Abstract
Rationale:
This study aims to evaluate the diagnostic value of beta-endorphin (β-EP) and brain natriuretic peptid (BNP) plasma concentrations for the early diagnosis of acute left heart failure and atrial fibrillation.
Patient concerns:
A total of 45 patients were included. These patients comprised 23 male and 22 female patients,and 20 healthy subjects who underwent physical examinations in the Outpatient Department during the same periodwere included and assigned to the control group.
Diagnoses:
The diagnos stand was that of the Chinese guidelines for the diagnosis and treatment of heart failure.
Interventions:
Enzyme-linked immunosorbent assay was performed to detect the plasma concentration of β-EP and BNP in the treatment and control groups, and electrocardiogram targeting was performed to determine the left ventricular ejection fraction (LVEF).
Outcomes:
BNP, β-EP, and LVEF levels were higher in the treatment group (688.01 ± 305.78 ng/L, 394.06 ± 180.97 ng/L, and 70.48 ± 16.62%) compared with the control group (33.90 ± 8.50 ng/L, 76.87 ± 57.21 ng/L, and 32.11 ± 5.25%). The P-values were .015, .019, and .026, respectively, which were <.05. The difference was statistically significant. The BNP and β-EP's 4 correlations (r = 0.895, P <.001), BNP, β-EP, and the combination of BNP and β-EP for acute left heart failure diagnosis in maximizing Youden index sensitivity, specific degree, area under the ROC curve (AUC), and 95% confidence interval (CI) were respectively 93.5%, 81.3%, 0.921, 0.841, 0.921; 80.5%, 78.6%, 0.697, 0.505, 0.697; 94.1%, 83.5%, 0.604 to 0.979, and 0.604. Acute left heart failure in patients with LVEF acuity plasma BNP and β-EP 50% group was obviously lower than that in the LVEF <50% group (P <.01). BNP, β-EP, and LVEF were negatively correlated (r = −0.741, −0.635, P = .013, .018).
Lessons:
β-EP and BNP have high specificity and sensitivity for detecting early acute left heart failure and atrial fibrillation in patients, which is convenient, easy to perform, and suitable for clinical applications.
Keywords: acute left heart failure, beta-endorphin, brain natriuretic peptide
1. Introduction
Acute heart failure pertains to the symptom and signs the sudden onset of heart failure, or worse, which requires urgent medical treatment and hospitalization. It is a severe life-threatening disease, and it is the most common in clinic. Due to its clinical onset, illness, rapid disease progression, and prognosis, there is a great uncertainty due to the high expectations of patients. At the same time, medical disputes in the medical diagnosis and treatment of this disease can easily occur.[1] Hence, there is a need to perform a correct diagnosis and evaluate this in a short period of time, in order to allow for reasonable treatment measures and improve the prognosis of patients. It is difficult to diagnose heart failure, while echocardiography can effectively evaluate cardiac systolic function. However, diastolic function evaluation is limited and cannot be applied for emergency situations. Hence, there is a need to seek a more convenient and feasible method with high specificity and sensitivity. Plasma brain natriuretic peptide (BNP) and beta-endorphin (β-EP) are important markers for heart failure.[2,3] Therefore, β-EP and BNP levels have been monitored for the early diagnosis and treatment of acute left heart failure. The details are reported as follows.
2. Data and methods
This study was conducted in accordance with the Declaration of Helsinki, and was conducted with approval of the Ethics Committee of our hospital. A written informed consent was obtained from all the participants.
2.1. General information
Patients who presented with acute left heart failure and atrial fibrillation in the Internal Medicine Emergency Department of the hospital were included according to the Chinese guidelines for the diagnosis and treatment of heart failure in 2014.[4] A total of 45 patients were included. These patients comprised 23 male and 22 female patients, and their age ranged from 23 to 88 years, with an average age of 45.3 ± 7.5 years. In addition, 20 healthy subjects (average age: 44.3 ± 9.3 years) who underwent physical examinations in the Outpatient Department during the same period were included and assigned to the control group.
2.2. Methods
From each patient, 3-mL venous blood was collected, placed in aprotinin tubes containing ethylenediaminetetraacetic acid (EDTA), centrifuged at 2500 rpm for 2 hours, centrifuged for 10 minutes to separate the plasma, and stored in a cryogenic refrigerator at −70°C. Enzyme-linked immunosorbent assay (ELISA) was performed to determine the plasma levels of β-EP and BNP.
