Abstract
This study was conducted to compare the effects of whole brain radiotherapy (WBRT) and stereotactic radiotherapy (SRS) in treatment of brain metastasis.
A systematical retrieval in PubMed and Embase databases was performed for relative literatures on the effects of WBRT and SRS in treatment of brain metastasis. A Bayesian network meta-analysis was performed by using the ADDIS software. The effect sizes included odds ratio (OR) and 95% confidence interval (CI). A random effects model was used for the pooled analysis for all the outcome measures, including 1-year distant control rate, 1-year local control rate, 1-year survival rate, and complication. The consistency was tested by using node-splitting analysis and inconsistency standard deviation. The convergence was estimated according to the Brooks–Gelman–Rubin method.
A total of 12 literatures were included in this meta-analysis. WBRT + SRS showed higher 1-year distant control rate than SRS. WBRT + SRS was better for the 1-year local control rate than WBRT. SRS and WBRT + SRS had higher 1-year survival rate than the WBRT. In addition, there was no difference in complication among the three therapies.
Comprehensively, WBRT + SRS might be the choice of treatment for brain metastasis.
Keywords: Bayesian network meta-analysis, brain metastasis, stereotactic radiotherapy, whole brain radiotherapy
1. Introduction
Brain metastasis is a common adult intracranial tumor; the overall incidence rate is about 8.3/100,000.[1,2] In clinic, about 21% to 83% of advanced cancer patients develop brain metastases.[2,3] The most common source of brain metastases are lung cancer, breast cancer, malignant melanoma, and gastrointestinal malignant tumors. There has been an increasing trend of the brain metastasis incidence[4] with the progress of medicine, improvement of treatment program for malignant tumor, and longer survival time.
Radiotherapy is still the main method for brain metastasis management due to the limited number of patients with indication for surgery.[5] Recently, the whole brain radiotherapy (WBRT) dominates the main strategies for the treatment of brain metastases, its effect, however, is unsatisfied because of the short median survival time, radiation resistance in some patients, and frequent complications.[6,7] Stereotactic radiosurgery (SRS) technology emerged in this context, and its therapeutic efficacy has been reported to be satisfactory and the complications are fewer, which makes it favored by clinicians.[8,9] Nevertheless, whether there is a need to plus SRS after WBRT remains controversial.[6,10,11]
There have been several related meta-analyses comparing the effects of WBRT, SRS, and/or WBRT + SRS in patients with brain metastasis,[12–15] which only focused on the comparison of WBRT + SRS with WBRT alone or SRS alone. To the best of our knowledge, no literature reports a comprehensive comparison of these 3 methods. In addition, important studies on this aspect have been published since then and might change the derived conclusions in the previous meta-analyses.[16–19] Therefore, this paper comprehensively compared these 3 methods (WBRT + SRS vs WBRT vs SRS) for the treatment of brain metastases by a network meta-analysis, with an expectation to provide a reference for the choice of treatment.
2. Methods
Ethical approval was not necessary as this study was a meta-analysis for relevant literatures all of which were separately approved by the ethics committee or institutional review board.
2.1. Search strategy
Electrical databases, PubMed and Embase, were searched for the relevant English papers regarding WBRT and SRS for the management of brain metastases. The keywords for retrieval were (“Brain metastases” OR “Brain metastasis” OR “brain metastatic tumor” OR “intracranial metastasis” OR “metastatic tumor of brain” OR “metastatic encephaloma”), (“whole brain radiotherapy” OR WBRT OR “whole brain irradiation” OR “whole brain radiation therapy”), and (“Stereotactic radiosurgery” OR “stereotactic radiotherapy”).
2.2. Inclusion criteria
The literature were selected according to the following criteria: English literature on the effects of WBRT, SRS, and/or WBRT + SRS in the treatment of brain metastases; the participants must be adults; at least one of the following indexes were reported, 1-year local control rate, 1-year survival rate, 1-year distant control rate, and complication; summary, report, commentary, and correspondence were excluded.
