P = .005).
TABLE 3.
Comparison of the Relative Achilles Tendon Resting Angle (ATRA) With Time Between Group 1 (4-Strand Repair) and Group 2 (6-Strand Repair)a
| Relative ATRA | Postinjury | Postrepair | 6 Weeks | 3 Months | 6 Months | 9 Months | 12 Months |
|---|---|---|---|---|---|---|---|
| Group 1 | –12.5 (6.7) | 6.6 (4.3) | –0.1 (7.0) | –9.1 (6.0) | –8.3 (5.1) | –7 (5.9) | –6.2 (4.0) |
| Group 2 | –13.3 (6.8) | 8.0 (5.0) | 0.8 (7.7) | –6.2 (4.9) | –6.0 (4.3) | –5.1 (4.4) | –4.8 (3.9) |
| Overall | –13.1 (6.7) | 7.6 (4.8) | 0.6 (7.4) | –7.0 (5.3) | –6.6 (4.6) | –5.6 (4.8) | –5.2 (3.9) |
aResults are reported in degrees as mean (SD). A negative ATRA indicates relative ankle dorsiflexion compared with the noninjured side. There was no significant difference between groups (P = .469).
Figure 3.
The changes of the Achilles tendon resting angle (ATRA) with time after injury, after operative repair, and at 6 weeks, 3 months, 6 months, 9 months, and 12 months following repair. A negative ATRA is relative ankle dorsiflexion compared with the noninjured side.
The proportion of patients receiving a 4-strand repair with an ATRA ≥–12° was almost twice that of those having a 6-strand repair at the 3-month time point; this had fallen to 1.5 times by the 12-month time point, but there was no significant difference between groups (Table 4).
TABLE 4.
Patients in Group 1 (4-Strand Repair) and Group 2 (6-Strand Repair) With a Relative ATRA of ≥ –12°a
| 6 Weeks | 3 Months | 6 Months | 9 Months | 12 Months | |
|---|---|---|---|---|---|
| Overall | 6.2 (4/65) | 20.3 (13/64) | 10.8 (7/65) | 13.8 (9/65) | 8.3 (5/60) |
| Group 1 (4-strand) | 5.2 (1/19) | 31.6 (6/19) | 21.1 (4/19) | 21.1 (4/19) | 10.5 (2/19) |
| Group 2 (6-strand) | 6.5 (3/46) | 15.6 (7/45) | 13 (3/46) | 10.9 (5/46) | 7.3 (3/41) |
| P value between groups | >.999 (NS) | .168 (NS) | .448 (NS) | .242 (NS) | .631 (NS) |
a Results are reported as % (n/total patients). ATRA, Achilles tendon resting angle; NS, not significant.
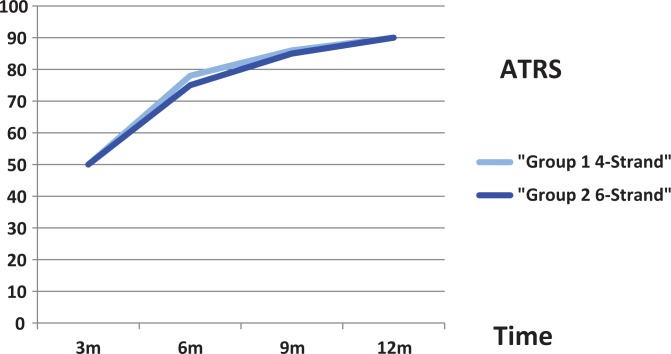
There were significant improvements in symptoms over time, as measured with ATRS, until 12 months (Figure 4 and Table 5), with no significant differences between the 2 groups (P = .827). The ATRS was significant for all pairwise comparisons.
Figure 4.
Comparison of the Achilles Tendon Total Rupture Score (ATRS) over time between group 1 (4-strand repair) and group 2 (6-strand repair) and overall. There was no significant difference between the groups (P = .827).
TABLE 5.
