Abstract
Background:
Even though several studies comparing vasectomy and cardiovascular disease (CVD) risk have been reported, most are small series with conflicting results. However, the extent of the risk is still uncertain. We therefore explored whether an association exists between vasectomy and CVD incidence and mortality.
Methods:
We searched PubMed, Embase, Web of Science, and Cochrane Library databases for relevant studies published before January 2017. Multivariate adjusted odds ratio (OR) and associated 95% confidence intervals (CIs) and those by subgroups were extracted and pooled using random-effects models.
Results:
Overall, 12 observational studies (2 cross-sectional studies, 4 case–control studies, and 6 retrospective cohort studies) comprising 299,436 participants were identified. There was no statistically significant relationship between vasectomy and CVD risk (OR: 0.90, 95% CI: 0.81–1.00). Moreover, vasectomy was not associated with CVD mortality (OR: 0.90, 95% CI: 0.81–1.00), coronary heart disease (CHD) incidence (OR: 0.94, 95% CI: 0.88–1.01), stroke incidence (OR: 0.90, 95% CI: 0.72–1.13), and myocardial infarction (MI) incidence (OR: 0.95, 95% CI: 0.88–1.02), with no significant publication bias. In subgroup analyses, the findings on the association between vasectomy and CVD risk were consistent.
Conclusion:
Our findings suggest that vasectomy is not associated with the excess risk of CVD incidence and mortality. Nevertheless, large-volume, well-designed observational studies, with different ethnic populations, low risk of bias, and adjusted confounding factors, are awaited to confirm and update the findings of this analysis.
Keywords: cardiovascular disease, meta-analysis, systematic review, vasectomy
1. Introduction
Vasectomy is a highly effective method of permanent contraception that has gained wide acceptance among adult men in both developed and developing countries.[1,2] In 1995, over 15% males underwent vasectomy in the United States compared with only 4.5% in 1965.[3,4] Vasectomy plays a large role in influencing a person's decisions on family planning, which is regarded as a basic state policy in China.
Cardiovascular diseases (CVD), such as coronary heart disease (CHD), myocardial infarction (MI), and stroke, are a major cause of mortality and morbidity in the general population worldwide. Furthermore, approximately 17.5 million people die of CVD each year, accounting for over 30% of all deaths worldwide according to the World Health Organization.[5,6] Cardiovascular disorders, which are preventable, have brought enormous economic and psychological burden to people who have undergone vasectomy.[7,8] The identification of new cardiovascular risk factors is important for the development of interventions that have therapeutic effects on patients with CVD who are undergoing vasectomy.[9–12]
Considering the effect of CVD risk potentially resulting from vasectomy, a number of studies have detected an association between vasectomy and CVD risk. However, individual studies have yielded inconsistent or conflicting findings, possibly caused by limitations associated with an individual study. Moreover, the potential relationship between vasectomy and CVD risk, to justify either their recommendation or their clinical role, has not been evaluated. Hence, we performed a comprehensive meta-analysis of published studies to shed light on these contradictory results and evaluate the relationship between vasectomy and CVD risk to help clinicians perform related clinical applications of vasectomy.
2. Methods
2.1. Search strategies
This study was executed in line with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[13] and reported based on the guidelines developed by the Meta-Analysis of Observational Studies in Epidemiology group.[14] All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
To identify eligible studies, 2 investigators (Z-LG and J-LX) conducted the main search in the electronic databases of PubMed, Embase, Web of Science, and Cochrane Library to retrieve studies that reported the relationship between vasectomy and CVD risk from database inception up to January 2017. Each database was searched without restrictions to languages, publication types, or regions using the following combination of Medical Subject Headings (MeSH) and non-MeSH search terms: vasectomy, cardiovascular disease, coronary heart disease, coronary artery disease, myocardial infarction, ischemic heart disease, transient ischemic attack, and stroke. Hand searching techniques were also used to identify other potentially relevant studies (manual searches of reference lists were also performed). Any discrepancy was resolved through consultation of an investigator not involved in the initial procedure.
2.2. Study selection criteria
Two independent investigators (Z-LG and J-LX) selected eligible studies that detected a potential relationship between vasectomy and CVD risk in line with the following inclusion criteria: participants were selected without limitations to regions, ages, or social status; studies contained predefined diagnosis criteria for both vasectomy and CVDs; studies had sufficient original data (excluding reviews) on odds ratio (OR), risk ratio, or hazard ratio estimates and 95% confidence intervals (CIs) describing the correlation between vasectomy and CVD risk; and studies used either a case–control, cross-sectional, retrospective, or prospective design. Trials were excluded if any of the following factors were identified: duplicate or overlapping data, animal trials, and conference abstracts, letters, and review articles. Any disagreement was resolved through adjudication of senior authors.
2.3. Data extraction
Data from the included studies were extracted and independently summarized by 2 of the authors (Z-LG and S-SW) using a predefined data extraction form. We resolved any disagreements through discussion. We abstracted study design information, baseline population characteristics (i.e., mean age, sample size, and country), CVD incidence, mortality, and risk estimates from the most fully adjusted model with 95% CIs from all included studies into a standardized evidence table. We also checked these data for accuracy. Moreover, we contacted, if possible, the primary authors for studies with insufficient information to acquire and verify the data.
