Abstract
This study aimed to investigate the association between the prevalence of peptic ulcer disease (PUD) and mental health problems, such as severe stress, depressive mood, and suicidal ideation.
The population-based cross-sectional study was comprised of 14,266 subjects participating in the fourth annual Korea National Health and Nutrition Examination survey from 2007 to 2009. The participants were divided into 2 groups according to the self-reported questionnaires: the PUD group and the non-PUD group. The association between PUD and mental health problems, such as severe stress, depressed mood, suicidal ideation, and psychological counseling history, were evaluated by using multivariate analysis and logistic regression.
Among the 14,266 participants over 19-years old, 813 participants (5.6%) had PUD. Compared to the non-PUD group (n = 13,453), the PUD group had a significantly higher percentage of males, current smokers, and heavy drinkers, lower education status, lower income, and greater presence of diabetes mellitus, hypertension, metabolic syndrome and mental health problems, including severe stress, depressed mood, suicidal ideation, and psychological counseling history. After adjustment for lifestyle and medical and environmental factors, mental health problems were found to be associated with a significantly higher risk for PUD.
Psychological problems, such as severe stress, depressed mood, suicidal ideation, and psychological counseling, were associated with PUD prevalence.
Keywords: depressed mood, mental health, peptic ulcer disease, severe stress, suicidal ideation
1. Introduction
Peptic ulcer disease (PUD) is defined as ulcerations and erosions that occur in the stomach and duodenum.[1] Because of the disruption of the normal mucosal defense, PUD can provoke many symptoms and signs such as dyspepsia, abdominal pain, and hemorrhage.[1–3] The complex and multifactorial pathogenesis of PUD has been studied over several decades and has been found to involve proteolytic pepsin, which plays a key role in the patho-mechanism of PUD and is mainly activated by gastric acid. Helicobacter pylori, NSAIDs, neurotransmitters, and corticosteroids are also known to influence the release of pepsin and gastric acid.[4] Among environmental factors, smoking, excessive alcohol use, and drug use are considered risk factors for PUD; however, none of them have been identified as an individual ulcerogenic agent.[5]
Emotional stress and psychological factors are frequently identified as important contributors to PUD.[6,7] Since the mid-20th century, stress has been considered as the main cause of PUD.[8] Several studies suggested that psychological stress may play a role in the onset and course of PUD.[9] Studies have also shown that subjects with anxiety disorders,[10,11] personality disorders,[12] and panic disorders[11] are more likely to have had PUD. Individuals with neuroticism[13] or with a history of childhood abuse[14] are also more likely to have PUD. The detrimental effect of stress on PUD was shown in a Japanese study that demonstrated a rise in bleeding gastric ulcers in elderly people after a catastrophic earthquake in Japan.[15] Recently, Levenstein et al reported that psychological stress increased the incidence of peptic ulcers. The authors revealed that stress had similar effects on ulcers associated with H pylori infection as well as those unrelated to either H pylori or the use of nonsteroidal anti-inflammatory drugs.[16] However, the relationship between psychological problems and PUD is still controversial. In contrast to previous studies, Lee et al[17] reported that PUD was not related to stress and depression. The authors revealed that subjects with depression had a lower risk for PUD compared to a control group.[17]
Multiple social, psychological, and biological factors contribute to mental health problems. Among mental health problems, severe stress, depressive mood, and suicidal ideation are considered particularly serious problems for contemporaries who need to adapt to rapidly changing circumstances.
The aim of this study was to investigate the association between the prevalence of PUD and mental health problems, such as stress, depressive mood, suicidal ideation, and psychological counseling history.
2. Materials and methods
2.1. Study population and data collection
In this study, population-based data were obtained from a representative sample between 2007 and 2009, gathered by the Division of Chronic Disease Surveillance, a division of the Korea Centers for Disease Control and Prevention. The Fourth Korean National Health and Nutrition Examination Survey (KNHANES-IV) was conducted after approval from the Institutional Review Board of the Korea Centers for Disease Control and Prevention (KNHANES-IV, IRB No. 2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C). The study design followed the tenets of the Declaration of Helsinki for biomedical research. The design required a weighting scheme to accurately estimate the health status of the Korean population.
