There are many potential sources of injury, such as sharp objects that penetrate the skin, thermal or chemical burns, and friction or scraping. Depending on the individual patient and the size and location of the skin injury, the resulting wounds may heal in multiple possible ways. These range from minimally visible scarring to severe thickening and tightening of the skin that can be disfiguring and/or prevent normal movement. Recent advances in treatment are improving the outlook for patients with traumatic scarring.
The Facts of Traumatic Scarring
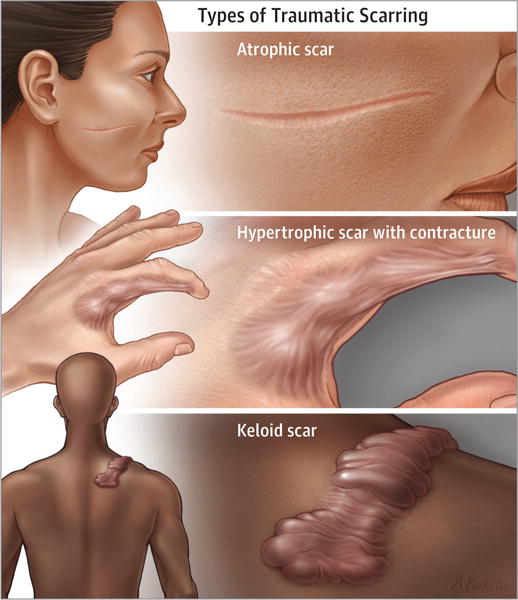
Traumatic scarring may occur in people of all ethnicities and ages. Atrophic scars are lower and thinner than the surrounding skin. Hypertrophic scars are thickened and elevated above the skin but remain within the boundaries of the initial injury. Keloid scars are elevated and extend beyond the boundaries of the initial injury. Traumatic scars may affect patients physically, psychologically, and socially. Scar tightening (contractures), especially over joints, may limit normal movement and the ability to participate in normal activities of daily living. Disfigurement can affect the way people perceive themselves and the way others perceive them, possibly even leading to feelings of depression or anxiety. Traumatic scars can frequently cause pain, itch, and other abnormal sensations.
Diagnosis and Testing
Scar types and their associated problems are determined primarily by medical history and physical examination performed by a physician. Therapists may perform measurements to assess movement. Biopsies and laboratory tests may be of limited use.
Treatment
There is no cure for traumatic scarring, so injury prevention and effective early wound care are important to minimize scar formation. Physical therapy, pressure, and other treatments can help minimize contracture formation after injury. Medical teams that treat scars can include dermatologists, plastic surgeons, physical and occupational therapists, and psychologists. Other professionals may assist with scar camouflage. Common treatments include topical and injected corticosteroids, injected chemotherapeutic agents (eg, fluorouracil), silicone gel sheeting, cryotherapy with liquid nitrogen, and irradiation. Atrophic scars may be treated with tissue fillers. Lasers that target blood vessels are commonly used for reds cars, and newer ablative (destructive) and nonablative fractional lasers have advanced treatment substantially for some patients with traumatic scars, although multiple treatments are usually needed. Severe scars and contractures may require surgery.
Acknowledgments
Funding/Support: Dr Jagdeo is a recipient of a National Institutes of Health (NIH) K23 Career Development Award focused on the investigation of novel light-based antiscar therapy. Information reported in this publication is based on research that was supported by the National Institute of General Medical Sciences of the NIH under Award No. K23GM117309.
Role of the Funder/Sponsor: The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the NIH, Department of Defense, or the United States government.
Section Editor: Misha Rosenbach, MD
The JAMA Dermatology Patient Page is a public service of JAMA Dermatology. The information and recommendations appearing on this page are appropriate in most instances, but they are not a substitute for medical diagnosis. For specific information concerning your personal medical condition, JAMA Dermatology suggests that you consult your physician. This page may be photocopied noncommercially by physicians and other health care professionals to share with patients. To purchase bulk reprints, call (312) 464-0776.
Contributor Information
Jared Jagdeo, Department of Dermatology, UC Davis, Department of Dermatology, SUNY Downstate Medical Center and Dermatology Service, Sacramento VA.
Peter R. Shumaker, Department of Dermatology, Naval Medical Center San Diego.
References
- 1.Mamalis AD, Lev-Tov H, Nguyen DH, Jagdeo JR. Laser and light-based treatment of Keloids–a review. J Eur Acad Dermatol Venereol. 2014 Jun;28(6):689–99. doi: 10.1111/jdv.12253. Epub 2013 Aug 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson RR, Donelan MB, Hivnor C, Greeson E, Ross EV, Shumaker PR, Uebelhoer NS, Waibel JS. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014 Feb;150(2):187–93. doi: 10.1001/jamadermatol.2013.7761. [DOI] [PubMed] [Google Scholar]
- 3.Mamalis A, Koo E, Garcha M, Murphy WJ, Isseroff RR, Jagdeo J. High fluence light emitting diode-generated red light modulates characteristics associated with skin fibrosis. J Biophotonics. 2016 Dec;9(11–12):1167–1179. doi: 10.1002/jbio.201600059. Epub 2016 May 13. [DOI] [PMC free article] [PubMed] [Google Scholar]