2.4. Methodological quality assessment
The methodological quality of included studies was assessed by 2 independent reviewers (Z-LG and S-SW) based on the modified Newcastle–Ottawa Scale (NOS),[15] which consists of the following domains: patient selection, study group comparability, and outcome assessment. A score of 0 to 9 (denoted as stars) was allocated for observational studies. Disagreements were also settled through discussion among authors.
2.5. Statistical analysis
For meta-analysis, the total effectiveness rates of extracted data were pooled via Stata 12.0 using ORs with 95% CIs to determine the relationship between vasectomy and CVD risk. The aggregated results and 95% CIs for effect size were calculated using inverse-variance weighted random-effects meta-analysis. The I-square (I2) test was performed to assess the effect of study heterogeneity on the meta-analysis results, with I2 values of 0%, 25%, 50%, and 75% representing no, low, moderate, and high heterogeneity, respectively. Based on the Cochrane review guidelines, a severe heterogeneity of I2 ≥50% warrants the use of random-effects models. Otherwise, a fixed-effects model is utilized. Statistical significance was set at P < .05.[16] Sensitivity analysis was conducted through deletion of each study to evaluate the quality and consistency of the results. Visual inspection of the funnel plot and Egger linear regression test were carried out to assess publication bias. Subgroup analyses were performed in accordance with the different countries and study designs.
3. Results
3.1. Study selection process
Figure 1 presents a flow chart describing this study's selection process. Overall, 485 references were identified through our initial search. Only 420 studies were retrieved after removal of duplicates. Following the screening of titles and abstracts, only 35 studies remained. Finally, a total of 23 full-text articles were discarded for the following reasons: 4 studies did not provide a full text, 6 studies did not present risk estimate with 95% CIs, seven studies did not match the exposure definition, and 5 studies did not regard CVD as its outcome. Therefore, 12 observational studies[17–28] comprising 299,436 participants were subsequently included in our meta-analysis in line with the inclusion criteria.
Figure 1.
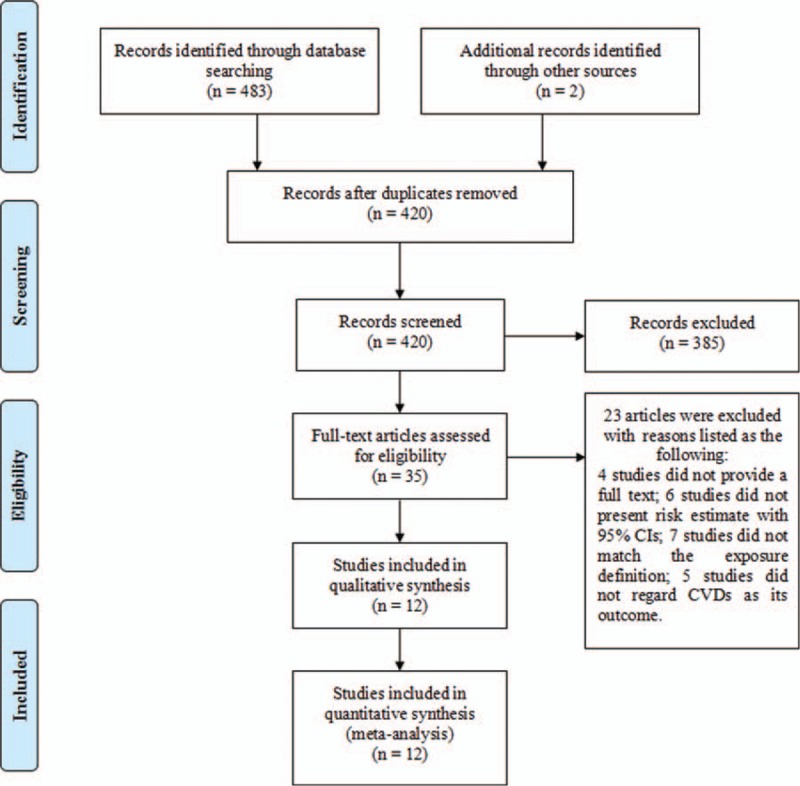
Flow diagram of study selection. Note: Overall, 485 references were identified through our initial search. Only 420 studies were retrieved after removal of duplicates. Following the screening of titles and abstracts, only 35 studies remained. A total of 23 full-text articles were discarded after their full texts were read.
3.2. Study characteristics and methodological quality
Table 1 displays the basic characteristics of the 12 included studies. Moreover, 2 were cross-sectional,[19,25] 4 were case–control,[17,18,21,26] and 6 were retrospective cohort studies.[20,22–24,27,28] The publication years of the included studies ranged from 1981 to 2005. Among them, seven were conducted in the United States,[19,20,23–26,28] 1 in China,[27] 2 in England,[21,22] and 2 in Korea.[17,18] Furthermore, 6 studies were performed among the middle-aged and elderly populations,[17–24,26–28] but one study did not report this.[25] The follow-up length was from 1 to 36 years. In the included clinical trials, the sample sizes varied between 413 and 184,253 participants.
Table 1.
Basic characteristics of the included studies.