The study was conducted using a rolling sampling design that involved a complex, stratified, multistage, probability cluster survey of a representative sample of the civilian population of South Korea. A total of 192 sampling units were randomly selected from primary sampling units encompassing the target population. Each sampling unit contained 20 households; 3800 households were surveyed in 1 year. According to the National Health Enhancement Act, subjects had the right to refuse participation. All who agreed to take part provided written informed consent. The Korea Centers for Disease Control and Prevention obtained consent from the participants to draw blood during the health interview survey and use the samples for further research. The KNHANES-IV included 24,871 participants who agreed to participate in the survey, 78.4% of the selected 31,705 subjects. The survey consisted of 3 components: a health interview, a nutrition interview, and health examination. All questionnaires were administered by either physicians or trained interviewers in person at participant homes.
2.2. Anthropometry and laboratory measurements
Questionnaires were used to collect data on smoking status, alcohol consumption, regular exercise, educational status, and medical history such as diabetes and hypertension. Smoking status was categorized into 2 groups: current smokers and nonsmokers. The amount of pure alcohol consumed (in grams per day) was calculated using the average number of alcoholic beverages consumed by the respondents and the frequency of alcohol consumption. Respondents who drank >30 g/d were classified as heavy drinkers. Regular exercise was defined as strenuous physical activity performed for at least 20 minutes at a time at least 3 times a week. The education level was classified as high if the respondent had completed high school.
Subject anthropometric measurements were obtained by a specially trained examiner. Waist circumference was measured to the nearest 0.1 cm in a horizontal plane at the level of the midpoint between the iliac crest and the costal margin at the end of a normal expiration. The body mass index (BMI) was calculated as an individual's weight in kilograms divided by the square of the individual's height in meters. Systemic hypertension was defined as systolic blood pressure >160 mm Hg and/or a diastolic blood pressure > 90 mm Hg or current use of anti-hypertensive drugs. Diabetes was defined as a fasting blood glucose level of > 126 mg/dL or current use of antidiabetic medication. Metabolic syndrome was defined as the presence of any 3 of the following 5 risk factors: (1) large waist circumference (≥90 cm for males, ≥80 cm for females); (2) elevated triglycerides (≥150 mg/dL) or drug treatment for elevated triglycerides; (3) reduced high-density lipoprotein cholesterol (<40 mg/dL for males, <50 mg/dL for females) or drug treatment for reduced high-density lipoprotein cholesterol; (4) elevated blood pressure (systolic ≥130 and/or diastolic ≥85 mm Hg) or antihypertensive drug treatment; and (5) elevated fasting glucose (≥100 mg/dL) or drug treatment.
2.3. Definitions of peptic ulcer disease and mental health problems
PUD was defined as self-reported questionnaires. Participants who answered “yes” to the questions, “Regardless of the time of diagnosis, have you been diagnosed as PUD by physician?” were categorized as the PUD group. Psychological stress was evaluated from responses indicative of cognitive complaints collected with a questionnaire using a 4-point Likert scale as follows: 1 (very severe), 2 (severe), 3 (moderate), and 4 (low). Meaningful cognition of stress was defined as psychological stress rated as more than severe (scale 1 or 2). Participants who answered “yes” to the question, “During the past year, has your daily life been burdened by feelings of hopelessness or dejection for more than 2 continuous weeks?” were categorized as having depressed mood. Suicidal ideation was defined as thoughts of committing suicide during the past year. The subjects were also asked if they received psychological counseling more than once during the past year.
2.4. Statistical analyses
Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC) and SUDAAN release 10.1 (Research Triangle Institute, Research Triangle Park, NC), a software package that incorporates sample weights and adjusts analyses for the complex sample design of the survey.
The demographic characteristics of the study participants were expressed as either means ± standard error (SE) or percentage ± SE, as appropriate, for all participants. The survey weights were taken into account to obtain the SEs of prevalence. Data were analyzed with a Student's t test or χ2 test, as appropriate, using the SURVEYMEANS or SURVEYFREQ procedures in SAS to reflect the study weights, respectively. Multivariate adjusted logistic regression analysis was conducted to examine the odds ratios (OR) and 95% confidence intervals (CI) for the association between PUD and psychological stress perception, depressed mood, suicidal thoughts, and psychological counseling. Age, education, smoking history, alcohol consumption, BMI, waist circumference, hypertension, and diabetes were used as covariates for calculating adjusted ORs. For logistic regression analyses, the SURVEYLOGISTIC procedure in SAS was used. All reported P values were 2 tailed and P < .05 was considered statistically significant.
