Abstract
Background
Malalignment of the lower extremity is commonly seen in patients with severe osteoarthritis undergoing total knee arthroplasty (TKA) and is believed to play a role in quadriceps strength loss. Deformity correction is typically achieved through surgical techniques to provide appropriate ligamentous balancing. Therefore, this study examined the influence of change in lower extremity alignment on quadriceps strength outcomes following TKA.
Methods
Seventy-three participants (36 male; mean age 62 years; mean BMI 29.7) undergoing primary unilateral TKA were used in this investigation. Prior to surgery and at 1 and 6 months following surgery measures of isometric knee extensor strength, quadriceps activation, and long standing plain films were collected. Using the films, measures of Mechanical Axis (MA), Distal Femoral Angle (DFA), Proximal Tibial Angle (PTA), and Patellar Femoral Angle (PFA) were performed. Hierarchical linear regression was used to evaluate how change in alignment from baseline to 1 and 6 months influenced the change in quadriceps strength.
Results
DFA was found to significantly contribute to changes in quadriceps strength at 1 and 6 months following TKA, above that contributed by associated covariates. None of the other measures of lower extremity alignment were found to contribute to quadriceps strength in this sample.
Conclusion
Reductions in quadriceps strength experienced following TKA are likely to be influenced by changes in lower extremity alignment. Specifically, measures of DFA angle were found to significantly contribute to these changes. Future work is needed to prospectively examine measures of lower extremity alignment change and recovery following TKA.
Keywords: TKA, quadriceps strength, lower extremity alignment
Introduction
Malalignment of the lower extremity is commonly seen in patients with severe osteoarthritis undergoing a total knee arthroplasty (TKA).[1, 2] Deformity correction is typically achieved through a combination of planned bone resection and soft tissue releases to provide appropriate ligamentous balancing.[3, 4] Early after TKA, patients will experience significant declines in quadriceps strength, with deficits as high as 60% compared to pre-operative values at 1 month after TKA.[5–7] Failure to resolve limitations in quadriceps strength in the early post-operative period can result in residual deficits impacting physical function more than one year following the operative procedure.[5, 7, 8] Interestingly, the relationship between the magnitude of surgical deformity correction and quadriceps strength has yet to be fully elucidated.[9, 10] Previous studies, including those examining the use of computer assisted techniques, have been primarily limited to self-reported outcomes, and fail to capture meaningful declines in quadriceps strength likely to impact function during the early postoperative period.[11, 12] Furthermore, those that have examined relationships between surgical deformity and strength outcomes have been limited to one measurement of alignment: mechanical axis (MA).[13, 14] Additional measures of alignment, including the distal femoral angle (DFA), proximal tibial angle (PTA) and patellofemoral alignment (PFA) correction, have not been studied as potential contributors to quadriceps strength loss after TKA. Given the paucity of literature, understanding the relationship between each of these measures and the critical outcome of quadriceps strength is important, and may help guide future surgical decision making.
The purpose of this study was to determine whether the magnitude of lower extremity alignment correction, measured using alignment parameters including the MA, DFA, PTA, and PFA contribute to changes in quadriceps strength from before TKA to 1 and 6 months after TKA. We hypothesize that larger changes in these measures will result in greater deficits in quadriceps muscle strength after TKA.