2.3. Data extraction
The following data were extracted independently by 2 investigators, including the first author, the year of publication, the year of study, the area of study, the total number of patients in each group, demographic characteristics (age and sex), 1-year local control rate, 1-year survival rate, 1-year distant control rate, and complication. If a dispute arised during the data extraction process, a panel discussion was held to reach a consensus with a 3rd investigator.
2.4. Statistical analysis
All the statistical analyses were performed by using ADDIS software (version 1.16.5). ADDIS software is a nonprogramming software based on the Bayesian framework and the priori evaluation and data processing using the Markov chain Monte Carlo algorithms.[20,21] Parameters for the ADDIS software were as follows: number of chains, 4; tuning iterations, 20,000; simulation iterations, 50,000; thinning interval, 10; inference samples, 10,000; and variance scaling factor, 2.5. Then, 1-year local control rate, 1-year survival rate, 1-year distant control rate, and complication were analyzed by network meta-analysis.
The effect sizes were odds ratio (OR) and 95% confidence interval (CI). A random effects model was used for the tests of all data. The consistency test was performed using the inconsistency standard deviation (ISD) and the node-splitting analysis, which is an alternative method to assess inconsistency in network meta-analysis. If the P value of the node-splitting analysis more than 0.05, a consistency model was used, otherwise, the nonconsistency model was used.[22] Similarly, if the range of 95% CI of ISD includes, the consistency model was used otherwise the inconsistency model was used. For the closed-loop index, both node-splitting analysis and ISD were used to judge the consistency, while, for the open-loop indicators, ISD was used to test the consistency. The convergence of the model was determined by the potential scale reduction factor (PSRF) of the Brooks–Gelman–Rubin method[23]; PSRF closer to 1 indicated the better convergence; generally, PSRF less than 1.2 was acceptable.
3. Results
3.1. Literature selection
Literature search and screening process are shown in Fig. 1. With the predeveloped search strategy, 1388 iterature were retrieved from PubMed and Embase database. After removing the duplicates, 815 articles remained. By browsing the titles and abstracts, 689 articles were found to be incompatible with the inclusion criteria. Further, 114 articles were excluded after reading the full text. Finally, 12 articles were included.[16–19,24–31] The eligible studies were published from 1999 to 2016; the study area included Germany, Japan, the United States, and other countries or regions. There was no statistically difference in demographics characteristics (Table 1).
Figure 1.
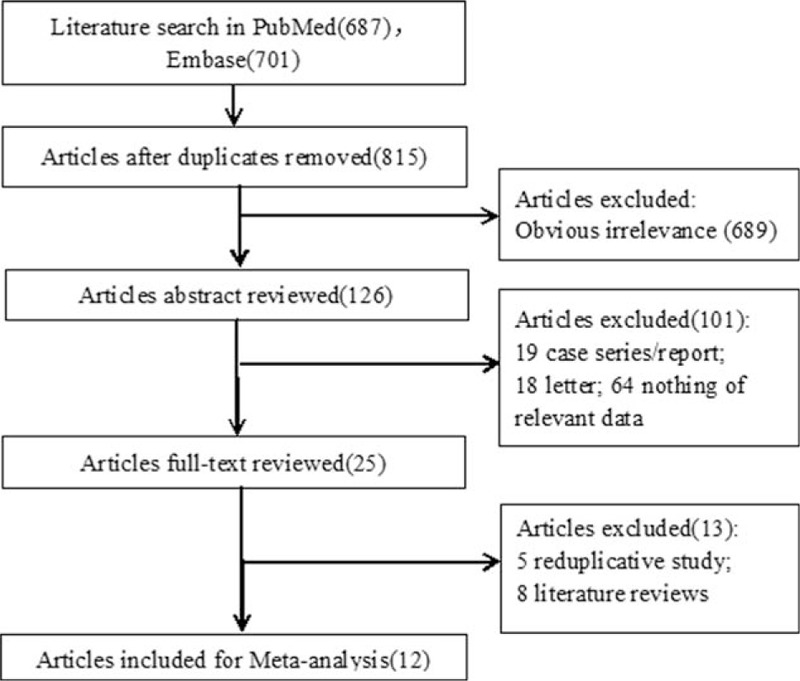
Flow chart for literature search and study selection. SRS = stereotactic radiosurgery, WBRT = whole-brain radiation therapy.
