Abstract
Influenza virus evolves rapidly to constantly escape from natural immunity. Most humoral immune responses to influenza virus target the hemagglutinin glycoprotein (HA), which is the major antigen on the surface of the virus. The HA is comprised of a globular head domain for receptor binding and a stem domain for membrane fusion. The major antigenic sites of HA are located in the globular head subdomain, which is highly tolerant of amino-acid substitutions and continual addition of glycosylation sites. Nonetheless, the evolution of the receptor-binding site (RBS) and the stem region on HA is severely constrained by their functional roles in engaging the host receptor and in mediating membrane fusion, respectively. Here, we review how broadly neutralizing antibodies (bnAbs) exploit these evolutionary constraints to protect against diverse influenza strains. We also discuss the emerging role of other epitopes that are conserved only in subsets of viruses. This rapidly increasing knowledge of the evolutionary biology, immunology, structural biology, and virology of influenza virus is invaluable for development and design of more universal influenza vaccines as well as novel therapeutics.
Graphical abstract

Introduction
Influenza virus imposes a substantial health and socioeconomic burden globally [1]. There are four known types of influenza virus, named as A-D. Type A and B viruses circulate in human population and are responsible for pandemics (type A), epidemics and seasonal outbreaks (types A and B), while type C and the recently discovered type D [2] viruses do not cause significant disease or epidemics. Influenza A viruses are further classified into subtypes according to the antigenic properties of their two viral surface glycoproteins, namely the hemagglutinin (HA) and neuraminidase (NA). There are 18 known HA subtypes (H1 to H18) and 11 known NA subtypes (N1 to N11) [3]. The 18 HA subtypes can further be classified into group 1 (H1, H2, H5, H6, H7, H8, H9, H11, H12, H13, H16, H17, and H18) or group 2 (H3, H4, H7, H10, H14, and H15) [4]. Out of the 198 (11 × 18) possible combinations, only three (H1N1, H2N2, H3N2) are known to have caused human pandemics. The main natural reservoir for influenza A viruses are wild aquatic birds, but domestic poultry also become infected and hence harbor influenza A viruses [5, 6]. Pigs and other mammals, such as horses, dogs, seals, minks, and bats [7], can also be infected by influenza A viruses and contribute to possible sources of viruses that infect humans [5]. Certain subtypes found in natural reservoirs occasionally emerge in the human population, as exemplified by H5N1, H5N6, H6N1, H7N7, H7N9, H9N2, and H10N8 viruses. Some of these zoonotic subtypes can be highly pathogenic and have a high mortality rate (>50% of hospitalized individuals) when infecting humans [8, 9].
Influenza has been a long-term threat to humans and the first major pandemic that was documented was that of the 1918 H1N1 Spanish flu that was responsible for more than 50 million deaths worldwide [10, 11]. Since then, there were three pandemics, namely the Asian flu (H2N2) pandemic in 1957, the Hong Kong flu (H3N2) pandemic in 1968, and the most recent swine flu (H1N1) pandemic in 2009. Over the past five decades, annual (seasonal) outbreaks have been caused by influenza A H1N1 and H3N2 subtypes as well as the two lineages of influenza B virus (B/Victoria/2/87 and B/Yamagata/16/88). As compared to influenza B, influenza A generally results in higher morbidity and mortality [12, 13]. In addition, influenza A viruses evolve three times faster than influenza B viruses [14, 15]. Therefore, influenza A viruses have often received more attention and concern as a global threat compared to influenza B viruses [16]. Of note, the quadrivalent influenza vaccine that is recently licensed in many countries [17] now offers protection against both lineages of influenza B virus as well as the two influenza A subtypes [18].
Among all influenza virus proteins, HA evolves at the highest rate [19, 20] due to it being the major target of the immune response. Phylogenetic analysis suggests that different HA subtypes of influenza A virus diverged around 2,000 years ago [21]. Although the protein sequences of their HAs share as low as 40% sequence identity, they adopt the same protein fold [22]. As a class I viral fusion protein, HA plays an important role for viral entry by binding to the host receptor, sialylated glycans on endothelial cells in the respiratory tract, and facilitating membrane fusion in the low pH environment of the endosomal compartments after cell entry via endocytosis. During virus replication, the uncleaved precursor of the HA, namely HA0, is synthesized and is then cleaved by cellular proteases into two subunits HA1 and HA2, to produce the fully functional form of the protein [23]. Although this cleavage is usually catalyzed by trypsin-like serine endoproteases [24, 25], HAs from highly pathogenic H5 and H7 subtypes that contain a polybasic cleavage site can also be cleaved by the ubiquitous protease furin [26–28]. This maturation process is a prerequisite to attain the fusion-competent, metastable form of the HA that undergoes the large conformational rearrangements required for the membrane fusion process.
While a large portion of HA1 amino-acid sequence is highly variable [22] and is intrinsically tolerable to mutations, the receptor-binding site (RBS) is an exception [29, 30]. The HA RBS is composed of the 130-loop, 150-loop, 190-helix, and 220-loop, named after their relative positions on the HA amino-acid sequence. The stem region, which is composed primarily of HA2 with some residues from the N- and C- termini of HA1, is even more conserved [22]. During the membrane fusion process that is triggered by acidic pH [31–33], the α-helices in stem region [34] undergo large conformational rearrangements to form a 100 Å triple-helical coiled-coil [35]. This molecular machine consists of many moving parts that impose strong evolutionary constraints on many residues in the stem region.