Methods
Approval for this study was obtained by our institutional review board prior to initiation. A review of patients undergoing primary TKA from at our institution between May 2011 and August 2015 was performed. All patients underwent a primary TKA using a posterior-stabilized cemented TKA implanted using a gap-balancing method by five surgeons. A gap-balancing technique was used which involves cutting the distal femur and proximal tibia to create the extension gap. The extension gap was then assessed and appropriate soft tissue releases were sequentially performed in a standardized fashion until coronal plane balance was achieved. All limbs were aligned to have neutral mechanical axis alignment. The flexion gap was then matched (balanced) to the extension gap via precise rotation of the femoral component. Additionally, 68 of 73 participants who underwent this procedure received patellar resurfacing. Inclusion for the study were patients who received unilateral total knee replacement nested within a larger randomized clinical trial (RCT) (NCT01537328). Participants were excluded if they reported contralateral knee pain greater than 4 on a numerical pain rating scale (NPRS) that limited function, previous knee surgery in the last 12 months, uncontrolled diabetes (HbA1C>7.0), or the presence of unstable cardiovascular, neurological, or other disease limiting function. All patients received no preoperative physical therapy and were provided the same standard rehabilitation protocol for TKA, consisting of a standard set of core exercises as previously described.[15] Outcome variables were assessed preoperatively and at 1 and 6 month follow-up appointments in 73 patients for whom full-length standing radiographs were available pre and post TKA.
Outcome Variables
Isometric Quadriceps Muscle Strength and Activation
Maximal isometric quadriceps muscle strength was measured using a HUMAC NORM (CSMi, Stoughton, MA) electromechanical dynamometer, with the patient positioned as previously described.[16] Isometric quadriceps muscle strength was normalized to body weight for between subject comparisons. Quadriceps muscle activation was tested using the doublet interpolation technique, where a supramaximal stimulus (2-pulse, 600-μs pulse duration, 100-Hz electrical train) was applied during a maximum voluntary isometric contraction (MVIC) and again, immediately afterwards, while the quadriceps muscle was at rest. A value of 100% represents full voluntary muscle activation; less than 100% indicates incomplete motor unit recruitment or decreased motor unit discharge rates.[17, 18] Strength and activation data were collected using a Biopac Data Acquisition System.
Predictor Variables
Lower Extremity Deformity Correction
All radiographic measurements were retrospectively assessed by author JJ, an adult reconstruction fellowship trained orthopedic surgeon, blinded to strength outcomes and covariate predictor variables at the time of radiographic measurement. The following previously described radiographic parameters were used to determine the magnitude of deformity correction between the preoperative and postoperative images: MA (Figures 1A&1B), DFA (Figures 2A&2B), PTA (Figures 3A&3B), and the PFA (Figure 4A&4B).
Figures 1.


A&B: Measures of preoperative deformity and postoperative correction of the mechanical axis.
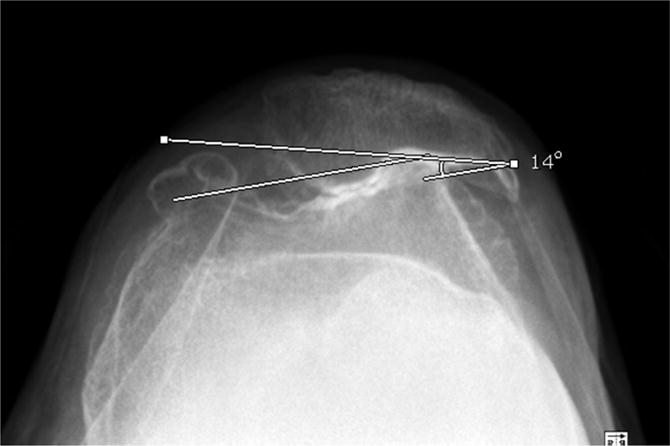
Figures 2.


A&B: Measures of preoperative deformity and postoperative correction of the distal femoral angle.
Figures 3.


A&B: Measures of preoperative deformity and postoperative correction of the proximal tibial angle.
Figures 4.