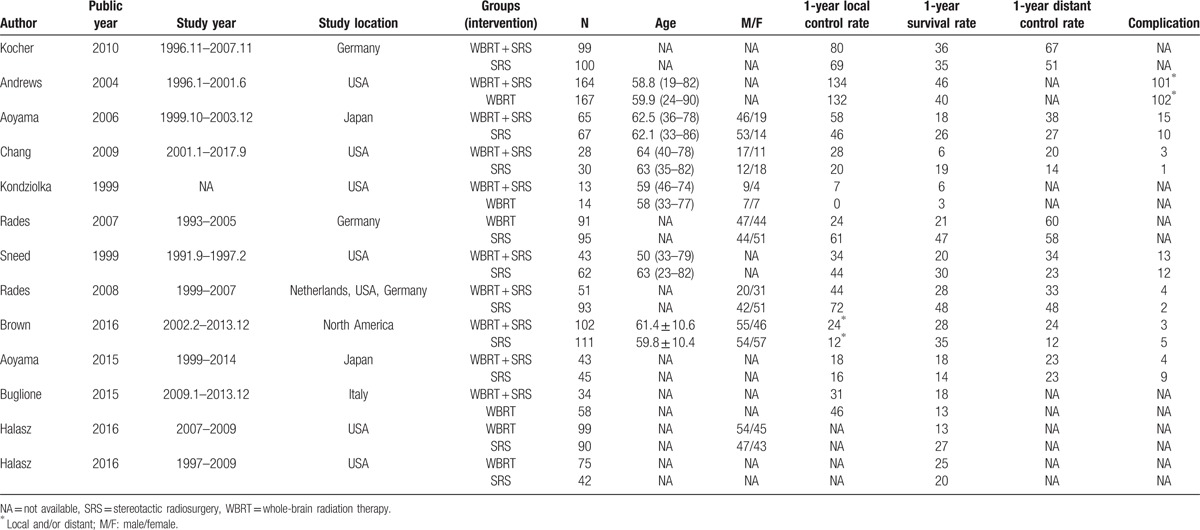
Table 1.
Characteristics of the included literature.
3.2. Network meta-analysis for the 1-year distant control rate
For 1-year distant control rate, the results of the ISD were OR = 0.91, 95% CI: 0.04 to 1.76. All the PSRFs were in the range of 1.00 to 1.01, which proved that the model was convergent and the result was stable. So, the consistency model was adopted. Figure 2A indicates that WBRT + SRS has the highest probability to rank 1 compared with WBRT or SRS alone. But on the whole there was no statistically significant difference between WBRT + SRS and WBRT (OR = 0.54, 95% CI: 0.14–1.92, Table 2).
Figure 2.
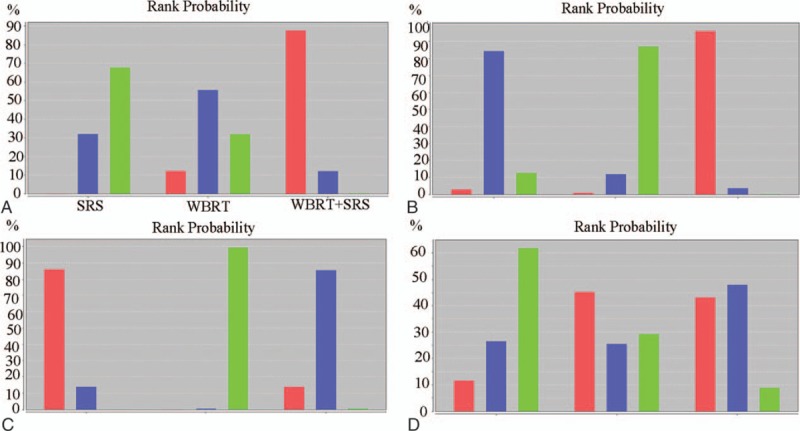
Rank probability diagram of the 1-year distant control rate (A), 1-year local control rate (B), 1-year survival rate (C), and complication (D).
