Abstract
Objective To determine the effect of combinations of statins, aspirin, β blockers, and angiotensin converting enzyme inhibitors in the secondary prevention of all cause mortality in patients with ischaemic heart disease.
Design Open prospective cohort study with nested case-control analysis.
Setting 1.18 million patients registered with 89 general practices across 23 strategic health authority areas within the United Kingdom. Practices had longitudinal data for a minimum of eight years and were contributing to QRESEARCH, a new database.
Patients All patients with a first diagnosis of ischaemic heart disease between January 1996 and December 2003. Cases were patients with ischaemic heart disease who died. Controls were patients with ischaemic heart disease who were matched for age, sex, and year of diagnosis and were alive at the time their matched case died.
Main outcome measures Odds ratio with 95% confidence interval for risk of death in cases compared with controls. Exposure was current use of different combinations of statins, aspirin, β blockers, and angiotensin converting enzyme inhibitors before death in cases, or the equivalent date in controls.
Results 13 029 patients had a first diagnosis of ischaemic heart disease (incidence rate 338 per 100 000 person years). 2266 cases were matched to 9064 controls. Drug combinations associated with the greatest reduction in all cause mortality were statins, aspirin, and β blockers (83% reduction, 95% confidence interval 77% to 88%); statins, aspirin, β blockers, and angiotensin converting enzyme inhibitors (75% reduction, 65% to 82%); and statins, aspirin, and angiotensin converting enzyme inhibitors (71% reduction, 59% to 79%). Treatments associated with the smallest reduction in all cause mortality were β blockers alone (19% reduction, 37% reduction to 4% increase), angiotensin converting enzyme inhibitors alone (20% reduction, 1% to 35%), and combined statins and angiotensin converting enzyme inhibitors (31% reduction, 57% reduction to 12% increase).
Conclusions Combinations of statins, aspirins, and β blockers improve survival in high risk patients with cardiovascular disease, although the addition of an angiotensin converting enzyme inhibitor conferred no additional benefit despite the analysis being adjusted for congestive cardiac failure.
Introduction
Randomised controlled trials have shown that statins improve the survival of patients with ischaemic heart disease.1-5 Although combinations of drugs (as proposed in the Polypill)6 have been received with enthusiasm, we found no direct evidence evaluating the effects of statins, aspirin, β blockers, and angiotensin converting enzyme inhibitors in combination.
Uncritical acceptance of medical innovations or lack of evidence can result in the endorsement of ineffective or potentially dangerous treatments, subsequently leading to the withdrawal of drugs (for example, rofecoxib) or limitations on use.7-9 Limitations on use can occur years after worldwide adoption, as was the case with hormone replacement therapy.10 Although randomised trials provide relatively unbiased evidence of the effectiveness of interventions in selected patients, the application of trial results to representative populations of patients is often inaccurate.11 In addition, further trials can be difficult, or even unethical if a true benefit is suspected.
Routinely collected data from aggregated general practice databases have been used successfully to evaluate the risks and benefits of treatments in a population.12,13 This method enables access to longitudinal data, to a large sample size, and to representative populations. Also, because data on exposure can be collected before the outcome occurs, recall bias is limited; the quality of the electronic record now surpasses that of the paper based system.14
We determined the effect of combinations of drugs in the secondary prevention of all cause mortality in patients with ischaemic heart disease in a large UK population based sample.
Methods
We carried out a prospective open cohort study with nested case-control analysis using data from 89 general practices contributing to a new UK database, QRESEARCH (version 1, downloaded 17 December 2003). This database will ultimately contain the records of over 7.5 million patients from 500 practices in the United Kingdom. For our study we selected only practices with at least eight years of longitudinal data—that is, with Egton Medical Information Services (EMIS) software before 1 January 1996. The practices were spread throughout 23 of the 29 strategic health authority areas across the United Kingdom.