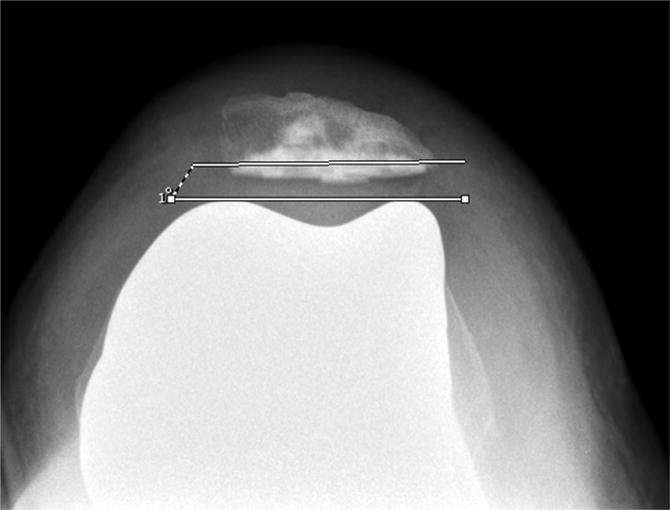
A&B: Measures of preoperative deformity and postoperative correction of the patellofemoral angle.
Statistical Approach
Distributions of radiographic change scores did not meet assumptions of normality, thus changes in surgical alignment were calculated as absolute values and dichotomized using a median split. Each outcome at 1 month and 6 months was regressed separately on all predictor variables, along with known confounders of age, gender, and body mass index (BMI), with adjustment for baseline values. Any variable that contributed meaningfully to prediction of these outcomes (p<0.10) was entered in a multivariable, hierarchical model.[19] We used hierarchical linear regression to evaluate how alignment changes during surgery influence quadriceps strength change beyond the influence of the known confounders of age, gender, BMI, quadriceps activation, and baseline strength or function. Because each of the four surgical deformity corrections we evaluated rarely occur in isolation, it was decided to use hierarchical regression to evaluate the overall influence of surgical correction (the entire group of significant surgical variables from univariate analysis) on the outcome of quadriceps strength. Our primary hypothesis was that a high degree of deformity correction during surgery would be associated with poorer quadriceps strength outcomes both at 1 and 6 months. Separate hierarchical models were used for the change in quadriceps strength at 1 and at 6 months.
Both models had 3 steps. In step 1, we entered the baseline values of quadriceps strength to account for differences in change scores. In step 2, we entered meaningful covariates from the univariate regression. In step 3, we entered surgical alignment change values for MA, DFA, PFA, and PTA that were meaningful in the univariate regression. Partial F-tests were used to determine if the variables included in each step contributed significantly to the variance in the linear model. Goodness of fit was evaluated by testing the residuals for normality and homoscedasticity. Because of the exploratory nature of this study, we did not correct alpha to account for multiple analyses. A p<.05 (2-tailed) was considered to be significant. All analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Baseline measures of MA, DFA, PTA, and PFA are presented in Table 1. Baseline characteristics including demographic, anthropometric, and radiographic alignment values for participants are included in Table 2.
Table 1.
Baseline Radiographic Alignment Mean (95% CI)
| Measure | Degrees |
|---|---|
| Mechanical Axis | 175.84 (174.31 – 177.36) |
| Distal Femoral Angle | 96.08 (95.44 – 96.72) |
| Proximal Tibial Angle | 87.16 (86.47 – 87.86) |
| Patellar Femoral Angle | 6.48 (5.04 – 7.92) |
Table 2.
Baseline Characteristics of patients separated by median split in change in each of the radiographic measures.
