Abstract
The aim of this study is to examine the effects of acute administration of luseogliflozin, the sodium–glucose cotransporter 2 (SGLT2) inhibitor, on renal hemodynamics and tubular functions in anesthetized non-diabetic Sprague Dawley (SD) rats and 5/6 nephrectomized (Nx) SD rats. Renal blood flow (RBF), mean arterial pressure (MAP), and heart rate (HR) were continuously measured and urine was collected directly from the left ureter. Intraperitoneal injection of luseogliflozin (0.9 mg kg−1) did not change MAP, HR, RBF, or creatinine clearance (CrCl) in SD rats (n = 7). Luseogliflozin significantly increased urine volume, which was associated with significantly increased urinary glucose excretion rates (P < 0.001). Similarly, luseogliflozin significantly increased urinary sodium excretion (from 0.07 ± 0.01 µmol min−1 at baseline to 0.76 ± 0.08 µmol min−1 at 120 min; P < 0.001). Furthermore, luseogliflozin resulted in significantly increased urinary pH (P < 0.001) and decreased urinary osmolality and urea concentration (P < 0.001) in SD rats. Similarly, in Nx SD rats (n = 5–6), luseogliflozin significantly increased urine volume and urinary glucose excretion (P < 0.001) without altering MAP, HR, RBF, or CrCl. Luseogliflozin did not elicit any significant effects on the other urinary parameters in Nx SD rats. These data indicate that SGLT2 inhibitor elicits direct tubular effects in non-diabetic rats with normal renal functions.
Introduction
To manage type 2 diabetes mellitus, blockade of glucose reabsorption at the proximal tubule using sodium–glucose cotransporter 2 (SGLT2) inhibitors have been recently applied1, 2. SGLT2 is primarily expressed in the brush border membrane at S1 segments of the proximal convoluted tubule3. It has been suggested that approximately 90% of filtered glucose is reabsorbed by SGLT24. Therefore, inhibition of this transporter leads to glycosuria, and selective SGLT2 inhibitors are considered therapeutic tools for treating type 2 diabetes. A review article reported that SGLT2 inhibition reduces blood pressure5; however, the mechanism responsible for SGLT2 inhibitor-induced blood pressure reduction is unclear. We have recently reported that reductions in blood pressure using SGLT2 inhibitors are associated with natriuresis in metabolic syndrome6, 7. Similarly, a clinical study reported that treatment with canagliflozin, the SGLT2 inhibitor, significantly increased urinary sodium excretion in patients with type 2 diabetes8. These findings suggest that SGLT2 inhibitor-induced blood pressure reduction is accompanied by natriuresis in patients with metabolic syndrome and diabetes.
Genetic knockout of SGLT2 resulted in increased urine flow and glucosuria without affecting the glomerular filtration rate (GFR) in mice9, and chronic treatment with an SGLT2 inhibitor showed sustained increases in urinary glucose excretion in wild-type mice10. Additionally, in a micropuncture study, it was found that acute injection of an SGLT2 inhibitor increased urine flow, urinary glucose, and sodium excretion in a rat model of early diabetes11. However, the effects of acute administration of SGLT2 inhibitors have not been examined in non-diabetic subjects. It is of particular importance that the pharmacological effects of SGLT2 inhibitors in non-diabetic subjects are studied to minimize any indirect influence induced by changes in blood glucose levels. In this regard, a study with pooled urine reported that treatment with an SGLT2 inhibitor increased the 24-h urine volume, urinary glucose, and sodium excretion in non-diabetic mice12. Similarly, an SGLT2 inhibitor tended to increase 24-h urinary excretion of sodium, potassium, and chloride in dogs13. However, it is difficult to exclude the possibility that urinary sodium excretion was influenced by sodium intake in these urine-storing studies. Thus, it remains unclear whether SGLT2 inhibitor-induced urinary changes are actually mediated by its direct tubular action or by other indirect mechanisms.
In the current study, we investigated the direct effects of SGLT2 inhibition on renal hemodynamics and tubular functions in vivo by examining the acute effects of luseogliflozin, the selective SGLT2 inhibitor1, 3, in anesthetized non-diabetic rats with normal kidney function. Clinically, side effects of SGLT2 inhibitors, such as polyuria and polydipsia, have been reported during the early stages of treatment1, 2, which leads to the restriction of use of an SGLT2 inhibitor, particularly in patients with chronic kidney disease (CKD). Therefore, we also examined the effects of a SGLT2 inhibitor on renal hemodynamics and functions in 5/6 nephrectomized (Nx) rat, a model of CKD.
Results
A major limitation of these studies with intravenous infusion of luseogliflozin was that intravenously administered vehicle (2-hydroxylpropyl-β-cyclodextrin (HP-β-CD)) had considerable effects on urinary parameters. Specifically, vehicle significantly increased urine flow from 3.27 ± 0.57 to 8.47 ± 1.17 µl min−1 and urinary sodium excretion from 0.20 ± 0.02 to 0.44 ± 0.03 µmol min−1 after 60 minutes in Sprague Dawley (SD) rats (Figs 1 and 2). To minimize the effects of vehicle, preliminary experiments with intraperitoneal injection of luseogliflozin were performed. We found that intraperitoneal administration of vehicle did not change urine flow or urinary sodium excretion. Based on these findings, further experiments using intraperitoneal injection of luseogliflozin were also performed.
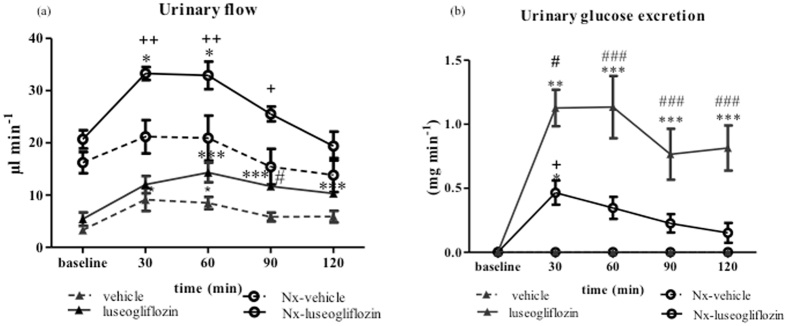
Figure 1.
