Abstract
Mothers living with HIV (MLWH) experience stressors inherent to parenting, often within a context characterized by poverty, stigma, and/or limited social support. Our study assessed the relationship between parenting stress and child perceptions of family functioning in families with MLWH who have healthy school-age children. MLWH and their children (N = 102 pairs) completed measures addressing parenting stress, and perceptions of family functioning (i.e., parent-child communication, family routines, and family cohesion). We used covariance structural modeling to evaluate the relationship between these factors, with results showing greater maternal parenting stress associated with poorer family functioning outcomes (reported by both the child and the mother). Findings offer support for the parenting stress-family functioning relationship by providing the child perspective along with the maternal perspective, and point to the need for interventions aimed at minimizing the impact of maternal parenting stress on family functioning.
Keywords: family functioning, maternal HIV, parenting stress
Nearly a quarter of people living with HIV in the United States are women (Centers for Disease Control and Prevention [CDC], 2015). In 2010, girls and women ages 13 to 44 accounted for approximately 76% of newly infected women (CDC, 2012), an age span representing prime childbearing and childrearing years. Because women are often the primary caregivers in their families (Henry J. Kaiser Family Foundation, 2006), mothers living with HIV (MLWH) face coping with the physical and psychological impact of a chronic health condition in addition to the stress associated with parenting roles.
The responsibilities of parenthood bring both reward and distress. The demands of being a parent produce a unique type of stress, distinct from that experienced in other life domains and more general major life events (Cooper, McLanahan, Meadows, & Brooks-Gunn, 2009). Because parenting stress is an ongoing within-family process, it is conceptualized as consisting of multiple components, including salient characteristics of the parent, child, and context of the family environment (Reitman, Currier, & Stickle, 2002). Together with external situational variables, such as adverse life events, increased risk for dysfunction is purported to occur through depletion of parents’ emotional resources and limited coping (Abidin, 1995). As such, MLWH are at particularly high risk for parenting stress; they are more likely to be ethnic minorities and to have less education and reduced employment, fewer financial and social resources, and more health or mental health diagnoses than other women (Muze, 2013; Waldrop & Miles, 2009). MLWH are at increased risk for stress and anxiety symptoms (Ivanova, Hart, Wagner, Aljassem, & Loutfy, 2012) and are less likely to demonstrate active coping behaviors (Catz, Gore-Felton, & McClure, 2002). Given this strain, some aspects of positive family functioning are likely to be affected.
Family functioning refers to how a family system typically operates (McCubbin & Thompson, 1991) and includes such characteristics as a sense of cohesion among family members, quality of family relationships/communication, and family structure/routines. While our study examined parenting stress and family functioning in families with an MLWH, the majority of research investigating the relationship between stress and functioning has focused on families with a child suffering from chronic disease or disability (e.g., Gray, Graef, Schuman, Janicke, & Hommel, 2013; Streisand, Kazak, & Tercyak, 2003) and the number of recent studies are limited. For example, in a study of families with an autistic child, the majority of parents reported that parenting stress impacted factors associated with family functioning, such as limited time for family activities, lack of flexibility, and marital strain (Hutton & Caron, 2005). Another study used empirically-derived cut-offs to compare “normal” versus “clinicallyelevated” general family functioning scores in families with a child diagnosed with inflammatory bowel disease; they found significantly greater parenting stress among those with unhealthy levels of family functioning (Gray et al., 2013).
Family cohesion, considered a critical feature of family functioning, is defined as the feeling of togetherness and closeness among family members (Bloom, 1985; Olson, Sprenkle, & Russell, 1979). Studies of families with a child coping with a disability or illness (Johnston et al., 2003; Moreira, Frontini, Bullinger, & Canavarro, 2013), as well as those examining families with healthy children (Brophy-Herb et al., 2013; Shigeto, Mangelsdorf, & Brown, 2014), have found that greater family cohesion is associated with less parental stress. There are far fewer studies, however, that have investigated the effects of parental illness as opposed to child illness on measures of family connectedness or cohesion. Of these, evidence has historically indicated that families coping with parental illness reported lower family cohesion than those with healthy parents (e.g., Dura & Beck, 1988; Peters & Esses, 1985). In addition, physically ill parents have reported experiencing more stress in their parenting roles than healthy parents (Billhult & Segesten, 2003). For MLWH, parenting stress is particularly high due to HIV infection combined with other environmental and mental health risk factors (Ivanova et al., 2012; Muze, 2013); thus, maintaining a cohesive family environment is likely to be challenging for many of these mothers.
