Abstract
Background
Gross trunnion failure (GTF) is a rare complication in total hip arthroplasty reported across a range of manufacturers. Specific lots of the Stryker LFIT Anatomic cobalt chromium alloy (CoCr) V40 femoral head were recalled in August of 2016. In part, the recall was based out of concerns for disassociation of the femoral head from the stem and GTF.
Methods
We report on 28 patients (30 implants) with either GTF (n=18) or head-neck taper corrosion (n=12) of the LFIT CoCr femoral head and the Accolade TMZF femoral stems. All of these cases were associated with adverse local tissue reaction (ALTR) requiring revision of the THA.
Results
In our series, a conservative estimate of the incidence of failure was 4.7% (n = 636 total implanted) at 8.0±1.4 years from the index procedure. Failures were associated with a high offset 127° femoral stem nec k angle and increased neck lengths. 43.3% (13/30) of the observed failures included implant sizes outside of the voluntary recall (27.8% (5/18) of the GTF and 75.0% (8/12) of the taper corrosion cases). Serum cobalt and chromium levels were elevated (Cobalt: 8.4±7.0μg/mL; Chromium: 3.4±3.3μ/L; Cobalt/Chromium ratio: 3.7). MARS MRI demonstrated large cystic fluid collections typical with ALTR. During revision, a pseudotumor was observed in all cases. Pathology suggested a chronic inflammatory response. Impending GTF could be diagnosed based on aspiration of black synovial fluid and an oblique femoral head as compared to the neck taper on radiographs.
Conclusion
In our series of the recalled LFIT CoCr femoral head, the risk of impending GTF or head-neck taper corrosion should be considered as a potential diagnosis in a painful Accolade TMZF THA with unknown etiology. Almost half of the failures we observed included sizes outside of the voluntary recall.
Keywords: Recall, gross trunnion failure, trunnion corrosion, head-neck taper corrosion, total hip arthroplasty, adverse local tissue reaction, ALTR
Introduction
Cobalt chromium alloy (CoCr) has been the primary material used for femoral heads in modern day total hip arthroplasty (THA). Its material properties to resist wear and corrosion make it an ideal choice as a bearing surface. The overall longevity and survival of CoCr heads on cementless titanium alloy stems in prospective, registry, and retrospective studies is impressive at more than 80% with 15 to 25 years follow-up[1–3].
A disadvantage of CoCr femoral heads is increased concerns with adverse local tissue reaction (ALTR) from corrosion or wear debris at the trunnion interface. After its initial description in metal-on-metal bearing surfaces[4, 5], ALTR has been associated, as a rare event, at the head-neck interface between a CoCr femoral head and titanium femoral stem[6]. Clinical studies have reported ALTR association with head-neck taper corrosion[6, 7] and with gross trunnion failure (GTF)[8]. A small series of cases involving GTF with the Low Friction Ion Treatment (LFIT) CoCr femoral head and the Accolade titanium-molybdenum-zirconium-iron alloy (TMZF) stem, as well as other designs, has also been reported[9, 10].
The Stryker LFIT Anatomic CoCr V40 femoral head had a limited voluntary recall in August 2016. Recalled lots included femoral heads diameter and offsets of 36+5, 40+4, 40+8, 40+12, 44+4, 44+8, and 44+12 (head diameter, neck offset). Other remaining femoral head sizes have not been recalled. One of the reported hazards noted was disassociation of the femoral head-stem and GTF. There is limited data on the initial evaluation of these cases, on the ability to preoperative plan for head-liner verses femoral stem revision, and on how to diagnose possible impending failure.
We report on thirty revisions associated with ALTR between the LFIT femoral head and Accolade TMZF femoral stem. These revised implants involved femoral heads sizes that are outside of the recall. An additional mode of failure that is not listed as a potential hazard on the recall, head-neck taper corrosion, was included to investigate its potential association with the recall. The purpose of this report is to describe the presentation, diagnosis, and intraoperative findings of these cases, and report on our experience in diagnosing possible impending trunnion failure.
Methods
Study Population
After receiving institutional review board approval, we retrospectively reviewed 28 patients that underwent a THA with an LFIT femoral head and Accolade TMZF femoral stem that subsequently presented with GTF or head-neck taper corrosion and underwent revision arthroplasty (n=30). Surgical revision was completed by one of three fellowship trained arthroplasty surgeons from February 2012 to October 2016. Inclusion criteria included all patients identified with GTF or head-neck taper corrosion at the time of revision surgery. GTF was defined as all THA patients where the femoral head had disassociated from the femoral neck morse taper secondary to gross loss of material volume at the femoral neck trunnion interface[8]. Diagnosis was made with radiographs at presentation and confirmed during revision arthroplasty of the failed femoral stem.