Comparison of the ATRS Over Time Between Group 1 (4-Strand Repair) and Group 2 (6-Strand Repair) and Overalla
| ATRS | 3 Months | 6 Months | 9 Months | 12 Months |
|---|---|---|---|---|
| Group 1 | ||||
| Median (range) | 55 (14-80) | 76 (57-98) | 92 (48-100) | 93 (45-100) |
| Mean (SD) | 50 (22) | 78 (14) | 86 (14) | 90 (14) |
| Group 2 | ||||
| Median (range) | 45 (3-86) | 77 (28-98) | 89 (52-100) | 94 (35-100) |
| Mean (SD) | 50 (17) | 75 (16) | 86 (13) | 90 (13) |
| Overall | ||||
| Median (range) | 45 (3-86) | 77 (28-98) | 89 (48-100) | 93 (35-100) |
| Mean (SD) | 50 (18) | 76 (15.2) | 86 (13.2) | 90 (13) |
| P value | <.0001 | <.0001 | .005 |
aThere was no significant difference between the groups (P = .827). ATRS, Achilles Tendon Total Rupture Score.
The maximal mean (SD) reduction in calf circumference occurred at the 6-week time point: –2.0 (1.6) cm. This atrophy improved with time, but circumference was still reduced at 12 months following repair: –1.3 (1.0) cm. There was significant calf atrophy from rupture until 6 weeks and then from 6 weeks to 3 months (P < .001) (Table 6). The calf increased in circumference from 3 to 6 months (P = .012); after this time, although the calf increased in size, this improvement was not significant. Calf circumference at 6 and 9 months only weakly correlated with the relative ATRA at 12 months (r = 0.316, P = .019 and r = 0.285, P = .035, respectively).
TABLE 6.
Comparison of the Change in Calf Circumference Difference With Time Between the 2 Groupsa
| Calf Circumference Difference | Postinjury | 6 Weeks | 3 Months | 6 Months | 9 Months | 12 Months |
|---|---|---|---|---|---|---|
| Group 1 | 0.18 (1.4) | –2.2 (1.2) | –0.7 (1.3) | –0.8 (1.6) | –1.1 (1.1) | –1.3 (1.0) |
| Group 2 | –0.1 (1.2) | –1.9 (1.8) | –0.9 (1.4) | –1.3 (1.3) | –1.6 (1.1) | –1.3 (1.0) |
| Overall | 0.0 (1.3) | –2.0 (1.6) | –0.9 (1.3) | –1.2 (1.4) | –1.4 (1.1) | –1.3 (1.0) |
aResults are reported in centimeters as mean (SD). There was no significant difference between the 2 groups (P = .508).
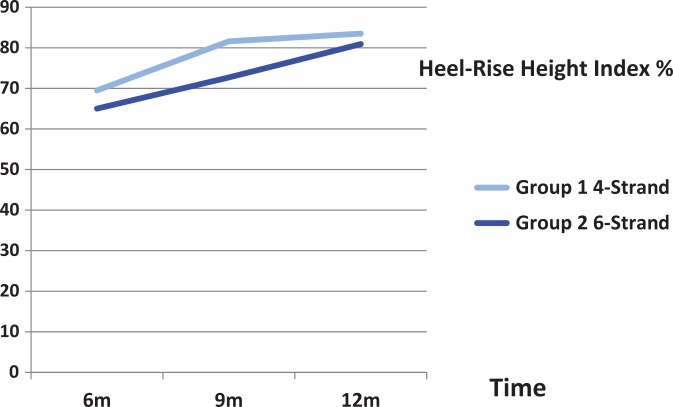
At the 12-month time point, the mean (SD) HRHI and HRRI were 81% (0.22%) and 82.6% (0.17%), respectively. The HRHI improved significantly over time, for pairwise comparisons, between 6 and 9 months (P < .001) and at 9 and 12 months (P = .047). The mean HRHI at 6 months was 66% (26%): group 1, 69.5% (27.0%); group 2, 65% (26.3%). At 9 months, the mean HRHI was 75.3% (21.4%), with 81.6% (18.9%) in group 1 and 72.7% (22.0%) in group 2. Overall HRHI improved to 81.7% (22%) at 12 months: 83.5% (16.6%) for group 1 and 80.9% (23.8%) for group 2 (Figure 5 and Table 7). There was no significant difference in HRHI over time between the groups (P = .323). In both groups 1 and 2, ATRA correlated with HRHI; however, ATRA was not found to correlate with HRRI in group 2.
Figure 5.
Comparison of the Heel-Rise Height Index over time between group 1 (4-strand repair) and group 2 (6-strand repair).
TABLE 7.