While cohesiveness describes the emotional connectivity among family members, open parent-child communication (e.g., expression of needs, discussion of problems) and engagement in family routines (e.g., family meals or bedtime routines) constitute important behavioral components of healthy family functioning (Bandura, Caprara, Barbaranelli, Regalia, & Scabini, 2011; Koome, Hocking, & Sutton, 2012). Parents reporting greater parenting stress have been shown to be less involved in their children’s lives (Crnic & Low, 2002) and were less likely to engage in open parent-child communications (Ponnet et al., 2013). Due to the numerous stressors associated with being infected with HIV, the link between parenting stress and parenting behaviors is particularly profound and requires attention due to the negative impact it can have on the parent-child relationship (Kotchick et al., 1997). A study by Murphy, Marelich, Armistead, Herbeck, and Payne (2010) found that MLWH reporting more stress in their parenting roles and personal health were less likely to engage their children in family routines and more likely to report poorer parent-child communication. Interventions targeting parenting stress and family interactions with MLWH and their children have demonstrated positive outcomes related to reduced stress (Johnson et al., 2015) and improved open communication (Murphy, Armistead, Marelich, Payne, & Herbeck, 2011). Although such behavioral interventions have shown promise in affecting change, little is known regarding the relationship between parenting stress and indicators of family functioning from the child’s perspective.
Our study fills a gap in the literature by investigating the impact of parenting stress, as reported by MLWH, on children’s perceptions of family functioning (i.e., parent-child communication, family routines, and family cohesion). Much of the research on the effects of parenting stress has focused solely on the parent perspective. There is ample evidence, however, that points to marked differences in parent and child perspectives (e.g., Achenbach, McConaughy, & Howell, 1987; De Los Reyes & Kazdin, 2005). Moreover, concordance between parent and child raters in samples with chronically ill parents may create further disparity in perceptions of family connectedness and interactions due to the impact of illness on the parent’s physical abilities and affective states (Armistead, Klein, & Forehand, 1995). Because parental stress has been identified as a potential risk factor for child and adult psychopathology (Costa, Weems, Pellerin, & Dalton, 2006; Gordon & Hinshaw, 2015), findings can inform future services for MLWH and their children by identifying family practices that children perceive as most impaired by maternal stress. Thus, we assessed the influence of parenting stress on family functioning in families with MLWH who had healthy school-age children, focusing first on child perceptions of family functioning, followed by maternal perceptions. We then used covariance structural modeling to construct a latent family functioning construct, with the expectation that increased maternal stress would negatively affect family functioning.
Method
Setting and Sample
We recruited MLWH and their children through HIV service organizations in Los Angeles, CA, and Atlanta, GA, as part of the Teaching, Raising, and Communicating with Kids (TRACK-II) project. TRACK-II is an intervention designed to assist MLWH in disclosing their HIV serostatus to their well children (see Murphy et al., 2011 for pilot study of intervention). Our study used baseline data collected as part of a larger project examining the efficacy of the intervention in increasing the likelihood of maternal disclosure to their children; as such, children had to be unaware of their mothers’ status at the time of study intake. Staff at recruitment agencies described the study to potentially eligible mothers and provided interested mothers with brochures about the study, which included contact information for research study staff. Recruitment materials and information sessions were provided in Spanish and English. Interested mothers contacted research staff who conducted phone screens to determine eligibility. Motherchild dyads were eligible for the TRACK-II study if the mother had a confirmed HIV diagnosis and was the primary caregiver of a well child (without HIV infection) between the ages of 6 and 14, who was residing with her and was unaware of her HIV status. Families had to be fluent in English or Spanish, although only the Los Angeles site enrolled Spanish-speaking participants. No potential participants at the Atlanta site were excluded based on language spoken. The larger, parent study is ongoing and continues to conduct follow-up interviews; however, our study used only baseline data from 102 mother/child pairs.
Procedures
Parents and children provided informed consent and assent, respectively, in order to participate. Families were excluded from the study if the child had a developmental disorder or mental illness that would prevent him/her from participating in the study, based on maternal report. If mothers had more than one well child in the targeted age range, the target child was chosen using random selection. Of the MLWH who were screened, approximately 53% were eligible for participation. The most common reason for ineligibility was that they had already disclosed their HIV status to their children.
All procedures were approved by the Institutional Review Boards at Georgia State University and University of California, Los Angeles (UCLA). Interviewers were trained on a range of topics, including recruitment, informed consent, confidentiality, conducting young child interviews, triage of emergency cases, the computerized interviewing program, and tracking and retention. Interviews were conducted using computer-assisted personal interviewing (CAPI), which involved having an interviewer read each question aloud to the participant and enter the participant’s data directly into a laptop computer. Consent/assent and interviews were conducted in the participant’s preferred language (English or Spanish), and took place at the participant’s home, the recruitment site, or at a participant-preferred location with sufficient privacy.