Urinary flow and glucose excretion in Protocol 1. Intravenous injection of luseogliflozin significantly increased urine flow (a) and glucose excretion (b) in both SD and Nx SD rats. SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. *P < 0.05, **P < 0.01 and ***P < 0.001 vs. baseline, # P < 0.05 and ### P < 0.001 vs. vehicle, + P < 0.05 and ++ P < 0.01 vs. Nx-vehicle.
Figure 2.
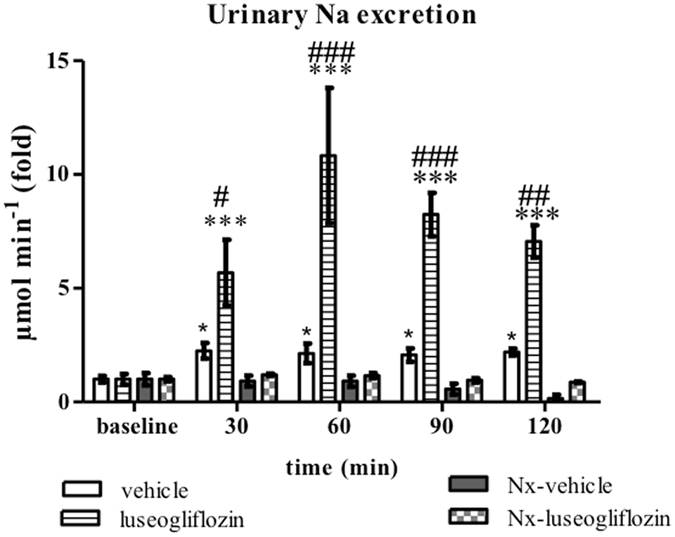
Urinary sodium excretion in Protocol 1. Intravenous injection of luseogliflozin significantly increased urinary sodium excretion in SD rats. SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. *P < 0.05 and ***P < 0.001 vs. baseline, # P < 0.05, ## P < 0.01 and ### P < 0.001 vs. vehicle.
Effects of intravenous injection of the SGLT2 inhibitor
Renal hemodynamics
Intravenous injection of luseogliflozin did not change mean arterial pressure (MAP), renal blood flow (RBF), heart rate (HR), or creatinine clearance (CrCl) in either SD or Nx SD rats (Table 1).
Table 1.
Renal hemodynamics data of Protocol 1.
| vehicle | luseogliflozin | Nx -vehicle | Nx-luseogliflozin | ||
|---|---|---|---|---|---|
| MAP (mmHg) | baseline | 103 ± 2 | 98 ± 3 | 104 ± 2 | 105 ± 1 |
| 15 | 103 ± 3 | 99 ± 3 | 106 ± 5 | 113 ± 2 | |
| 45 | 108 ± 2 | 98 ± 3 | 102 ± 7 | 111 ± 4 | |
| 75 | 104 ± 2 | 97 ± 3 | 103 ± 3 | 107 ± 2 | |
| 105 | 104 ± 3 | 97 ± 2 | 104 ± 2 | 100 ± 4 | |
| 120 | 105 ± 3 | 99 ± 6 | 96 ± 4 | 97 ± 3 | |
| HR (beats min−1) | baseline | 390 ± 8 | 386 ± 14 | 373 ± 18 | 339 ± 13 |
| 15 | 384 ± 9 | 385 ± 13 | 372 ± 25 | 340 ± 11 | |
| 45 | 417 ± 8 | 400 ± 8 | 391 ± 11 | 358 ± 10 | |
| 75 | 427 ± 7 | 388 ± 13 | 381 ± 10 | 368 ± 13 | |
| 105 | 413 ± 10 | 369 ± 14 | 397 ± 16 | 367 ± 11 | |
| 120 | 418 ± 16 | 380 ± 10 | 390 ± 9 | 381 ± 9 | |
| Mean RBF (fold) | baseline | 1.00 ± 0.02 | 1.00 ± 0.04 | 1.00 ± 0.12 | 1.00 ± 0.05 |
| 5 | 0.91 ± 0.01 | 1.05 ± 0.05 | 1.00 ± 0.11 | 0.81 ± 0.11 | |
| 10 | 0.92 ± 0.01 | 0.96 ± 0.03 | 1.00 ± 0.11 | 1.00 ± 0.03 | |
| 15 | 1.03 ± 0.04 | 1.05 ± 0.05 | 0.97 ± 0.13 | 1.01 ± 0.04 | |
| 30 | 1.12 ± 0.13 | 0.98 ± 0.06 | 0.94 ± 0.08 | 1.02 ± 0.06 | |
| 60 | 1.08 ± 0.04 | 1.00 ± 0.03 | 0.87 ± 0.06 | 0.99 ± 0.07 | |
| 90 | 1.11 ± 0.02 | 0.99 ± 0.04 | 0.85 ± 0.03 | 0.89 ± 0.11 | |
| 120 | 1.08 ± 0.05 | 1.04 ± 0.04 | 0.81 ± 0.03 | 0.83 ± 0.14 | |
| CrCl (µl min−1 g−1 body weight) | baseline | 3.22 ± 0.56 | 3.32 ± 0.71 | 5.24 ± 0.40 | 5.41 ± 0.42 |
| 30 | 3.99 ± 0.45 | 4.10 ± 0.54 | 5.54 ± 0.42 | 5.97 ± 0.26 | |
| 60 | 3.76 ± 0.25 | 4.24 ± 0.63 | 5.48 ± 0.30 | 5.64 ± 0.29 | |
| 90 | 3.66 ± 0.21 | 4.14 ± 0.70 | 5.15 ± 0.40 | 5.22 ± 0.28 | |
| 120 | 3.75 ± 0.32 | 4.21 ± 0.76 | 4.94 ± 0.60 | 4.91 ± 0.33 |
MAP, mean blood pressure; HR, heart rate; RBF, renal blood flow; CrCl, creatinine clearance; SD, Sprague-Dawly; Nx, 5/6 nephrectomized SD rats; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 nephrectomized SD rats treated with vehicle; Nx-luseogliflozin, 5/6 nephrectomized SD rats treated with luseogliflozin. Values are mean ± SEM.