Correlation Between ATRA and ATRS, HRHI, and HRRIa
| HRHI 9 Months | ATRS 12 Months | HRHI 12 Months | HRRI 12 Months | |||||
|---|---|---|---|---|---|---|---|---|
| ATRA at Time Point and Group | Correlation | P Value | Correlation | P Value | Correlation | P Value | Correlation | P Value |
| 3 months | ||||||||
| Group 1 | 0.59 | .013b | 0.624 | .006b | 0.698 | .002b | ||
| Group 2 | 0.017 | .913 | 0.421 | .006b | 0.666 | <.0001b | 0.209 | .276 |
| 6 months | ||||||||
| Group 1 | 0.589 | .016b | 0.344 | .176 | 0.721 | .001b | ||
| Group 2 | 0.002 | .987 | 0.307 | .048b | 0.398 | .01b | 0.303 | .104 |
| 9 months | ||||||||
| Group 1 | 0.761 | <.0001b | 0.486 | .048b | 0.717 | .002b | ||
| Group 2 | 0.489 | .001b | –0.068 | .675 | –0.006 | .973 | 0.214 | .264 |
| 12 months | ||||||||
| Group 1 | 0.845 | <.0001b | 0.588 | .01b | 0.800 | <.0001b | ||
| Group 2 | 0.005 | .974 | 0.367 | .018b | 0.488 | .001b | 0.327 | .083 |
aATRA, Achilles tendon resting angle; ATRS, Achilles Tendon Total Rupture Score; HRHI, Heel-Rise Height Index; HRRI, Heel-Rise Repetition Index.
bSignificant correlation.
The overall relative ATRA at 3 months and 12 months both moderately correlated significantly with HRHI at 12 months (r = 0.617, P < .001 and r = 0.535, P < .001, respectively). For both groups 1 and 2, there was significant correlation between ATRA at 3 months and ATRS and HRHI at 12 months (Table 7).
The ATRA was not found to correlate with HRRI in group 2. The relative ATRA had no significant correlation with HRRI at 3, 6, 9, or 12 months (r = 0.209, P = .276; r = 0.303, P = .104; r = .214, P = .264; and r = 0.327, P = .083, respectively). At 12 months, the HRRI correlated with the HRHI (r = 0.449, P = .013).
PPP in terms of return to play was noted (Table 8). There were no significant differences in PPP between group 1 (4-strand repairs) and group 2 (6-strand repairs) (P = .685).
TABLE 8.
Comparison of Return to Play Over Time and Between Groups
| 6 Months, % (n) | 9 Months, % (n) | 12 Months, % (n) | |
|---|---|---|---|
| Not yet | |||
| Group 1 | 84 (16) | 67 (12) | 47 (7) |
| Group 2 | 89 (40) | 58 (26) | 46 (27) |
| Overall | 88 (56) | 64 (38) | 45 (20) |
| Same | |||
| Group 1 | 16 (3) | 28 (5) | 40 (6) |
| Group 2 | 11 (5) | 40 (18) | 45 (26) |
| Overall | 13 (8) | 37 (23) | 45 (20) |
| Improved | |||
| Group1 | 0 | 6 (1) | 13 (2) |
| Group 2 | 0 | 2 (1) | 10 (6) |
| Overall | 0 | 3 (2) | 9 (4) |
| Same and improved | |||
| Group 1 | 16 (3) | 33 (6) | 53 (8) |
| Group 2 | 11 (5) | 42 (19) | 55 (32) |
| Overall | 13 (8) | 40 (25) | 54 (24) |
| Tegner | |||
| Group 1 | 5 (3-5) | 5 (5-7) | 6 (3-8) |
| Group 2 | 5 (1-8) | 5 (1-8) | 5 (3-9) |
| Overall | 5 (1-8) | 5 (1-8) | 5 (3-9) |
At the 3-month time point, 31.1% (19/61) of patients were able to perform a single heel-rise, whereas 93.7% (59/63) were able to do so at the 6-month time point. Four patients were unable to perform a single heel-rise at 6 months. One patient was from group 1 and 3 patients from group 2. The patients in group 2 were still unable to perform a single heel-rise by 12 months.
Discussion
The most important finding of this study was that there was no difference in outcome for patients whose Achilles tendons were repaired using a 4-strand repair and a 6-strand repair. The 6-strand repair tended to lead to a smaller ATRA after rehabilitation; however, the 4- and 6-stranded repairs did not show a significantly different ATRA at follow-up. There was no difference in heel-rise height between the 2 groups, and a reduced height (80.9%) was found compared with the noninjured side at 12 months. The ATRA at 3 months for both 4- and 6-strand repairs correlated with the ATRS and HRHI at 12 months.