2.3. Main instruments and reagents
BNP detection kits were purchased from Measured Biological Genetic Engineering Co., Ltd, Zhejiang University, β-endorphin detection kits were purchased from Shanghai Letter Biotechnology Co., Ltd, and the washing machine and enzyme standard instrument were obtained from Rayto (Shenzhen) Co., Ltd.
Heart function parameters were determined by echocardiography (HP 5500 color Doppler ultrasound diagnostic instrument) to evaluate the left ventricular ejection fraction (LVEF). The parameters were measured 3 times, and the average was taken.
SPSS 17.0 software was used for data processing and statistical analysis. Measurement data was presented as ±SD. Comparisons were performed by 2-sample t-test. The receiver operating characteristic (ROC) curve was plotted with Graph Pad 5.0 software. Two variables were compared using linear correlation analysis. By correlation analysis, P value <.05 was considered statistically significant.
3. Results
3.1. BNP, β-EP, and LVEF results in patients with acute left heart failure
BNP, β-EP, and LVEF levels in patients with acute left heart failure were compared with that in healthy controls. BNP, β-EP, and LVEF levels were higher in the case group (688.01 ± 305.78 ng/L, 394.06 ± 180.97 ng/L, 70.48 ± 16.62%) than in the control group (33.90 ± 8.50 ng/L, 76.87 ± 57.21 ng/L, 32.11 ± 5.25%) (t = 13.85, 9.17, 0.026, respectively). P < .05 was considered statistically significant (Table 1).
Table 1.
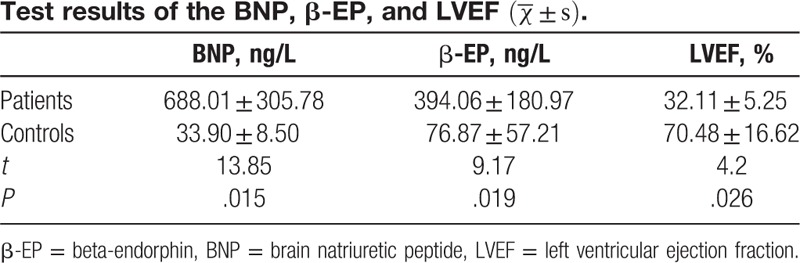
3.2. The correlation of BNP and β-EP in patients with acute left heart failure
BNP and β-EP in patients with acute left heart failure were positively correlated (r = 0.895, P < .001; Table 1, Fig. 1).
Figure 1.
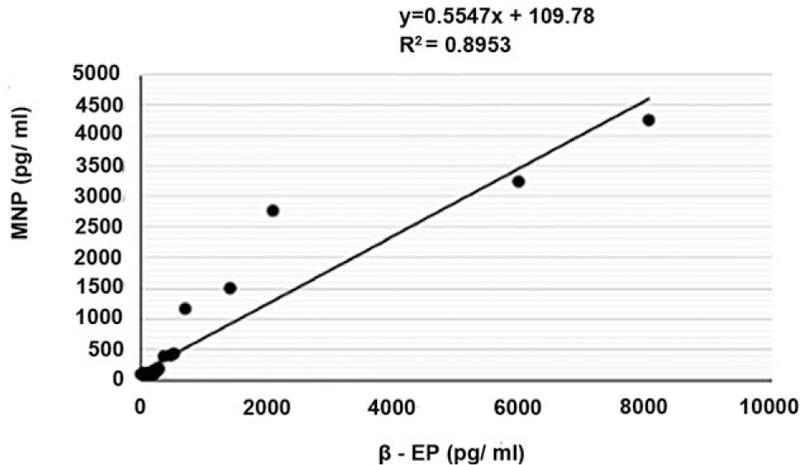
The correlation of BNP and β-EP in patients with acute left heart failure. β-EP = beta-endorphin, BNP = brain natriuretic peptide.
3.3. Comparison of the diagnostic features of BNP and β-EP for acute left heart failure
In terms of BNP, β-EP, and the combination of BNP and β-EP for the diagnosis of acute left heart failure, the maximize Youden index sensitivity, specific degree, area under the ROC curve (AUC), and 95% confidence interval (CI) were 93.5%, 81.3%, 0.921, 0.841, 0.921; 80.5%, 78.6%, 0.697, 0.505, 0.697; 94.1%, 83.5%, 0.604 to 0.979 and 0.979, respectively, as shown in Table 2 and Fig. 2.
Table 2.
The BNP and β-EP for acute left heart failure diagnostic features comparison.