Urine flow and urinary glucose excretion
In SD rats, luseogliflozin significantly increased urine flow from 5.40 ± 1.27 µl min−1 at baseline to 10.33 ± 0.73 µl min−1 at 120 min (P < 0.001; Fig. 1a), which was associated with a significant increase in the urinary glucose excretion rate from 0.003 ± 0.001 mg min−1 at baseline to 0.81 ± 0.18 mg min−1 at 120 min (P < 0.001; Fig. 1b). These changes induced by luseogliflozin were significantly greater than those induced by vehicle (Fig. 1a and b). On the other hand, luseogliflozin-induced changes in glucose excretion were significantly less in Nx SD rats compared with SD rats (Fig. 1b).
Urinary excretion of sodium
In SD rats, luseogliflozin increased urinary sodium excretion from 0.34 ± 0.08 µmol min−1 at baseline to 2.41 ± 0.24 µmol min−1 at 120 min, by approximately seven-fold (P < 0.001). These changes induced by luseogliflozin were significantly greater than those induced by vehicle (Fig. 2). On the other hand, intravenous infusion of luseogliflozin did not have an acute effect on urinary sodium excretion in Nx SD rats (from 0.42 ± 0.04 µmol min−1 at baseline to 0.37 ± 0.01 µmol min−1 at 120 min) (Fig. 2).
Effects of intraperitoneal injection of the SGLT2 inhibitor
Renal hemodynamics and blood glucose
Intraperitoneal injection of vehicle or luseogliflozin did not change MAP, RBF, HR, or CrCl in either SD or Nx SD rats (Table 2). Intraperitoneal injection of luseogliflozin did not significantly change plasma glucose level (from 142 ± 3 mg dl−1 at baseline to 147 ± 3 mg dl−1 at 120 min) in SD rats. Similarly, luseogliflozin did not significantly change plasma glucose level (from 131 ± 5 mg dl−1 at baseline to 133 ± 5 mg dl−1 at 120 min) in Nx SD rats.
Table 2.
Renal hemodynamics data of Protocol 2.
| vehicle | luseogliflozin | Nx -vehicle | Nx-luseogliflozin | ||
|---|---|---|---|---|---|
| MAP (mmHg) | baseline | 102 ± 2 | 101 ± 2 | 119 ± 3 | 123 ± 4 |
| 15 | 106 ± 2 | 103 ± 2 | 123 ± 2 | 128 ± 4 | |
| 45 | 106 ± 2 | 104 ± 2 | 125 ± 3 | 128 ± 4 | |
| 75 | 105 ± 2 | 102 ± 2 | 127 ± 2 | 128 ± 3 | |
| 105 | 106 ± 2 | 103 ± 2 | 122 ± 2 | 131 ± 4 | |
| 120 | 109 ± 1 | 102 ± 1 | 119 ± 6 | 127 ± 5 | |
| HR (beat min−1) | baseline | 385 ± 15 | 370 ± 15 | 386 ± 3 | 418 ± 7 |
| 15 | 394 ± 15 | 376 ± 14 | 410 ± 14 | 398 ± 8 | |
| 45 | 397 ± 17 | 379 ± 12 | 380 ± 11 | 389 ± 7 | |
| 75 | 387 ± 16 | 378 ± 11 | 410 ± 17 | 373 ± 7 | |
| 105 | 398 ± 15 | 376 ± 10 | 372 ± 9 | 384 ± 8 | |
| 120 | 403 ± 2 | 378 ± 6 | 385 ± 9 | 388 ± 5 | |
| Mean RBF (fold) | baseline | 1.00 ± 0.11 | 1.00 ± 0.09 | 1.00 ± 0.13 | 1.00 ± 0.18 |
| 5 | 1.08 ± 0.10 | 1.06 ± 0.12 | 1.00 ± 0.13 | 1.04 ± 0.17 | |
| 10 | 1.06 ± 0.10 | 1.02 ± 0.10 | 1.01 ± 0.12 | 1.05 ± 0.18 | |
| 15 | 1.09 ± 0.11 | 1.02 ± 0.10 | 0.99 ± 0.12 | 1.03 ± 0.19 | |
| 30 | 1.09 ± 0.10 | 1.07 ± 0.11 | 0.97 ± 0.11 | 1.04 ± 0.18 | |
| 60 | 1.06 ± 0.11 | 1.06 ± 0.10 | 1.05 ± 0.11 | 1.07 ± 0.16 | |
| 90 | 1.10 ± 0.13 | 1.09 ± 0.10 | 1.07 ± 0.12 | 1.01 ± 0.14 | |
| 120 | 1.05 ± 0.12 | 1.19 ± 0.08 | 1.04 ± 0.13 | 1.07 ± 0.17 | |
| CrCl (µl min−1 g−1 body weight) | baseline | 2.50 ± 0.16 | 2.49 ± 0.14 | 4.74 ± 0.16 | 4.73 ± 0.69 |
| 30 | 2.77 ± 0.16 | 2.55 ± 0.15 | 5.08 ± 0.57 | 4.62 ± 0.67 | |
| 60 | 2.54 ± 0.19 | 2.98 ± 0.15 | 4.38 ± 0.17 | 4.68 ± 0.54 | |
| 90 | 2.60 ± 0.18 | 2.79 ± 0.26 | 4.61 ± 0.32 | 4.72 ± 0.43 | |
| 120 | 2.53 ± 0.27 | 2.76 ± 0.18 | 4.15 ± 0.21 | 4.62 ± 0.40 |
MAP, mean blood pressure; HR, heart rate; RBF, renal blood flow; CrCl, creatinine clearance; SD, Sprague-Dawly; Nx, 5/6 nephrectomized SD rats; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 nephrectomized SD rats treated with vehicle; Nx-luseogliflozin, 5/6 nephrectomized SD rats treated with luseogliflozin. Values are mean ± SEM.