Head-neck taper corrosion was identified based on a combination of painful THA with elevated serum cobalt and chromium levels, evidence of ALTR on metal artifact reduction (MARS) magnetic resonance imaging (MRI), and intraoperative observation of black corrosion debris on the trunnion interface. At the time of surgery, ALTR was judged to be present to some degree in all cases based on intraoperative observation. ALTR was defined as the presence of fluid, necrotic soft tissue destruction, “pseudotumor”, and osteolysis[11, 12]. The surface of capsular tissue was black in cases of GTF, consistent with metallic debris.
Index Surgical Procedure
The initial index surgical procedure was between October 1999 and November 2007 using a cementless THA with a metal-on-polyethylene bearing surface. During this period, THA was performed using a single implant combination, a LFIT CoCr femoral head and an Accolade TMZF tapered wedge stem (Stryker Orthopaedics, Mahwah, New Jersey). All implants used a high offset 127° f emoral stem neck angle, a 36mm diameter femoral head, and a range of femoral neck lengths of -5 (n=2), +0 (n=4), +5 (n=17), and +10 (n=7). The implant was used during a time period of 2.5 years by a single, fellowship trained surgeon in our practice using a posterior approach, with the last implant placed in 2007. During this time period, there were 636 Accolade TMZF femoral stems with LFIT CoCr femoral heads implanted at our institution.
Surgical Revision
For patients diagnosed with GTF, surgical revision included removal of the femoral stem as the trunnion was severely damaged. A posterior approach was utilized, and a complete synovectomy was performed with removal of abnormal hypertophic tissue. An extended trochanteric osteotomy was used in three cases to remove the stem, and, in the remainder of cases, the stem could be removed with either flexible osteotomes or a variation of the “top-out” method for removal of femoral stems[13]. A modular revision femoral stem was used with a BIOLOX delta ceramic femoral head (CeramTec, Plochingen, Germany). In one case, the acetabular component needed to be revised as there was damage to the polyethylene liner locking mechanism from abrasion with the disassociated trunnion (case 5).
In cases involving head-neck taper corrosion, surgical revision included an exchange of the femoral head and polyethylene liner. The femoral stems and acetabular components were well fixed. A bovie scratch pad was used to remove the black corrosion precipitate from the stem taper. A titanium-alloy adapter sleeve with a BIOLOX OPTION delta ceramic femoral head (CeramTec, Plochingen, Germany) was inserted over the existing taper. This combination was selected out of concerns for an additional modular junction of a cobalt alloy and possible fracture of the ceramic head on a damaged taper[6, 14].
Statistical Analysis
Demographic characteristics of our sample participants were analyzed using univariate descriptive statistics. Means and standard deviations were calculated for approximately normally distributed variables; medians and inter-quartile ranges (IQRs) were computed for continuous variables with skewed distributions. Frequencies and percentages were determined for categorical variables, and double-tailed Fisher’s exact test was used to test for statistical significance in these cases.
Results
Incidence and Presentation
In our series, the overall incidence of revision due to GTF or ALTR and head-neck taper corrosion was conservatively estimated at 30/636 (4.7%). In the GTF group, 5/18 failures (27.8%) included head sizes not listed on the recall. In the head-neck taper corrosion group, 8/12 failures (75.0%) included head sizes not listed on the recall (Table 1). The difference in incidence between the GTF and taper corrosion groups was not significant (p = 0.06).
Table 1.
Demographics, Patient, and Implant Characteristics
| Case | Failure Type | Age | Gender | BMI | Time to Failure (yr) | Follow Up (yr) | Accolade Stem | Head Size | Neck Offset | Recalled |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | GTF | 63 | Male | 28.2 | 9.6 | 1.2 | 127° Neck | 36 | (+) 5 | Yes |
| 2 | GTF | 66 | Male | 41.5 | 8.3 | 1.5 | 127° Neck | 36 | (+) 5 | Yes |
| 3 | GTF | 82 | Male | 25.6 | 9.3 | 1.8 | 127° Neck | 36 | (+) 5 | Yes |
| 4 | GTF | 50 | Male | 29.6 | 9.5 | 1.8 | 127° Neck | 36 | (+) 0 | No |