3. Results
3.1. Participant characteristics
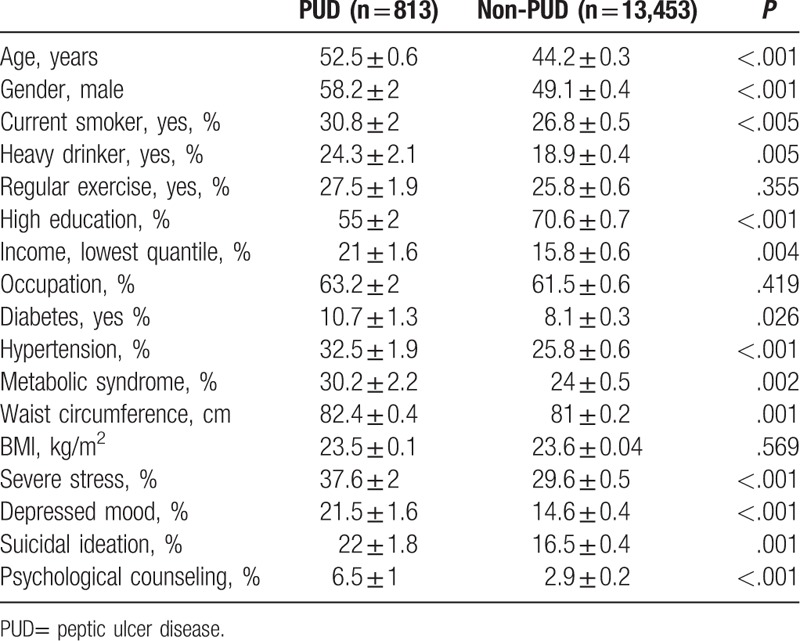
Of the 24,871 KNHANES-IV participants, 14,266 subjects over 19 years of age responded to the question on PUD history and were included in this study. Subjects with missing data for variables in the analysis were excluded. Among the total 14,266 participants, 813 subjects were reported to be diagnosed with PUD, with a prevalence of 5.7%. Table 1 shows subjects’ basic characteristics. The PUD group was significantly older and more male-predominant than the non-PUD group. Subjects with PUD had a higher habitual history of current smoking and heavy drinking, and were also more likely to have other comorbidities such as diabetes, hypertension, and metabolic syndrome than non-ulcer subjects. Education level and income in the lowest quantile were also significantly different between subjects with or without PUD (Table 1).
Table 1.
Comparison of basic characteristics in subjects with or without PUD (total n = 14,266).
3.2. Associations between PUD and mental health problems
We also evaluated the association between PUD and psychological problems. Subjects with PUD had a significantly higher risk of stress (37.6 ± 2.0% vs 29.6 ± 0.5%, P < .0001), depressed mood (21.5 ± 1.6% vs 14.6 ± 0.4%, P < .0001), and suicidal ideation (22.0 ± 1.8% vs 16.5 ± 0.4%, P = .0005) compared to those without PUD. The PUD group also had significantly more frequent visits to physicians for psychological counseling (6.5 ± 1.0% vs 2.9 ± 0.2%, P < .0001) compared to the non-PUD group.
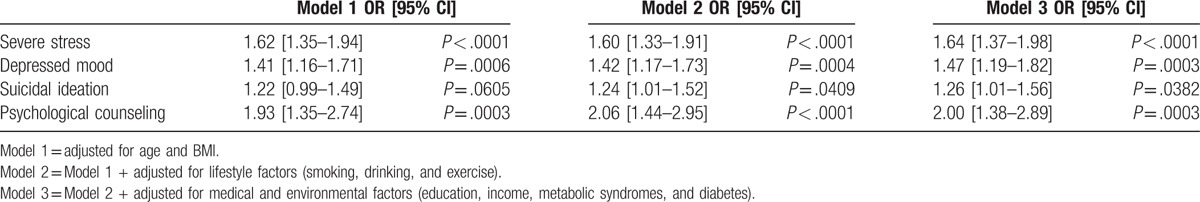
To adjust for confounding factors based on the association between PUD and factors related to psychological problems, multivariate logistic regression tests were performed. We examined 3 models adjusted for different variables—Model 1: age and BMI, Model 2: Model 1 + lifestyle factors (smoking, drinking, and exercise), Model 3: Model 2 + medical and environmental factors (education, household income, metabolic syndrome, and diabetes). Based on the results of multivariate logistic regression analysis, psychological problems had significantly increased ORs for PUD (severe stress, OR = 1.62 [1.35–1.94] in Model 1, 1.64 [1.37–1.98] in Model 2, 1.64 [1.37–1.98] in Model 3; depression, OR = 1.41 [1.16–1.71] in Model 1, 1.42 [1.17–1.73] in Model 2, and 1.47 [1.19–1.82] in Model 3; suicidal ideation, OR = 1.22 [0.99–1.49] in Model 1, 1.24 [1.01–1.52] in Model 2, and 1.26 [1.01–1.56] in Model 3; and psychological counseling, OR = 1.93 [1.35–2.74] in Model 1, 2.06 [1.44–2.95] in Model 2, and 2.00 [1.38–2.89] in Model 3, Table 2).