| MA Change | P value | PT Change | P value | PF change | P value | DF change | P value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥ 4 | <4 | ≥ 3 | < 3 | ≥ 6 | < 6 | ≥ 2 | < 2 | |||||
| N | 43 | 30 | – | 44 | 29 | – | 38 | 35 | – | 52 | 21 | – |
| Sex (% male) | 54.05 | 45.95 | 0.39 | 59.5 | 40.5 | 0.88 | 51.4 | 48.6 | 0.9 | 81.1 | 18.9 | 0.05 |
| BMI | 30.2 | 28.9 | 0.29 | 29.5 | 30.1 | 0.59 | 29.4 | 29.9 | 0.68 | 30.0 | 28.9 | 0.33 |
| Age (years) | 61.8 | 63.6 | 0.47 | 61.9 | 63.4 | 0.40 | 61.9 | 63.2 | 0.47 | 61.8 | 64.3 | 0.23 |
| Normalized Quadriceps strength (N-m/kg) | 1.34 | 1.19 | 0.29 | 1.33 | 1.20 | 0.34 | 1.26 | 1.30 | 0.73 | 1.27 | 1.30 | 0.79 |
| Mechanical Axis Angle | 173.8 | 178.7 | 0.0003* | 174.1 | 178.5 | 0.003* | 177.0 | 174.6 | 0.11 | 176.3 | 174.8 | 0.39 |
| Proximal Tibial Angle | 86.3 | 88.5 | 0.0006* | 85.7 | 89.4 | 0.0001* | 87.4 | 86.9 | 0.49 | 87.2 | 87.1 | 0.97 |
| Patellar Femoral Angle | 6.0 | 7.1 | 0.48 | 6.7 | 6.1 | 0.68 | 7.2 | 5.7 | 0.31 | 7.6 | 3.7 | 0.01* |
| Distal Femoral Angle | 95.4 | 97.1 | 0.005* | 95.8 | 96.4 | 0.39 | 96.6 | 95.5 | 0.09 | 96.3 | 95.7 | 0.29 |
The beta coefficients and p-values for the univariate analysis of the predictor variables and quadriceps strength change are presented in Table 3a and 3b respectively. In the univariate regression model, age, BMI, quadriceps activation, and DFA were all significant contributors to changes in normalized quadriceps strength at one month. Specific to our research questions, a greater change in DFA was significantly related to lower normalized quadriceps strength (.25 Newton-meters/kg) at one month post TKA (p<.001). In the univariate analysis at six months following TKA, sex, BMI, quadriceps activation, and DFA contributed significantly to quadriceps strength. Specifically, greater change in DFA was associated with significantly (p<.001) lower normalized quadriceps strength (0.32 N-m/kg) at 6 months.
Table 3.
Univariate analysis of change in normalized quadriceps strength from baseline to 1 and 6 months regressed on known covariates (3a) and radiographic measures (3b).
| 3a. Covariates | |||||
|---|---|---|---|---|---|
| 1 month | Change in Normalized Quadriceps strength (N-m/kg) | 6 month | Change in Normalized Quadriceps strength (N-m/kg) | ||
| Beta Coefficient | p-value | Beta Coefficient | p-value | ||
| Age | 0.014 | 0.0034** | Age | <0.001 | 0.95 |
| Sex | −0.07 | 0.43 | Sex | −0.32 | 0.0015** |
| BMI | −0.03 | 0.0007** | BMI | −0.03 | 0.0005** |
| Quadriceps Activation | 0.01 | <0.0001** | Quadriceps Activation | 0.01 | 0.0031** |
| 3b. Radiographic measures | |||||
|---|---|---|---|---|---|
| 1 month | Change in Normalized Quadriceps strength (N-m/kg) | 6 month | Change in Normalized Quadriceps strength (N-m/kg) | ||
| Beta Coefficient | p-value | Beta Coefficient | P-value | ||
| MA | 0.09 | 0.19 | MA | 0.08 | 0.41 |
| DF | −0.25 | 0.0009** | DF | −0.32 | 0.0007** |
| PF | −0.03 | 0.67 | PF | −0.06 | 0.53 |
| PT | −0.06 | 0.41 | PT | −0.09 | 0.34 |
indicates variables found to have p<0.2 and included in hierarchical model building.
indicate variables found to significantly (p<0.05) relate to quadriceps strength change in univariate regression.
Significant variables from the univariate analysis above were retained for the hierarchical multivariable regression. Each step of the hierarchical regression was tested using a partial F-test to determine whether the addition of each group of variables contributed significantly to variance in normalized strength and to give an estimate of the magnitude of each contribution. In the first step, change in quadriceps strength was regressed on baseline quadriceps strength. Baseline strength values were significant contributors to the variance (adj. R2) in quadriceps strength change at both 1 and 6 months after TKA (Table 4). The addition of each group of confounders meeting inclusion (p<0.1; Table 3a) from univariate regression (step 2) also resulted in significant contributions to 1 and 6 month quadriceps strength change in the regression model (Table 4).