| 5 | GTF | 50 | Female | 53.6 | 8.8 | 1.8 | 127° Neck | 36 | (+) 10 | No |
| 6 | GTF | 65 | Male | 41.5 | 7.8 | 2.4 | 127° Neck | 36 | (+) 5 | Yes |
| 7 | GTF | 73 | Male | 28.6 | 7.9 | 2.9 | 127° Neck | 36 | (+) 10 | No |
| 8 | GTF | 79 | Male | 27.6 | 8.0 | 2.9 | 127° Neck | 36 | (+) 10 | No |
| 9 | GTF | 63 | Male | 25.8 | 7.6 | 3.5 | 127° Neck | 36 | (+) 5 | Yes |
| 10 | GTF | 65 | Male | 30.0 | 7.8 | 3.5 | 127° Neck | 36 | (+) 5 | Yes |
| 11 | GTF | 56 | Female | 27.4 | 6.3 | 3.7 | 127° Neck | 36 | (+) 5 | Yes |
| 12 | GTF | 69 | Male | 29.5 | 4.7 | 4.7 | 127° Neck | 36 | (+) 5 | Yes |
| 13 | GTF | 80 | Male | 22.7 | 11.0 | 0.3 | 127° Neck | 36 | (+) 10 | No |
| 14 | GTF | 80 | Female | 33.7 | 9.4 | 0.6 | 127° Neck | 36 | (+) 5 | Yes |
| 15 | GTF | 68 | Female | 31.9 | 9.0 | 0.7 | 127° Neck | 36 | (+) 5 | Yes |
|
| ||||||||||
| 16 | GTF | 82 | Male | 31.9 | 10.5 | 0.0 | 127° Neck | 36 | (+) 5 | Yes |
| 17 | Impending GTF | 89 | Male | 25.0 | 10.9 | 0.1 | 127° Neck | 36 | (+) 5 | Yes |
| 18 | Impending GTF | 76 | Male | 31.9 | 10.1 | 0.0 | 127° Neck | 36 | (+) 5 | Yes |
|
| ||||||||||
| 19 | Corrosion | 68 | Female | 31.9 | 8.9 | 0.5 | 127° Neck | 36 | (+) 5 | Yes |
| 20 | Corrosion | 82 | Male | 27.6 | 9.6 | 0.4 | 127° Neck | 36 | (−)5 | No |
| 21 | Corrosion | 59 | Female | 21.1 | 9.1 | 0.5 | 127° Neck | 36 | (+) 10 | No |
| 22 | Corrosion | 72 | Female | 27.5 | 9.6 | 1.4 | 127° Neck | 36 | (+) 5 | Yes |
| 23 | Corrosion | 61 | Female | 20.5 | 7.4 | 2.0 | 127° Neck | 36 | (+) 10 | No |
| 24 | Corrosion | 75 | Female | 21.8 | 7.1 | 2.6 | 127° Neck | 36 | (+) 0 | No |
| 25 | Corrosion | 80 | Female | 27.1 | 5.1 | 4.2 | 127° Neck | 36 | (+) 5 | Yes |
| 26 | Corrosion | 88 | Female | 21.9 | 6.8 | 2.1 | 127° Neck | 36 | (+) 0 | No |
| 27 | Corrosion | 60 | Female | 30.1 | 8.2 | 1.7 | 127° Neck | 36 | (+) 0 | No |
| 28 | Corrosion | 73 | Female | 24.0 | 8.3 | 1.8 | 127° Neck | 36 | (−)5 | No |
| 29 | Corrosion | 70 | Male | 28.0 | 7.7 | 1.3 | 127° Neck | 36 | (+) 5 | Yes |
| 30 | Corrosion | 74 | Male | 33.7 | 6.2 | 2.7 | 127° Neck | 36 | (+) 10 | No |
Patients presented with either GTF or head-neck taper corrosion at 8.0±1.4 years (range, 4.7 to 9.6 years, median: 8.3 years) from surgery (Table 1). In the GTF group, patients were initially asymptomatic until an acute, severe hip pain, an inability to bear weight, and radiographs demonstrating implant failure. A group of patients (n=5; 27.8%) had noticed an audible sound in their hip usually described as “clicking” within the month prior to presentation. Patients that presented with head-neck taper corrosion complained of a chronic hip pain (10/12). Overall, there was a statistical significant difference in demographics between both groups for BMI (GTF mean: 31.8±8.0 kg/m2, taper corrosion mean: 26.2±4.2 kg/m2, p=0.03). There was no statistical difference in age (GTF mean: 67.3±10.4 yrs, taper corrosion mean: 73.2±9.9 yrs, p=0.13). In both groups, no infections were identified based on definition of the musculoskeletal infection society criteria[15]. Out of concern for falsely elevated automated nucleated synovial cell counts, manual cell counts were performed when necessary[16].
Imaging
In the GTF group, radiographs demonstrated failure of the modular junction with a dissociation of the femoral head from the taper. A large radiolucent fluid collection from metal debris (Figure 1A) was identified in 13 of the 18 cases (73.3%). Careful evaluation of previous radiographs collected prior to presentation did not demonstrate any obvious signs of impending trunnion failure. In a patient with bilateral GTF (case 3 and 7), the patient was seen as part of post-operative follow up one month prior to presentation for failure on his opposite extremity. No obvious signs of impending failure could be seen on these radiographs. In a subset of 9/18 (50%) patients, small, not abnormal, amounts of a faint radiodensity around the hip capsule, similar to early heterotopic ossification, could be identified in the last set of normal radiographs prior to failure. MRI was collected in only one patient given the urgent need for revision. In this patient, a large fluid-filled cystic lesion typical for ALTR was present. In the head-neck taper corrosion group, MARS MRI demonstrated fluid collections of various size and cystic lesions.
Figure 1.