Standard Spanish versions of measures were used when available (i.e., Parenting Stress Index). The other measures were translated by the Worldwide Translation Center (WTC) in San Diego, CA. A team of three translators (1 translator and 2 editors) conducted the translations and analyzed the measures for accuracy, grammar, and style. Additionally, a blind back-translation was conducted by a translator at UCLA, using procedures described by Marin and Marin (1991).
Mother interviews typically lasted 75 minutes, and child interviews lasted approximately 45 minutes. Mothers were paid $60 USD in cash for each assessment, and children were given a $30 USD gift card. The UCLA Institutional Review Board reviewed all participant reimbursements to ensure that they were within a typical range for U.S. research studies; the mother and child payments were approved as standard compensation.
Child and Maternal Measures
Parenting stress
The Parenting Stress Index (Abidin, 1990) was developed for early identification of stressful parent-child systems, and was completed only by mothers as it was used as our main predictor for both child- and maternal-report models. Higher scores were indicative of higher levels of stress. Cronbach’s alpha in our sample was .93.
Family cohesion
The Cohesion subscale from the Family Functioning Scale (Bloom & Naar, 1994) rated the degree to which specific family characteristics were like the participant’s family, with higher scores indicating a more cohesive family style. The scale was completed by both the child and her/his mother. The two negatively worded items were excluded from the analysis, with Cronbach’s alphas of .70 for child-report, and .82 for maternal-report.
Family routines
A subset of questions from the Child Routines Inventory (Sytsma, Kelley, & Wymer, 2001) was administered to children and their mothers. Cronbach’s alpha was .78 for child-report, and .88 for maternal-report.
Parent-child communication
The Parent-Child Communication Scale (Loeber, Farrington, Stouthamer-Loeber, & Van Kammen, 1998) was administered to children, with higher values indicating better communication. Cronbach’s alpha was .71 for this sample. For maternal assessment, the Loeber measure was not available. Instead, the Parent-Adolescent Communication Scale was used, consisting of seven items, excluding those negatively worded from the original scale (Miller, Forehand, & Kotchick, 1999). Reliability was .86.
Analysis
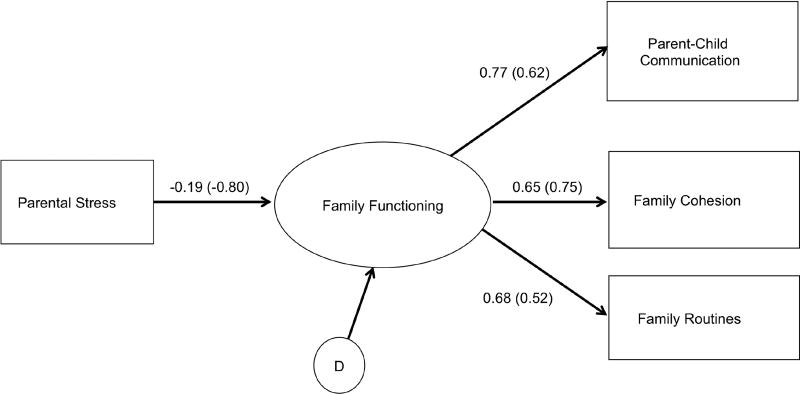
First, correlations between measures intended to assess factors associated with family functioning were evaluated along with maternal stress. Then, covariance structural modeling was applied using structural equation modeling (EQS; Bentler, 2006), forming a latent construct reflecting family functioning from parent/child communication, family cohesion, and routines (see Figure 1). A bootstrap procedure was adopted for model verification (Nevitt & Hancock, 2001), requesting 500 samples with the N set at our study’s sample size (Bentler, 2006) in order to assess model robustness.
Figure 1.
Standardized Covariance Structural Model effects for parental stress on child and MLWH perceptions of family functioning.
Note: All parameters (standardized) are significant at p < .05 or better. Values in parentheses are for the MLWH perception model. Family Routines for both modes was fixed at 1.00 for identification purposes. Disturbance terms (D) are 0.98 for child-report model, and 0.60 for maternal-report. Child-model n = 102; Maternal-model n = 101. For child report, the Loeber et al. (1998) Parent-Child Communication Scale was used; for maternal report, the Miller et al. (1999) Parent-Adolescent Communication Scale was used; MLWH = mothers living with HIV.