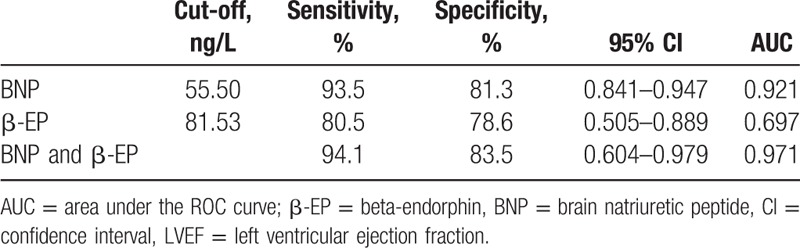
Figure 2.
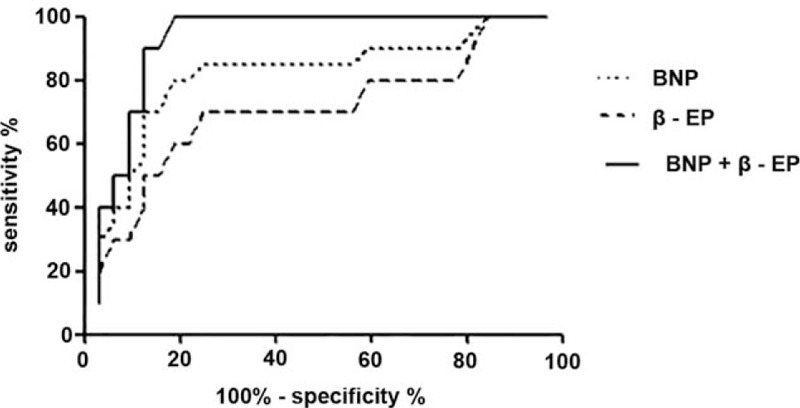
The ROC curve of BNP and β-EP. β-EP = beta-endorphin, BNP = brain natriuretic peptide, ROC = receiver operating characteristics.
3.4. Comparison of BNP and β-EP levels in acute left heart failure patients among the different LVEF groups
Plasma BNP and β-EP levels in acute left heart failure patients of the LVEF 50% group were significantly lower than those of the LVEF <50% group (P < .05). The BNP, β-EP, and LVEF levels were negatively correlated (r = −0.741, −0.635; P = .013, .018), as shown in Table 3 and Fig. 3.
Table 3.
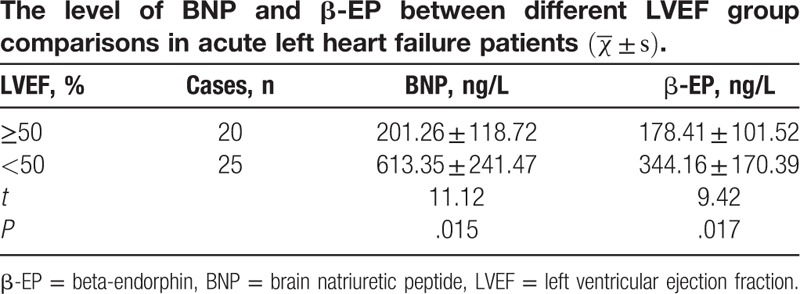
Figure 3.
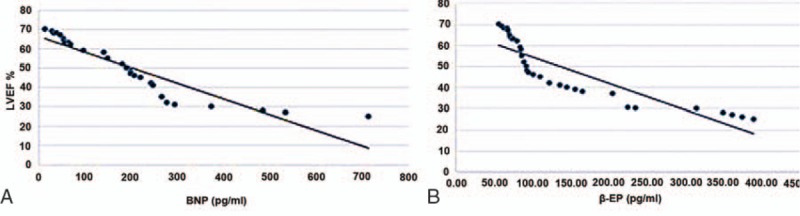
(A) The correlation between the BNP and LVEF%; (B) The correlation between the β-EP and LVEF (%). β-EP = beta-endorphin, BNP = brain natriuretic peptide, LVEF = left ventricular ejection fraction.