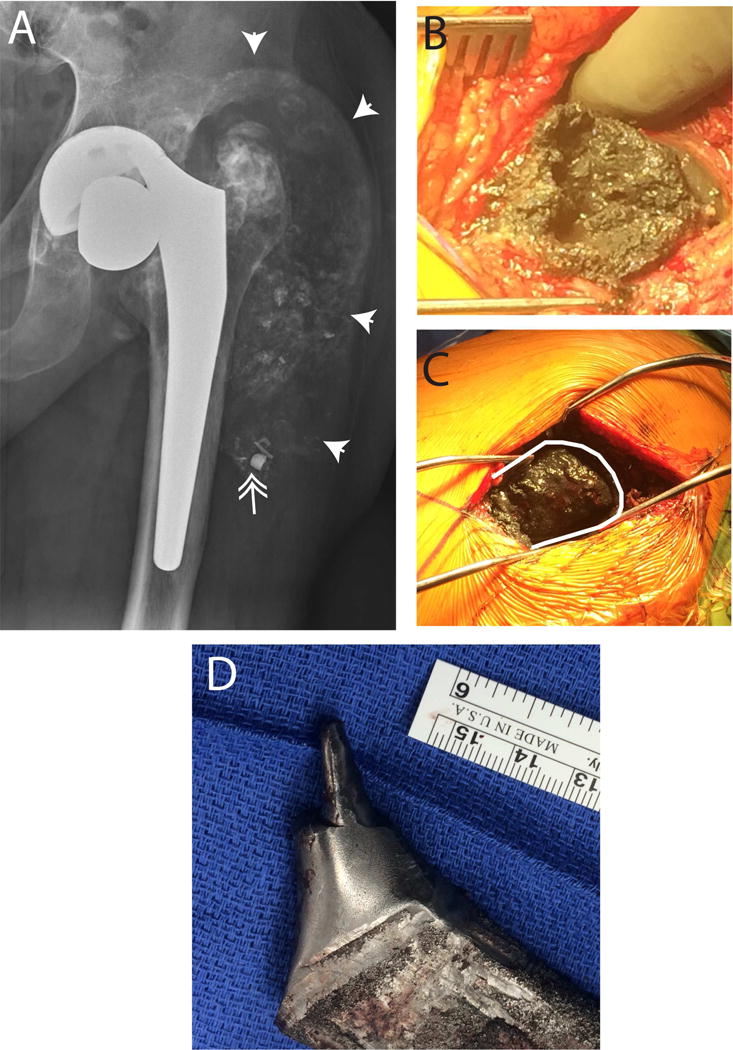
Gross trunnion failure radiographic and intraoperative findings. (A) A large radiotranslucent fluid collection surrounded the proximal femur (arrows). Pieces of metallic debris were observed at the base of the fluid collection (double arrow) that were intraoperatively identified as pieces of the polyethylene liner locking mechanism. Note the appearance of the greater trochanter appearing with increased radiodensity in place of normal bone. This increased radiodensity in the greater trochanter was fine metallic debris. (B) Opening of the fascia revealed friable black tissue with the absence of viable muscle tissue. (C) The greater trochanter (outlined with white line) was a thin cortical shell. Viable bone was replaced with a viscous black substance that had increased radiodensity as compared to bone as seen on radiographs. There were no abductors attached. (D) Direct examination of the trunnion after stem removal demonstrated severe erosion of the taper.
Metal Ion Levels
Serum cobalt (Co) and chromium (Cr) levels were elevated[17, 18] (>4.5 μg/L) in 80.0% (20/25) of patients tested preoperatively (Table 2). Mean cobalt levels were 8.9±8.2 μg/L for GTF and 7.8±5.7 μg/L for head-neck taper corrosion (p=0.68). Mean chromium levels were 4.4±3.3 μg/L for GTF and 2.3±3.2 μg/L for head-neck taper corrosion (p=0.11). Serum cobalt levels were elevated, typically more than chromium levels. The ratio of Co/Cr was 2.5 in the GTF group and 4.9 in the head-neck taper corrosion group, and these differences were statistically significant (p=0.01).
Table 2.