Results
Mean age for mothers in our study was 38.6 years (SD = 7.5), and 37% of mothers self-identified as Hispanic, 55% as African American, 2% as White (not Hispanic), 1% as Asian, and 5% as mixed or other. The largest percentage (41%) of mothers had never been married, 22% were currently married, 16% were separated, 15% were divorced, and 7% were widowed. Fiftysix percent had at least a high school education, with 35% attending college or vocational school. Approximately 29% of mothers reported being employed in the past 30 days, and the mean total monthly income was $1,420 USD (SD = 935). On average, mothers had been aware of their HIV status for 8.26 years. The vast majority of mothers in this sample were healthy. Of those able to report, 13% had very low CD4+ T cell counts (< 200 cells/mm3), and 15% had low CD4+ T cell counts (200–400 cells/mm3). For viral load, only 3% reported values higher than 2,000 copies/mL; 82% reported values in the undetectable range (< 50 copies/mL). Seven percent self-assessed their health as poor whereas 75% believed their health was good, very good, or excellent.
The mean age for children at baseline was 9.7 years (SD = 2.5), and 50% were female. Children’s racial/ethnic identifications included Hispanic (38%), African American (55%), White non-Hispanic (1%), Asian (1%), and mixed or other (5%). Neither significant (p < .05) associations nor differences were noted for child’s age, race (Hispanic vs. non-Hispanic), or gender on the parenting stress.
Table 1 contains variable means, standard deviations, correlations, and covariances used for the child- and maternal-report models. For child-report, family functioning variables showed large effect associations with each other and small effect associations with parental stress (based on r of .10, .30, and .50 for small, medium, and large effects; Cohen, 1992). For maternal report (due to missing data on 1 case, n = 101), the family functioning variables showed medium-large effect associations with each other, and medium-large effect associations with parenting stress. Overall, higher parental stress was associated with lower levels of family routines, parent-child communication, and cohesion. Within the family functioning variables, those reporting a greater number of family routines also reported more family cohesion and higher levels of parent-child communication. In addition, greater family cohesion was associated with better parent-child communication.
Table 1.
Observed Covariances and Correlations, Means, and Standard Deviations for Parental Stress and Family Functioning Measures, Childa and Maternal Report
| Parenting Stress | Routines | Cohesion | Communication | |
|---|---|---|---|---|
| Child Report (n = 102) | ||||
| Parenting Stressa | 527.32 | −.11 | −.19 | −.11 |
| Routines | −30.54 | 139.79 | .43 | .53 |
| Cohesion | −10.16 | 12.02 | 5.58 | .50 |
| Communicationb | −19.51 | 46.28 | 8.73 | 55.17 |
| Mean (SD) | 77.58 (22.96) | 61.67 (11.82) | 9.46 (2.36) | 36.93 (7.43) |
|
| ||||
| Maternal Report (n = 101) | ||||
| Parenting Stress | 518.33 | −.38 | −.61 | −.50 |
| Routines | −113.27 | 171.26 | .40 | .37 |
| Cohesion | −27.95 | 10.67 | 4.09 | .43 |
| Communicationb | −44.33 | 18.81 | 3.40 | 15.12 |
| Mean (SD) | 77.95 (22.77) | 62.02 (13.09) | 9.66 (2.02) | 23.14 (3.89) |
Note: Covariances are in the lower diagonal; variances along the diagonal; correlations in upper diagonal.
Parenting stress is based on maternal-report only.
For child report, the Loeber et al. (1998) Parent-Child Communication Scale was used; for maternal report, the Miller et al. (1999) Parent-Adolescent Communication Scale was used.
Child-Report Model
For the proposed covariance structural model, error variances for the endogenous variables were allowed to vary as was the disturbance term for the family functioning construct. As is standard practice in covariance structural models (Byrne, 2006), one parameter for the family functioning construct was set to 1.0 for identification purposes (here, family routines) and disturbance term estimation. Model fit was assessed using robust fit statistics, which provided better standard error estimates and accounted for issues with non-normal data and small sample size (Bentler, 2006). Fit statistics included the Satorra-Bentler Scaled χ2, the Yuan-Bentler Residual-Based F statistic, the Comparative Fit Index (CFI), the Incremental Fit Index (IFI), the Non-Normed Fit Index (NNFI), and the Root Mean Squared Error of the Approximation (RMSEA). Values for the CFI at .95 or higher are indicative of good model fit, and a cutoff of .06 or smaller indicate good model fit for the RMSEA (Hu & Bentler, 1999). Regarding the NNFI, values in the mid .90s ranging up to 1.0 indicate good fit (Raykov & Marcoulides, 2006). For the IFI, values close to 1.0 indicate good model fit (Bollen, 1990), with a .95 cutoff often adopted.