Influenza H1N1 and H3N2 viruses entered the human population in 1918 and 1968, respectively [36]. While the seasonal H3N2 virus continues to circulate until the present day, the history of human H1N1 virus is more complex [36, 37]. In the last century, the human H1N1 virus first appeared in 1918, but discontinued circulating in human population in 1957 for around 20 years. It remerged in 1977 as a relatively benign epidemic and continued to circulate as a seasonal virus until 2009, when the pandemic swine flu (A(H1N1)pdm09) emerged and displaced the seasonal H1N1 virus. Of note, HAs from both seasonal H1N1 virus and A(H1N1)pdm09 are derived from the HA of 1918 Spanish flu, while the other genes have different origins [38]. Nonetheless, the seasonal H1N1 virus had mutated so much that was antigenically very distant from both the 1918 Spanish flu and the A(H1N1)pdm09. Thus, when the A(H1N1)pdm09 emerged, immunity was lacking in the younger to middle-aged population [39]. Despite the difference in circulation history between H1N1 and H3N2 subtypes in human population, both subtypes are subjected to continual pressure to escape from the human immune system.
In this review, we will discuss the interplay between immune evasion associated with influenza virus, the countermeasures offered by the humoral immune system to combat ongoing variation in influenza viruses, and the requirement for the virus to maintain function throughout this complex evolutionary process. We will mostly focus on the HA protein due to its role as the main antigen of influenza virus and the major seasonal vaccine target, but will also touch on the emerging role of anti-neuraminidase antibodies. Throughout this review, all residues on HA are named according to H3 numbering.
Antigenic drift: point mutations and glycosylation
Most antibodies elicited by influenza virus by natural infection and vaccination target the globular head domain of HA1, which is distal from the virus surface and readily accessible for immune recognition. Influenza virus HA, in turn, mutates to escape from pre-existing immunity. This mutation-based immune evasion process is known as antigenic drift. Early studies proposed five major antigenic sites in the HA1 globular head domain for both H1 and H3 HAs [40–44], namely Sa, Sb, Ca1, Ca2, and Cb for H1 HA [40, 41] (Fig. 1a), and sites A-E for H3 HA [42–44] (Fig. 1b). The locations of Sa, Sb and Ca2 of H1 HA, and antigenic sites A and B of H3 HA partially overlap with the RBS, whereas Ca1 and Cb of H1 HA, and antigenic sites C-E of H3 HA are more distant from the RBS. These antigenic sites provide a structural framework to understand the evolutionary dynamics and constraints of influenza virus in response to humoral immunity.
Figure 1. Major antigenic sites on HA.
(a) The locations of the five major antigenic sites on H1 HA [40, 41] are shown on the HA trimer structure of A/California/04/2009 (PDB 3UBE) [84]. (b) The locations of the five major antigenic sites on H3 HA [42–44] shown on the HA trimer structure of A/Hong Kong/1/1968 (PDB 2YPG) [85]. (a–b) The human receptor analog pentasaccharide lactoseries tetrasaccharide c (LSTc) is shown in sticks representation (yellow).
Over the past half-century, the HAs from human H3N2 viruses have accumulated at least 75 substitutions (13% of the entire protein) (Fig. 2a–b). Interestingly, most mutations that account for major antigenic drift in human H3N2 viruses reside within or immediately proximate to the RBS [45–48] (Fig. 2c). Similar observations are found in the recent antigenic drift of A(H1N1)pdm09 and type B viruses [48–50]. Thus, there seems to be a preference for neutralizing antibodies to target the RBS-proximal region. One explanation is that targeting the RBS-proximal region can sterically hinder receptor binding to achieve neutralization. Another plausible explanation is the location of the glycosylation sites on the HA. In both H1N1 and H3N2 viruses, the number of N-glycosylation sites on the HA1 globular head domain has substantially increased since they were introduced into the human population [51–58]. For example, the number of N-glycosylation sites in the HA1 globular head domain of the human H1N1 virus increased from one to at least three sites per protomer (3 to 9 per trimer) from 1918 until its temporary eradication from the human population in 1957 [56, 57]. Similarly, the number of N-glycosylation sites in the HA1 globular head domain of the human H3N2 virus has constantly increased with up to 10 new sites being added over the past half-century [57–59], but only at least six additional sites per protomer (18 per trimer) being present in any circulating strain. Including the 5 highly conserved glycosylation sites per protomer (15 per trimer), the end result is a total of at least 33 glycosylation sites per trimer in current H3N2 viruses (Fig. 2d–e). Of note, some glycosylation sites only appear temporarily during the evolution of human H3N2 virus, such as Asn81, Asn276, and potentially Asn144. Accretion of conformationally flexible oligosaccharides on the HA further shields the antigenic sites to facilitate immune evasion [43, 59–62]. Nonetheless, the added N-glycosylation sites can also affect binding of the natural receptor when they are proximal to the RBS [54, 63–67]. The functional constraints of the RBS render it difficult, if not impossible, to be completely shielded by oligosaccharides. As an increasing proportion of the HA1 globular domain becomes masked by oligosaccharides, the RBS and its immediate proximal region becomes relatively more vulnerable to be targeted by antibodies which have specific features, such as long CDR loops (see below). This may explain why the more exposed RBS-proximal antigenic site B (Fig. 1b) has become immunodominant in recent years [47, 68].