Preoperative Laboratory Findings
| Case | Type | Cobalt | Chromium | Co/Cr Ratio |
|---|---|---|---|---|
| 1 | GTF | 3.6 | 2.3 | 1.6 |
| 2 | GTF | 6.2 | 3.7 | 1.7 |
| 3 | GTF | |||
| 4 | GTF | |||
| 5 | GTF | 5.2 | 5.0 | 1.0 |
| 6 | GTF | 7.0 | 4.1 | 1.7 |
| 7 | GTF | 3.5 | ||
| 8 | GTF | |||
| 9 | GTF | 33.8 | 9.8 | 3.4 |
| 10 | GTF | |||
| 11 | GTF | 11.3 | 9.3 | 1.2 |
| 12 | GTF | 10.4 | 2.0 | 5.2 |
| 13 | GTF | 3.4 | 4.0 | 0.9 |
| 14 | GTF | 6.7 | 1.0 | 6.7 |
| 15 | GTF | 0.6 | 2.2 | 0.3 |
| 16 | GTF | 13.0 | 11.0 | 1.2 |
|
| ||||
| 17 | Impending | 7.3 | 1.6 | 4.6 |
| 18 | Impending | 10.8 | 1.4 | 7.7 |
|
| ||||
| 19 | Corrosion | 13.0 | 11.0 | 1.2 |
| 20 | Corrosion | 10.8 | 1.4 | 7.7 |
| 21 | Corrosion | 4.9 | 1.3 | 3.8 |
| 22 | Corrosion | 8.0 | 1.2 | 6.7 |
| 23 | Corrosion | 5.2 | 1.2 | 4.3 |
| 24 | Corrosion | 5.9 | 1.1 | 5.4 |
| 25 | Corrosion | 22.8 | 6.5 | 3.5 |
| 26 | Corrosion | 7.1 | 0.8 | 8.9 |
| 27 | Corrosion | 0.7 | 0.2 | 3.5 |
| 28 | Corrosion | 6.0 | 1.1 | 5.5 |
| 29 | Corrosion | 3.8 | 1.1 | 3.5 |
| 30 | Corrosion | 4.8 | 1.0 | 4.8 |
Postoperative serum cobalt and chromium levels were measured in 15 patients. Serum cobalt and chromium levels as compared to preoperative levels were decreased in both groups. In the GTF group, nine patients had a serum cobalt level of 0.9±0.5 μg/L and serum chromium level of 1.6±0.9 μg/L at a mean follow-up of 0.9±0.4 years. In the head-neck taper corrosion group, six patients had a serum cobalt level of 0.9±0.7 μg/L and serum chromium level of 0.7±0.6 μg/L at a mean follow-up of 0.7±0.3 years.
Intraoperative Findings
Intraoperative findings confirmed a diagnosis of ALTR. In cases involving GTF, incision in the deep fascia revealed a large collection of black synovial fluid and black, friable hypertophic pseudotumor to varying degrees in all cases (Figure 1B). There was a complete absence or damage to the abductors (Figure 1C) and extensive erosion of the trunnion (Figure 1D). In cases involving head-neck taper corrosion, incision in the deep fascia revealed a straw-colored or brown-grey fluid with hypertrophic synovial tissue. There was severe damage or absence of abductors. After removal of the head, there was a circumferential ring of black corrosion material around the femoral taper.
Tissue specimens were sent to pathology in sixteen cases (11 GTF and 5 taper corrosion). A fibrous tissue surrounded by a chronic inflammatory infiltrate was observed with no acute inflammation. Description of the cellular infiltrate varied between each sample, and included macrophages, granuloma, giant cells, histiocytes, and necrotic tissue. In cases of GTF, a foreign material consistent with the large amount of trunnion wear debris was also noted.
Post-Surgical Complications
In both groups, there was an increased incidence of post-operative instability after revision THA (30.0%; 9/30 cases). These patients required a constrained liner, and no further instability has occurred. Patients with instability had notable abductor damage at the time of surgery, and in 5 cases had complete or near loss of the abductors. Post-surgical follow up ranged from 0.1 to 4.7 years (2.6±1.1 years).
Impending GTF
There were two cases of impending trunnion failure that were revised before failure (case 17 and 18). Radiographs demonstrated a slight oblique angle between the head-neck taper of the femoral stem. In case 17, there was a slight radiodensity around the hip capsule (Figure 2A). Aspiration of the synovial fluid was black. MRI was unable to be obtained secondary to contraindications. Intraoperatively, after the femoral head was removed, there was a gross erosion of the proximal portion of the neck taper of approximately 20% (Figure 2B).
Figure 2.
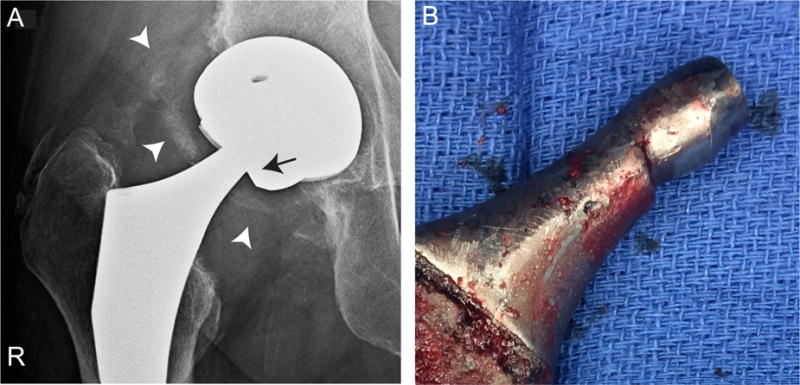
Impending gross trunnion failure radiographic and intraoperative findings. (A) Radiographs show radiodensities around the hip capsule (white arrow heads) and a slight oblique angle of the femoral head-neck taper (black arrow). (B) Direct examination of the trunnion demonstrated erosion of the proximal portion of the taper.