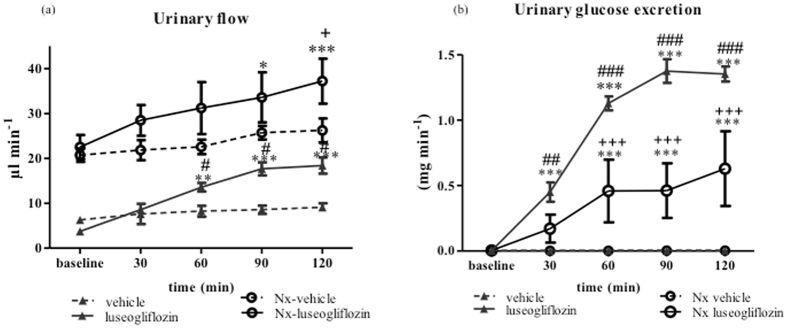
Urine flow and urinary excretion of glucose
In SD rats, intraperitoneal injection of vehicle did not change any urinary parameters. However, intraperitoneal injection of luseogliflozin significantly increased urine flow from 3.71 ± 0.21 µl min−1 at baseline to 18.38 ± 1.8 µl min−1 at 120 min (P < 0.001; Fig. 3a), and was accompanied by a concomitant increase in urinary glucose excretion from 0.003 ± 0.001 mg min−1 at baseline to 1.35 ± 0.05 mg min−1 at 120 min (P < 0.001; Fig. 3b). Luseogliflozin-induced changes in urine flow and glucose excretion were significantly less in Nx SD rats compared with SD rats (Fig. 3a and b).
Figure 3.
Urinary flow and glucose excretion in Protocol 2. Intraperitoneal injection of luseogliflozin significantly increased urinary flow (a) and glucose (b) excretion in both SD and Nx SD rats. SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. *P < 0.05, ** P < 0.01 and ***P < 0.001 vs. baseline, # P < 0.05, ## P < 0.01 and ### P < 0.001 vs. vehicle, + P < 0.05 and +++ P < 0.001 vs. Nx-vehicle.
Urinary excretions of sodium
In SD rats, intraperitoneal administration of luseogliflozin induced an increase in urinary sodium excretion from 0.07 ± 0.01 µmol min−1 at baseline to 0.76 ± 0.08 µmol min−1 at 120 min, by approximately 10-fold (P < 0.001; Fig. 4). On the other hand, intraperitoneal administration of luseogliflozin did not have a significant effect on urinary sodium excretion in Nx SD rats (from 0.26 ± 0.15 µmol min−1 at baseline to 0.66 ± 0.17 µmol min−1 at 120 min; Fig. 4). Urinary potassium excretion was not significantly affected by acute intraperitoneal injection of luseogliflozin in either SD rats or Nx SD (data not shown).
Figure 4.
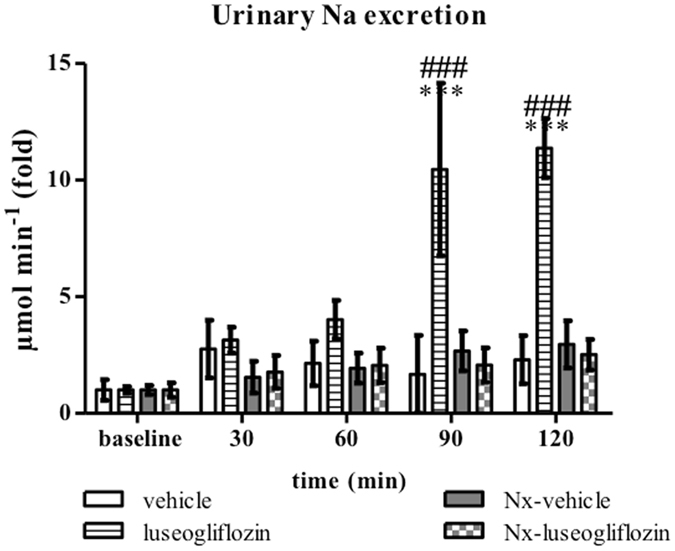
Urinary sodium excretion in Protocol 2. Intraperitoneal injection of luseogliflozin significantly increased urinary sodium excretion in SD rats. SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. ***P < 0.001 vs. baseline, ### P < 0.001 vs. vehicle.
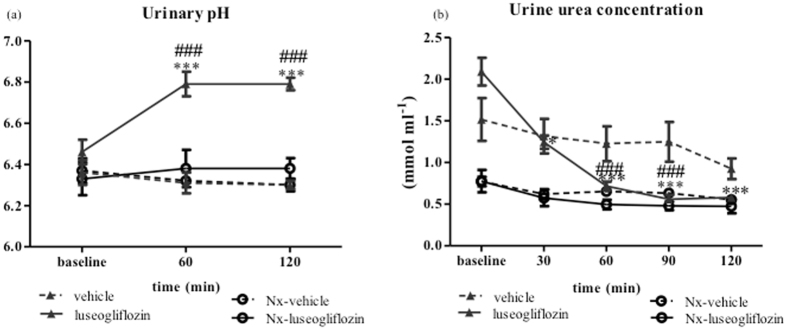
Urinary pH and urea
In SD rats, luseogliflozin induced a significant increase in urinary pH from 6.53 ± 0.06 at baseline to 6.79 ± 0.03 at 120 min (P < 0.001; Fig. 5a), which was associated with significant reduction in urinary urea concentration from 2.09 ± 0.16 mmol ml−1 at baseline to 0.58 ± 0.04 mmol ml−1 at 120 min (P < 0.001; Fig. 5b).
Figure 5.
Urinary pH and urea concentration in Protocol 2. Effect of intraperitoneal injection of luseogliflozin on urine pH (a) and urea concentration (b). SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. *P < 0.05 and ***P < 0.001 vs. baseline, ### P < 0.001 vs. vehicle.
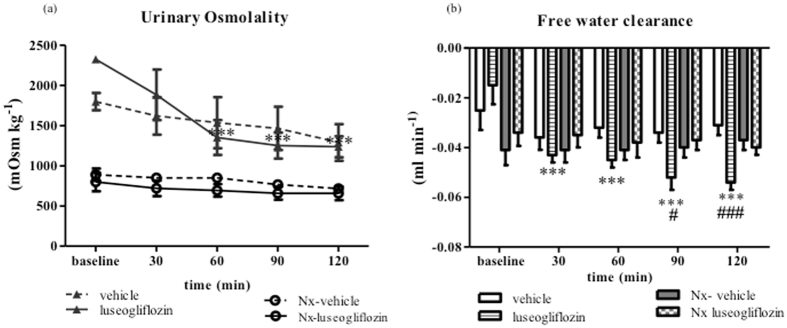
Urinary osmolality and free water clearance
In SD rats, luseogliflozin generate a significant reductions in urinary osmolality from 2325 ± 44 mOsm kg−1 at baseline to 1236 ± 121 mOsm kg−1 at 120 min (P < 0.001; Fig. 6a). Accordingly, augmentation of calculated negative values of free water clearance were concomitant with these urinary changes induced by luseogliflozin in these rats (P < 0.001; Fig. 6b). Luseogliflozin did not have any significant effects on urinary pH, urea concentration, or osmolality in Nx SD rats.