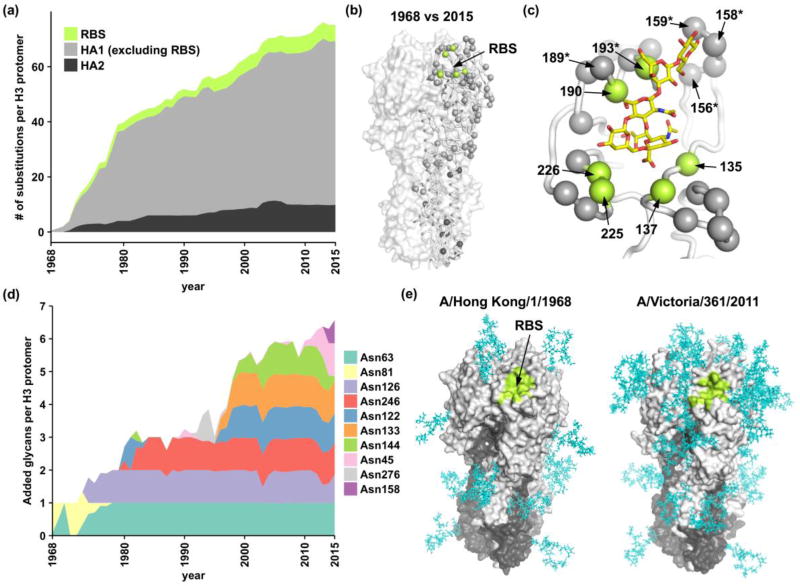
Figure 2. Natural substitutions and emerging N-glycosylation sites in the HA of human H3N2 viruses.
(a) Stacked graph showing the cumulative average number of amino-acid substitutions in the HA in strains isolated from different years as compared to the ancestral strain, A/Hong Kong/1/1968. (b–c) HA residues that have different amino-acid identities between A/Hong Kong/1/1968 and the consensus sequence of the 2015 human H3N2 strains are shown as spheres on one protomer of A/Hong Kong/1/1968 HA trimer (PDB 4FNK) [69]. The other two protomers are shown in surface representation. Color scheme follows that of panel a. (c) Zoom-in view for the receptor binding site (RBS) of A/Hong Kong/1/1968 in complex with a human receptor analog pentasaccharide lactoseries tetrasaccharide c (LSTc) (PDB 2YPG) [85]. LSTc is shown as yellow sticks (carbons) with nitrogens in blue and oxygens in red. Residues within the RBS are labeled. Residues responsible for major antigenic changes are labeled with asterisks [48]. (d) Stacked graph showing the normalized percentage of strains that contain the indicated N-glycosylation sites. While the N-glycosylation site Asn81 disappeared in year 1977, nine other N-glycosylation sites have emerged in human H3N2 viruses since 1968. Five absolutely conserved N-glycosylation sites in human H3 strains (HA1 Asn22, Asn38, Asn165, Asn285; HA2 Asn154) are not included in the stacked graph. This analysis includes a total of 4625 sequences were downloaded from Influenza Research Database [190]. This plot is an updated version of the plot in Lee et al., 2014 [58]. (e) Oligomannoses (cyan) on A/Hong Kong/1/1968 (PDB 4FNK) [69] and A/Victoria/361/2011 (PDB 4O5N) [58] were modeled by Glyprot [191]. HA1 is colored in grey and HA2 is colored in black. The receptor-binding site (RBS) is colored in lime. The absolutely conserved N-glycosylation sites in human H3 strains (HA1 Asn22, Asn38, Asn165, Asn285; HA2 Asn154) are included in the display.
Functionally conserved region 1: Receptor-binding site
As a functionally conserved region on the HA1 globular head domain, the RBS is a target for broadly neutralizing antibodies (bnAbs) [58, 69–81] (Fig. 3a–c). RBS-targeted bnAbs inhibit viral entry by preventing HA binding to its host receptor, and may also prevent HA conformational changes during membrane fusion by cross-linking neighboring subunits of the HA trimer [79]. Common features of RBS-targeted bnAbs have been gleaned through crystal structure determination of multiple antibody HA complexes [74] (Fig. 4a). These characteristics involve mimicking the binding mode of sialic acid to some extent using a single complementarity determining region (CDR) loop [78]. The most prevalent mimicry strategy is to insert a hydrophobic amino acid into the hydrophobic pocket that interacts with the acetamide group of sialic acid [78]. Many RBS-targeted bnAbs also interact with a polar pocket that is occupied by the sialic acid carboxylate group that forms numerous hydrogen bonds to the HA. Some antibodies mimic this interaction precisely by inserting an aspartic acid at the tip of one of its CDRs (H2 or H3) into this binding pocket [75, 76, 78–82].
Figure 3. Binding footprints of RBS-targeted bnAbs.
(a) Amino-acid sequence conservation is projected onto the HA structure of A/Hong Kong/1/1968 (PDB 4FNK) [69]. One protomer is shown in Cα ribbon representation and the other two protomers are shown in a surface representation. Human H1, H2, and H3 strains were used for computing the amino-acid sequence conservation. For each subtype, we randomly sampled at most 5 strains from each year for this analysis. (b) The sequence conservation of the HA RBS region of A/Hong Kong/1/1968 (PDB 4FNK) [69] is shown. Several highly conserved residues that interact with the sialic acid receptor are labeled. (c) The binding footprints of RBS-targeted bnAbs are shown on the structure of the HA RBS of A/Hong Kong/1/1968 (PDB 4FNK) [69]. Epitope usage represents the frequency of a specified residue being targeted by RBS-targeted bnAbs. Epitopes from nine RBS-targeted bnAbs, namely C05 [69], S139/1 [71], F045–092 [58], 2G1 [74], 8M2 [74], 5J8 [76], 1F1 [192], HC63 [79], and CH65 [75], were analyzed here. Locations of naturally occurring indels are indicated. (d–e) Same as panel b and c, except that the stem region is now shown. N38, which is a highly conserved N-glycosylation site in group 2 HAs, but not in group 1 HAs, is labeled. (e) Epitopes from nine stem-binding bnAbs, namely CR6261 [99], CR9114 [101], CR8043 [109], F10 [100], CR8020 [107], C179 [102], MEDI8852 [105], 39.29 [113], and FI6v3 [111], were analyzed here. Amino-acid substitutions associated with stem-binding bnAbs escape were annotated. HA1: T318K (C179 escape) [103]. HA2: D19N (CR8020 escape) [107], R25M (CR8043 escape) [109], G33E (CR8020 escape) [107], Q34R (CR8020 and CR8043 escape) [109], Q42K (39.29 escape) [118], D46Y/G (39.29 escape) [118], V52E (C179 escape) [103], and H111L (CR6261 escape) [108]. Of note, HA1 H111L is a buried behind the surface. “Site 1” indicates the epitope region of CR9114, CR6261, and other VH1–69 encoded stem-binding bnAbs. “Site 2” indicates the epitope region of the two group 2-specific stem-binding bnAbs, namely CR8020 and CR8043. Site 2 is lower down the stem as compared to site 1. “Both” indicates the overlapping region of sites 1 and 2.
