Abstract
Rationale:
We report a case of acute steroid myopathy in a patient with eczema receiving one dose of intra-muscular injection of Compound betamethasone.
Patient concerns:
Acute steroid myopathy (ASM) is usually caused by exogenous corticosteroids, and typically, occurs with therapy using intravenous corticosteroids at high doses.
Diagnoses:
The patient was considered as a diagnosis of acute steroid myopathy.
Interventions:
The patient was treated with non-steroid anti-inflammatory drug and other symptomatic therapy.
Outcomes:
ASM was gradually improved after 2 weeks symptomatic treatment and completely recovered after one-month treatment.
Lessons:
The diagnosis of steroid myopathy is a clinical diagnosis based on characteristic symptoms. Higher dose of steroids, especially fluorinated steroids, for longer periods of time increases the risk of steroid-induced myopathy.
Keywords: acute steroid myopathy, betamethasone, eczema
1. Introduction
Steroid myopathy is presented as diffuse myalgia and weakness of proximal muscles of lower extremities, which is caused by either endogenous or exogenous excess of corticosteroid. In the clinic of dermatology, chronic steroid myopathy is more common and develops after prolonged usage of steroid.[1] In contrast, acute steroid myopathy (ASM) is rare and poorly understood. Typically, ASM presents as acute muscle weakness and muscular pain in response to receiving high doses of steroid therapy. It has been reported that ASM occurs in patients with asthma receiving high-dose intravenous corticosteroids[2,3] or patients received oral methylprednisolone[4] or 1 dose of oral corticosteroid therapy.[5]
Betamethasone, a synthetic and fluorinated steroids, is one of the commonly used glucocorticoids and rarely has side effect. Here, we report a case of acute steroid myopathy in a patient with eczema receiving one dose of intra-muscular injection of Compound betamethasone (betamethasone sodium phosphate and betamethasone dipropionate).
2. Case presentation
This study was approved by The Institutional Review Board of Ethics Committee of Beijing Anzhen Hospital, Capital Medical University. A 64-year-old Chinese woman presented to the outpatient clinic with complaints of pain in the muscle of 2 legs for 3 days. She was diagnosed with pan eczema 3 years ago, which was exacerbated for 2 weeks. She was given ebastine tablets without significant effect and thus, given intra-muscular injection of 1 mg betamethasone. Although the symptoms of eczema were relieved, myalgia and muscle weakness progressed to involve arms and legs on day 3, and the patient had difficulty in walking and suffered with depress. She never drinks or smokes. No history of chronic diseases or cardiovascular diseases. She did not use any statins recently. Eczema was controlled by external or oral anti-histamine drugs for last 3 years.
On physical examination, her vital signs including blood pressure (125/75 mm Hg) and pulse (70 beats/min), respiratory rate (21 breaths/min), temperature (36.4°C) were normal. Erythema, scratch, and scar were observed on her trunk and extremities. Edema and palpation pain were found on both tibial anterior legs musculature. Tendon reflex on both legs was decreased, but Babinski's sign was absent. Muscle strength on both arms and legs were grade IV.
On laboratory examination, lactate dehydrogenase (LDH) and aspartate aminotransferase (AST) were 4 times higher than normal value, and creatinine kinase (CK) was 25 times higher than normal range (Table 1). Her serum potassium was 3.2 mmol/L, but other results of basic metabolic panel and complete blood count were normal. Ultrasound examination on the left tibialis anterior compartment showed cloudy or ground-glass-like appearance with echo enhancement; the liquid dark area between the muscles or between muscle and bone; and the unsmooth surface of arterial intima. Muscle biopsy and electromyography (EMG) were not performed.
Table 1.
Laboratory examination results on different days after betamethasone injection.