Figure 6.
Urine osmolality and free water clearance in Protocol 2. Effect of intraperitoneal injection of luseogliflozin on urine osmolality (a) and free water clearance (b). SD, Sprague Dawley; Nx, 5/6 nephrectomized; vehicle, SD rats treated with vehicle; luseogliflozin, SD rats treated with luseogliflozin; Nx-vehicle, 5/6 Nx SD rats treated with vehicle; Nx-luseogliflozin, 5/6 Nx SD rats treated with luseogliflozin. Values are mean ± SEM. ***P < 0.001 vs. baseline, # P < 0.05 and ### P < 0.001 vs. vehicle.
Effects of intraperitoneal injection of the SGLT2 inhibitor in inactin-anesthetized SD rats
We examined the effects of intraperitoneal administration of luseogliflozin in SD rats under inactin anesthesia (100 mg kg−1, i.p.; Protocol 3). Luseogliflozin significantly increased urinary glucose from 0.002 ± 0.0004 mg min−1 at baseline to 0.73 ± 0.07 mg min−1 at 120 min (P < 0.001). However, urinary sodium excretion was not significantly changed (from 0.09 ± 0.02 µmol min−1 at baseline to 0.11 ± 0.04 µmol min−1 at 120 min). Other renal parameter results in Protocol 3 are shown in Supplementary Figures 1–3.
Discussion
Chronic treatment of a SGLT2 inhibitor elicits several systemic effects on blood glucose, body weight, blood pressure, etc. To avoid any systemic changes, the present study utilized acute renal clearance method to examine the effects of luseogliflozin on renal hemodynamics and tubular functions. We found that acute administration of an SGLT2 inhibitor induced natriuresis without changing renal hemodynamics in non-diabetic SD rats. In Protocol 1, rats were anesthetized with sodium pentobarbital and maintained with isoflurane, and luseogliflozin was injected intravenously. Luseogliflozin significantly increased urine flow and urinary glucose excretion in SD rats without affecting MAP, RBF, or CrCl. To avoid any possible effects from the vehicle, luseogliflozin was also injected intraperitoneally (Protocol 2). We confirmed that intraperitoneal injection of vehicle did not change any parameters. However, intraperitoneal injection of luseogliflozin resulted in substantial glycosuria and natriuresis without changing renal hemodynamics in SD rats. The findings that these acute tubular effects of the SGLT2 inhibitor were observed in non-diabetic rats strongly support the hypothesis that the SGLT2 inhibitor elicits direct tubular effects independently of blood-glucose changes.
Our data showed that acute administration of luseogliflozin did not have any effects on MAP, mean RBF, or CrCl in non-diabetic SD rats. Previous studies have reported that chronic SGLT2 inhibitor treatment reduced GFR in type 1 diabetic patients with glomerular hyperfiltration14 and in type 1 diabetic Akita mice10. Similarly, chronic SGLT2 blockade significantly decreased GFR in type 2 diabetic rats1, 15 and patients16, 17. These studies have indicated that SGLT2 inhibitor-induced reduction in GFR is associated with an increase in the activity of tubuloglomerular feedback (TGF) mechanism. However, SGLT2 inhibitor did not have a significant effect on GFR in the early diabetic condition18. In agreement with the results in non-diabetic mice9 and rats19, our data also showed that acute infusion of luseogliflozin did not have any immediate significant effects on renal hemodynamics in non-diabetic SD rats. Thus, it seems that SGLT2 inhibitor-induced renal hemodynamic changes are significant in diabetes and not obvious in non-diabetes. Less amount of glucose reabsorption with SGLT2 inhibition may be related to less effect of SGLT inhibition on the activation of TGF mechanism11.
Acute administration of luseogliflozin significantly increased urine flow and urinary sodium excretion without affecting renal hemodynamics in non-diabetic SD rats. These acute responses are consistent with a previous study in which it was reported that luseogliflozin increased urinary sodium excretion 3 days after its administration in metabolic syndrome rats6. A clinical study has also shown that canagliflozin, a SGLT2 inhibitor, significantly increased urine volume and urinary sodium excretion in patients with type 2 diabetes8. As previously noted, a micropuncture study reported that an SGLT2 inhibitor increased urinary sodium excretion in diabetic rats11. Collectively, these data suggest that SGLT2 inhibitor elicits direct tubular effects in both diabetic and non-diabetic subjects.
In the current study, we expected urinary osmolality to increase following treatment with the SGLT2 inhibitor owing to a significant urinary glucose excretion. However, acute administration of the SGLT2 inhibitor consistently reduced urinary osmolality in SD rats (P < 0.001). We also observed that the urea concentration significantly decreased with the SGLT2 inhibitor (P < 0.001) in SD rats. As suggested previously20, high urinary glucose retains water in the tubular lumen, which dilutes urinary urea. Further studies are needed to examine the effects of SGLT2 inhibitors on the activities of water and urea transporters.
In this study, we also examined the effects of luseogliflozin in Nx SD rats, a model of CKD. In agreement with previous findings21, MAP elevation was observed in anesthetized Nx SD rats. Studies have indicated that in the remnant kidney model, chronic reduction in renal mass leads to an increase in blood pressure22, 23. In these animals, glomerular hyperfiltration of the remaining nephrons was observed, probably to compensate for nephron loss24 and following structural damage, and the kidney may have allowed an increase in the GFR for adaptation25. However, acute administration of the SGLT2 inhibitor did not alter RBF or CrCl in Nx SD rats. These data are inconsistent with a previous clinical study in which SGLT2 inhibitor significantly decreased the GFR in type 1 diabetic patients with glomerular hyperfiltration14. Therefore, it is possible that SGLT2 inhibitor-induced changes in renal hemodynamics are not obvious in non-diabetics with glomerular hyperfiltration. Alternatively, the possibility cannot be excluded that responses in the GFR to SGLT2 inhibitors are species specific.