Figure 4. Binding of broadly neutralizing antibody (bnAb) to influenza hemagglutinin (HA).
(a) Interaction between RBS-targeted bnAbs and HA is shown. Binding of C05 [69] (cyan; PDB 4FP8), S139/1 [71] (pink; PDB 4GMS), F045–092 [58] (lime; PDB 4O58), 2G1 [74] (purple; PDB 4HG4), 8M2 [74] (orange; PDB 4HFU), 5J8 [76] (blue; PDB 4M5Z), 1F1 [192] (green; PDB 4GXU), HC63 [79] (gray; PDB 1KEN), and CH65 [75] (red; PDB 5UGY) Fabs to HA trimer (white). (b) Interaction between stem-binding bnAbs and HA is shown. Binding of CR6261 [99] (yellow; PDB 3GBN), CR9114 [101] (blue; PDB 4FQI), CR8043 [109] (orange; PDB 4NM8), CR8020 [107] (cyan; PDB 3SDY), C179 [102] (red; PDB 4HLZ), MEDI8852 [105] (pink; PDB 5JW4), 39.29 [113] (green; PDB 4KVN), and FI6v3 [111] (gray; PDB 3ZTJ) Fabs to HA trimer (white). The curved arrow indicates that the approach angle has to be from no more than perpendicular to at an upward disposition to avoid a steric clash with the membrane. CR6261 Fab is obscured by CR9114 Fab, as they both have very similar angles of approach to the HA and, therefore, is not visible in these views. (c) The approach angle of RBS-targeted bnAbs and stem-binding bnAbs was quantified by adapting the method described in [115]. Briefly, the trimer axis of HA is on the z-axis such that the x-y plane (horizontal plane) represents the viral membrane. Vertical plane represents the y-z plane. The long axis of the Fab is defined as the line connecting the averaged coordinate of Cα-atoms of the conserved cysteines in the constant domain to that in the variable domain. The angle between the long axis of the Fab and the horizontal plane or the vertical plane is shown. (d) Binding of H5M9 [128] (wheat; PDB 4MHJ) and CR8071 [101] (teal; PDB 4FQJ) Fabs to the same protomer of the HA trimer (white). To visually compare their epitope locations with other bnAb epitopes, the RBS and the epitope of a stem-binding bnAb CR6261 are colored in lime and pink, respectively.
While the portion of the RBS that interacts with the sialic acid of sialoside receptors is very highly conserved, some amino-acid variation can be observed in natural circulating strains in the other regions of the RBS that interact with the other sugar moieties of the receptor. Structural and functional characterization has also revealed how HAs from human H1N1 and H3N2 viruses interact differently with human receptor analogs [83–91]. These differences are mostly attributed to amino-acid substitutions at residue 190 in the helix atop the RBS and to the 220-loop that interacts with Gal-2 of the receptor analog. Furthermore, evolution of residues in the 150-loop, 190-helix, and 220-loop in recent human H3N2 viruses are observed [85], which has resulted in bias of the receptor preference towards long, branched sialylated glycans [92]. However, despite those structural variations among strains and subtypes, certain RBS-targeted bnAbs are able to neutralize virus strains from both human H1 and H3 subtypes [58, 69–72]. In addition, one pan-H3 bnAb F045–92 is able to neutralize all tested H3 strains isolated over five decades [58, 72]. These observations suggest that the neutralization activity of the RBS-targeted bnAbs can be robust to many structural variations within or proximal to the RBS.
Besides the small binding footprint that is preferred for bnAbs to specifically target the relatively small RBS [58], which thereby restricts the interaction to the most conserved region of this site, the neutralizing activity of RBS-targeted bnAbs is promoted by an avidity effect [69, 71, 76]. The bivalency of IgG allows RBS-targeted bnAbs to enhance neutralizing activity and to increase breadth against strains that interact weakly with its Fab (fragment antigen binding) only. This avidity effect relies on the high density of HAs on influenza virus [93, 94]. While the high density of receptor-binding proteins is not a universal feature for all viruses [95], it promotes high receptor-binding avidity during virus entry and is critical for influenza virus due to the extremely weak monovalent binding between sialylated glycan and HA (Kd in low mM range) [96]. As a consequence, this functional constraint allows RBS-targeted bnAbs to accommodate the changing landscape of the RBS and increase neutralization breadth by avidity.
One common obstacle that restricts the neutralization breadth of RBS-targeted bnAbs is the insertions and deletions (indels) near the RBS (Fig. 3c). The 133a insertion (between residues 133 and 134), which is common in H1 and H5 strains, is perhaps the most well-known example. This insertion produces a bulge in the 130-loop. Binding of RBS-targeted bnAbs CH65 [75], C05 [69], S139/1 [71], and F045–092 [58] are abolished by the 133a insertion. In addition to 133a insertion, many isolates from subtypes H4, H6, H7, H10, H14, and H15 have single (158a) or double (156a/158b) amino-acid insertions in the 150-loop that can negatively influence the binding of C05 [69], 139/1[71], and F045–092 [58]. Some H7 viruses also have an 8-residue deletion in the 220-loop [97, 98], which may decrease the contact surface and hence affinity of RBS-targeted bnAbs. Although it is much more difficult for the virus to acquire indels than point mutations, it is necessary for the development of an RBS-targeted universal vaccine or therapeutic to account for potential indels.