4. Discussion
Acute left heart failure, also known as acute left cardiac insufficiency, is clinically a common type of tendon, and also has one of the highest mortality rates of emergency. The prognosis of acute heart failure remains poor, hospital mortality is 3%, 60-day case fatality rate is 9.6%, >6 months hospitalization rate is ∼50%, and fatality rate in 3 or 5 years can reach as high as 30% or 50%, respectively.[5] There are approximately 6 million patients with heart failure in the USA, and the hospitalization for heart failure patients per year reaches up to 1 million or so.[6,7] The main clinical manifestations of this disease include breathe difficulties, acute pulmonary edema, cardiac shock, etc. The life of these patients is seriously threatened. Hence, first aid and treatment of acute left heart failure is particularly crucial. At present, the clinical diagnosis of heart failure is based on a simple, direct, noninvasive, and effective index obtained through heart ultrasound. LVEF is the most sensitive response to cardiac systolic function and is a specific indicator. In clinic, echocardiographic LVEF and power failure can be divided into decreased acute ejection fraction or power failure (acute heart failure with reduced ejection fraction, AHFREF) (LVEF <50%) and acute ejection fraction reserve force also failure (acute heart failure with preserved ejection fraction, AHFPEF) (LVEF >50%) for guidance in clinical treatment of acute heart faiure.[8] However, echocardiography is not convenient, and the technical level varies in different operators, such as subjective and objective factors, reducing the accuracy of the diagnosis of heart failure and cardiac function evaluation to a certain extent. At the same time, for echocardiography sensitivity for early heart failure, low LVEF has a lag for emergency first aid. Determining a rapid, objective, simple, and easy method for early detection is particularly important. Heart failure is a condition where there is neural endocrine imbalance. In the process of the development of heart failure, under a state of stress, the ventricular muscle cells and other sympathetic nervous systems can synthesize and secrete endogenous peptide substances such as BNP, β-EP, etc. These neuroendocrine factors are closely related to myocardial damage and heart function, and can be used for the early diagnosis and prognosis of heart failure.
B-type BNP from ventricular muscle cells induces diuretic natriuretic function synthesis and the secretion of endogenous peptides. In the ventricular wall, through mechanical force, ischemic damage, lack of oxygen and angiotensin, and when factors such as adrenaline are excited, all can stimulate BNP secretion release. BNP comprises of 32 amino acid peptides and has the neurohumoral bioactive natural hormone. A study found that blood BNP levels were positively correlated with the degree of myocardial ischemia and ventricular pressure.[9] In the present study, patients with acute left heart failure were compared with healthy controls. It was found that plasma BNP levels were higher in the cases group (688.01 ± 305.78 ng/L) than in the control group (33.90 ± 8.50 ng/L) (t = 13.85, P < .05), and the difference was statistically significant. Acute left heart failure was significantly lower in patients in the LVEF group 50% or higher plasma BNP (201.26 ± 118.72 ng/L) compared to the LVEF <50% group (613.35 ± 241.47) (t = 11.12, P = .015), and was negatively correlated with BNP and LVEF (r = −0.741, P = .013). This suggests that BNP and LVEF were correlated, and that the cardiac systolic function index also can be used in the reaction. The results of this study show that the cutoff value of BNP for acute left heart failure diagnosis was <55.50 ng/L based on maximize Youden index sensitivity, specific degree, AUC, and 95% CI which were 93.5%, 81.3%, 0.921, and 0.841 to 0.921, respectively. The result was higher than that of the Chinese guidelines for the diagnosis and treatment of heart failure in 2014, in which for BNP, the standard was <35.50 ng/L, showing a certain difference. This may be due to the correlation of BNP with age, gender, and history, causing the reasons for the gap.