When compared with SD rats, rats after 2 weeks of 5/6 nephrectomy displayed a marked increase in urine volume at baseline. Previous studies have indicated that increases in urine volume were associated with downregulation of the water channels in the collecting duct and proximal tubule26. Intraperitoneal administration of luseogliflozin induced a significant increase in urine output in Nx SD rats (P < 0.001). In agreement with previous studies24, after administering luseogliflozin, Nx SD rats exhibited lower glucose excretion compared with the SD rats, probably due to renal functional impairments27. In agreement with previous studies28–30, Nx SD rats showed greater urinary sodium and potassium excretion compared with SD rats. However, acute blockade of SGLT2 by luseogliflozin did not alter urinary sodium excretion in Nx SD rats. We have no good explanation as to why the SGLT2 inhibitor does not increase urinary sodium excretion in 5/6 Nx SD rats. One possibility is that reduced renal mass diminishes the functional activities of the sodium transporters, as shown by previous studies28, 31, 32. Consistent with a previous study33, we observed a significant reduction in the ability of urine to be concentrated and the urinary urea concentration in Nx SD rats. Luseogliflozin treatment similarly did not result in further reductions in urine osmolality or urea concentration in Nx SD rats. Interestingly, we found a significant increase in urinary pH in SD rats after luseogliflozin administration (P < 0.001), which was not observed in Nx SD rats. These results are consistent with a previous study in which systemic administration of phlorizin (a non-selective SGLT inhibitor) resulted in bicarbonaturia34. However, precise mechanism responsible for tubular effect of SGLT2 inhibitor is not clear, due to the limitations of in vivo clearance studies. Further studies are needed to explore the molecular mechanisms for tubular effects of SGLT2 inhibitor.
The major challenge in this study was the solubility of luseogliflozin. In this study, we used dimethyl sulfoxide (DMSO) and HP-β-CD as vehicle. Luseogliflozin could be dissolved in only 100% DMSO, but acute administration of high concentration DMSO caused hematuria. Intravenous administration of HP-β-CD caused neither hematuria nor renal hemodynamic changes; however, urinary parameters were significantly affected by administration of HP-β-CD. On the other hand, we confirmed that intraperitoneal administration of HP-β-CD showed minimal effect on systemic and renal parameter. Preliminary experiments showed that 0.9 mg kg−1 is the maximum dose of luseogliflozin and the minimum concentration of HP-β-CD is 4.5%. We have also documented that intraperitoneal administration of luseogliflozin at 0.9 mg kg−1 caused significant glucosuria, whereas 4.5% HP-β-CD did not change any renal parameters. Another crucial point is the application of an adequate anesthetic. In Protocol 3, we administered luseogliflozin in SD rats under inactin anesthesia. However, the predicted effect on urinary sodium excretion by luseogliflozin was absent, possibly because of the effects of inactin. Previous studies have clearly shown that inactin has a strong ability to inactivate urinary sodium excretion35. For these reasons, we used sodium pentobarbital and isoflurane as anesthetics in the current study.
In conclusion, acute administration of the SGLT2 inhibitor induced significant increases in urinary glucose and sodium excretion without altering renal hemodynamics in non-diabetic SD rats. These renal effects of the SGLT2 inhibitor were markedly attenuated in 5/6 Nx SD rats. These findings support the hypothesis that SGLT2 inhibitors elicit direct tubular effects without changes in plasma glucose levels.
Methods
Animals
All experimental procedures were performed according to the guidelines for the care and use of animals established by Kagawa University (Kagawa, Japan). Male SD rats (Japan SLC, Inc., Shizuoka, Japan) were housed in specific pathogen-free animal facilities at a controlled temperature (24 ± 2 °C) and humidity (55 ± 5%) on a 12-h light–dark cycle. Animals had free access to standard chow and water. All surgical and experimental procedures were approved by the Animal Care and Use Committee, Kagawa University.
By following the excision remnant kidney model22, an experimental Nx rat model was induced by ablation of two thirds of the left kidney at 7 weeks of age and, after a further week, a total right nephrectomy was performed. After a 2-week acclimation period, rats were assigned to one of two groups: Nx-luseogliflozin and Nx-vehicle.
Experimental procedures
SD and Nx SD rats were anesthetized with sodium pentobarbital (50 mg kg−1, i.p.) and isoflurane (0.5–1.5% in air) or inactin (100 mg kg−1, i.p.) at 9–11 weeks of age. Then, animals were placed on a heated pad to maintain body temperature at 37 °C. A polyethylene catheter (PE-60; Becton Dickinson and Company, Sparks, MD, USA) was inserted into the abdominal aorta via the right femoral artery for blood pressure measurement and collection of arterial blood. We collected urinary samples for every 30 minutes. The left kidney was exposed through a retroperitoneal flank incision. The renal artery was carefully isolated from the tissue connecting the renal hilum cephalic. A Doppler flow probe (HDP 10.20 R; Crystal Biotech, Northborough, MA, USA) was placed around the renal artery and RBF was continuously monitored. A polyethylene catheter (tapered PE-50; Becton Dickinson and Company) was inserted into the left ureter for urine collection. After surgery, each rat was kept isolated for 60 min to allow for stabilization of MAP, RBF, and urine flow. All rats were given saline as a maintenance fluid at a dose of 0.7 ml h−1. Blood was collected in EDTA- containing tubes. At the end of experiments, animals were euthanized by overdose of pentobarbital (250 mg kg−1).
Experimental protocols
Full details of experimental protocols are given in Supplementary Figures 4 and 5.
Protocol 1
SD and Nx SD rats were anesthetized with pentobarbital and isoflurane, and randomly assigned to one of four groups (n = 5–7 for each): Group 1, SD rats administered luseogliflozin; Group 2, SD rats administered vehicle (HP-β-CD at 4.5%); Group 3, Nx SD rats administered luseogliflozin; and Group 4, Nx SD rats administered vehicle. Luseogliflozin (0.3 mg kg−1) or vehicle at 0.1 ml was administered intravenously. Preliminary experiments showed that intravenous injection of luseogliflozin (0.3 mg kg−1) significantly increased urinary glucose excretion.