Table 2.
Association between mental health problems and PUD by multivariate logistic regression analysis.
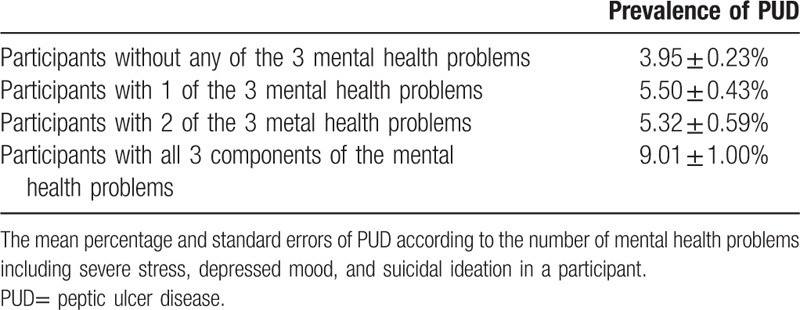
The relationship between PUD prevalence and the number of relevant mental health components, including severe stress, depressed symptoms, and suicidal thoughts, is presented in Table 3. Higher psychological symptom number predicted PUD.
Table 3.
Relationship between the prevalence of PUD and the number of psychological problems.
4. Discussion
In this population-based study, we found a close relationship between PUD and mental health problems such as severe stress, depressive mood, and suicidal ideation. The subjects with PUD were more likely to have psychological problems. Psychological problems were significantly associated with the history of PUD even after adjusting for other well-known risk factors such as age, gender, smoking, drinking, low socio-economic status, and metabolic diseases.
In previous meta-analyses, the 3 major risk factors for PUD were H pylori infection (OR = 3.3), NSAID use (OR = 3.7), and smoking (OR = 1.99), followed by former smoking (OR = 1.55), former alcohol use (OR = 1.29), and diabetes (OR = 1.13).[18,19] In a recent study, Levenstein et al[16] reported that stress had similar effects on ulcers associated with H pylori infection. These results were consistent with the present study; the ORs for mental health problems (1.64 for severe stress, 1.47 for depressed mood, 1.26 for suicidal ideation, and 2.00 for psychological counseling) in the present study were comparable to the well-known risk factors identified in the previous study.[1]
Interestingly, we found that the more psychological problems the subjects had, the more likely they were to have PUD (Table 3). The prevalence of PUD increased with an increase in the number of mental health problem components. Previous studies found that there was a relationship between PUD and psychological problems; however, this study specifically identified significant association between PUD and mental health problems including severe stress, depressive mood, and suicidal ideation, and further clarified that an increased number of mental health problems in a subject were significantly associated with prevalence of PUD. Severe stress, depressive mood, and suicidal ideation are strongly correlated with each other and are not regarded as separate components of mental health problems. A possible explanation for this finding is that subjects with more mental health problems are more likely to have comorbid dependence on nicotine and alcohol, which are well-known risk factors for PUD.