Participants
We identified all patients registered with the practices from 1 January 1996 until the end of the study period (17 December 2003, the date of the most recent computer download at the time of the analysis). Our start date was the 1 January 1996 as this was just over 12 months after the publication of the Scandinavian simvastatin survival study.1 Our open cohort was selected on the basis of registration dates and dates of leaving the study or death. We identified all patients with incident ischaemic heart disease diagnosed after the 1 January 1996 from the date of first diagnosis of the disease recorded on computer. To minimise information bias, we excluded patients whose diagnosis was made within the first three months of registration with the general practice, patients prescribed statins before the diagnosis of ischaemic heart disease, and patients with a first diagnosis after death (postmortem diagnosis).
Nested case-control study
We undertook a nested case-control analysis to determine the effects of different combinations of drugs on survival in patients with ischaemic heart disease. Cases were patients with ischaemic heart disease who died from all causes during the follow-up period, the index date being defined as the date of death. We used incidence density sampling to randomly select four controls for each case, matched for age at diagnosis of ischaemic heart disease (five year bands, < 45; 45-49, etc), year of diagnosis, and sex. Controls had to be alive when their matched case died. The index date for controls was the date when their matched case died.
Statistical analysis
For cases and controls we reviewed the medical history and data on exposure between the date of diagnosis of ischaemic heart disease and the index date. To measure exposure for each drug we determined the dates of the first and the last prescriptions before the index date. We considered patients as currently receiving a drug if their last prescription was issued within 90 days before the index date. We derived a categorical variable for exposure, which contained levels according to different combinations of four drugs (statins, angiotensin converting enzyme inhibitors, β blockers, and aspirin) taken within 90 days of the index date. The reference group was no current use of any of these drugs.
We used conditional logistic regression for individually matched case-control studies to derive odds ratios with 95% confidence intervals for the risk of death associated with different combinations of aspirin, angiotensin converting enzyme inhibitors, β blockers, and statins before death, or the equivalent date in the matched controls. We adjusted for comorbidity (diabetes, congestive cardiac failure, hypertension, myocardial infarction) and current use of calcium channel blockers. We also adjusted for last recorded smoking status (ever smoker, never smoker, not recorded), body mass index (kg/m2; < 25, 25-30, > 30, not recorded), and fifth of Townsend score (as a measure of deprivation). The Townsend score was calculated on the basis of the 2001 census data associated with the output area of the patient's postcode. We tested for an interaction between current use of each drug and each type of comorbidity, sex, and age. To address concerns about confounding by indication, we carried out an analysis restricted to patients without diabetes, congestive cardiac failure, or myocardial infarction.15 All the analyses were carried out in Stata (version 8.2). We selected a P value of 0.01 (two tailed) as statistically significant.
Results
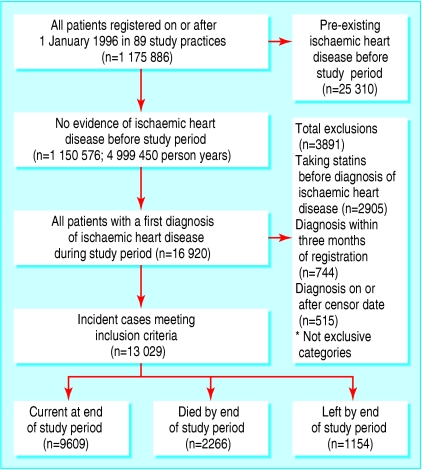
Eighty nine practices met our selection criteria (figure). Overall, 1 175 886 patients were registered on or after 1 January 1996 (604 781 women and 571 105 men), accumulating almost five million (4 999 450 patients) person years of observation. Of these registered patients, 25 310 patients had ischaemic heart disease recorded before 1 January 1996 and were not included in this analysis.
Figure 1.
Flow of patients through trial
In total, 16 920 patients were identified with a first diagnosis of ischaemic heart disease during the study period (overall incidence rate of ischaemic heart disease 338.4 per 100 000 person years, 95% confidence interval 333.4 to 343.6). The crude incidence of ischaemic heart disease in women was 286.2 per 100 000 person years and in men was 392.4 per 100 000 person years. The age standardised incidence rate per 100 000 person years was, respectively, 250.8, 245.0 to 256.6 and 427.5, 418.9 to 436.1. Our inclusion criteria were met by 13 029 of the 16 920 patients with ischaemic heart disease. During the 43 460 person years of observation there were 2266 deaths for all causes for patients with ischaemic heart disease giving an overall all cause mortality of 52.1 per 1000 person years, 50.3 to 54.3.