Table 2.
Results for the network meta-analysis, OR (95%CI).
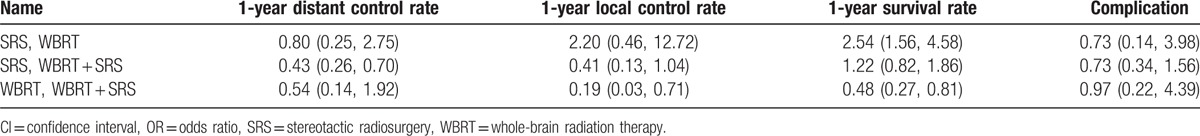
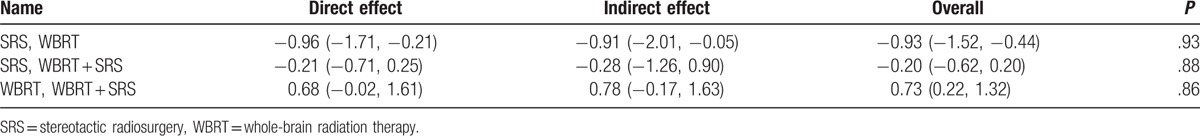
3.3. Network meta-analysis for the 1-year local control rate
For 1-year local control rate, the consistency test was analyzed by using the ISD. The results were: OR = 1.60, 95% CI: 0.07 to 3.40, P > .05 (Table 3). The PSRFs were between 1.00 and 1.01, which proved that the model converged completely, the effect of iteration was very good and the result was stable, so the consistency model was adopted. Similar with Fig. 2A, B shows that WBRT + SRS has the highest probability to rank 1 compared with WBRT or SRS alone. But on the whole there was no statistically significant difference between WBRT + SRS and SRS (OR = 0.41, 95% CI: 0.13–1.04, Table 2).
Table 3.
Node-splitting analysis of the 1-year local control rate.
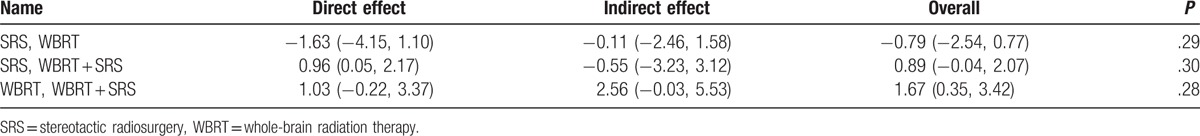
3.4. Network meta-analysis for the 1-year survival rate
The insistency of studies for 1-year survival rate was analyzed by using the method of node-splitting analysis (P > .05, Table 4) and ISD (ISD: OR = 0.59; 95% CI: 0.02–1.68). All the PSRFs are in the range of 1.00 to 1.01. It proved that the model converges completely, the effect of iteration is very good, and the result is stable, so the consistency model is adopted. As shown in Fig. 2C, SRS has the highest probability to rank 1 in the 1-year survival rates, but on the whole there was no statistically significant difference between WBRT + SRS and SRS (OR = 1.22, 95% CI: 0.82–7.189, Table 2).
Table 4.
Node-splitting analysis of the 1-year survival rate.
3.5. Network meta-analysis for the complication
Consistency of studies for complication was noted according to the results of ISD (OR = 0.63, 95% CI: 0.03–1.23). All PSRFs between 1.00 and 1.01, indicating the convergence of the model was complete, so the consistency model was adopted. From Fig. 2D for complication, the difference among 3 groups was not statistically significant (P > .05, Table 2).
4. Discussion
Compared with the previous reports of meta-analyses,[12–15] this study firstly used the network meta-analysis to comprehensively estimate the effects of WBRT, SRS, and WBRT + SRS for the treatment of brain metastasis. On the whole, WBRT + SRS should be the choice of treatment.