Possible pathologic mechanisms for the development of PUD due to mental health problems have been suggested in several previous studies. First, the GI system and brain are closely connected via the autonomic nervous system, namely the brain-gut axis.[20–22] During stressful or depressed conditions, neurologic function might be disturbed which could increase the secretion of pepsin and gastric acid[4] and induce mucosal injury. Second, psychological problems may alter cortisol secretion by influencing the hypothalamic-pituitary-adrenal axis.[23] During stressful conditions, the cortisol level is usually elevated which may lead to an increase in gastric acid secretion levels.[4] The increased level of cortisol and gastric acid may hamper the normal inflammatory response in the GI tract. Third, depressed individuals may be less likely to receive treatment for mild dyspepsia caused by gastritis or duodenitis, so their condition could progress to PUD more readily. Fourth, smoking and alcohol use are more common in people with mental health problems.[1,21,24] Smoking promotes the production of free radicals and induces vasoconstrictors to affect mucosal blood flow. Alcohol also disturbs the mucosal barrier by causing the release of vasoactive and inflammatory molecules. However, our results revealed that psychological problems were associated with the development of PUD after adjusting for the effects of smoking and alcohol.
This population-based study has several limitations. First, this study design is cross-sectional and therefore cannot support allegations of causality. It was not possible to determine if PUD was a cause or consequence of psychological problems. Also, the medication and family history of PUD in each subject were not available in the dataset. We were unable to examine the effects of GI medications such as a proton pump inhibitors or H2-blockers. Second, there is a high prevalence of H pylori infection in Korea; however, testing for H pylori was not included in this study. Therefore, correlations or confounding due to H pylori infection cannot be ruled out. Third, although it typically requires an endoscopic confirmation, PUD was determined based on a previous diagnosis by a physician in this study. The incidence of endoscopically confirmed PUD in Korea has been reported to be 2.45–7.0%[25–27] which was consistent with our results. Also, as the lifetime screening rate for stomach cancer during the study period was about 65%, we believe that the majority of subjects in this study had been diagnosed with PUD by endoscopy.[28] Upper gastrointestinal endoscopy is readily available in Korea, either provided at a low cost or free of charge in the biennial governmental health examination or yearly employee health examination. Therefore, self-reported PUD diagnosed by a physician is considered credible data.
Despite these limitations, the present study has a major strength since it is a population based-study with a sample that is representative of the entire Korean population. Therefore, the results from this study can be applied to disease and mental conditions in all Koreans. This study also included subjects who reported whether they felt stress or were depressed in everyday life, and not only patients with clinician-diagnosed mental illness. Therefore, this study included a broad range of individuals who had mental health problems but were not necessarily visiting psychological clinics.
In summary, mental health problems such as stress, depression, and suicidal ideation were closely correlated with PUD. These psychological problems were found to be associated with PUD. Individuals under severe stress or with a depressed mood might be more likely to develop PUD. Therefore, physicians should pay close attention to the close relationship between the prevalence of PUD and psychological problems.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence intervals, KNHANES = Korean National Health and Nutrition Examination Survey, NSAIDs = nonsteroidal anti-inflammatory drugs, OR = odds ratio, PUD= peptic ulcer disease, SE = standard error.
YBL and JHY equally contributed to this study.
Authorship: CHS designed the research; CHH, JBS, KHK, KSW, and KSS performed the research; YJ and LYB analyzed the data; YJ, LYB, and CHS wrote the paper. All authors contributed to this work with conception, drafting, revision, and approval of final version of the manuscript.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Najm WI. Peptic ulcer disease. Prim Care 2011;38:383–94. vii. [DOI] [PubMed] [Google Scholar]
- [2].Ford AC, Moayyedi P. Dyspepsia. BMJ 2013;347:f5059–15059. [DOI] [PubMed] [Google Scholar]
- [3].Axon A. Helicobacter pylori and public health. Helicobacter 2014;19(suppl 1):68–73. [DOI] [PubMed] [Google Scholar]