In addition, the use of a nonabsorbable suture during minimally invasive repair of an Achilles tendon rupture and accelerated rehabilitation did not prevent an increase in relative ATRA. The ATRA was reduced following surgical repair and then increased during weightbearing with a protective anterior brace to a similar angle to the noninjured side. Patients commenced active plantar flexion, inversion, and eversion exercises nonweightbearing during this time period. Subsequent increase of the angle until the 3-month time point coincided with weightbearing protected with a heel-wedge rather than anterior brace, and the commencement of a strengthening program. After this time point, the angle tended to decrease toward that of the noninjured side, although this was clinically not relevant and not statistically significant.
The degree and progress of ATRA in this series of patients with Achilles tendons repaired using nonabsorbable suture were comparable to a previous study where the Achilles tendon was repaired using an 8-strand absorbable suture.5 In that series, the ATRA was reduced to 7° following surgical repair and then reduced with weightbearing in the brace to 2.6°. Subsequently, the ATRA increased at the 3-month time point to –6.5° and was at –4.7° at the 12-month follow-up. The similar progression with time suggests that the absorption of the suture is not the reason for the increase in ATRA. The pull-through of the suture within tendon with initial loading may, however, explain this increase.
Although there was no difference in mean outcome between the use of 4- and 6-strand nonabsorbable repairs, the proportion of patients receiving a 4-strand repair who had a relative ATRA of ≥–12 was almost twice that of those having a 6-strand repair at the 3-month time point; however, this had fallen to 1.5 times by the 12-month time point (Figure 3). Thus, the decision to increase the number of strands did not influence the mean outcome but did reduce the proportion of patients with an increased ATRA. A similar progression of ATRA has been seen using an 8-strand absorbable repair. This suggests that repairs using more suture strands may be less likely to have an increased ATRA. It may be that differing suture configurations, in particular locking sutures, may have greater resistance to elongation. Conversely, it has been noted that with a greater quantity of suture material and a tighter repair, presumably a stiffer repair may have less favorable long-term biomechanical properties.35,36 Absorbable sutures have the advantage that they absorb with time, and removal may not be required should infection or sural nerve involvement occur.
The ATRA reflects the resting posture of the ankle, subtalar, and midfoot joint, but a direct relationship of this angle to the length of the Achilles tendon has yet to be shown, and future imaging studies are needed. Extended field-of-view ultrasound imaging has been shown to be a reliable and valid method of determining calcaneal to gastrocnemius length (intraclass correlation coefficient, 0.895; SEM, 0.67).37 In cadaveric studies, Costa et al10 determined that 1 cm of tenotomized tendon-end separation corresponded to a 12° increase in ankle dorsiflexion, and it is reasonable to compare this to lengthening of the Achilles tendon. It was for this reason that ≥–12° angle change, corresponding to ≥1 cm elongation, was chosen as a threshold for comparison of predictability of repair.36
Although there are differences in postoperative and nonoperative rehabilitation protocols, a consistent finding for studies regarding resting angle is that changes were related to the period of time mobilizing after splint removal. The 12-month findings of a relative ATRA of 5.5° and an HRHI of 80% are almost identical to a recent series of nonoperatively managed patients.15 In the study of Ecker et al,15 patients were protected for a longer time using a 20° equinus weightbearing cast for the first 6 weeks and then a boot with heel wedges of diminishing height until 12 weeks. In the present study, a brace was used for 6 weeks, with a 15-mm heel wedge until 3 months. Using steel suture markers, Cetti et al9 reported a significant elongation of 6.3 mm during this time period. The change in ATRA relates to the period of early weightbearing and early mobilization, suggesting reconsideration of the concept of early rehabilitation. It is appreciated that some of the change in ATRA may be the alleviation of stiffness resultant from brace use. In addition, the wedges alone did not prevent increments in ATRA, although it should be noted that patient compliance for wedge use was not recorded.
The complication rate was low, particularly the rerupture rate of 2.9% (2 patients). It is notable that both of these patients were noncompliant. There was a 1.5% superficial infection rate, treated with oral antibiotics and there were no cases of sural nerve injury related to surgery. A postinjury sural nerve rate of 10% was identified prior to surgery being performed. This rate was comparable to the injury-related neuropraxia rate reported by Lim et al23 in a randomized controlled trial of percutaneous versus open repair. It is recommended that clinicians check for the presence of injury-related neurapraxia before commencing management.