Table 4.
Results of 3 step hierarchical regression analysis of change in quadriceps strength from baseline to 1 and 6 months post-TKA. Step 1) inclusion of baseline quadriceps strength, step 2) baseline strength and covariates meeting inclusion criteria in univariate regression, and step 3) baseline strength with covariates and radiographic variables meeting inclusion criteria of univariate regression.
| 1 Month Change | Adj. R2 | ΔF-statistic | p-value | |
|---|---|---|---|---|
| Step 1 | Baseline strength | 0.54 | 84.26 | <0.0001* |
| Step 2 | Baseline + Covariates (Age, BMI and Quadriceps Activation) | 0. 82 | 17.33 | <0.0001* |
| Step 3 | Baseline + Covariates + (DF) Radiographic | 0. 86 | 7.52 | 0.0008* |
| 6 month change | Adj. R2 | ΔF-statistic | p-value | |
|---|---|---|---|---|
| Step 1 | Baseline strength | 0.28 | 26.70 | <0.0001* |
| Step 2 | Baseline + Covariates (Sex, BMI and Quadriceps Activation) | 0.61 | 4.3 | <0.0001* |
| Step 3 | Baseline strength + Covariates + Radiographic (DF) | 0.65 | 1.53 | 0.02* |
p-values of partial F-test with significance set at p<0.05
Finally, the addition of radiographic variables meeting inclusion (p<0.1; Table 3b) from univariate regression were included as a third step of the hierarchical regression modeling. Using this criteria, only DFA was found to meet a level of significance for inclusion. The addition of DFA to the hierarchical model was found to significantly contribute (p<0.05) to change in quadriceps strength from baseline to 1 month post-TKA. This addition explained an additional 4% of the variability in quadriceps strength change (change in adjusted R2 from .82 to .86). Similarly, when DFA was added to the hierarchical model for change in quadriceps strength from baseline to 6 months post-TKA, a 4% contribution to the variability was also observed.
Discussion
Although numerous studies have reported outcomes in patients with restoration of a relatively neutral mechanical axis, to our knowledge, this study represents the first attempt to correlate the magnitude of deformity correction after TKA with quadriceps strength deficits. Our findings suggest DFA has a significant relationship to the change in quadriceps strength indicating the need for future prospective analysis powered to more specifically examine this relationship.
Declines in quadriceps strength following TKA are significant and remain a major barrier to optimizing recovery following surgery. Multiple factors associated with the surgical procedure have been studied for influence on quadriceps strength following TKA including minimally invasive surgery[20], tourniquet use[21], and computer assisted surgery[22, 23]. In addition, studies have examined the influence of lower extremity alignment on certain outcomes following TKA. These studies have primarily examined complication rates and prosthesis longevity[24, 25].
Stucinskas et al.,[14] investigated the influence of coronal alignment of the mechanical axis on strength and functional outcomes. Their results suggest no significant differences between the two groups on measures of quadriceps strength, knee range of motion, and Knee Society Score (KSS). In concordance with this study, Matziolis et al.[26] found no differences between patients in KSS, WOMAC, or SF-36 based on post-operative alignment. On the contrary, others have reported improved outcomes in those patients with a neutral alignment without mention of actual deformity correction.[13, 23, 27] However, by quantifying the magnitude of change in a comprehensive battery of lower extremity alignment measures the current study provides a more complete picture of how multiple measures of lower extremity alignment may influence patient quadriceps strength change.
The magnitude of change in the DFA angle was found to significantly contribute to changes in quadriceps strength in this sample. Patients with a greater than 2 degree change in DFA angle during the surgery had significantly reduced quadriceps strength at 1 and 6 months post TKA. This relationship remained significant after adjusting for known contributors to post-operative quadriceps strength, suggesting the relationship between DFA and quadriceps strength is meaningful. This relationship may be especially meaningful to patients attempting to rehabilitate to high levels of function, such as return to sport or work.