Functionally conserved region 2: Membrane fusion
The stem region is the other functionally conserved region on HA. As compared to the RBS, there is much less sequence variation in the stem region across strains and subtypes. In fact, the stem region contains the most conserved epitopes across HA for antibody recognition (Fig. 3a, d and e). As a result, stem-binding bnAbs can acquire higher neutralization breadth than RBS-targeted bnAbs [99–113]. These stem-binding bnAbs inhibit virus replication by preventing the pH-induced conformational changes that are essential for membrane fusion. Unlike the RBS, the stem region does not have a natural interacting partner. Nevertheless, similar to RBS-targeted bnAbs, a number of stem-binding bnAbs also share recurring motifs [114]. Due to the proximity to the viral membrane, stem-binding bnAbs have less conformational freedom for approach angles as compared to RBS-targeted bnAbs (Fig. 4a–b). They have to approach the stem perpendicularly or at an upward disposition as otherwise they would clash with the membrane. The difference between the approach angles of RBS-targeted bnAbs and stem-binding bnAbs can be quantified using a method that was previously employed to compare approach angles in HIV bnAbs [115] (Fig. 4c). The approach angle of RBS-targeted bnAbs has a range (maximum – minimum) of 37° in the horizontal plane and 60° in the vertical plane, whereas stem-binding bnAbs have a range of 29° in the horizontal plane and 39° in the vertical plane. This analysis supports the notion that the approach angle of stem-binding bnAbs.is more restricted due to proximity to the membrane.
Stem-binding bnAbs are often encoded by the VH1–69 germline gene, which is characterized by encoding hydrophobic residues at positions 53 (Ile) and 54 (Phe) in CDR H2, as well as an aromatic Tyr98 in CDR H3 [99–101, 114]. These three residues insert into the hydrophobic groove in the stem region and are critical for high affinity binding. In fact, the VH1–69 germline gene has been proposed as a critical “SOS component” of the antibody repertoire that allows rapid and robust response against influenza and other infections [116, 117]. However, several stem-binding bnAbs that are encoded by VH1–69 germline gene neutralize group 1 but not group 2 influenza subtypes [78, 99, 100, 108]. The problem of neutralizing group 2 influenza subtypes has been attributed to an N-glycosylation site at HA1 Asn38, which is immediately adjacent to the conserved epitope [99, 100] (Fig. 3d). This N-glycosylation site at Asn38 is conserved among group 2 HAs but is not present in group 1 HAs. Binding of these bnAbs to HA can be sterically hindered by the oligosaccharide at Asn38. In fact, two group 2-specific stem-binding bnAbs, namely CR8020 [107] and CR8043 [109], find a solution by recognizing an epitope lower down the stem, which may avoid a direct clash with the oligosaccharide at Asn38. Another stem-binding bnAb MEDI8852 binds to an epitope slightly higher than that of CR8020 and CR8043 and can neutralize both group 1 and 2 subtypes [105]. These bnAbs do not use VH1–69 germline gene. CR8020, CR8043, and MEDI8852 are derived from VH1–18, VH1–3, and VH6-1 germlines, respectively.
In comparison, the VH1–69 encoded stem-binding bnAbs analyzed to date are more group 1-specific. Nonetheless, a VH1–69 encoded stem-binding bnAb CR9114 has been identified that binds both group 1 and 2 influenza subtypes by interacting with a similar epitope as the group 1-specific VH1–69 encoded stem-binding bnAbs but accesses this site through reorientation of the group-2 specific glycan at HA1 Asn38 [101]. This binding feature is also observed in a VH3–30 encoded stem-binding cross-group bnAbs FI6v3 [111]. Overall, these observations suggest that Asn38 is a major obstacle for stem-binding bnAbs to overcome against influenza A group 2 and also influenza B viruses. At the same time, it demonstrates that N-glycosylation is critical not only for shielding the HA1 globular head domain, but also for interfering with recognition of the HA surface by stem-binding bnAbs.
While the shielding effect from oligosaccharides in the stem region can be overcome by some stem-binding bnAbs, HA mutants that are able to escape from stem-binding bnAbs have been identified by extensive passaging, although they are much fewer than for head binding antibodies [103, 106–109, 118] (Fig. 3e). For example, passaging an H3N2 virus in the presence of 39.29, a stem-binding bnAb that can neutralize both group 1 and 2 influenza viruses [113], has led to identification of three escape mutants [118]. One mutant completely abolished binding of antibody 39.29 to the HA stem, whereas the other two mutants escape by increasing fusion efficiency [118]. Other examples include escape mutants against stem-binding bnAbs C179 [103], CR8020 [107, 119], CR6261 [108], and CR8043 [109]. Although some escape mutants against stem-binding bnAbs have been shown to reduce viral replication fitness [106, 118], compensatory mutations may exist. Although stem-binding bnAbs have provided valuable insights into vaccine design [120–122] and computational design of antiviral proteins [123, 124], we should always be prepared for the possibility of emerging escape mutants in circulating influenza viruses.
Viral replication fitness effect of thousands of influenza virus mutants can be measured in parallel using deep mutational scanning [29, 30, 125]. A proof-of-concept study has shown that deep mutational scanning can be applied to rapidly identify antibody escape mutants [126]. This technique will be useful in mapping bnAb escape mutants, which will facilitate a better mechanistic understanding of potential escape strategy, if any. Recently, we demonstrated that many single amino-acid substitutions in the RBS alone impose a detrimental effect on viral replication fitness, but are neutral when combined together [127]. This phenomenon is known as epistasis. Interestingly, a number of the combinatorial mutants can escape RBS-targeted bnAb S139/1 [71, 127]. Whether such epistatic effects can be found in the stem region and whether it will promote stem-binding bnAb escape remain to be explored.