β-EP is one of the main bodies of endogenous opioid peptides, is a kind of strong opioid agonist, mainly exists in the cranial nerve system, and is an important neuroendocrine factor of heart. In a state of emergency, the body releases a large amount of β-EP. In the stress state, this is released through the hypothalamus releasing factor, allowing the release of pituitary ACTH and β-EP. This increases the plasma concentration of β-EP to 5 to 6 times.[10–12] β-EP is the main junction with opioid receptors and is involved in the pathological processes of many diseases, such as pain, breathing, circulation, digestion, and the hypothalamus-pituitary-target gland function, which play an important role. Its action mechanism mainly includes: the inhibition of catecholamine (CA) and prostaglandin (PG) on the regulation of cardiovascular function, inhibiting myocardial contraction force, the expansion of the capillaries, combined with capillary permeability of the blood, and bleeding that causes blood pressure to drop and shock; allow β-EP release to inhibit the respiratory center, reduce medulla, aorta, aortic sinus chemoreceptor sensitivity to hypoxia and hypercapnia, respiratory frequency and lower tidal volume, lessen ventilatory response caused by CO2, oxygen and CO2 retention, leading to more β-EP released into the bloodstream, which is a vicious cycle, and increase in central inhibition; the role in brainstem reticular structure upward excited system and nonspecific thalamus cortex system, participate in the occurrence and development of brain dysfunction, and according to research, opioid receptors in the process of sensory afferent gate have an effect, which is caused by changes associated with EP.[13–15] In this experimental study, the plasma level of β-EP in patients with acute left heart failure was 394.06 ± 180.97 ng/L, which was higher than that in the control group (76.87 ± 57.21 ng/L) (t = 9.17, P = .019); and the difference was statistically significant. The plasma β-EP level in patients with acute left heart failure in the LVEF group 50% or higher was 178.41 ± 101.52 ng/L, which was significantly lower than that in the LVEF <50% group (344.16 ± 170.39 ng/L) (t = 9.42, P = .017); and β-EP and LVEF were negatively correlated (r = −0.635, P = .018). The difference was statistically significant. According to literature, the heart started after the acute myocardial ischemia injury mechanism of self-protection, the activation of the opioid system in the body, causing the release of endogenous opioid peptides in the body, making the plasma β-EP levels rise rapidly, inducing myocardial ischemia. Furthermore, β-EP increases the extent and the degree of myocardial ischemia, the myocardial necrosis area, cardiac function, etc. The experiment results show that β-EP was significantly higher in patients with acute left heart failure than in subjects of the control group, and LVEF was negatively correlated. The acute left heart failure diagnosis value of β-EP was <81.53 ng/L, which was based on the maximum Youden index of degree of sensitivity, specificity, AUC,, and 95% CI which were 80.5%, 78.6%, 0.697, and 0.505 to 0.697, respectively. β-EP has a certain diagnostic value for acute left heart failure.
The consideration of traditional diagnosis for acute left heart failure mode depends on medical history, physical examination, echocardiography, and blood gas analysis. However, these have been able to meet the needs of the existing clinical diagnosis model. The diagnosis and treatment of heart failure in 2014 guidelines suggest that for BNP in patients with acute left heart failure detection, echocardiography and blood gas analysis detection should be employed to improve the accuracy of acute left heart failure diagnosis, which is gradually becoming the clinical diagnosis mode at present.[16–20] This study revealed that a cutoff value of BNP for acute left heart failure was <55.50 ng/L, based on sensitivity, specific degree, AUC, and 95% CI were 93.5%, 81.3%, 0.921, and 0.841 to 0.921, respectively, which has a good diagnosis performance. Furthermore, this clinical study revealed that β-EP distribution and receptors in heart blood vessels, myocardial cell secretion also can synthesize β-EP and participates in the regulation of cardiovascular function. In addition, this study also examines the performance of β-EP for acute left heart failure diagnosis, and the cutoff value was <81.53 ng/L based on maximum Youden index sensitivity, specific degree, AUC and 95% CI which were 80.5%, 78.6%, 0.697, and 0.505 to 0.697, respectively. Furthermore, BNP has a certain gap in the early diagnosis of acute left heart failure. However, naloxone can reverse β-EP-mediated cardiopulmonary cerebral inhibition function. Hence, β-EP is expected to be used to monitor the efficacy of naloxone treatment. The level of BNP and β-EP is negatively correlated with LVEF in echocardiography indexes (r = −0.741, −0.635, P = .013, 0.018), and acute left heart failure patients with BNP and β-EP were 4 correlations (r = 0.895, P < .001). In combination of the BNP and β-EP for acute left heart failure diagnosis in maximum Youden index sensitivity, specific degree, AUC and 95% CI, the results were 94.1%, 83.5%, 0.604, 0.604 and 0.604.
Overall, plasma BNP and β-EP levels and echocardiographic heart failure correlation index has a certain relevance, which can be used for diagnosing patients with acute left heart failure and in evaluating the severity of cardiac function. These have certain advantages such as they are convenient and fast. When combining BNP and β-EP, the diagnostic efficiency of early acute left heart failure can be improved.
Footnotes
Abbreviations: β-EP = beta-endorphin, AHFPEF = acute heart failure with preserved ejection fraction, AHFREF = acute heart failure with reduced ejection fraction, AUC = area under the ROC curve, BNP = brain natriuretic peptid, CA = catecholamine, CI = confidence interval, EDTA = ethylamine tetraacetic acid, LVEF = left ventricular ejection fraction, PG = prostaglandin.
Funding: This work was financially supported by Emergency branch of Chinese Medical Theory Rui E (Ruiyi) of Emergency Medicine Research Fund (R2014005) and Fujian province health family planning personnel training the backbone of middle-aged and young items (2016-ZQN-41).