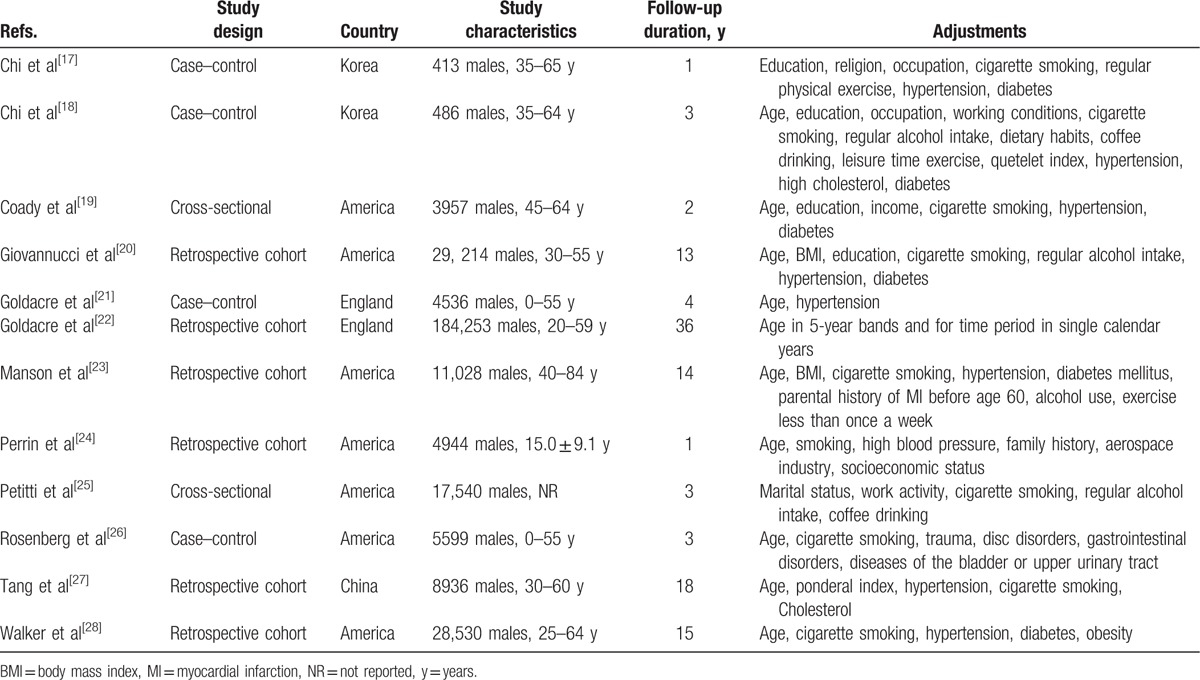
In addition, 9 studies were considered to have high methodological quality,[17,18,20,22–24,26–28] and 3 studies[19,21,25] were regarded to be of poor quality in accordance with the NOS. The main deficiency was selection bias related to insufficient adjustment of core factors among the included studies.
3.3. Vasectomy and CVD risk
3.3.1. Overall results
Meta-analysis of the included studies[17–28] performed through a random-effects model showed that vasectomy was not associated with CVD risk (Fig. 2). The pooled OR was 0.90 (95% CI: 0.81–1.00). However, significant heterogeneity was found (I2 = 80.5%, P = .000). Thus, subgroup analyses were conducted to investigate the potential factors that may substantially affect the between-study heterogeneity.
Figure 2.
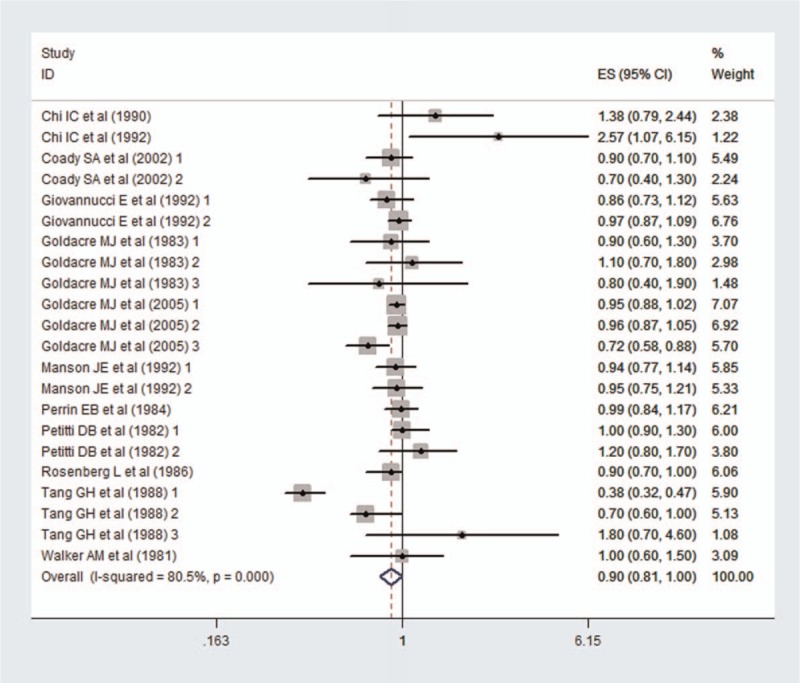
Overall meta-analysis results. Note: A meta-analysis of the included studies conducted through a random-effects model showed that vasectomy was not associated with CVD risk. The pooled OR was 0.90 (95% CI: 0.81–1.00). However, significant heterogeneity was found (I2 = 80.5%, P = .000).