Controversial conclusions exist among different studies even among the reports of meta-analyses. Lv et al[15] evaluated the effects of WBRT with or without SRS and found that WBRT + SRS improved local tumor control rate and 1-year survival rate. Duan et al[12] compared the SRS with WBRT or without WBRT and found that SRS + WBRT has advantages in local recurrence and new brain metastasis rates, but SRS alone is associated with better neurological function. Tsao et al[13] respectively performed these 2 comparisons and concluded that although additional WBRT improves distant control and local control, SRS alone should be considered a routine treatment option due to favorable neurocognitive outcomes and less risk of late side effects. Except the studies those have been included in the previous studies, our study also included several new reported studies[16–19] which have been published during 2015 to 2016. Our study indicated that WBRT + SRS had higher 1-year distant control rate than SRS and higher 1-year local control rate than WBRT, as well as considerable 1-year survival rate and complications with SRS. Thus, the combined therapy should be recommended.
However, due to the limitations of the present study, the conclusion should be used critically. The inadequacies of this study included: covariates were not corrected because of the incomplete data in some studies; as confounding factors they may have a potential influence on the results of the meta-analysis; however, further subgroup analysis was not conducted; and although the ADDIS software is easy to use, it can be constrained by the fact that it cannot be programmed freely. For example, a random effects model can only be reported when estimating the effect size, which may be conservative in estimating our results.
In conclusion, WBRT + SRS may be a better method for the treatment of brain metastasis according to the comprehensive evaluation in this network meta-analysis.
Footnotes
Abbreviations: CI = confidence interval, ISD = inconsistency standard deviation, MCMC = Markov chain Monte Carlo, PSRF = potential scale reduction factor, SRS = stereotactic radiotherapy, WBRT = whole brain radiotherapy.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Barnholtz-Sloan JS, Sloan AE, Davis FG, et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol Off J Am Soc Clin Oncol 2004;22:2865–72. [DOI] [PubMed] [Google Scholar]
- [2].Wiley, Suki D. Sawaya R. Intracranial Metastases: Current Management Strategies. The Epidemiology of Brain Metastasis 2008;20–34. [Google Scholar]
- [3].Walker AE, Robins M, Weinfeld FD. Epidemiology of brain tumors: the national survey of intracranial neoplasms. Neurology 1985;35:219–26. [DOI] [PubMed] [Google Scholar]
- [4].Shao YY, Lu LC, Cheng AL, et al. Increasing incidence of brain metastasis in patients with advanced hepatocellular carcinoma in the era of antiangiogenic targeted therapy. Oncologist 2011;16:82–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lindner C, Schackert G. Treatment of multiple brain metastases: is there still an indication for surgery? Kongress Der Deutschen Gesellschaft Für Chirurgie; Meeting Abstract 2012. http://www.egms.de/static/en/meetings/dgch2012/12dgch238.shtml. [Google Scholar]
- [6].Park E, Gutin PH, Phillips TL. Radiosurgery for brain metastases: is whole brain radiotherapy necessary? Int J Radiat Oncol Biol Phys 1999;43:549–58. [DOI] [PubMed] [Google Scholar]
- [7].Abe E, Aoyama H. The role of whole brain radiation therapy for the management of brain metastases in the era of stereotactic radiosurgery. Curr Oncol Rep 2012;14:79–84. [DOI] [PubMed] [Google Scholar]
- [8].Breneman JC, Warnick RE, Albright RE, et al. Stereotactic radiosurgery for the treatment of brain metastases. Cancer 1997;79:551–7. [DOI] [PubMed] [Google Scholar]
- [9].Linskey ME, Andrews DW, Asher AL. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Barton R. Inoperable brain metastases from non-small cell lung cancer: what part does whole brain radiotherapy play in standard treatment? Thorax 2008;63:1–2. [DOI] [PubMed] [Google Scholar]