Figure 1 illustrates the model results using standardized parameter estimates, showing good fit as evidenced by a Satorra-Bentler Scaled χ2 of 1.26 (df = 2) and the Yuan-Bentler Residual-Based F statistic (F[2, 100] = .86, p = .42). The CFI, NNFI, and IFI all were 1.0, and the RMSEA was 0.001 (90% CI = .001 to .17). No model modifications were required. A bootstrap procedure was used to evaluate the robustness of the model fit statistics and parameters (Nevitt & Hancock, 2001; see also Bentler, 2006). Results showed 495 converged replications out of 500, with all model parameters and fit statistics falling within the 95% confidence range of the bootstrap models. Overall, results suggested that increased maternal parenting stress negatively affected family functioning (represented by parent-child communication, routines, and family cohesion) as reported by the child.
Maternal-Report Model
The maternal-report model was next evaluated. The same model restrictions used for the child model were applied, with error variances and the disturbance term allowed to vary, and one parameter on the family functioning construct set to 1.0 for identification purposes. Fit was assessed in the same manner using the Satorra-Bentler Scaled χ2, the Yuan-Bentler Residual-Based F statistic, the CFI, IFI, NNFI, and RMSEA.
As with the child-report model, the maternal-report model showed good fit, with a Satorra-Bentler Scaled χ2 of 1.07 (df = 2), and Yuan-Bentler Residual-Based F statistic (F[2, 99] = .51, p = .60). All parameter estimates were significant at the .05 or better level (see Figure 1 for parameter estimates in parentheses). The CFI, NNFI, and IFI were 1.0, and the RMSEA was .001 (90% CI = .001 to .16). No model modifications were required. Bootstrap analyses for the maternal-report showed 499 replications out of 500. As with the child-report model, all model parameters and fit statistics fell within the 95% confidence range of the bootstrap models. Parenting stress was negatively associated with family functioning as reported by mothers.
Discussion
This study was the first to investigate, from the child’s perspective, the outcomes of maternal stress on family functioning in a sample of children affected by maternal HIV. In addition, a geographically (Los Angeles and Atlanta) and ethnically diverse sample of children and their MLWH, participated in the study. As hypothesized, parenting stress was significantly negatively associated with the family functioning latent construct, both from the child and maternal perspectives. Thus far, the literature examining parenting stress and family functioning variables (cohesion, routines, communication) has overwhelmingly focused on home environments in which the child was ill (e.g., Gray et al., 2013; Johnston et al., 2003; Moreira et al., 2013; Streisand et al., 2003). Among families with a parent suffering from chronic disease or disability, those with chronic illnesses were more likely to experience stress in their parenting roles (Billhult & Segesten, 2003) and reported less emotional engagement than healthy parents (Dura & Beck, 1988; Peters & Esses, 1985). Our study’s unique examination of the child’s point-of-view on the components of family functioning in families with a chronically ill parent, specifically MLWH, highlighted how a child’s family experience and home life can be influenced by maternal distress.
Consistent with findings from our previous work with other samples of MLWH and their children (Murphy, Marelich, Herbeck & Payne, 2009), we found that greater engagement in family routines was associated with better family cohesion and better parent-child communication. Further, greater family cohesion was related to better parent-child communication. These family behaviors provide the foundation that children need for healthy relationships and better problem solving and coping skills as they develop (Huff, Widner, & McCoy, 2003). Family routines are critical in establishing a child’s sense of predictability and security, and are linked to fewer behavioral problems. In families with more frequent family routines, children and young adolescents exhibit lower rates of aggressive behavior, anxiety/worry, depressive symptoms, conduct disorder behaviors, and binge drinking (Murphy et al., 2009). Moreover, among well children living with MLWH, children experiencing a home with more frequent routines also reported better self-concept scores when compared to adolescents in families with a lower frequency of family routines (Murphy et al., 2009). Additionally, MLWH who were more stressed in their parental roles also reported poorer parenting skills – specifically related to engaging children less frequently in family routines, poorer parent-child communication, and poorer and less consistent parenting discipline (Murphy et al., 2010).
Our study indicated that young children were aware that communication with their mothers may have felt insufficient, that family routines were not carried out either frequently or well, and that they did not feel close to their MLWH or family at times. However, an interesting question remained: whether the children were aware in any sense that these outcomes were occurring partially due to maternal parenting stress. We did not design this study to answer that question, but future research may delve deeper into this area. Regardless, it is important for mothers to know that these links exist and that children—even young children—are well aware of family changes when their mothers experience parenting stress. In our experience, MLWH in family interventions have been more likely to work diligently at strategies (i.e., to reduce parenting stress) if they understand that the stress not only affected them, but also affected their children’s perceptions of the family in numerous arenas.