The outcomes in this study are similar to others regarding symptoms reflected by the ATRS1,5,6,33,36 and function, as well as the HRHI, except for at the 3-month time point when 30% of patients in this study were able to perform a single-heel rise compared with 50% in the series of Olsson et al.31 The reason could be differences in the rehabilitation or patient evaluation. In the series of Olsson et al, the evaluation was performed after a warm-up exercise period, including double-heel rise, prior to assessment. This was not possible in the clinical setting in which this study was conducted.
The strength of this study is its pragmatic nature, evaluating the outcomes of current practice and using simple, inexpensive outcome measures that can easily be adopted in the clinical setting. An additional strength of the present study is that a single surgeon operated and assessed outcomes on all patients; although this might introduce an aspect of performance bias, it also eliminates interobserver error. Limitations of this study include the small sample size; lack of randomization; unbalanced design, with only 19 patients in the 4-strand group introducing selection bias; and lack of blinding. In addition, the HRRI was performed only in patients in group 2. The use of a more accurate muscle-lab assessment to determine heel-rise endurance may reveal a correlation with ATRA in future studies. Repairs performed using 4 strands were ceased out of concern that the sutures in this group were cutting through the tendon with loading, leading to elongation. However, on final outcome analysis, this concern did not appear to be justified.
The absence of a direct measure of tendon length, such as magnetic resonance imaging (MRI) or ultrasonography, and an accurate determination of heel-rise work and endurance are also considered limitations of the present study. An additional limitation is that the weak correlation between calf circumference and relative ATRA may be related to the presence of asymptomatic deep vein thrombosis (DVT), increasing the calf circumference due to interstitial fluid edema. Ultrasound scanning could have allowed for patients with a DVT to be excluded and increased the correlation. Alternatively, calf muscle size and volume could have been determined using computed tomography and MRI scanning.
It is possible that the suture technique may be important in the early stages of healing after repair to preserve intratendinous tension. The aspects of duration of brace protection while weightbearing and the timing of loading commencement to prevent elongation require further investigation.
Conclusion
There was no difference in ATRA or clinical outcome performed using 4-strand and 6-strand minimally invasive repair. Nonabsorbable suture technique and accelerated rehabilitation did not prevent an increased ATRA over time. Increasing the number of suture strands did not affect the increment in ATRA or the heel-rise index. The ATRA at 3 months following surgery correlated moderately with ATRS and HRHI at 12 months. The aspects of the duration of brace protection while weightbearing and the timing of commencement of loading require further investigation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was provided in part by the British Association of Sport and Exercise Medicine (to M.R.C.). M.R.C. is an instructor and member of the teaching faculty for Arthrex.
Ethical approval for this study was obtained from the Shrewsbury and Telford Hospital NHS Trust.
References
- 1. Al-Mouazzen L, Rajakulendran K, Najefi A, Ahad N. Percutaneous repair followed by accelerated rehabilitation for acute Achilles tendon ruptures. J Orthop Surg (Hong Kong). 2005;23(3):352–356. [DOI] [PubMed] [Google Scholar]
- 2. Bostick GP, Jomha NM, Suchak AA, Beaupre LA. Factors associated with calf muscle endurance recovery 1 year after Achilles tendon rupture repair. J Orthop Sports Phys Ther. 2010;40(6):345–351. [DOI] [PubMed] [Google Scholar]
- 3. Braunstein M, Baumbach SF, Boecker W, Carmont MR, Polzer H. Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair [published online September 26, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3795-1. [DOI] [PubMed] [Google Scholar]