3.3.2. CVD mortality
Data on CVD mortality were available for analysis from 4 studies (2 case–control[17,18] and 4 retrospective cohort studies[20,27]; Fig. 3). Similarly, meta-analysis did not show a significant difference in CVD mortality between vasectomy and nonvasectomy participants (OR = 0.95; 95% CI: 0.48–1.87) with significant heterogeneity observed among the individual studies (I2 = 94.2%, P = .000).
Figure 3.
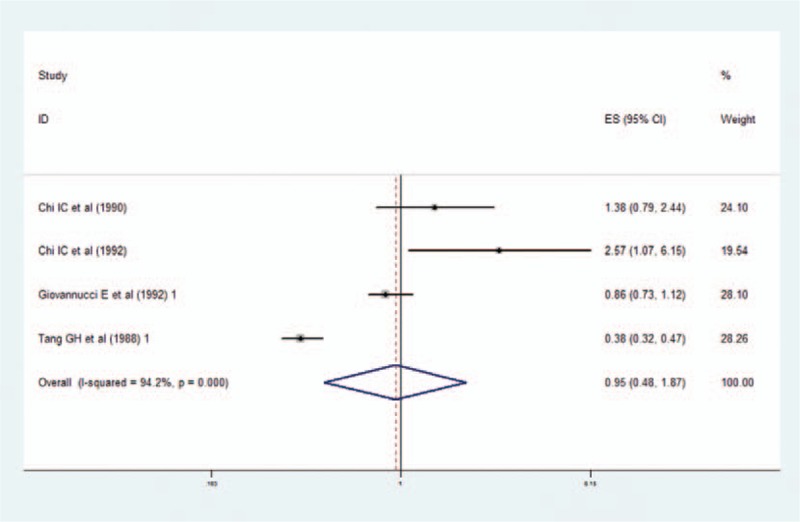
Meta-analysis results of CVD mortality. Note: Data on CVD mortality were available for analysis from 4 studies (2 case–control and 2 retrospective cohort studies). Similarly, the meta-analysis did not show a significant difference in CVD mortality between vasectomy and nonvasectomy participants (OR = 0.95, 95% CI: 0.48–1.87) with significant heterogeneity noted among the individual studies (I2 = 94.2%, P = .000).
3.3.3. CVD incidence
Data on CVD incidence were available for analysis from 10 studies (2 case–control,[21,26] 2 cross-sectional,[19,25] and 6 retrospective cohort studies[20,22–24,27,28]; Fig. 4). The results suggested that vasectomy was not associated with CHD (OR, 0.94; 95% CI, 0.88–1.01), stroke (OR, 0.90; 95% CI, 0.72–1.13), and MI (OR, 0.95; 95% CI, 0.88–1.02) incidences with no significant heterogeneity (I2 = 7%, P = .372).
Figure 4.
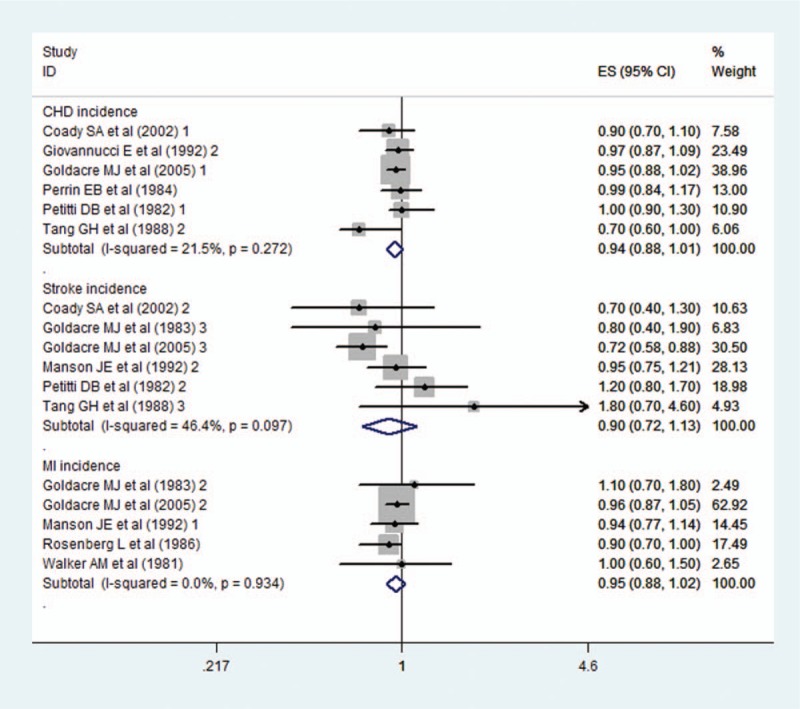
Meta-analysis results of CVD incidence. Note: Data on CVD incidence were available for analysis from 10 studies (2 case–control, 2 cross-sectional, and 6 retrospective cohort studies). The results suggested that vasectomy was not associated with CHD (OR, 0.94; 95% CI, 0.88–1.01), stroke (OR, 0.90; 95% CI, 0.72–1.13), and MI (OR, 0.95; 95% CI, 0.88–1.02) incidences with no significant heterogeneity (I2 = 12.2%, P = .311).