Our findings offer support for the parenting stress-family functioning relation from the child’s perspective and indicated that, in families in which MLWH were experiencing high parenting stress, children were observing and experiencing various aspects of poorer family functioning. Parenting interventions for MLWH need to provide skills for implementation of family routines, and assist with strategies for older children or other support figures to maintain family routines if MLWH are unable to do so (e.g., illness, hospitalization, fatigue). Future services informed by the child’s perceptions of aspects of family functioning under strain could potentially reduce the risk for child and adult psychopathology related to maternal stress.
While offering a new perspective on the roles of maternal parenting stress in family functioning, this study is not without limitations. The convenience sample (taken from the larger, TRACK-II maternal HIV disclosure intervention study) consisted only of families in which the mother had not disclosed her HIV status to the participating child. Parenting stress and family functioning may operate differently in families in which disclosure has occurred. Additionally, constructs were exclusively based on self-report; however, relations between constructs were consistent across mother and child report. Furthermore, the sample offered greater diversity across geographic and ethnic/racial domains than is often seen in the extant literature, but primarily African American and Latino mothers, to the exclusion of fathers living with HIV, comprised the sample, and generalization to other populations may be limited.
Although we report full demographics for individuals who participated in the study, we did not have detailed information on those who were ineligible. However, given that recruitment took place in various clinics and outreach programs that consisted of rather static background characteristics, those who were unable to participate in the study were likely to have been similar to those who did participate. Finally, according to the most recent U.S. Department of Health and Human Services (2017) poverty guidelines, the poverty threshold for American families consisting of three persons was $1,701 USD per month; our sample’s average total monthly income was reported at $1,420 USD. Although this comparison only gave a rough estimate of our sample’s socioeconomic status within the contiguous United States (i.e., did not account for geographic variations in cost of living, fewer or more individuals within the household), it did provide a general context of financial strain.
The children in our study reinforced previously identified points of intervention for families affected by HIV. MLWH may benefit from individual- or family-based interventions aimed at reducing parenting stress and maintaining family functioning even under times of parenting stress. Moreover, due to ongoing environmental and cultural changes, it is important that studies examining the relationship between parenting stress and family functioning continue. Current literature addressing these constructs in families affected by parental illness, however, is limited. We believe this gap in the literature is part of what makes our study significant and suggest future research continue to investigate this dynamic relationship.
Conclusions
We used covariance structural modeling to evaluate the relationship between parenting stress and factors of family functioning (i.e., parent-child communication, family routines, and family cohesion) in families with MLWH who had healthy school-age children. We found that greater maternal parenting stress was associated with poorer family functioning outcomes, as reported by both the child and the mother. Our findings offer support for the parenting stress-family functioning relationship by providing the child perspective, a viewpoint often neglected in the literature. Our study highlighted the importance of interventions aimed at reducing maternal stress among MLWH as a means for positively impacting children’s experiences within the family.
Key Considerations.
Mothers living with HIV (MLWH) are believed to be at greater risk for parenting stress due to poverty, stigma, and/or limited social support.
Increased parental stress has been associated with negative parenting beliefs and behaviors; however, existing literature has neglected to examine this relationship from the child’s perspective.
In our study, greater parenting stress was associated with poorer family functioning outcomes based on both child and maternal report.
These findings support a parenting stress-family functioning relationship from the child perspective and highlight the need for interventions to address parental stress in MLWH.
Acknowledgments
Research reported in this manuscript was supported by the National Institute of Mental Health of the National Institutes of Health by Grant Numbers 5R01MH094148 (PI: Marya T. Schulte) and 5R01MH094233 (PI: Lisa P. Armistead). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Contributor Information
Marya T. Schulte, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, Los Angeles, California, USA (mtschulte@ucla.edu).
Lisa Armistead, Department of Psychology, Georgia State University, Atlanta, Georgia, USA.
William D. Marelich, Department of Psychology, California State University, Fullerton, Fullerton, California, USA.
Diana L. Payne, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, Los Angeles, California, USA.
Nada M. Goodrum, Department of Psychology, Georgia State University, Atlanta, Georgia, USA.
Debra A. Murphy, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, Los Angeles, California, USA.