- 4. Carmont MR, Maffulli N. Modified percutaneous repair of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2008;16:199–203. [DOI] [PubMed] [Google Scholar]
- 5. Carmont MR, Silbernagel KG, Brorsson A, Olsson N, Maffulli N, Karlsson J. The Achilles tendon resting angle as an indirect measure of Achilles tendon length following rupture, repair and rehabilitation. Asia Pacific J Sports Med Arthrosc Rehabil Technology. 2015;2(2):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carmont MR, Silbernagel KG, Edge A, Mei-Dan O, Karlsson J, Maffulli N. Functional outcome of percutaneous Achilles repair: improvements in Achilles Tendon Total Rupture Score during the first year. Orthop J Sports Med. 2013;1(1):2325967113494584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carmont MR, Silbernagel KG, Mathy A, Mulji Y, Karlsson J, Maffulli N. Reliability of Achilles tendon resting angle and calf circumference measurement techniques. Foot Ankle Surg. 2013:19(4):245–249. [DOI] [PubMed] [Google Scholar]
- 8. Carmont MR, Silbernagel KG, Nilsson-Helander K, Mei-Dan O, Karlsson J, Maffulli N. Cross cultural adaptation of the Achilles Tendon Total Rupture Score with reliability, validity and responsiveness evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1356–1360. [DOI] [PubMed] [Google Scholar]
- 9. Cetti R, Christiansen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus non-operative treatment of Achilles tendon rupture. A prospective randomised study and review of the literature. Am J Sports Med. 1993;21:791–799. [DOI] [PubMed] [Google Scholar]
- 10. Costa ML, Logan K, Heylings D, Donell ST, Tucker K. The effect of Achilles tendon lengthening on ankle dorsiflexion: a cadaver study. Foot Ankle Int. 2006:27(6):414–417. [DOI] [PubMed] [Google Scholar]
- 11. Cretnik A, Kosanovic M, Smrkolj V. Percutaneous versus open repair of the ruptured Achilles tendon: a comparative study. Am J Sports Med. 2005;33(9):1369–1379. [DOI] [PubMed] [Google Scholar]
- 12. De La Fuente C, Peña y Lillo R, Carreño G, Marambio H. Prospective randomized clinical trial of aggressive rehabilitation after acute Achilles tendon ruptures repaired with Dresden technique. Foot (Edin). 2016;26:15–22. [DOI] [PubMed] [Google Scholar]
- 13. Del Buono A, Volpin A, Maffulli N. Minimally invasive versus open surgery for acute Achilles tendon rupture: a systematic review. Br Med Bull. 2014;109:45–54. [DOI] [PubMed] [Google Scholar]
- 14. Demetracopoulos CA, Gilbert SL, Young E, Baxter JR, Deland JT. Limited open Achilles tendon repair using locking sutures versus non-locking sutures: an in-vitro model. Foot Ankle Int. 2014;35(6):612–618. [DOI] [PubMed] [Google Scholar]
- 15. Ecker TM, Bremer AK, Krause FG, Müller T, Weber M. Prospective use of a standardized non-operative early weight-bearing protocol for Achilles tendon rupture: 17 years of experience. Am J Sports Med. 2016;44(4):1004–1010. [DOI] [PubMed] [Google Scholar]
- 16. Gross CE, Nunley JA II. Acute Achilles tendon ruptures. Foot Ankle Int. 2016;37(2):233–239. [DOI] [PubMed] [Google Scholar]
- 17. Guillo S, Del Buono A, Dias M, Denaro V, Maffulli N. Percutaneous repair of acute ruptures of the tendo Achillis. Surgeon. 2013;11(1):14–19. [DOI] [PubMed] [Google Scholar]
- 18. Hansen MS, Barfod KW, Kristensen MT. Development and reliability of the Achilles tendon length measure and comparison with the Achilles tendon resting angle on patients with an Achilles tendon rupture [published online August 21, 2016]. Foot Ankle Surg. doi:http://dx.doi.org/10.1016/j.fas.2016.08.002. [DOI] [PubMed]
- 19. Heikkinen J, Lantto I, Flinkkilä T, et al. Augmented compared to non-augmented surgical repair after total Achilles rupture: results of a prospective randomized trial with 13 or more years of follow up. J Bone Joint Surg Am. 2016;98(2):85–92. [DOI] [PubMed] [Google Scholar]
- 20. Horstmann T, Lukas C, Merk J, Bruaner T, Mündermann A. Deficits 10 years after Achilles tendon repair. Int J Sports Med. 2012;33(6):474–479. [DOI] [PubMed] [Google Scholar]
- 21. Keller A, Ortiz C, Wagner E, Wagner P, Mococain P. Mini-open tenorrhaphy of acute Achilles tendon ruptures: a medium term follow up of 100 cases. Am J Sports Med. 2014;42(3):731–736. [DOI] [PubMed] [Google Scholar]