Discussion
A series of trunnion failures associated with the recalled LFIT CoCr femoral head implants are described, which at our institution was used with the Accolade TMZF femoral stem. Modes of failure included GTF or corrosion at the head-neck taper interface. Intraoperatively, we observed a spectrum of ALTR. Approximately one half of the failures we observed included implant sizes outside of the August 2016 LFIT CoCr femoral head recall. Head-neck taper corrosion was not listed as a potential mode of failure as part of the recall. These two types of failure have been observed across a range of other manufacturers as a rare event[6–10, 19–22].
In our series, 43% (13/30) of the failed trunnions included 36(−5), 36(+0), and 36(+10) femoral heads, and were not part of the voluntary recall. Failures in implant sizes outside of the recall showed a trend of being skewed towards the taper corrosion group, but that association was at the borderline of statistical significance (p = 0.06). We cannot presently conclude, based on the limited sample size, whether there is statistically a higher incidence of taper corrosion cases outside the recall than in the GTF group. A larger sample size would be needed to further address this issue. When we consider the entire population of revisions in our series, almost all femoral head sizes at and above 36mm have reported failures. In another recent series of 5 cases of failed Accolade TMZF and LFIT femoral head, all of the femoral head diameters and offsets reported were listed in the recall[9].
We have observed patterns that may help predict impending implant failure associated with the implant, imaging, and laboratory values. From an implant perspective, failure has an association with high offset 127° neck angle femoral stems and increased femoral neck offset. In two cases, impending GTF was diagnosed based on radiographs that demonstrated a slight oblique angle between the femoral head and neck taper. In other cases, a faint radiodensity around the hip capsule, similar to a small amount of early heterotopic ossification, has been observed. MRI findings appeared similar to those associated with ALTR, including fluid collections and the development of cystic lesions[23]. We observed elevated serum metal ion levels and a preferential elevated cobalt level as compared to chromium level in both the head-neck taper corrosion and GTF groups. Similar to ALTR associated with other pathologies, all of these methods, imaging, serum metal ion levels, and symptoms are important, but not independent diagnostic tools[24]. These observations have allowed us to diagnose impending GTF before the femoral head disassociates from the neck taper.
We have been able to differentiate between impending GTF and head-neck taper corrosion in this combination of femoral head and stem by aspiration of fluid under image guidance using a simple colorimetric assay. Black synovial fluid is associated with wear at the trunnion interface, and the need to replace the entire stem at the time of revision. Brown, light grey, or straw colored synovial fluid, with or without turbidity, has been associated with head-neck taper corrosion and no gross damage to the trunnion. In these cases, an exchange of the modular head and liner was required at the time of revision. In both types of failure, we recommend the use of a ceramic femoral head with a titanium sleeve. This colorimetric test may aid in preoperative planning by differentiating between failure from head-neck taper corrosion and impending GTF, and determining if the femoral stem may need to be revised from trunnion damage prior to failure.
Adverse local tissue reaction was defined in our study as heterogeneous cellular infiltrate with the presence of corrosion products in the periprosthetic tissue. This was observed in all cases sent to pathology. We are unable to assess if this occurred from the cobalt, chromium, or titanium, however all three metals likely had elevated levels in the tissue given the wear from the titanium trunnion and the elevated serum cobalt and chromium levels. Other groups have observed that ALTR can encompass a range of histological patterns depending on the involved implant [25]. We would anticipate a similar pattern here. Secondary to ALTR, we observed abductor damage with a range from minimal abductor loss to complete absence of abductors. Abductor damage appeared to be similar to other corrosion scenarios where ALTR has been observed [26, 27]. We have approached this issue with a standard strategy [28]. Hip stability is optimized intraoperatively using length, offset, stem version, and minimizing any sources of impingement. If repeated episodes of instability occur and no obvious etiology can be identified, we have been using a constrained liner for additional stability.
The etiology of GTF is unknown. One possibility, supported by visual observation at the time of revision, includes abrasive wear of a loose taper trunnion inside the female taper of the femoral head. Another possible mechanism includes failure representing the end stage of mechanically assisted crevice corrosion (MACC) at an initially well-fixed modular junction. Gradual material loss at the taper junction in MACC could lead to late loosening of the taper, and a progressively loose junction would allow continued abrasive wear. Retrieval analyses of the explanted components, beyond the scope of the current study, may provide insight into the mechanism of GTF in these cases.