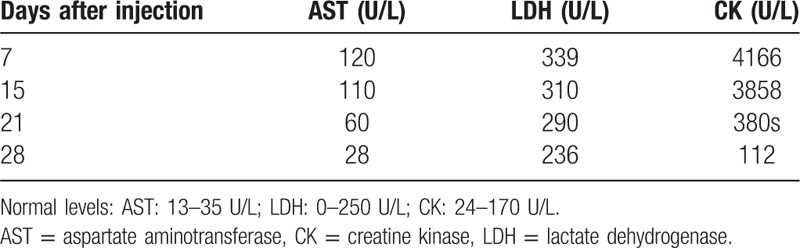
She was considered as a diagnosis of acute steroid myopathy. She was treated with combination of ibuprofen and codeine (0.2 mg and 12.5 mg for each piece) as needed for myalgia, and potassium orally for hypo-potassium. Eczema was treated with Claritin and symptoms got relieved. After 7 days treatment, CK decreased, and symptoms including myalgia, neck, and shoulder discomfort were relieved. One month after treatment, all symptoms were relieved and all levels of laboratory examinations were back to normal.
3. Discussion
Skeletal muscle accounts for 45% of body weight, and due to high metabolic capability and blood circulation, skeletal muscle is often targeted by variety kinds of drugs.[6] Steroid-induced myopathy is one of the drug-induced side-effects and it is caused by either endogenous or exogenous excess of steroid, which leads to proximal muscle weakness and decrease of muscle strength. Here, we report a case of exogenous betamethasone-induced acute myopathy.
In 1958, Dubois first reported iatrogenic steroid-induced myopathy.[7] Since then, with wide application of steroid in clinic, incidence of steroid-induced myopathy has been increased and reported from 7to 60% of prevalence.[8] Susceptible population of steroid-induced myopathy includes seniors, cancer patients, malnutrition, or physically inactive patients.[9] Type and dose of steroid are associated with steroid myopathy. In this regard, the use of fluorinated synthetic steroids in doses of 40 mg/day or higher may result in muscle weakness, whereas the use of non-fluorinated steroids and in doses of lower than 10 mg/day are rarely associated with glucocorticoid-induced myopathy.[10,11] Betamethasone, which was given to this patient by intra-muscular injection (1 mg), is a synthetic fluorinated steroid and often used for skin diseases. To our knowledge, this is the first case of betamethasone-induce myopathy.
Steroid-induced myopathy can be either acute or chronic form. The acute form is characterized by rapidly progressive weakness of the proximal and distal muscle group.[12] In contrast, chronic form of steroid-induced myopathy is featured by chronic development of muscle weakness, which progresses slowly and is usually painless or mildly painful.[9] Weakness is primarily proximal muscle of lower extremities, and the distal muscles are rarely affected.[9] In the current study, however, palpation pain was found on both tibial anterior legs musculature.
The diagnosis of steroid myopathy is a clinical diagnosis and involves history of exogenous glucocorticoid use and clinical manifestations. Typical presentations include diffuse myalgia and muscle weakness. Our patient received betamethasone, and she had myalgia and progressive muscle weakness. Based on the history of betamethasone injection and clinical manifestation of muscle weakness, she was diagnosed as acute steroid myopathy. This diagnosis was further supported by the laboratory examination of lactate dehydrogenase (LDH), aspartate aminotransferase (AST), and creatine kinase (CK), which were significantly higher than normal values. However, differentiating diagnosis with compartment syndrome should be considered. Compartment syndrome is often caused by overuse of the muscles, ischemia, or trauma. The patient of this case report, however, did not have a history of overuse muscle, ischemia, or trauma. Thus, the compartment syndrome was excluded in this case.
The serum potassium level was lower than normal in this case. Hypokalemia might be due to insufficient uptake with food or diarrhea. It may also be caused by medications including betamethasone.[13] However, in this case, hypokalemia is unlikely caused by betamethasone in that it was used only once by intramuscular injection, and furthermore, the patient's serum calcium level was normal.
When the exogenous cause of steroid-induced myopathy is diagnosed, reducing steroid dose and switching to a nonfluorinated agent should be considered. An increase in muscle strength can be observed within 3 to 4 weeks after discontinuation of the glucocorticoid.[9,11] Various medications including creatine, androgens, potassium, and vitamins have been investigated for use in steroid myopathy.[14,15] Physical therapy may be useful in preventing and treating muscle weakness in patients receiving glucocorticoids.[16,17] In the current study, the patient was simply treated with general medicine to control the symptoms, for instance, nonsteroid anti-inflammatory drugs for myalgia. After 1-month treatment, symptoms of steroid-induced myopathy were relieved and laboratory examinations were back to normal.