3.4. Subgroup analyses
In the subgroup analyses of the study designs (Fig. 5) and different countries (Fig. 6), we found that the findings regarding the association between vasectomy and CVD risk were consistent. Accordingly, study designs did not significantly contribute to heterogeneity except the cross-sectional design. Similarly, heterogeneity could not be explained by the subgroup analyses on the different countries except the United States. However, subgroup analyses were not performed for age and follow-up length considering the limited number of independent datasets.
Figure 5.
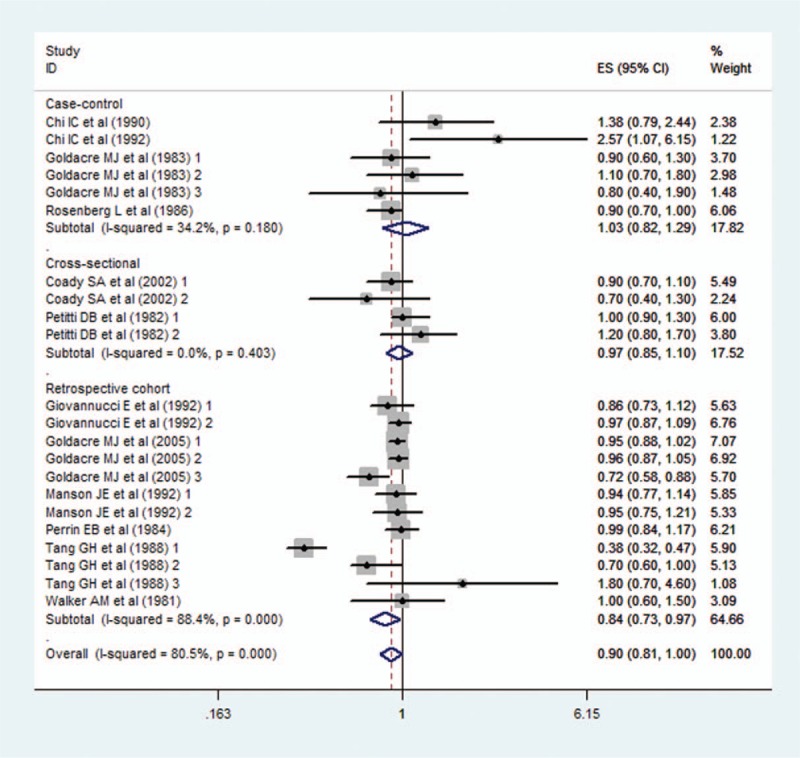
Subgroup meta-analysis for the effect of different study designs. Note: The included studies could be classified into cross-sectional, case–control, and retrospective designs. Subgroup meta-analysis showed that the findings on the association between vasectomy and CVD risk were consistent. The heterogeneity was low or zero when studies had cross-sectional and case–control designs.
Figure 6.
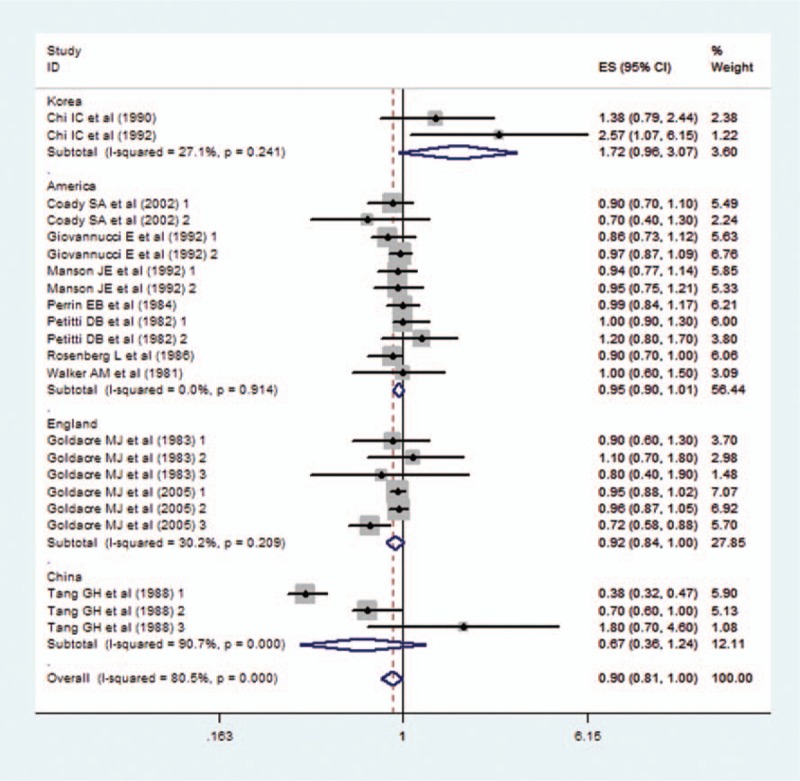
Subgroup meta-analysis for the effect of different countries. Note: All the included studies were from the United States, China, Korea, and England. Subgroup meta-analysis showed that the results on the association between vasectomy and CVD risk were consistent. The heterogeneity was low or zero when studies were divided into the United States, Korea, and England.