- 22. Lantto I, Heikkinen J, Flinkkilä T, et al. Early functional treatment versus cast immobilization in tension after Achilles rupture repair: results of a prospective randomized trial with 10 years or more of follow up. Am J Sports Med. 2015;43(9):2302–2309. [DOI] [PubMed] [Google Scholar]
- 23. Lim J, Dalai R, Waseem M. Percutaneous versus open repair of the ruptured Achilles tendon: a prospective randomized controlled study. Foot Ankle Int. 2001;22(7):559–568. [DOI] [PubMed] [Google Scholar]
- 24. Longo UG, Forriol F, Campi S, Maffulli N, Denaro V. A biomechanical comparison of the primary stability of two minimally invasive techniques for repair of ruptured Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1392–1397. [DOI] [PubMed] [Google Scholar]
- 25. Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon: a prospective study in 174 patients. Am J Sports Med. 1998;26:266–270. [DOI] [PubMed] [Google Scholar]
- 26. Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in diabetic patients. Arch Orthop Trauma Surg. 2011;131(1):33–38. [DOI] [PubMed] [Google Scholar]
- 27. Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in elite athletes. Foot Ankle Int. 2011:32(1):9–15. [DOI] [PubMed] [Google Scholar]
- 28. Maffulli N, Longo UG, Ronga M, Khanna A, Denaro V. Favourable outcome of percutaneous repair of Achilles tendon ruptures in the elderly. Clin Orthop Relat Res. 2010;468(4):1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mavrodontidis A, Lykissas M, Koulouvaris P, Pafilas D, Kontogeorgakos V, Zalavras C. Percutaneous repair of acute Achilles tendon rupture: a functional evaluation study with a minimum 10 year follow up. Acta Orthop Traumatol Turc. 2015;49(6):661–667. [DOI] [PubMed] [Google Scholar]
- 30. Nilsson-Helander K, Thomeé R, Grävare Silbernagel K, et al. The Achilles Tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–425. [DOI] [PubMed] [Google Scholar]
- 31. Olsson N, Karlsson J, Eriksson BI, Brorsson A, Lundberg M, Silbernagel KG. Ability to perform a single heel-rise is significantly related to patient reported outcome after Achilles tendon rupture. Scand J Med Sci Sports. 2014;24(1):152–158. [DOI] [PubMed] [Google Scholar]
- 32. Olsson N, Nilsson-Helander K, Karlsson J, et al. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19:1385–1393. [DOI] [PubMed] [Google Scholar]
- 33. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus non-surgical management for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41(12):2867–2876. [DOI] [PubMed] [Google Scholar]
- 34. Ortiz C, Wagner E, Mococain P, et al. Biomechanical comparison of four methods of repair of the Achilles tendon: a laboratory study with bovine tendons. J Bone Joint Surg Br. 2012;94(5):663–667. [DOI] [PubMed] [Google Scholar]
- 35. Schepull T, Aspenberg P. Healing human Achilles tendon ruptures: radiodensity reflects mechanical properties. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):884–889. [DOI] [PubMed] [Google Scholar]
- 36. Schepull T, Kvist J, Aspenberg P. Early E modulus of healing Achilles tendons correlates with late function: similar results with or without surgery. Scand J Med Sci Sports. 2012;22(1):18–23. [DOI] [PubMed] [Google Scholar]
- 37. Silbernagel KG, Nilsson-Helander K, Thomeé R, Eriksson BI, Karlsson J. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):258–264. [DOI] [PubMed] [Google Scholar]
- 38. Silbernagel KG, Steele R, Manal K. Deficits in heel-rise height and Achilles tendon elongation occur in patients recovering from an Achilles tendon rupture. Am J Sports Med. 2012;40(7):1564–1571. [DOI] [PubMed] [Google Scholar]
- 39. Simmonds FA. The diagnosis of the ruptured Achilles tendon. Practitioner. 1957;179(1069):56–58. [PubMed] [Google Scholar]
- 40. Suydam SM, Buchannan TS, Manal K, Silbernagel KG. Compensatory muscle activation caused by tendon lengthening post Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tegner Y, Lyholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 42. Willits K, Amendola A, Bryant D, et al. Operative versus non-operative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:767–775. [DOI] [PubMed] [Google Scholar]
- 43. Zellers J, Carmont MR, Grävare-Silbernagel K. Return to play post Achilles tendon rupture: a systematic review and meta-analysis of rate and measures of return to play. Br J Sports Med. 2016;50(21):1325–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]