The authors have no conflicts of interest to disclose.
References
- [1].Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics 2012 update a report from the American Heart Association. Circulation 2012;125:e2–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Xiu LW, He KL, Li F. BNP application research in the identification of diastolic heart failure. Chin Med J 2010;33:328–30. [Google Scholar]
- [3].Zhang RR. Invasive mechanical ventilation on the breathing, circulation function of patients with severe acute left heart failure. Pract Med 2016;11:76–7. [Google Scholar]
- [4].Editorial Committee of Chinese Journal of Cardiology. Cardiovascular epidemiology branch of Chinese Medical Association, the Chinese magazine editorial board. Cardiovascular disease diagnosis and treatment of heart failure in China guide 2014. Chin J Cardiovasc 2014;42:98–122. [Google Scholar]
- [5].O’Connor CM, Abraham WT, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure(OPTIMIZE-HF). Am Heart J 2008;156:662–73. [DOI] [PubMed] [Google Scholar]
- [6].Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics-2011 update: a report from the American Heart Association. Circulation 2011;123:e18–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Storrow AB, Jenkins CA, Self WH, et al. The burden of acute heart failure on US Emergency Departments. JACC Heart Fail 2014;2:269–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].AbouEzzeddine OF, Wong YW, Mentz RJ, et al. Evaluation of novel metrics of symptom relief in acute heart failure: the Worst Symptom Score. J Card Fail 2016;22:853–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hu D, Liu Y, Tao H, et al. Clinical value of plasma B-type natriuretic peptide assay in pediatric pneumonia accompanied by heart failure. Exp Ther Med 2015;10:2175–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bitar Z, Maadarani O, Almerri K. Sonographic chest B-lines anticipate elevated B-type natriuretic peptide level, irrespective of ejection fraction. Ann Intensive Care 2015;5:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Abdeen Y, Sen P, Safdar S, et al. The usefulness of brain natriuretic peptide level in diagnosis and prognosis of patients admitted to critical care unit with shortness of breath. J Emerg Trauma Shock 2015;8:205–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Isenberg D, Appel GB, Contreras G, et al. Influence of race ethnicity on response to lupus nephritis treatment: the ALMS study. Rheumatology (Oxford) 2010;49:128–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Brar S, McAlister FA, Youngson E, et al. Do outcomes for patients with heart failure vary by emergency department volume? Circ Heart Fail 2013;6:1147–54. [DOI] [PubMed] [Google Scholar]
- [14].Temporelli PL, Scapellato F, Eleuteri E, et al. Doppler echocardiography in advanced systolic heart failure: a noninvasive alternative to Swan-Ganz catheter. Circ Heart Fail 2010;3:387–94. [DOI] [PubMed] [Google Scholar]
- [15].Nazerian P, Vanni S, Zanobetti M, et al. Diagnostic accuracy of emergency Doppler echocardiography for identification of acute left ventricular heart failure in patients with acute dyspnea: comparison with Boston criteria and N-terminal prohormone brain natriuretic peptide. Acad Emerg Med 2010;17:18–26. [DOI] [PubMed] [Google Scholar]
- [16].Sanders-van Wijk S, Maeder MT, Nietlispach F, et al. Long-term results of intensified, N-terminal-pro-B-type natriuretic peptide-guided versus symptom-guided treatment in elderly patients with heart failure five-year follow-up from TIME-CHF. Circ Heart Fail 2014;7:131–9. [DOI] [PubMed] [Google Scholar]
- [17].Adlbrecht C, Hülsmann M, Neuhold S, et al. Prognostic utility of the Seattle Heart Failure Score and amino terminal pro B-type natriuretic peptide in varying stages of systolic heart failure. J Heart Lung Transplant 2013;32:533–8. [DOI] [PubMed] [Google Scholar]
- [18].Berin R, Zafrir B, Salman N, et al. Single measurement of serum N-terminal pro-brain natriuretic peptide: the best predictor of long-term mortality in patients with chronic systolic heart failure. Eur J Intern Med 2014;25:458–62. [DOI] [PubMed] [Google Scholar]
- [19].Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147–239. [DOI] [PubMed] [Google Scholar]
- [20].Velibey Y, Golcuk Y, Golcuk B, et al. Determination of a predictive cutoff value of NT-proBNP testing for long-term survival in ED patients with acute heart failure. Am J Emerg Med 2013;31:1634–7. [DOI] [PubMed] [Google Scholar]