3.5. Sensitivity analysis
Sensitivity analysis was conducted to determine whether a certain study strongly influences the estimates between vasectomy and CVD risk or affected the final heterogeneity. We evaluated the effect of each study on the methodological quality through sequential exclusion of single studies. The finding demonstrated that the stability of results had no significant changes (Fig. 7), which validated the rationality and reliability of our analysis.
Figure 7.
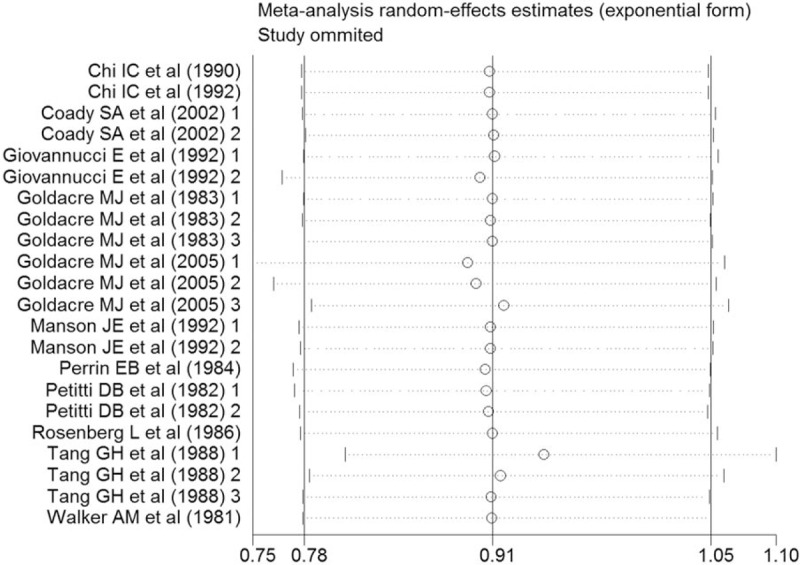
Sensitivity analysis. Note: This figure shows the pooled analysis result after one certain study was omitted. The stability of results had no significant changes, which validated the rationality and reliability of our analysis.
3.6. Evaluation of publication bias
Visual inspection of the funnel plot and Egger linear regression test were carried out to assess for publication bias (Fig. 8). Finally, Egger test result (P = .873) was found to be insignificant, indicating that our study presented low probability of publication bias.
Figure 8.
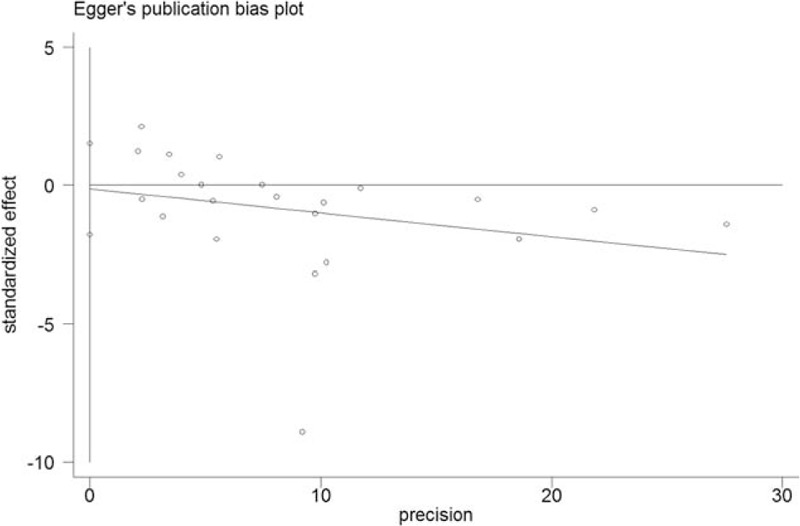
Funnel plot. Note: Visual inspection of the funnel plot and Egger linear regression test were performed to assess publication bias. Egger test result (P = .873) was insignificant, indicating that our study presented low probability of publication bias.
4. Discussion
In this study, we analyzed the associations between vasectomy and CVD risk using a meta-analysis of the 12 included studies[17–28] to obtain a robust conclusion. This research is the first meta-analysis providing comprehensive insights into the relationship between vasectomy and CVD risk through a summary and review of previously published, quantitative studies to answer a wide variety of clinical questions related to this field. Overall, our results demonstrate that vasectomy was not associated with a significant risk of CVD incidence and mortality. Furthermore, no evident publication bias was obtained through the visual distribution of funnel plot and Egger test. The subgroup meta-analyses indicated that the association between vasectomy and CVD risk was not significantly modified by the different countries and study designs. Sensitivity analysis suggests that the results were rational and reliable through omission of any single study.