We believe that quadriceps strength change may be more sensitive to smaller corrections in DFA secondary to its intimate relationship with the quadriceps musculature. These small alignment changes may have a greater impact on chronically shortened and lengthened sarcomeres which results in a greater disruption of the muscle length-tension relationship for maximal force generation. This finding is intriguing as it poses a critical surgical consideration—is a larger correction of the lower extremity alignment (i.e. greater change of the DFA) beneficial if it reduces strength—but helps to restore mechanical alignment. Future studies exploring the role of mechanical alignment vs. kinematic alignment in this area is an interest to the authors.
There were several limitations to this study. It was retrospectively performed with regards to radiographic assessment and therefore, suffers the inherent limitations of the study design. Due to the exploratory nature of this analysis and our limited sample size the authors chose a more liberal alpha level of 0.1 to identify radiographic variables likely to contribute to quadriceps strength change in a more robust sample. Furthermore, we were limited by the small sample of patients available from the parent RCT and, therefore, unlikely to have a sample with extremes of deformity correction. This also limited our ability to determine the influence of patellar resurfacing on quadriceps strength change, as nearly our entire sample (>93%) had undergone patellar resurfacing. Yet, even with a small cohort, we noted statistically significant differences in our preoperative radiographic parameters with regards to DFA. There were 5 surgeons performing the TKAs in this study. We concede there may have been minor variations in technique which may contribute to subtle differences in outcomes. However, at our institution, surgeons follow similar techniques with regards to gap balancing and the algorithms used for soft tissue releases to achieve ligamentous balance with appropriate coronal alignment. Lastly, we did not investigate the relationship between deformity correction and functional performance, however, previous studies have shown that quadriceps strength is closely related to recovery of function following TKA.[6] Lastly, subjects were only tested at a maximum follow-up duration of six months. We are therefore unable to comments if the findings of this report persist at long-term follow-up evaluation.
Conclusions
Quadriceps strength loss represents a significant challenge after TKA. This study serves as an important first step in identifying how changes in lower extremity alignment, occurring as a result of surgery, play a critical role in recovery of quadriceps strength after TKA. It appears that quadriceps strength is most sensitive to changes in DFA, according to our findings. Future studies are needed to see if these changes correlate with patient functional outcomes and to examine the influence of patellar resurfacing on the recovery of quadriceps strength.
Acknowledgments
Funding: This work was supported by the National Institutes of Health (R01- HD06590) and the National Institutes of Health University of Colorado, Center on Aging Training Grant (NIH T32 AG000279).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fukagawa S, Matsuda S, Mizu-uchi H, Miura H, Okazaki K, Iwamoto Y. Changes in patellar alignment after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(1):99. doi: 10.1007/s00167-010-1164-7. [DOI] [PubMed] [Google Scholar]
- 2.Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meloni MC, Hoedemaeker RW, Violante B, Mazzola C. Soft tissue balancing in total knee arthroplasty. Joints. 2014;2(1):37. [PMC free article] [PubMed] [Google Scholar]
- 4.Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. The Journal of bone and joint surgery American. 2005;87(Suppl 1(Pt 2)):271. doi: 10.2106/JBJS.E.00308. [DOI] [PubMed] [Google Scholar]
- 5.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. journal of orthopaedic & sports physical therapy. 2010;40(9):559. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clinical Biomechanics. 2008;23(3):320. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meier W, Mizner RL, Marcus RL, Dibble LE, Peters C, Lastayo PC. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther. 2008;38(5):246. doi: 10.2519/jospt.2008.2715. [DOI] [PubMed] [Google Scholar]