Protocol 2
SD and Nx SD rats were anesthetized with pentobarbital and isoflurane, and randomly assigned to one of four groups (n = 5–7 for each): Group 1, SD rats administered luseogliflozin; Group 2, SD rats administered vehicle; Group 3, Nx SD rats administered luseogliflozin; and Group 4, Nx SD rats administered vehicle. Luseogliflozin (0.9 mg kg−1) or vehicle at 0.1 ml was administered intraperitoneally. Preliminary studies showed that the minimum dose of HP-β-CD was 4.5% in 0.1 ml to dissolve 0.9 mg kg−1 luseogliflozin.
Protocol 3
SD rats were anesthetized with inactin and assigned to one of two groups (n = 7 for each): Group 1, SD rats administered luseogliflozin; and Group 2, SD rats administered vehicle. Luseogliflozin (0.9 mg kg−1) or vehicle was administered at 0.1 ml intraperitoneally.
Electrolyte and other analyses
Plasma and urine electrolytes (Na+ and K+) were determined by flame photometry (EFOX 5053; Eppendorf, Burladingen, Germany). Plasma and urinary glucose levels were measured using an automated analyzer (7020 Automatic Analyzer; Hitachi High-Technologies, Tokyo, Japan). Urinary and plasma levels of creatinine (LabAssayTM creatinine, Wako Pure Chemical Industries, Osaka, Japan), urea (urea assay kit; Biovision, Milpitas, CA, USA), and blood urea nitrogen (Urea N B, Urease-Indophenol method, Wako) were determined using commercially available assay kits. Urine and plasma osmolality were measured by vapor pressure osmometry (Wescor, Logan, UT, USA). Urinary pH was determined using PEHANON pH-test strips (Macherey-Nagel, Düren, Germany).
Statistical analysis
Data are mean ± standard error of the mean (SEM). The statistical significance of difference was determined using two-way analysis of variance followed by Bonferroni post-tests using GraphPad Prism software ver. 5.0 (GraphPad, La Jolla, CA, USA). A P-value < 0.05 was considered statistically significant.
Materials
Luseogliflozin, a selective SGLT2-inhibitor, was provided by Taisho Pharmaceutical Co. (Tokyo, Japan)1, 3. HP-β-CD was purchased from Wako (Osaka, Japan).
Electronic supplementary material
Acknowledgements
This study was partially supported by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (KAKENHI) (26460343 to Akira Nishiyama).
Author Contributions
Tuba M. Ansary, sample collection, analysis, interpretation, and manuscript writing and manuscript revision; Yoshihide Fujisawa, surgical preparation and sample collection; Kento Kitada, data analysis; Asadur Rahman, data interpretation and supervision; Daisuke Nakano, data interpretation; Hirofumi Hitomi, data interpretation; Hideki Kobara, data nalysis; Tsutomu Masaki, data analysis, Jens M. Titze, data analysis; Akira Nishiyama, conception, design, interpretation of the work, and manuscript revision.
Competing Interests
Luseogliflozin was provided by Taisho Pharmaceutical Co., Ltd. (to A.N.). This is a collaborative study, in part, with Taisho Pharmaceutical Co., Ltd. (to A.N.).
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-09352-5
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kojima N, Williams JM, Takahashi T, Miyata N, Roman RJ. Effects of a new SGLT2 inhibitor, luseogliflozin, on diabetic nephropathy in T2DN rats. J Pharmacol Exp Ther. 2013;345:464–472. doi: 10.1124/jpet.113.203869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagata T, et al. Tofogliflozin, a novel sodium-glucose co-transporter 2 inhibitor, improves renal and pancreatic function in db/db mice. Br J Pharmacol. 2013;170:519–531. doi: 10.1111/bph.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto K, et al. TS-071 is a novel, potent and selective renal sodium-glucose cotransporter 2 (SGLT2) inhibitor with anti-hyperglycaemic activity. Br J Pharmacol. 2011;164:181–191. doi: 10.1111/j.1476-5381.2011.01340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vallon V, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. J Am Soc Nephrol. 2011;22:104–112. doi: 10.1681/ASN.2010030246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliva RV, Bakris GL. Blood pressure effects of sodium-glucose co-transport 2 (SGLT2) inhibitors. J Am Soc Hypertens. 2014;8:330–339. doi: 10.1016/j.jash.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Rahman A, et al. Effects of diuretics on sodium-dependent glucose cotransporter 2 inhibitor-induced changes in blood pressure in obese rats suffering from the metabolic syndrome. J Hypertens. 2016;34:893–906. doi: 10.1097/HJH.0000000000000871. [DOI] [PubMed] [Google Scholar]
- 7.Takeshige Y, et al. A sodium-glucose co-transporter 2 inhibitor empagliflozin prevents abnormality of circadian rhythm of blood pressure in salt-treated obese rats. Hypertens Res. 2016;39:415–422. doi: 10.1038/hr.2016.2. [DOI] [PubMed] [Google Scholar]
- 8.Iijima H, Kifuji T, Maruyama N, Inagaki N. Pharmacokinetics, Pharmacodynamics, and Safety of Canagliflozin in Japanese Patients with Type 2 Diabetes Mellitus. Adv Ther. 2015;32:768–782. doi: 10.1007/s12325-015-0234-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vallon V, et al. Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in diabetes mellitus. Am J Physiol Renal Physiol. 2013;304:F156–167. doi: 10.1152/ajprenal.00409.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vallon V, et al. SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice. Am J Physiol Renal Physiol. 2014;306:F194–204. doi: 10.1152/ajprenal.00520.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomson SC, et al. Acute and chronic effects of SGLT2 blockade on glomerular and tubular function in the early diabetic rat. Am J Physiol Regul Integr Comp Physiol. 2012;302:R75–83. doi: 10.1152/ajpregu.00357.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin B, et al. Glycemic control with empagliflozin, a novel selective SGLT2 inhibitor, ameliorates cardiovascular injury and cognitive dysfunction in obese and type 2 diabetic mice. Cardiovasc Diabetol. 2014;13 doi: 10.1186/s12933-014-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang W, et al. EGT1442, a potent and selective SGLT2 inhibitor, attenuates blood glucose and HbA(1c) levels in db/db mice and prolongs the survival of stroke-prone rats. Pharmacol Res. 2011;63:284–293. doi: 10.1016/j.phrs.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Cherney DZ, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587–597. doi: 10.1161/CIRCULATIONAHA.113.005081. [DOI] [PubMed] [Google Scholar]