There are limitations to this study. First, this is a retrospective study of an unexpected problem limiting our ability to have complete follow-up of the entire patient cohort in our practice that received LFIT femoral heads and Accolade TMZF stems. We are unable to report on demographic, implant, and laboratory values of patients that did not have any issues with implant failure. We observed these failures were associated with increased offset stems and femoral neck offsets. The ability to compare outcomes in a group of patients that did not have failure would strengthen the validity of this observation. Second, there was an observational bias associated with our study. After an initial series of GTF, we more actively screened for possible or impending implant failure using MARS MRI and serum metal ion levels. This may have increased the overall number of failures detected secondary to head-neck taper corrosion. Finally, a single surgeon performed all index surgeries. We were unable to assess the role of surgical technique in trunnion failure. The technique used to impact the femoral head onto the trunnion has been postulated to play a role in trunnion corrosion[9]. We cannot comment on this, however the identical technique was used on other femoral stems used before and after this implant in our practice. We have not observed similar levels of failure in these other stems.
We observed a series of modular junction failures of the LFIT femoral head and Accolade TMZF stem. Approximately one half of the failures were observed outside of the voluntary recall of Stryker LFIT femoral head size and offsets. Although there is limited evidence, these events seem to be associated with increased offset stems and femoral heads. Serum metal ion levels, radiographs, and MARS MRI should be obtained as part of the initial evaluation, and can be used to help predict impending trunnion failure. Black synovial fluid from a hip aspiration appears to be associated with impending GTF requiring a complete revision of the femoral stem as compared to a femoral head and liner exchange, allowing appropriate preoperative planning. Based on this experience, we have changed our clinical practice from using CoCr femoral heads to ceramic heads based on the lower risk of corrosion and metal release[29, 30], which should theoretically mitigate ALTR issues in the future.
Supplementary Material
Acknowledgments
The study was supported in part by funding from the National Institutes of Health (NIH) through grants KL2 TR000146, KL2 TR001856, and R01 AR47904. The authors would like to thanks Genymphas Higgs, Drexel University, for his contributions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Level of Evidence: Diagnostic Level III
References
- 1.Kolb A, Grubl A, Schneckener CD, Chiari C, Kaider A, Lass R, Windhager R. Cementless total hip arthroplasty with the rectangular titanium Zweymuller stem: a concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2012;94(18):1681. doi: 10.2106/JBJS.K.01574. [DOI] [PubMed] [Google Scholar]
- 2.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. A concise follow-up, at twenty years, of previous reports. J Bone Joint Surg Am. 2011;93(14):1335. doi: 10.2106/JBJS.J.00448. [DOI] [PubMed] [Google Scholar]
- 3.Makela KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90(10):2160. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 4.Kwon YM, Thomas P, Summer B, Pandit H, Taylor A, Beard D, Murray DW, Gill HS. Lymphocyte proliferation responses in patients with pseudotumors following metal-on-metal hip resurfacing arthroplasty. J Orthop Res. 2010;28(4):444. doi: 10.1002/jor.21015. [DOI] [PubMed] [Google Scholar]
- 5.Clayton RA, Beggs I, Salter DM, Grant MH, Patton JT, Porter DE. Inflammatory pseudotumor associated with femoral nerve palsy following metal-on-metal resurfacing of the hip. A case report. J Bone Joint Surg Am. 2008;90(9):1988. doi: 10.2106/JBJS.G.00879. [DOI] [PubMed] [Google Scholar]
- 6.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94(18):1655. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGrory BJ, MacKenzie J, Babikian G. A High Prevalence of Corrosion at the Head-Neck Taper with Contemporary Zimmer Non-Cemented Femoral Hip Components. J Arthroplasty. 2015;30(7):1265. doi: 10.1016/j.arth.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 8.Banerjee S, Cherian JJ, Bono JV, Kurtz SM, Geesink R, Meneghini RM, Delanois RE, Mont MA. Gross trunnion failure after primary total hip arthroplasty. J Arthroplasty. 2015;30(4):641. doi: 10.1016/j.arth.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 9.Matsen Ko L, Chen AF, Deirmengian GK, Hozack WJ, Sharkey PF. Catastrophic Femoral Head-Stem Trunnion Dissociation Secondary to Corrosion. J Bone Joint Surg Am. 2016;98(16):1400. doi: 10.2106/JBJS.15.00914. [DOI] [PubMed] [Google Scholar]