- 8.Yoshida Y, Zeni J, Snyder-Mackler L. Do Patients Achieve Normal Gait Patterns 3 Years After Total Knee Arthroplasty? The Journal of orthopaedic and sports physical therapy. 2012;42(12):1039. doi: 10.2519/jospt.2012.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? The Journal of arthroplasty. 2009;24(6):39. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 10.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. The Journal of arthroplasty. 2009;24(4):570. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Stevens-Lapsley JE, Schenkman ML, Dayton MR. Comparison of self-reported knee injury and osteoarthritis outcome score to performance measures in patients after total knee arthroplasty. PMR. 2011;3(6):541. doi: 10.1016/j.pmrj.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Dayton MR, Judd DL, Hogan CA, Stevens-Lapsley JE. Performance-based versus self-reported outcomes using the HOOS following total hip arthroplasty. American journal of physical medicine & rehabilitation/Association of Academic Physiatrists. 2016;95(2):132. doi: 10.1097/PHM.0000000000000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang NF, Dowsey MM, Ee E, Stoney JD, Babazadeh S, Choong PF. Coronal alignment correlates with outcome after total knee arthroplasty: five-year follow-up of a randomized controlled trial. The Journal of arthroplasty. 2012;27(9):1737. doi: 10.1016/j.arth.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 14.Stucinskas J, Robertsson O, Sirka A, Lebedev A, Wingstrand H, Tarasevicius S. Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength: 91 patients assessed after 1 year. Acta orthopaedica. 2015;86(6):728. doi: 10.3109/17453674.2015.1059689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41(12):932. doi: 10.2519/jospt.2011.3734. [DOI] [PubMed] [Google Scholar]
- 16.Mintken PE, Carpenter KJ, Eckhoff D, Kohrt WM, Stevens JE. Early neuromuscular electrical stimulation to optimize quadriceps muscle function following total knee arthroplasty: a case report. journal of orthopaedic & sports physical therapy. 2007;37(7):364. doi: 10.2519/jospt.2007.2541. [DOI] [PubMed] [Google Scholar]
- 17.Behm D, Power K, Drinkwater E. Comparison of interpolation and central activation ratios as measures of muscle inactivation. Muscle & nerve. 2001;24(7):925. doi: 10.1002/mus.1090. [DOI] [PubMed] [Google Scholar]
- 18.Behm D, St-Pierre D, Perez D. Muscle inactivation: assessment of interpolated twitch technique. Journal of Applied Physiology. 1996;81(5):2267. doi: 10.1152/jappl.1996.81.5.2267. [DOI] [PubMed] [Google Scholar]
- 19.Austin PC, Tu JV. Automated variable selection methods for logistic regression produced unstable models for predicting acute myocardial infarction mortality. Journal of clinical epidemiology. 2004;57(11):1138. doi: 10.1016/j.jclinepi.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Stevens-Lapsley JE, Bade MJ, Shulman BC, Kohrt WM, Dayton MR. Minimally invasive total knee arthroplasty improves early knee strength but not functional performance: a randomized controlled trial. J Arthroplasty. 2012;27(10):1812. doi: 10.1016/j.arth.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE. Does Tourniquet Use in TKA Affect Recovery of Lower Extremity Strength and Function? A Randomized Trial. Clin Orthop Relat Res. 2016;474(1):69. doi: 10.1007/s11999-015-4393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. The Journal of arthroplasty. 2007;22(8):1097. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. The Journal of arthroplasty. 2009;24(4):560. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y-H, Park J-W, Kim J-S, Park S-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. International orthopaedics. 2014;38(2):379. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim Y-H, Kim J-S, Yoon S-H. Alignment and orientation of the components in total knee replacement with and without navigation support A PROSPECTIVE, RANDOMISED STUDY. Journal of Bone & Joint Surgery, British Volume. 2007;89(4):471. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 26.Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Archives of orthopaedic and trauma surgery. 2010;130(12):1487. doi: 10.1007/s00402-010-1064-9. [DOI] [PubMed] [Google Scholar]
- 27.Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clinical Orthopaedics and Related Research®. 2011;469(12):3443. doi: 10.1007/s11999-011-1988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