References
- Abidin RR. Parenting Stress Index manual. Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- Abidin RR. Parenting Stress Index (3rd ed.): Professional manual. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Armistead L, Klein K, Forehand R. Parental physical illness and child functioning. Clinical Psychology Review. 1995;15:409–422. [Google Scholar]
- Bandura A, Caprara GV, Barbaranelli C, Regalia C, Scabini E. Impact of family efficacy beliefs on quality of family functioning and satisfaction with family life. Applied Psychology. 2011;60:421–448. [Google Scholar]
- Bentler PM. EQS 6 Structural equations modeling program manual. Encino, CA: Multivariate Software, Inc; 2006. [Google Scholar]
- Billhult A, Segesten K. Strength of motherhood: Non-recurrent breast cancer as experienced by mothers with dependent children. Scandinavian Journal of Caring Sciences. 2003;17:122–128. doi: 10.1046/j.1471-6712.2003.00219.x. [DOI] [PubMed] [Google Scholar]
- Bloom BL. A factor analysis of self-report measures of family functioning. Family Process. 1985;24:225–239. doi: 10.1111/j.1545-5300.1985.00225.x. [DOI] [PubMed] [Google Scholar]
- Bloom BL, Naar S. Self-report measures of family functioning: Extensions of a factorial analysis. Family Process. 1994;33:203–216. doi: 10.1111/j.1545-5300.1994.00203.x. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Overall fit in covariance structure models: Two types of sample size effects. Psychological Bulletin. 1990;107:256–259. [Google Scholar]
- Brophy-Herb HE, Martoccio TL, Hillaker B, Stansbury KE, Harewood T, Senehi N, Fitzgerald H. Profiles of low-income maternal well-being and family climate: Relations to toddler boys’ and girls’ behaviors. Family Relations. 2013;62(2):326–340. [Google Scholar]
- Byrne BM. Structural equation modeling with EQS: Basic concepts, applications, and programming. 2. New York, NY: Psychology Press; 2006. [Google Scholar]
- Catz SL, Gore-Felton C, McClure JB. Psychological distress among minority and low-income women living with HIV. Behavioral Medicine. 2002;28:53–59. doi: 10.1080/08964280209596398. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance supplemental report. 2012 Retrieved from https://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf.
- Centers for Disease Control and Prevention. HIV surveillance report, 2013. 2015 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2013-vol-25.pdf.
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cooper CE, McLanahan SS, Meadows SO, Brooks-Gunn J. Family structure transitions and maternal parenting stress. Journal of Marriage and Family. 2009;71:558–574. doi: 10.1111/j.1741-3737.2009.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa NM, Weems CF, Pellerin K, Dalton R. Parenting stress and childhood psychopathology: An examination of specificity to internalizing and externalizing symptoms. Journal of Psychopathology and Behavioral Assessment. 2006;28:113–122. [Google Scholar]
- Crnic KA, Low C. Everyday stresses and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 5. Practical issues in parenting. Mahaway, NJ: Erlbaum; 2002. pp. 243–267. [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dura JR, Beck SJ. A comparison of family functioning when mothers have chronic pain. Pain. 1988;35:79–89. doi: 10.1016/0304-3959(88)90279-5. [DOI] [PubMed] [Google Scholar]
- Gordon CT, Hinshaw SP. Parenting stress as a mediator between childhood ADHD and early adult female outcomes. Journal of Clinical Child and Adolescent Psychology. 2015;6(1):1–12. doi: 10.1080/15374416.2015.1041595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray WM, Graef DM, Schuman SS, Janicke DM, Hommel KA. Parenting stress in pediatric IBD: Relations with child psychopathology, family functioning, and disease severity. Journal of Developmental and Behavioral Pediatrics. 2013;34:237–244. doi: 10.1097/DBP.0b013e318290568a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry J. Kaiser Family Foundation. Women and HIV/AIDS in the United States. HIV/AIDS policy fact sheet. 2006 Retrieved from http://www.kff.org/hivaids/upload/6092-03.pdf.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Huff C, Widner M, McCoy K. The influence of challenging outdoor recreation on parent-adolescent communication. Therapeutic Recreation Journal. 2003;37:18–37. [Google Scholar]
- Hutton AM, Caron SL. Experiences of families with children with autism in rural New England. Focus on Autism and Other Developmental Disabilities. 2005;20:180–189. [Google Scholar]
- Ivanova EL, Hart TA, Wagner AC, Aljassem K, Loutfy MR. Correlates of anxiety in women living with HIV of reproductive age. AIDS Behavior. 2012;16:2181–2191. doi: 10.1007/s10461-011-0133-6. [DOI] [PubMed] [Google Scholar]