Other conserved antibody epitopes
Isolation and characterization of broadly neutralizing or cross-reactive antibodies have facilitated the discovery of other conserved region as antibody epitopes. H5M9 [128] and CR8071 [101] are bnAbs that can neutralize diverse H5N1 strains and influenza B strains, respectively. H5M9 is able to block both receptor binding and membrane fusion steps [128], whereas CR8071 inhibits the viral budding process [101]. Interestingly, they both bind to the vestigial esterase subdomain of HA1 that is conserved within a given subtype or in type B [101, 128, 129], but not across all subtypes (Fig. 3a and Fig. 4d). A fully functional esterase domain is present in the influenza C virus haemagglutinin-esterase-fusion glycoprotein (HEF) [130–132], which also contains the RBS and membrane fusion machinery. The esterase domain in influenza C virus HEF is responsible for cleaving the host receptor to facilitate viral budding [133], which is analogous to the function of NA in influenza A and B viruses. When influenza A and B viruses diverged from influenza C viruses, which is estimated to be around 4,000 years ago [21], a separate receptor-destroying enzyme, the neuraminidase (NA) emerged and the esterase subdomain became obsolete.
Notwithstanding, while the evolutionary constraints associated with epitopes of RBS-targeted bnAbs and stem-binding bnAbs are intuitive, they are not as clear for the HA vestigial esterase subdomain in influenza A and B viruses. Similarly, sera before and after immunization with a trivalent seasonal influenza vaccine in young adults were analyzed and a large fraction provided in vivo protection against H1N1 and H3N2 viruses by binding to another conserved epitope in the head domain but without any in vitro neutralizing activity [134]. The in vivo protection effect for these types of antibodies are likely to rely on the effector functions of the Fc domain, such as antibody-dependent cell-mediated cytotoxicity (ADCC), as for HA anti-stem antibodies [101, 111, 119, 120, 135–137]. The evolutionary constraints of these types of epitopes require further investigation and will be important for evaluating the genetic barrier for the emergence of escape mutants.
Protective immunity against zoonotic influenza viruses
Pandemic threats from highly pathogenic zoonotic influenza viruses have been a global concern. In recent years, avian influenza virus H5N1 and H7N9 subtypes have caused hundreds of human infections with a mortality rate of 20% to 60% [9]. Studies have demonstrated that “original antigenic sin” [138] is a key determinant for the susceptibility of zoonotic influenza viruses [138–140]. “Original antigenic sin” arises when our immune system employs immunological memory based on an earlier infection by a virus with an slightly different antigenicity, which then skews the current immune response towards antibodies that were previously produced and to epitopes recognized during previous infections [138]. During 1918 Spanish flu H1N1 pandemic, people aged between 15 and 35 had an atypically high fatality rate [141, 142]. Based on phylogenetic, seroarcheological, and epidemiological evidence, this atypically high fatality rate was proposed to be associated with childhood exposure of H3N8 virus, which was antigenically distinct from Spanish flu [139, 143, 144]. On the other hand, it is suggested that those that were born before or after this age group were exposed to H1 or H1-like influenza viruses during childhood [139]. These studies implied higher protection against strains that are antigenically similar to those that were encountered during childhood.
In fact, a serological study on seasonal H3N2 viruses has indeed shown that individuals produce high antibody titers towards strains that were encountered during childhood and that the antibody titer was less against strains that subsequently emerged [145]. Based on statistical modeling, such childhood imprinting is also important for determining the susceptibility against emerging avian influenza viruses H5N1 and H7N9 subtypes [140]. Briefly, those who were infected with seasonal H1 or H2 subtype (group 1) during their first encounter of influenza virus are less susceptible to H5 viruses (group 1), whereas those who were infected with seasonal H3 subtype (group 2) during their first encounter of influenza virus are less susceptible to H7 viruses (group 2) [140]. Overall, these observations highlight the importance of “original antigenic sin” in protection against zoonotic influenza viruses. They also reaffirm that seasonal influenza virus infection or vaccination can elicit heterosubtypic antibodies against antigenically similar zoonotic influenza viruses [108, 146–149].
Nonetheless, heterosubtypic antibodies are only infrequently elicited by seasonal influenza vaccination [147–150]. Even if they are elicited, such immunity may not be sustainable due to “original antigenic sin”. For example, while HA stem-binding bnAbs were commonly elicited during the 2009 pandemic H1N1 influenza season [151], this response was not sustained in subsequent years [152, 153]. Given the significance of “original antigenic sin”, sustainable protection against zoonotic influenza virus infection likely requires the induction of heterosubtypic antibody responses during childhood. Furthermore, as most of the epitopes targeted to influenza virus during natural infection or vaccination are against the highly variable HA1 head, heterosubtypic response may be more readily triggered by focusing on the highly conserved HA stem region [154–158]. Over the past few years, several immunogens have been designed based on the conserved HA stem region [120–122, 157, 159–162]. All of these immunogens are able to consistently elicit heterosubtypic antibody responses [120–122, 157, 159–162], which then provide a framework for making progress towards a universal influenza vaccine.