- [11].Soon Y, Tham I, Lim KH, et al. The benefits and side effects of adding upfront whole brain radiotherapy to surgery or radiosurgery for treatment of brain metastases. John Wiley & Sons Ltd for the Cochrane Collaboration, 2014. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0063404/. [Google Scholar]
- [12].Duan L, Zeng R, Yang KH, et al. Whole brain radiotherapy combined with stereotactic radiotherapy versus stereotactic radiotherapy alone for brain metastases: a meta-analysis. Asian Pac J Cancer Prev 2014;15:911–5. [DOI] [PubMed] [Google Scholar]
- [13].Tsao M, Xu W, Sahgal A. A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer 2012;118:2486–93. [DOI] [PubMed] [Google Scholar]
- [14].Soon YY, Tham IWK, Lim KHC, et al. Addition of upfront whole-brain radiotherapy to surgery or stereotactic radiosurgery versus surgery or stereotactic radiosurgery alone for treatment of brain metastases: a systematic review and meta-analysis. J Clin Oncol 2012;30:2016.22508817 [Google Scholar]
- [15].Lv DL, Hu ZT, Wang C, et al. Efficacy comparison of whole brain radiotherapy alone vs in combination with stereotactic radiotherapy for the treatment of brain metastases: a meta-analysis. Med J Chin Peoples Liberation Army 2012;37:559–62. [Google Scholar]
- [16].Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases. JAMA 2016;316:401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Buglione M, Pedretti S, Gipponi S, et al. The treatment of patients with 1-3 brain metastases: is there a place for whole brain radiotherapy alone, yet? A retrospective analysis. Radiol Med 2015;120:1146–52. [DOI] [PubMed] [Google Scholar]
- [18].Halasz LM, Uno H, Hughes M, et al. Comparative effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for patients with brain metastases from breast or non-small cell lung cancer. Cancer 2016;122:2091–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Aoyama H, Tago M, Shirato H. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 randomized clinical trial. JAMA Oncol 2015;1:457–64. [DOI] [PubMed] [Google Scholar]
- [20].University of Groningen, Research Institute SOM (Systems, Organisations and Management), Hillege H, de Brock B, van Valkenhoef G, et al. ADDIS: An Automated Way to Do Network Meta-Analysis. 2012;12007-Other. [Google Scholar]
- [21].van Valkenhoef G, Tervonen T, Zwinkels T, et al. ADDIS: a decision support system for evidence-based medicine. Decis Support Syst 2013;55:459–75. [Google Scholar]
- [22].Dias S, Welton NJ, Caldwell DM, et al. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932–44. [DOI] [PubMed] [Google Scholar]
- [23].Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat 1998;7:434–55. [Google Scholar]
- [24].Aoyama H, Tago M, Shirato H, et al. Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 randomized clinical trial. JAMA Oncol 2015;1:457–64. [DOI] [PubMed] [Google Scholar]
- [25].Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 2009;10:1037–44. [DOI] [PubMed] [Google Scholar]
- [26].Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 2004;363:1665–72. [DOI] [PubMed] [Google Scholar]
- [27].Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 2010;29:134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kondziolka D, Patel A, Lunsford LD, et al. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 1999;45:427–34. [DOI] [PubMed] [Google Scholar]
- [29].Rades D, Kueter JD, Hornung D, et al. Comparison of stereotactic radiosurgery (SRS) alone and whole brain radiotherapy (WBRT) plus a stereotactic boost (WBRT+SRS) for one to three brain metastases. Strahlenther Onkol 2008;184:655–62. [DOI] [PubMed] [Google Scholar]
- [30].Rades D, Pluemer A, Veninga T, et al. Whole-brain radiotherapy versus stereotactic radiosurgery for patients in recursive partitioning analysis classes 1 and 2 with 1 to 3 brain metastases. Cancer 2007;110:2285–92. [DOI] [PubMed] [Google Scholar]
- [31].Sneed PK, Lamborn KR, Forstner JM, et al. Radiosurgery for brain metastases: is whole brain radiotherapy necessary? Int J Radiat Oncol Biol Phys 1999;43:549–58. [DOI] [PubMed] [Google Scholar]