- Johnson ER, Davies SL, Aban I, Mugavero MJ, Shrestha S, Kempf M-C. Improving parental stress levels among mothers living with HIV: A randomized control group intervention study. AIDS Patient Care and STDs. 2015;29:220–228. doi: 10.1089/apc.2014.0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston C, Hessl D, Blasey C, Eliez S, Erba H, Dyer-Friedman J, Reiss AL. Factors associated with parenting stress in mothers of children with Fragile X syndrome. Journal of Developmental and Behavioral Pediatrics. 2003;24:267–275. doi: 10.1097/00004703-200308000-00008. [DOI] [PubMed] [Google Scholar]
- Koome F, Hocking C, Sutton D. Why routines matter: The nature and meaning of family routines in the context of adolescent mental illness. Journal of Occupational Science. 2012;19:312–325. [Google Scholar]
- Kotchick BA, Forehand R, Brody G, Armistead L, Simon P, Morse E, Clark L. The impact of maternal HIV-infection on parenting in inner-city African American families. Journal of Family Psychology. 1997;11:447–461. [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. Mahwah, NJ: Erlbaum; 1998. [Google Scholar]
- Marin G, Marin B. Research with Hispanic populations. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- McCubbin H, Thompson A, editors. Family assessment inventories for research and practice. 2. Madison, WI: University of Wisconsin; 1991. [Google Scholar]
- Miller KS, Forehand R, Kotchick BA. Adolescent sexual behavior in two ethnic minority samples: The role of family variables. Journal of Marriage and the Family. 1999;61:85–98. [Google Scholar]
- Moreira H, Frontini R, Bullinger M, Canavarro MC. Caring for a child with Type 1 diabetes: Links between family cohesion, perceived impact, and parental adjustment. Journal of Family Psychology. 2013;27:731–742. doi: 10.1037/a0034198. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Armistead L, Herbeck DM, Payne DL. Anxiety/stress among mothers living with HIV: Effects on parenting skills & child outcomes. AIDS Care. 2010;22:1449–1458. doi: 10.1080/09540121.2010.487085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Herbeck DM, Payne DL. Family routines and parental monitoring as protective factors among early/middle adolescents affected by maternal HIV/AIDS. Child Development. 2009;80:1676–1691. doi: 10.1111/j.1467-8624.2009.01361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Armistead L, Marelich WD, Payne DL, Herbeck DM. Pilot trial of a disclosure intervention for HIV+ mothers: The TRACK program. Journal of Consulting and Clinical Psychology. 2011;79:203–214. doi: 10.1037/a0022896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muze R. Parenting and child outcomes of HIV-infected African American mothers: A literature review. Journal of Community Health Nursing. 2013;30:164–171. doi: 10.1080/07370016.2013.806704. [DOI] [PubMed] [Google Scholar]
- Nevitt J, Hancock GR. Performance of bootstrapping approaches to model test statistics and parameter standard error estimation in structural equation modeling. Structural Equation Modeling. 2001;8:353–377. [Google Scholar]
- Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family systems: I. Cohesion and adaptability dimensions, family types, and clinical applications. Family Process. 1979;18:3–28. doi: 10.1111/j.1545-5300.1979.00003.x. [DOI] [PubMed] [Google Scholar]
- Peters LC, Esses LM. Family environment as perceived by children with a chronically ill parent. Journal of Chronic Diseases. 1985;38:301–308. doi: 10.1016/0021-9681(85)90076-1. [DOI] [PubMed] [Google Scholar]
- Ponnet K, Wouters E, Mortelmans D, Pasteels I, De Backer C, Van Leeuwen K, Van Hiel A. The influence of mothers’ and fathers’ parenting stress and depressive symptoms on own and partner’s parent-child communication. Family Process. 2013;52:312–324. doi: 10.1111/famp.12001. [DOI] [PubMed] [Google Scholar]
- Raykov T, Marcoulides GA. A first course in structural equation modeling. 2. Mahwah, NJ: Erlbaum; 2006. [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Shigeto A, Mangelsdorf SC, Brown GL. Roles of family cohesiveness, marital adjustment, and child temperament in predicting child behavior with mothers and fathers. Journal of Social and Personal Relationships. 2014;31:200–220. [Google Scholar]
- Streisand R, Kazak AE, Tercyak KP. Pediatric-specific parenting stress and family functioning in parents of children treated for cancer. Children’s Health Care. 2003;32:245–256. [Google Scholar]
- Sytsma SE, Kelley ML, Wymer JH. Development and initial validation of the child routines inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23:241–251. doi: 10.1007/s10862-022-10007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Annual update of the HHS Poverty Guidelines. 2017 Retrieved from https://www.gpo.gov/fdsys/pkg/FR-2017-01-31/pdf/2017-02076.pdf.
- Waldrop J, Miles MS. Sources of distress for southern African American mothers with HIV. The Source. 2009;19:12–15. [Google Scholar]