Emerging role for neuraminidase in the humoral immune response
While both HA and NA are targets for the humoral immune response, the antigenic properties of the NA are much less well characterized as compared to the HA. The number of NAs is around 5- to 10-fold less than HAs on the viral surface [163, 164]. However, NA is required for completing the viral replication cycle by cleaving host receptor during viral budding and, hence, is a key target for antivirals. Although somewhat slower than HA, the adaptation rate of NA is also very high [19, 20, 165]. As observed in HA, NA evolution can also result in antigenic drift [166]. Over the past 30 years, several epitopes on NA have been described based on structural characterization [167–172] and mutagenesis studies [173–176]. Some anti-N1 antibodies are able to provide cross-reactivity against both human H1N1 and avian H5N1 viruses [175, 177], or against both seasonal H1N1 and A(H1N1)pdm09 viruses [178]. Furthermore, one antibody that targets a highly conserved region on NA can protect against influenza viruses from N1-N9 subtypes [176]. Emerging evidence suggests that serum titer of anti-NA antibodies also correlates with protection against influenza infection and can be an independent predictor for disease outcome [179–181]. Yet, the role of NA as a vaccine immunogen remains to be explored [182].
There is a tight interplay between HA receptor-binding function and NA receptor-destroying activity. Experimental studies have shown that a functional balance between HA and NA is required for efficient viral replication [183–186]. When the functional activities of HA and NA are not in balance, mutations often rapidly arise, either in HA or NA or both, to restore the optimal functional balance [185–188]. Furthermore, certain mutations in the HA can compensate against the fitness cost of an oseltamivir-resistant mutation on NA [189]. Given that mutations that cause immune evasion can impact the protein functional activity (as seen in HA), antigenic drift in either HA or NA may also drive mutations in the other protein. However, further studies are needed to comprehend more on how the functional balance between HA and NA influences antigenic drift.
Concluding Remarks
It has been almost four decades since the crystal structure of influenza virus hemagglutinin (HA), which is the major antigen of influenza virus, was determined [34] that allowed an understanding of the effects of natural variation and structural identification of the major antigenic sites [42]. The high evolutionary capacity allows influenza to constantly escape natural immunity. However, functional constraints on receptor binding and membrane fusion that are required for viral entry result in sequence conservation of the receptor-binding site and the stem region. Recent identification and characterization of human influenza broadly neutralizing antibodies (bnAbs) have provided important insights into the development of antivirals and vaccines against these functional regions. Identification of bnAbs against the vestigial esterase subdomain and neuraminidase (NA) can further expand the anti-influenza arsenal. As the knowledge from evolutionary biology, immunology, structural biology, and virology of influenza virus continues to accumulate, we are hopefully moving closer towards better control of influenza with a universal vaccine that confers long-term immunity.
Highlights.
Antigenic variation is a major challenge for influenza vaccine design
Comprehending evolutionary constraints for influenza function is critical for vaccine development
Broadly neutralizing antibodies reveal conserved epitopes
Eliciting long-term heterosubtypic immunity is the ultimate goal for vaccine design
Acknowledgments
We acknowledge NIH R56 AI117675 for support. N.C.W. was supported by the Croucher Foundation Fellowship.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Klepser ME. Socioeconomic impact of seasonal (epidemic) influenza and the role of over-the-counter medicines. Drugs. 2014;74:1467–79. doi: 10.1007/s40265-014-0245-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hause BM, Ducatez M, Collin EA, Ran Z, Liu R, Sheng Z, et al. Isolation of a novel swine influenza virus from Oklahoma in 2011 which is distantly related to human influenza C viruses. PLoS Pathog. 2013;9:e1003176. doi: 10.1371/journal.ppat.1003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tong S, Zhu X, Li Y, Shi M, Zhang J, Bourgeois M, et al. New world bats harbor diverse influenza A viruses. PLoS Pathog. 2013;9:e1003657. doi: 10.1371/journal.ppat.1003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hashem AM. Prospects of HA-based universal influenza vaccine. Biomed Res Int. 2015;2015:414637. doi: 10.1155/2015/414637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parrish CR, Murcia PR, Holmes EC. Influenza virus reservoirs and intermediate hosts: dogs, horses, and new possibilities for influenza virus exposure of humans. J Virol. 2015;89:2990–4. doi: 10.1128/JVI.03146-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. Evolution and ecology of influenza A viruses. Microbiol Rev. 1992;56:152–79. doi: 10.1128/mr.56.1.152-179.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tong S, Li Y, Rivailler P, Conrardy C, Castillo DA, Chen LM, et al. A distinct lineage of influenza A virus from bats. Proc Natl Acad Sci U S A. 2012;109:4269–74. doi: 10.1073/pnas.1116200109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peiris JS, de Jong MD, Guan Y. Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev. 2007;20:243–67. doi: 10.1128/CMR.00037-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poovorawan Y, Pyungporn S, Prachayangprecha S, Makkoch J. Global alert to avian influenza virus infection: from H5N1 to H7N9. Pathog Glob Health. 2013;107:217–23. doi: 10.1179/2047773213Y.0000000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patterson KD, Pyle GF. The geography and mortality of the 1918 influenza pandemic. Bull Hist Med. 1991;65:4–21. [PubMed] [Google Scholar]