Vasectomy is a common method of permanent contraception among adult men. Its relationship to excess risk of CVD mortality and incidence has been debated for many years.[29,30] However, the potential biological mechanisms underlying the observed association between vasectomy and CVD risk remain unclear. Alexander[31] emphasized that we should not ignore the fact that persistent autoimmune responses to spermatozoal antigens are generated in both vasectomized men and animals. In addition, Patel[32] found that vasectomy significantly increases the amount of esterified and total cholesterol in aortic tissue. Moreover, family physicians should be aware of the risks and effects between vasectomy and CVD, so they can appropriately counsel patients seeking sterilization.[33] Our findings indicated that vasectomy was not associated with excess CVD risk, and the decision to opt for a vasectomy resulted in benefits to public health.
In the 1980s, a number of observational studies suggested that vasectomy history is not related to the excess CVD risk.[17,19–28] Nevertheless, 1 case–control study[18] that was conducted in 1992 presented contradictory results, which showed that vasectomy is associated with the increase in CVD risk. The selection and recall bias might limit the statistical effects and explain the different results. Hence, our understanding of age and social status of the participants of the included studies is insufficient, although some of these factors have been rarely investigated in other studies. Moreover, our subgroup analyses found that the high heterogeneity across studies was potentially ascribed to the cross-sectional design and the population of the United States. Thus, further research is needed to verify the findings of this meta-analysis with regard to the different ethnic populations, low bias risk, and adjusted confounding factors on the extensive consequences.
In general, our meta-analysis exhibited several crucial strengths. First, to our knowledge, the latest guideline[34] has not yet discussed whether an association exists between vasectomy and CVD incidence and mortality, so the extent of the risk is still controversial. The meta-analysis was the first to assess a potential correlation between vasectomy and the risk of cancer incidence and mortality in populations around the world through thorough systematic search and rigorous analytical approaches. Second, multivariable-adjusted risk estimates were applied to minimize the confounding factors that might influenced the whole results and to result in well-founded conclusions. Third, the rationality and reliability of our meta-analysis was observably improved because the overall combined estimates were based on a large sample size. Furthermore, sufficient subgroup analyses and sensitivity analyses were also performed to ensure the reliability of this study.
The present meta-analysis has the following limitations that must be considered before our findings are accepted. First, the enrolled studies in this meta-analysis mostly date back to 10 to 20 years ago (1980–2000), and most of them have negative results. Second, residual confounding and nonmeasurable factors were present in the included observational studies. More accurate outcomes of our results would result from adjustments of other confounding factors, such as age, body mass index, and income. Third, the studies included in this analysis were insufficient, especially in terms of subgroup analysis. Thus, potential publication bias is very likely to exist even though no evidence was obtained from our statistical tests. Fourth, heterogeneity is another critical issue that must be given close attention considering this factor's possible association with the population's age and other underlying diseases. Lastly, only English language reports were included. Consequently, we may have missing data from important studies published in other languages.
5. Conclusions
In summary, our meta-analysis suggests that vasectomy was not associated with the excess risk of CVD mortality and incidence, including CHD, MI, and stroke. However, despite our rigorous methodology, the inherent limitations of the included studies and the considerable number of possible confounding factors may reduce the effect estimates and prevent us from reaching definitive conclusions. Therefore, large-scale, well-designed observational studies with various ethnic populations, low bias risk, and adjusted confounding factors are necessary to confirm and update the findings of this analysis.
Acknowledgment
We would like to thank KGSupport for editing the language of this study.
Footnotes
Abbreviations: CHD = coronary heart disease, CIs = confidence intervals, CVD = cardiovascular disease, MeSH = Medical Subject Headings, MI = myocardial infarction, NOS = Newcastle–Ottawa Scale, OR = odds ratio, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Trial registration number: PROSPERO 2017: CRD 42017055205.
Author contributions: Z-LG conceived the study idea. Z-LG and J-LX searched the literature and screened the studies. Z-LG and S-SW conducted data extraction and methodological quality evaluation. R-KL performed statistical analyses and interpretation of corresponding results. Z-LG drafted the initial manuscript. S-SW and R-KL modified the initial manuscript. S-SW and R-KL had primary responsibility for the final content. All authors made critical comments for the initial manuscript.
The authors have no conflicts of interest to disclose.