- 10.Spanyer J, Hines J, Beaumont CM, Yerasimides J. Catastrophic Femoral Neck Failure after THA with the Accolade((R)) I Stem in Three Patients. Clin Orthop Relat Res. 2016;474(5):1333. doi: 10.1007/s11999-015-4438-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engh CA, Jr, Ho H, Engh CA. Metal-on-metal hip arthroplasty: does early clinical outcome justify the chance of an adverse local tissue reaction? Clin Orthop Relat Res. 2010;468(2):406. doi: 10.1007/s11999-009-1063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs JJ, Cooper HJ, Urban RM, Wixson RL, Della Valle CJ. What do we know about taper corrosion in total hip arthroplasty? J Arthroplasty. 2014;29(4):668. doi: 10.1016/j.arth.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Kwon YM, Antoci V, Jr, Eisemon E, Tsai TY, Yan Y, Liow MH. Top-Out Removal of Well-Fixed Dual-Taper Femoral Stems: Surgical Technique and Radiographic Risk Factors. J Arthroplasty. 2016 doi: 10.1016/j.arth.2016.05.046. [DOI] [PubMed] [Google Scholar]
- 14.Pulliam IT, Trousdale RT. Fracture of a ceramic femoral head after a revision operation. A case report. J Bone Joint Surg Am. 1997;79(1):118. doi: 10.2106/00004623-199701000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992. doi: 10.1007/s11999-011-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yi PH, Cross MB, Moric M, Levine BR, Sporer SM, Paprosky WG, Jacobs JJ, Della Valle CJ. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res. 2015;473(2):498. doi: 10.1007/s11999-014-3902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griffin WL. Metal ion levels: how can they help us? J Arthroplasty. 2014;29(4):659. doi: 10.1016/j.arth.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Hart AJ, Sabah SA, Bandi AS, Maggiore P, Tarassoli P, Sampson B, AS J. Sensitivity and specificity of blood cobalt and chromium metal ions for predicting failure of metal-on-metal hip replacement. J Bone Joint Surg Br. 2011;93(10):1308. doi: 10.1302/0301-620X.93B10.26249. [DOI] [PubMed] [Google Scholar]
- 19.Pande K, Leong JF, Lo NN. Spontaneous Dissociation of Anatomic Medullary Locking A Plus (AML A Plus) Femoral Component at the Head-Neck Interface. Journal of orthopaedic case reports. 2015;5(3):48. doi: 10.13107/jocr.2250-0685.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kusaba A, Katsui M, Hakuta N, Tsuchida M, Maeda A, Kondo S. Catastrophic stem taper wear in ceramic on polyethylene bearing couple: a case report. Journal of long-term effects of medical implants. 2014;24(2–3):185. doi: 10.1615/jlongtermeffmedimplants.2014011133. [DOI] [PubMed] [Google Scholar]
- 21.Mann MA, Tanzer D, Tanzer M. Severe metal-induced osteolysis many years after unipolar hip endoprosthesis. Clin Orthop Relat Res. 2013;471(7):2078. doi: 10.1007/s11999-012-2780-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Talmo CT, Sharp KG, Malinowska M, Bono JV, Ward DM, LaReau J. Spontaneous modular femoral head dissociation complicating total hip arthroplasty. Orthopedics. 2014;37(6):e592. doi: 10.3928/01477447-20140528-62. [DOI] [PubMed] [Google Scholar]
- 23.Hauptfleisch J, Pandit H, Grammatopoulos G, Gill HS, Murray DW, Ostlere S. A MRI classification of periprosthetic soft tissue masses (pseudotumours) associated with metal-on-metal resurfacing hip arthroplasty. Skeletal radiology. 2012;41(2):149. doi: 10.1007/s00256-011-1329-6. [DOI] [PubMed] [Google Scholar]
- 24.Kwon YM, Lombardi AV, Jacobs JJ, Fehring TK, Lewis CG, Cabanela ME. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am. 2014;96(1):e4. doi: 10.2106/JBJS.M.00160. [DOI] [PubMed] [Google Scholar]
- 25.Ricciardi BF, Nocon AA, Jerabek SA, Wilner G, Kaplowitz E, Goldring SR, Purdue PE, Perino G. Histopathological characterization of corrosion product associated adverse local tissue reaction in hip implants: a study of 285 cases. BMC clinical pathology. 2016;16:3. doi: 10.1186/s12907-016-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nodzo SR, Esposito CI, Potter HG, Ranawat CS, Wright TM, Padgett DE. MRI, Retrieval Analysis, and Histologic Evaluation of Adverse Local Tissue Reaction in Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty. 2016 doi: 10.1016/j.arth.2016.11.046. [DOI] [PubMed] [Google Scholar]
- 27.Liow MH, Urish KL, Preffer FI, Nielson GP, Kwon YM. Metal Ion Levels Are Not Correlated With Histopathology of Adverse Local Tissue Reactions in Taper Corrosion of Total Hip Arthroplasty. J Arthroplasty. 2016;31(8):1797. doi: 10.1016/j.arth.2016.01.041. [DOI] [PubMed] [Google Scholar]
- 28.Wera GD, Ting NT, Moric M, Paprosky WG, Sporer SM, Della Valle CJ. Classification and management of the unstable total hip arthroplasty. J Arthroplasty. 2012;27(5):710. doi: 10.1016/j.arth.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Kocagoz SB, Underwood RJ, MacDonald DW, Gilbert JL, Kurtz SM. Ceramic Heads Decrease Metal Release Caused by Head-taper Fretting and Corrosion. Clin Orthop Relat Res. 2016;474(4):985. doi: 10.1007/s11999-015-4683-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurtz SM, Kocagoz SB, Hanzlik JA, Underwood RJ, Gilbert JL, MacDonald DW, Lee GC, Mont MA, Kraay MJ, Klein GR, Parvizi J, Rimnac CM. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471(10):3270. doi: 10.1007/s11999-013-3096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