Case-control analysis
For the 2266 cases who died during the follow-up period, we identified 9064 controls matched by age, sex, and year of diagnosis who were alive at the time their case died. Cases and controls were well matched at baseline for age and sex (table 1). The median duration of ischaemic heart disease before the index date was 20.3 months for cases and 21.0 months for controls. Overall, 445 cases (19.6% of 2266) had been prescribed any statin compared with 2303 of the controls (25.4% of 9064) between the date of diagnosis of ischaemic heart disease and the index date. Cases had a higher prevalence of congestive cardiac failure, diabetes, and myocardial infarction and a lower prevalence of hypertension (table 1).
Table 1.
Characteristics of cases with ischaemic heart disease who died and controls. Values are numbers (percentages) unless stated otherwise
| Characteristic | Cases (n=2266) | Controls (n=9064) |
|---|---|---|
| Median (interquartile range) age at index date | 80 (73-86) | 80 (73-85) |
| Median (interquartile range) No of months between diagnosis and index date | 20.3 (6.3-40.5) | 20.9 (7.9-40.9) |
| Women | 1003 (44.3) | 4012 (44.3) |
| Men | 1263 (55.7) | 5052 (55.7) |
| Median (interquartile range) Townsend score* | −0.8 (−2.7-2.3) | −1.2 (−3.0-1.8) |
| Drugs used before index date after diagnosis of ischaemic heart disease: | ||
| Any statin | 445 (19.6) | 2303 (25.4) |
| Angiotensin converting enzyme inhibitors | 1126 (49.7) | 3601 (39.7) |
| Aspirin | 1694 (74.8) | 6843 (75.5) |
| β blockers | 996 (44.0) | 4749 (52.4) |
| Calcium channel blockers | 969 (42.8) | 3848 (42.5) |
| Comorbidity before index date: | ||
| Diabetes | 367 (16.2) | 1024 (11.3) |
| Hypertension | 840 (37.1) | 3699 (40.8) |
| Congestive cardiac failure | 716 (31.6) | 1408 (15.5) |
| Myocardial infarction | 892 (39.4) | 2531 (27.9) |
Four controls per case were matched on age, sex, and year of diagnosis of ischaemic heart disease.
Townsend score is a proxy measure for material deprivation.
Table 2 shows the unadjusted and adjusted odds ratios for the different drug combinations. After adjustment for comorbidity (diabetes, hypertension, congestive cardiac failure, and myocardial infarction), use of calcium channel blockers, smoking status, body mass index (obese, not obese, not recorded), and Townsend score (fifths), the drugs associated with the greatest reductions in odds for all cause mortality were statins, aspirin, and β blockers (83% reduction, 95% confidence interval 77% to 88% reduction); statins, aspirin, angiotensin converting enzyme inhibitors, and β blockers (75% reduction, 65% to 82% reduction); and statins, angiotensin converting enzyme inhibitors, and aspirin (71% reduction, 59% to 79% reduction).
Table 2.