- 15.Tahara A, et al. Effects of SGLT2 selective inhibitor ipragliflozin on hyperglycemia, hyperlipidemia, hepatic steatosis, oxidative stress, inflammation, and obesity in type 2 diabetic mice. Eur J Pharmacol. 2013;715:246–255. doi: 10.1016/j.ejphar.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Haring HU, et al. Empagliflozin as add-on to metformin in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes care. 2014;37:1650–1659. doi: 10.2337/dc13-2105. [DOI] [PubMed] [Google Scholar]
- 17.Forst T, et al. Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes on background metformin and pioglitazone. Diabetes, obesity & metabolism. 2014;16:467–477. doi: 10.1111/dom.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whaley JM, et al. Targeting the kidney and glucose excretion with dapagliflozin: preclinical and clinical evidence for SGLT2 inhibition as a new option for treatment of type 2 diabetes mellitus. Diabetes, metabolic syndrome and obesity: targets and therapy. 2012;5:135–148. doi: 10.2147/DMSO.S22503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Neill J, et al. Acute SGLT inhibition normalizes O2 tension in the renal cortex but causes hypoxia in the renal medulla in anaesthetized control and diabetic rats. Am J Physiol Renal Physiol. 2015;309:F227–234. doi: 10.1152/ajprenal.00689.2014. [DOI] [PubMed] [Google Scholar]
- 20.Kim DU. Long-Term Regulation of Renal Urea Transporters during Antidiuresis. Electrolyte Blood Press. 2006;4:18–22. doi: 10.5049/EBP.2006.4.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pacurari M, et al. Endothelial cell transfusion ameliorates endothelial dysfunction in 5/6 nephrectomized rats. Am J Physiol Heart Circ Physiol. 2013;305:H1256–1264. doi: 10.1152/ajpheart.00132.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffin KA, Picken M, Bidani AK. Method of renal mass reduction is a critical modulator of subsequent hypertension and glomerular injury. J Am Soc Nephrol. 1994;4:2023–2031. doi: 10.1681/ASN.V4122023. [DOI] [PubMed] [Google Scholar]
- 23.Pollock DM, Divish BJ, Polakowski JS, Opgenorth TJ. Angiotensin II receptor blockade improves renal function in rats with reduced renal mass. J Pharmacol Exp Ther. 1993;267:657–663. [PubMed] [Google Scholar]
- 24.Zhang Y, Thai K, Kepecs DM, Gilbert RE. Sodium-Glucose Linked Cotransporter-2 Inhibition Does Not Attenuate Disease Progression in the Rat Remnant Kidney Model of Chronic Kidney Disease. PLoS One. 2016;11 doi: 10.1371/journal.pone.0144640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muller-Suur R, Norlen BJ, Persson AE. Resetting of tubuloglomerular feedback in rat kidneys after unilateral nephrectomy. Kidney Int. 1980;18:48–57. doi: 10.1038/ki.1980.109. [DOI] [PubMed] [Google Scholar]
- 26.Kwon TH, Frokiaer J, Knepper MA, Nielsen S. Reduced AQP1, -2, and -3 levels in kidneys of rats with CRF induced by surgical reduction in renal mass. Am J Physiol. 1998;275:F724–741. doi: 10.1152/ajprenal.1998.275.5.F724. [DOI] [PubMed] [Google Scholar]
- 27.Zanoli L, et al. Sodium-glucose linked transporter-2 inhibitors in chronic kidney disease. TheScientificWorldJournal. 2015;2015 doi: 10.1155/2015/317507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kwon TH, et al. Altered expression of Na transporters NHE-3, NaPi-II, Na-K-ATPase, BSC-1, and TSC in CRF rat kidneys. Am J Physiol. 1999;277:F257–270. doi: 10.1152/ajprenal.1999.277.2.F257. [DOI] [PubMed] [Google Scholar]
- 29.Chamberlain RM, Shirley DG. Time course of the renal functional response to partial nephrectomy: measurements in conscious rats. Exp Physiol. 2007;92:251–262. doi: 10.1113/expphysiol.2006.034751. [DOI] [PubMed] [Google Scholar]
- 30.Hayslett JP, Kashgarian M, Epstein FH. Mechanism of change in the excretion of sodium per nephron when renal mass is reduced. J Clin Invest. 1969;48:1002–1006. doi: 10.1172/JCI106056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diezi J, Michoud P, Grandchamp A, Giebisch G. Effects of nephrectomy on renal salt and water transport in the remaining kidney. Kidney Int. 1976;10:450–462. doi: 10.1038/ki.1976.132. [DOI] [PubMed] [Google Scholar]
- 32.Gava AL, Freitas FP, Balarini CM, Vasquez EC, Meyrelles SS. Effects of 5/6 nephrectomy on renal function and blood pressure in mice. International journal of physiology, pathophysiology and pharmacology. 2012;4:167–173. [PMC free article] [PubMed] [Google Scholar]
- 33.Li X, Chen G, Yang B. Urea transporter physiology studied in knockout mice. Front Physiol. 2012;3 doi: 10.3389/fphys.2012.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pessoa TD, Campos LC, Carraro-Lacroix L, Girardi AC, Malnic G. Functional role of glucose metabolism, osmotic stress, and sodium-glucose cotransporter isoform-mediated transport on Na+/H+ exchanger isoform 3 activity in the renal proximal tubule. J Am Soc Nephrol. 2014;25:2028–2039. doi: 10.1681/ASN.2013060588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knight TF, Sansom S, Hawk L, Frankfurt SJ, Weinman EJ. The effects of anesthesia on the excretion of an isotonic saline load in the rat. Pflugers Arch. 1978;373:139–143. doi: 10.1007/BF00584852. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.