References
- [1].Smith RP, Lipshultz LI, Kovac JR. Vasectomy reversal and other strategies to mitigate postvasectomy pain syndrome. Asian J Androl 2016;18:338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Muñoz X, Mata A, Bassas L, et al. Altered miRNA signature of developing germ-cells in infertile patients relates to the severity of spermatogenic failure and persists in spermatozoa. Sci Rep 2015;9:17991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Abma J, Chandra A, Mosher W, et al. Fertility, family planning, and women’ s health: new data from the 1995 National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 1997;23:62–3. [PubMed] [Google Scholar]
- [4].Eisenberg ML, Henderson JT, Amory JK, et al. Racial differences in vasectomy utilization in the United States: data from the national survey of family growth. Urology 2009;74:1020–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Haugen IK, Ramachandran VS, Misra D, et al. Hand osteoarthritis in relation to mortality and incidence of cardiovascular disease: data from the Framingham heart study. Ann Rheum Dis 2015;74:74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Rimm AA, Hoffmann RG, Anderson AJ, et al. The relationship between vasectomy and angiographically determined atherosclerosis in men. Prev Med 1983;12:262–73. [DOI] [PubMed] [Google Scholar]
- [8].Mullooly JP, Wiest WM, Alexander NJ, et al. Vasectomy, serum assays, and coronary heart disease symptoms and risk factors. J Clin Epidemiol 1993;46:101–9. [DOI] [PubMed] [Google Scholar]
- [9].Wang D, Wang J, Jin C, et al. Asymptomatic extracranial artery stenosis and the risk of cardiovascular and cerebrovascular diseases. Sci Rep 2016;6:33960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Samplaski MK, Daniel A, Jarvi K. Vasectomy as a reversible form of contraception for select patients. Can J Urol 2014;21:7234–740. [PubMed] [Google Scholar]
- [11].Liu JS, Jones M, Casey JT, et al. Diagnosis of varicoceles in men undergoing vasectomy may lead to earlier detection of hypogonadism. Urology 2014;83:1322–5. [DOI] [PubMed] [Google Scholar]
- [12].McDonald SW. Is vasectomy harmful to health. Br J Gen Pract 1997;47:381–6. [PMC free article] [PubMed] [Google Scholar]
- [13].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [15].Wells GA, Shea B, Connell DO, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (2011). [Google Scholar]
- [16].Fox MW, Piepgras DG, Bartleson JD. Anterolateral decompression of the atlantoaxial vertebral artery for symptomatic positional occlusion of the vertebral artery: case report. J Neurosurg 1995;83:737–40. [DOI] [PubMed] [Google Scholar]
- [17].Chi IC, Kong SK, Wilkens LR, et al. Vasectomy and cardiovascular deaths in Korean men: a community-based case-control study. Int J Epidemiol 1990;19:1113–5. [DOI] [PubMed] [Google Scholar]
- [18].Chi IC, Ko UR, Wilkens LR, et al. Vasectomy and non-fatal acute myocardial infarction: a hospital-based case-control study in Seoul, Korea. Int J Epidemiol 1990;19:32–41. [DOI] [PubMed] [Google Scholar]
- [19].Coady SA, Sharrett AR, Zheng ZJ, et al. Vasectomy, inflammation, atherosclerosis and long-term followup for cardiovascular diseases: no associations in the atherosclerosis risk in communities study. J Urol 2002;167:204–7. [PubMed] [Google Scholar]
- [20].Giovannucci E, Tosteson TD, Speizer FE, et al. A long-term study of mortality in men who have undergone vasectomy. N Engl J Med 1992;326:1392–8. [DOI] [PubMed] [Google Scholar]
- [21].Goldacre MJ, Holford TR, Vessey MP, et al. Cardiovascular disease and vasectomy. Findings from two epidemiologic studies. N Engl J Med 1983;308:805–8. [DOI] [PubMed] [Google Scholar]
- [22].Goldacre MJ, Wotton CJ, Seagroatt V, et al. Cancer and cardiovascular disease after vasectomy: an epidemiological database study. Fertil Steril 2005;84:1438–43. [DOI] [PubMed] [Google Scholar]
- [23].Manson JE, Ridker PM, Spelsberg A, et al. Vasectomy and subsequent cardiovascular disease in US physicians. Contraception 1999;59:181–6. [DOI] [PubMed] [Google Scholar]
- [24].Perrin EB, Woods JS, Namekata T, et al. Long-term effect of vasectomy on coronary heart disease. Am J Public Health 1984;74:128–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Petitti DB, Klein R, Kipp H, et al. A survey of personal habits, symptoms of illness, and histories of disease in man with and without vasectomies. Am J Public Health 1982;72:476–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rosenberg L. The risk of myocardial infarction 10 or more years after vasectomy in men under 55 years of age. Am J Epidemiol 1986;123:1049–56. [DOI] [PubMed] [Google Scholar]
- [27].Tang GH, Zhong YH, Ma YM, et al. Vasectomy and health: cardiovascular and other diseases following vasectomy in Sichuan province, People's Republic of China. Int J Epidemiol 1988;17:608–17. [DOI] [PubMed] [Google Scholar]
- [28].Walker AM, Jick H, Hunter JR, et al. Vasectomy and non-fatal myocardial infarction. Lancet 1981;1:13–5. [DOI] [PubMed] [Google Scholar]
- [29].Schwingl PJ, Guess HA. Safety and effectiveness of vasectomy. Fertil Steril 2000;73:923–36. [DOI] [PubMed] [Google Scholar]
- [30].Kovac JR, Lipshultz LI. Basic concepts and recent advancements in the study of male fertility. Asian J Androl 2016;18:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Alexander NJ. Possible mechanisms of vasectomy-exacerbated atherosclerosis. Aust J Biol Sci 1982;35:469–79. [DOI] [PubMed] [Google Scholar]
- [32].Patel AP, Smith RP. Vasectomy reversal: a clinical update. Asian J Androl 2016;18:365–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Raspa RF. Complications of vasectomy. Fam Phys 1993;48:1264–8. [PubMed] [Google Scholar]
- [34].Borque Á. European Association of Urology guidelines on vasectomy. Actas Urol Esp 2013;37:257. [DOI] [PubMed] [Google Scholar]