Unadjusted and adjusted odds ratios for all cause mortality according to current* use of different combinations of aspirin, statins, β blockers, and angiotensin converting enzyme inhibitors, Values are numbers (percentages) unless stated otherwise
| Current use of studied drugs* | Cases (n=2266) | Controls (n=9064) | Unadjusted odds ratio (95% CI) | Adjusted odds ratio†(95% CI) |
|---|---|---|---|---|
| None | 677 (29.9) | 1738 (19.2) | 1.00 | 1.00 |
| Statins alone | 26 (1.1) | 117 (1.3) | 0.48 (0.31 to 0.74) | 0.53 (0.33 to 0.86) |
| Angiotensin converting enzyme inhibitors | 211 (9.3) | 474 (5.2) | 1.14 (0.94 to 1.37) | 0.80 (0.65 to 0.99) |
| Aspirin alone | 420 (18.5) | 1830 (20.2) | 0.58 (0.51 to 0.67) | 0.59 (0.50 to 0.68) |
| β blockers alone | 109 (4.8) | 440 (4.9) | 0.63 (0.50 to 0.79) | 0.81 (0.63 to 1.04) |
| Statins or angiotensin converting enzyme inhibitors | 35 (1.5) | 65 (0.7) | 1.14 (0.74 to 1.75) | 0.69 (0.43 to 1.12) |
| Statins and aspirin | 72 (3.2) | 424 (4.7) | 0.37 (0.28 to 0.48) | 0.39 (0.29 to 0.52) |
| Statins and β blockers | 20 (0.9) | 92 (1.0) | 0.48 (0.29 to 0.79) | 0.46 (0.26 to 0.82) |
| Angiotensin converting enzyme inhibitors and aspirin | 256 (11.3) | 852 (9.4) | 0.76 (0.64 to 0.90) | 0.54 (0.45 to 0.66) |
| Angiotensin converting enzyme inhibitors and β blockers | 45 (2.0) | 144 (1.6) | 0.75 (0.53 to 1.06) | 0.64 (0.43 to 0.94) |
| Aspirin and β blockers | 151 (6.7) | 1087 (12.0) | 0.33 (0.27 to 0.41) | 0.38 (0.31 to 0.47) |
| Statins, angiotensin converting enzyme inhibitors, and aspirin | 60 (2.6) | 319 (3.5) | 0.41 (0.31 to 0.56) | 0.29 (0.21 to 0.41) |
| Statins, angiotensin converting enzyme inhibitors, and β blockers | 11 (0.5) | 34 (0.4) | 0.68 (0.34 to 1.37) | 0.67 (0.30 to 1.51) |
| Statins, aspirin, and β blockers | 45 (2.0) | 622 (6.9) | 0.16 (0.11 to 0.22) | 0.17 (0.12 to 0.23) |
| Angiotensin converting enzyme inhibitors, aspirin, and β blockers | 71 (3.1) | 420 (4.6) | 0.41 (0.31 to 0.54) | 0.34 (0.26 to 0.46) |
| Statins, angiotensin converting enzyme inhibitors, aspirin, and β blockers | 57 (2.5) | 406 (4.5) | 0.31 (0.23 to 0.42) | 0.25 (0.18 to 0.35) |
Last prescription for drug within 90 days before index date.
Adjusted for comorbidity (diabetes, hypertension, congestive cardiac failure, and myocardial infarction), use of calcium channel blockers, smoking status, body mass index (obese, not obese, not recorded), and Townsend score (fifths).
The drugs associated with the smallest reductions in all cause mortality were β blockers alone (19% reduction, 37% reduction to 4% increase), angiotensin converting enzyme inhibitors alone (20% reduction, 1% to 35% reduction), and combined statins and angiotensin converting enzyme inhibitors (31% reduction, 57% reduction to 12% increase).
We found a significant interaction between current use of aspirin and myocardial infarction. In drug combinations containing aspirin, the reductions in all cause mortality were greater in people with myocardial infarction—for example, a combination of statins, aspirin, and β blockers was associated with a 90% reduction in all cause mortality (95% confidence interval 82% to 94%). We found a significant interaction between current use of angiotensin converting enzyme inhibitors and age: drug combinations containing angiotensin converting enzyme inhibitors were associated with greater reductions in all cause mortality in people aged 75 and over. No other significant interactions were found.
Cases had a higher prevalence of congestive cardiac failure, diabetes, and myocardial infarction and a lower prevalence of hypertension. An analysis restricted to patients without diabetes, myocardial infarction, or congestive cardiac failure showed little change in the odds ratios except for angiotensin converting enzyme inhibitors alone (adjusted odds ratio 1.13, 0.69 to 1.84). Results were similar in an analysis of people aged 65 and over. An analysis restricted to people with recorded smoking status and body mass index gave results with lower odds ratios but wider confidence intervals.