- [4].Di Mario F, Goni E. Gastric acid secretion: changes during a century. Best Pract Res Clin Gastroenterol 2014;28:953–65. [DOI] [PubMed] [Google Scholar]
- [5].Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet 2009;374:1449–61. [DOI] [PubMed] [Google Scholar]
- [6].Peters MN, Richardson CT. Stressful life events, acid hypersecretion, and ulcer disease. Gastroenterology 1983;84:114–9. [PubMed] [Google Scholar]
- [7].Medalie JH, Stange KC, Zyzanski SJ, et al. The importance of biopsychosocial factors in the development of duodenal ulcer in a cohort of middle-aged men. Am J Epidemiol 1992;136:1280–7. [DOI] [PubMed] [Google Scholar]
- [8].Alp MH, Court JH, Grant AK. Personality pattern and emotional stress in the genesis of gastric ulcer. Gut 1970;11:773–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jones MP. The role of psychosocial factors in peptic ulcer disease: beyond Helicobacter pylori and NSAIDs. J Psychosom Res 2006;60:407–12. [DOI] [PubMed] [Google Scholar]
- [10].Rogers MP, White K, Warshaw MG, et al. Prevalence of medical illness in patients with anxiety disorders. Int J Psychiatry Med 1994;24:83–96. [DOI] [PubMed] [Google Scholar]
- [11].Goodwin RD, Talley NJ, Hotopf M, et al. A link between physician-diagnosed ulcer and anxiety disorders among adults. Ann Epidemiol 2013;23:189–92. [DOI] [PubMed] [Google Scholar]
- [12].Schuster JP, Limosin F, Levenstein S, et al. Association between peptic ulcer and personality disorders in a nationally representative US sample. Psychosom Med 2010;72:941–6. [DOI] [PubMed] [Google Scholar]
- [13].Goodwin RD, Cox BJ, Clara I. Neuroticism and physical disorders among adults in the community: results from the National Comorbidity Survey. J Behav Med 2006;29:229–38. [DOI] [PubMed] [Google Scholar]
- [14].Fuller-Thomson E, Bottoms J, Brennenstuhl S, et al. Is childhood physical abuse associated with peptic ulcer disease? Findings from a population-based study. J Interpers Violence 2011;26:3225–47. [DOI] [PubMed] [Google Scholar]
- [15].Aoyama N, Kinoshita Y, Fujimoto S, et al. Peptic ulcers after the Hanshin-Awaji earthquake: increased incidence of bleeding gastric ulcers. Am J Gastroenterol 1998;93:311–6. [DOI] [PubMed] [Google Scholar]
- [16].Levenstein S, Rosenstock S, Jacobsen RK, et al. Psychological stress increases risk for peptic ulcer, regardless of Helicobacter pylori infection or use of nonsteroidal anti-inflammatory drugs. Clin Gastroenterol Hepatol 2015;13:498–506. e491. [DOI] [PubMed] [Google Scholar]
- [17].Lee SP, Sung IK, Kim JH, et al. The effect of emotional stress and depression on the prevalence of digestive diseases. J Neurogastroenterol Motil 2015;21:273–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Garrow D, Delegge MH. Risk factors for gastrointestinal ulcer disease in the US population. Dig Dis Sci 2010;55:66–72. [DOI] [PubMed] [Google Scholar]
- [19].Kurata JH, Nogawa AN, Noritake D. NSAIDs increase risk of gastrointestinal bleeding in primary care patients with dyspepsia. J Fam Pract 1997;45:227–35. [PubMed] [Google Scholar]
- [20].Overmier JB, Murison R. Restoring psychology's role in peptic ulcer. Appl Psychol Health Well Being 2013;5:5–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Nardone G, Compare D. The psyche and gastric functions. Dig Dis 2014;32:206–12. [DOI] [PubMed] [Google Scholar]
- [22].Gazouli M, Wouters MM, Kapur-Pojskic L, et al. Lessons learned—resolving the enigma of genetic factors in IBS. Nat Rev Gastroenterol Hepatol 2016;13:77–87. [DOI] [PubMed] [Google Scholar]
- [23].Brown ES, Varghese FP, McEwen BS. Association of depression with medical illness: does cortisol play a role? Biol Psychiatry 2004;55:1–9. [DOI] [PubMed] [Google Scholar]
- [24].Graham DY. History of Helicobacter pylori, duodenal ulcer, gastric ulcer and gastric cancer. World J Gastroenterol 2014;20:5191–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kim HM, Cho JH, Choi JY, et al. NSAID is inversely associated with asymptomatic gastric ulcer: local health examination data from the Korean National Health Insurance Corporation. Scand J Gastroenterol 2013;48:1371–6. [DOI] [PubMed] [Google Scholar]
- [26].Kim HS, Baik SJ, Kim KH, et al. Prevalence of and risk factors for gastrointestinal diseases in Korean Americans and native Koreans undergoing screening endoscopy. Gut Liver 2013;7:539–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kim JJ, Kim N, Park HK, et al. Clinical characteristics of patients diagnosed as peptic ulcer disease in the third referral center in 2007. Korean J Gastroenterol 2012;59:338–46. [DOI] [PubMed] [Google Scholar]
- [28].Suh M, Choi KS, Park B, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004–2013. Cancer Res Treat 2016;48:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]