4. Conclusion
Steroids, which are widely used in clinic for treatment of variety kinds of diseases, can cause a number of adverse effects including ocular, cardiovascular, muscular, and psychiatric side effects.[11] Of those side effects, steroid myopathy needs to be recognized early to ameliorate its significant effects. The diagnosis of steroid myopathy is a clinical diagnosis based on characteristic symptoms. Higher dose of steroids, especially fluorinated steroids, for longer periods of time increases the risk of steroid-induced myopathy.
Footnotes
Abbreviations: ASM = acute steroid myopathy, AST = aspartate aminotransferase, CK = creatine kinase, EMG = electromyography, LDH = lactate dehydrogenase.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Naim MY, Reed AM. Enzyme elevation in patients with juvenile dermatomyositis and steroid myopathy. J Rheumatol 2006;33:1392–4. [PubMed] [Google Scholar]
- [2].MacFarlane IA, Rosenthal FD. Severe myopathy after status asthmaticus. Lancet 1977;2:615. [DOI] [PubMed] [Google Scholar]
- [3].Van Marle W, Woods KL. Acute hydrocortisone myopathy. Br Med J 1980;281:271–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Khan MA, Larson E. Acute myopathy secondary to oral steroid therapy in a 49-year-old man: a case report. J Med Case Rep 2011;5:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kumar S. Steroid-induced myopathy following a single oral dose of prednisolone. Neurol India 2003;51:554–6. [PubMed] [Google Scholar]
- [6].Evans M, Rees A. Effects of HMG-CoA reductase inhibitors on skeletal muscle: are all statins the same? Drug Saf 2002;25:649–63. [DOI] [PubMed] [Google Scholar]
- [7].Dubois EL. Triamcinolone in the treatment of systemic lupus erythematosus. J Am Med Assoc 1958;167:1590–9. [DOI] [PubMed] [Google Scholar]
- [8].Batchelor TT, et al. Steroid myopathy in cancer patients. Neurology 1997;48:1234–8. [DOI] [PubMed] [Google Scholar]
- [9].Pereira RM, Freire de Carvalho J. Glucocorticoid-induced myopathy. Joint Bone Spine 2011;78:41–4. [DOI] [PubMed] [Google Scholar]
- [10].Gupta A, Gupta Y. Glucocorticoid-induced myopathy: pathophysiology, diagnosis, and treatment. Indian J Endocrinol Metab 2013;17:913–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Caplan A, et al. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: ocular, cardiovascular, muscular, and psychiatric side effects and issues unique to pediatric patients. J Am Acad Dermatol 2017;76:201–7. [DOI] [PubMed] [Google Scholar]
- [12].van Balkom RH, et al. Corticosteroid-induced myopathy of the respiratory muscles. Neth J Med 1994;45:114–22. [PubMed] [Google Scholar]
- [13].Teagarden CM, Picardo CW. Betamethasone-induced hypokalemic periodic paralysis in pregnancy. Obstet Gynecol 2011;117:433–5. [DOI] [PubMed] [Google Scholar]
- [14].Minetto MA, et al. Steroid myopathy: some unresolved issues. J Endocrinol Invest 2011;34:370–5. [DOI] [PubMed] [Google Scholar]
- [15].Schakman O, Gilson H, Thissen JP. Mechanisms of glucocorticoid-induced myopathy. J Endocrinol 2008;197:1–0. [DOI] [PubMed] [Google Scholar]
- [16].Braith RW, et al. Resistance exercise prevents glucocorticoid-induced myopathy in heart transplant recipients. Med Sci Sports Exerc 1998;30:483–9. [DOI] [PubMed] [Google Scholar]
- [17].LaPier TK. Glucocorticoid-induced muscle atrophy. The role of exercise in treatment and prevention. J Cardiopulm Rehabil 1997;17:76–84. [DOI] [PubMed] [Google Scholar]