Discussion
Combinations of statins, aspirin, and β blockers improve the survival of high risk patients with ischaemic heart disease, although the addition of an angiotensin converting enzyme inhibitor conferred no additional benefit despite adjustment for congestive cardiac failure. The lack of additional benefit from an angiotensin converting enzyme inhibitor is consistent with the recently reported PEACE trial.16 Our study is the first large scale, long term community based study to report the effect of different combinations of drugs in the secondary prevention of all cause mortality in patients with ischaemic heart disease. We included patients with multiple comorbidity, elderly people, and women who may have been excluded from previous clinical trials.
The QRESEARCH database was validated by comparing the age-sex structure of the population with the 2001 census, the birth and death rates with figures from the Office for National Statistics, the prescribing rates with prescribing analysis and cost (PACT) data, the consultation rates with data from the general household survey, and prevalence data for common conditions with published data and data from similar databases such as the General Practice Research Database. We found good correspondence for all of these measures (data not shown). We also compared practices taking part in regional research networks on these and other measures and found good correspondence.17 Detailed analyses have shown high levels of completeness and consistency.18 We also carried out an analysis on these data to compare the effect of statins on overall all cause mortality with that reported in the Scandinavian simvastatin survival study1 and found a similar reduction in unselected patients in the community over an eight year period.19
Our study was observational and therefore at risk of bias and confounding. For example, confounding by indication could have occurred if patients with a better prognosis were more likely to be prescribed different combinations of treatments. This is a particular concern with observational studies of intended drug effects.15 If residual confounding explained our results then we would have expected the adjusted odds ratios from the restricted analysis to tend towards one, which was not the case in general. As mortality was high in this cohort, caution is needed in interpreting the odds ratios as relative risks. The measure of deprivation we used was calculated at an area level and there will be some heterogeneity within areas, which may result in some residual confounding.
Our identification of patients for the cohort was based on a diagnostic code for ischaemic heart disease rather than a definition that would have allowed the inclusion of patients prescribed cardiac drugs. Our study was designed in this way as our main exposures were drugs.
What is already known on this topic
Statins are associated with improved survival in patients with ischaemic heart disease
Direct evidence is lacking for the effects of combinations of drugs in cardiovascular disease
What this study adds
Combinations of statins, aspirin, and β blockers improve survival in high risk patients with cardiovascular disease
The addition of an angiotensin converting enzyme inhibitor conferred no additional benefit
Our outcome (whether patients died or not) is likely to be well recorded on the general practice clinical database. In the United Kingdom, a national electronic procedure comes into operation when a patient dies. This automatically updates the patient's electronic health record with the date of death. As our study comprised a nested case-control analysis and data were recorded prospectively, recall bias was not possible as the exposure data were recorded on computer before the date of death or the equivalent date in controls.
Misclassification of exposure status is unlikely as more than 99% of all repeat prescriptions from general practice are recorded on computer, and currently these drugs are not available over the counter. The exception is aspirin, and some patients taking this might have been misclassified on practice databases. This is likely to be a small proportion as patients over 65 are entitled to free prescriptions in the United Kingdom and so tend to have these prescribed rather than buy them. Such misclassification, if present and if non-differential, would have had the effect of biasing the odds ratio towards one, making the exposure seem less protective or less harmful.20 Simvastatin is now also available over the counter, but this will not have affected our results as it was given over the counter status in 2004, after our study had ended.
By excluding patients with a diagnosis of ischaemic heart disease within the first three months of registration with their practice, we reduced possible information bias from pre-existing diseases being recorded as if they were new events at registration.
Although we adjusted for several confounders, residual confounding may have resulted from misclassification of those variables and confounding by unmeasured variables. Such effects would have to be large to account for the substantial protective effects reported here.
We have not investigated the effect of the combination treatments in patients without ischaemic heart disease. Our results should therefore not be taken as evidence that the combination of treatments suggested by Wald et al should be prescribed to all patients over 55.6
Editorial by Fahey et al
We thank practices contributing to QRESEARCH and David Stables (EMIS Computing) for his help and expertise in establishing the database.
Contributors: JHC initiated and designed the study, obtained ethical approval, undertook the data extraction and manipulation and some of the analyses, and drafted the paper. She will act as guarantor for the paper. CC contributed to the study design and core ideas, undertook some of the analyses, advised on interpretation, and contributed to drafting the paper.
Funding: None.
Competing interests: None declared.
Ethical approval: Trent multicentre research ethics committee.
References
- 1.Scandinavian Simvastatin Survival Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study (4S). Lancet 1994;344: 1383-9. [PubMed] [Google Scholar]
- 2.Long-term Intervention with Pravastatin in Ischaemic Heart Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. New Engl J Med 1998;339: 1349-57. [DOI] [PubMed] [Google Scholar]
- 3.Sacks FM, Pfeffer MA, Moye LA. The effects of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. The CARE study. New Engl J Med 1996;335: 1001-9. [DOI] [PubMed] [Google Scholar]
- 4.Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high risk individuals: a randomised placebo-controlled trial. Lancet 2002;360: 7-22.12114036 [Google Scholar]
- 5.Cannon C, Braunwald E, McCabe C, Rader D, Rouleau J, Belder R, et al. Comparison of intensive and moderate lipid lowering with statins after acute coronary syndromes. New Engl J Med 2004; 350. [DOI] [PubMed]
- 6.Wald N, Law M. A strategy to reduce cardiovascular disease by more than 80%. BMJ 2003;326: 1149-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haines A, Jones R. Implementing findings of research. BMJ 1994;308: 1488-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Million Women Study Collaborators. Breast cancer and hormone replacement therapy in the million women study. Lancet 2003;362: 419-27. [DOI] [PubMed] [Google Scholar]
- 9.Hippisley-Cox J, Pringle M, Crown N, Coupland C. Dose hormone replacement therapy protect against ischaemic heart disease? Evidence from a general practice based case control study. Br J Gen Pract 2003;53: 191-6. [PMC free article] [PubMed] [Google Scholar]
- 10.Lagro-Janssen A, Rosser W, van Weel C. Breast cancer and hormone replacement therapy: up to general practice to pick up the pieces. Lancet 2003;362: 414-5. [DOI] [PubMed] [Google Scholar]
- 11.Anon. From research to practice. Lancet 1994;344: 417-8. [PubMed] [Google Scholar]
- 12.Jick H, Zornberg GL, Jick SS, Seshadri S, Drachman DA. Statins and the risk of dementia. Lancet 2000;356: 1627-31. [DOI] [PubMed] [Google Scholar]
- 13.Jick H, Kaye J, Vasilakis-Scaramozza C, Jick S. Risk of venous thromboembolism among users of third generation oral contraceptives compared with users of oral contraceptives with levonorgestrel before and after 1995: cohort and case control analysis. BMJ 2000;321: 1190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hippisley-Cox J, Pringle M, Cater R, Wynn A, Hammersley V, Coupland C, et al. Electronic record in primary care—regression or progression? Cross-sectional survey. BMJ 2003;326: 1439-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMahan AD. Approaches to combat with confounding by indication in observational studies of intended drug effects. Pharmacoepidemiol Drug Saf 2003;12: 551-8. [DOI] [PubMed] [Google Scholar]
- 16.Barnett AH, Bain SC, Bouter P, Karlberg B, Madsbad S, Jervell J, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. [See comment]. New Engl J Med 2004;351: 1952-61. [DOI] [PubMed] [Google Scholar]
- 17.Hammersley V, Hippisley-Cox J, Wilson A, Pringle M. A comparison of research general practices and their patients with other practices—cross sectional survey in Trent. Br J Gen Pract 2002;52: 463-8. [PMC free article] [PubMed] [Google Scholar]
- 18.Hippisley-Cox J, Hammersley V, Pringle M, Coupland C, Crown N, Wright L. How useful are general practice databases for research? Analysis of their accuracy and completeness in one research network. Health Informatics J 2004;10: 91-109. [Google Scholar]
- 19.Hippisley-Cox J, Coupland C. The effect of statins on mortality in patients with ischaemic heart disease: population based cohort study with nested case control analysis. Heart 2005. (in press). [DOI] [PMC free article] [PubMed]
- 20.Rothman K, Greenland S. Modern epidemiology. 2nd ed. Boston: Lippincott-Raven, 1998.