- 11.Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76:105–15. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease C, Prevention. Estimates of deaths associated with seasonal influenza --- United States, 1976–2007. MMWR Morb Mortal Wkly Rep. 2010;59:1057–62. [PubMed] [Google Scholar]
- 13.Johnson BF, Wilson LE, Ellis J, Elliot AJ, Barclay WS, Pebody RG, et al. Fatal cases of influenza a in childhood. PLoS One. 2009;4:e7671. doi: 10.1371/journal.pone.0007671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nobusawa E, Sato K. Comparison of the mutation rates of human influenza A and B viruses. J Virol. 2006;80:3675–8. doi: 10.1128/JVI.80.7.3675-3678.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamashita M, Krystal M, Fitch WM, Palese P. Influenza B virus evolution: co-circulating lineages and comparison of evolutionary pattern with those of influenza A and C viruses. Virology. 1988;163:112–22. doi: 10.1016/0042-6822(88)90238-3. [DOI] [PubMed] [Google Scholar]
- 16.van de Sandt CE, Bodewes R, Rimmelzwaan GF, de Vries RD. Influenza B viruses: not to be discounted. Future Microbiol. 2015;10:1447–65. doi: 10.2217/fmb.15.65. [DOI] [PubMed] [Google Scholar]
- 17.Tisa V, Barberis I, Faccio V, Paganino C, Trucchi C, Martini M, et al. Quadrivalent influenza vaccine: a new opportunity to reduce the influenza burden. J Prev Med Hyg. 2016;57:E28–33. [PMC free article] [PubMed] [Google Scholar]
- 18.Moa AM, Chughtai AA, Muscatello DJ, Turner RM, MacIntyre CR. Immunogenicity and safety of inactivated quadrivalent influenza vaccine in adults: A systematic review and meta-analysis of randomised controlled trials. Vaccine. 2016;34:4092–102. doi: 10.1016/j.vaccine.2016.06.064. [DOI] [PubMed] [Google Scholar]
- 19.Bhatt S, Holmes EC, Pybus OG. The genomic rate of molecular adaptation of the human influenza A virus. Mol Biol Evol. 2011;28:2443–51. doi: 10.1093/molbev/msr044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kilbourne ED, Johansson BE, Grajower B. Independent and disparate evolution in nature of influenza A virus hemagglutinin and neuraminidase glycoproteins. Proc Natl Acad Sci U S A. 1990;87:786–90. doi: 10.1073/pnas.87.2.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki Y, Nei M. Origin and evolution of influenza virus hemagglutinin genes. Mol Biol Evol. 2002;19:501–9. doi: 10.1093/oxfordjournals.molbev.a004105. [DOI] [PubMed] [Google Scholar]
- 22.Nobusawa E, Aoyama T, Kato H, Suzuki Y, Tateno Y, Nakajima K. Comparison of complete amino acid sequences and receptor-binding properties among 13 serotypes of hemagglutinins of influenza A viruses. Virology. 1991;182:475–85. doi: 10.1016/0042-6822(91)90588-3. [DOI] [PubMed] [Google Scholar]
- 23.Taubenberger JK. Influenza virus hemagglutinin cleavage into HA1, HA2: no laughing matter. Proc Natl Acad Sci U S A. 1998;95:9713–5. doi: 10.1073/pnas.95.17.9713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaipan C, Kobasa D, Bertram S, Glowacka I, Steffen I, Tsegaye TS, et al. Proteolytic activation of the 1918 influenza virus hemagglutinin. J Virol. 2009;83:3200–11. doi: 10.1128/JVI.02205-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bottcher E, Matrosovich T, Beyerle M, Klenk HD, Garten W, Matrosovich M. Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. J Virol. 2006;80:9896–8. doi: 10.1128/JVI.01118-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steiner DF, Smeekens SP, Ohagi S, Chan SJ. The new enzymology of precursor processing endoproteases. J Biol Chem. 1992;267:23435–8. [PubMed] [Google Scholar]
- 27.Stieneke-Grober A, Vey M, Angliker H, Shaw E, Thomas G, Roberts C, et al. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 1992;11:2407–14. doi: 10.1002/j.1460-2075.1992.tb05305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawaoka Y, Webster RG. Sequence requirements for cleavage activation of influenza virus hemagglutinin expressed in mammalian cells. Proc Natl Acad Sci U S A. 1988;85:324–8. doi: 10.1073/pnas.85.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thyagarajan B, Bloom JD. The inherent mutational tolerance and antigenic evolvability of influenza hemagglutinin. eLife. 2014;3:e03300. doi: 10.7554/eLife.03300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu NC, Young AP, Al-Mawsawi LQ, Olson CA, Feng J, Qi H, et al. High-throughput profiling of influenza A virus hemagglutinin gene at single-nucleotide resolution. Sci Rep. 2014;4:4942. doi: 10.1038/srep04942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skehel JJ, Bayley PM, Brown EB, Martin SR, Waterfield MD, White JM, et al. Changes in the conformation of influenza virus hemagglutinin at the pH optimum of virus-mediated membrane fusion. Proc Natl Acad Sci U S A. 1982;79:968–72. doi: 10.1073/pnas.79.4.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Earp LJ, Delos SE, Park HE, White JM. The many mechanisms of viral membrane fusion proteins. Curr Top Microbiol Immunol. 2005;285:25–66. doi: 10.1007/3-540-26764-6_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–69. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 34.Wilson IA, Skehel JJ, Wiley DC. Structure of the haemagglutinin membrane glycoprotein of influenza virus at 3 Å resolution. Nature. 1981;289:366–73. doi: 10.1038/289366a0. [DOI] [PubMed] [Google Scholar]
- 35.Bullough PA, Hughson FM, Skehel JJ, Wiley DC. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature. 1994;371:37–43. doi: 10.1038/371037a0. [DOI] [PubMed] [Google Scholar]
- 36.Kilbourne ED. Influenza pandemics of the 20th century. Emerg Infect Dis. 2006;12:9–14. doi: 10.3201/eid1201.051254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zimmer SM, Burke DS. Historical perspective--Emergence of influenza A (H1N1) viruses. N Engl J Med. 2009;361:279–85. doi: 10.1056/NEJMra0904322. [DOI] [PubMed] [Google Scholar]
- 38.Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fisman DN, Savage R, Gubbay J, Achonu C, Akwar H, Farrell DJ, et al. Older age and a reduced likelihood of 2009 H1N1 virus infection. N Engl J Med. 2009;361:2000–1. doi: 10.1056/NEJMc0907256. [DOI] [PubMed] [Google Scholar]
- 40.Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype) Cell. 1982;31:417–27. doi: 10.1016/0092-8674(82)90135-0. [DOI] [PubMed] [Google Scholar]
- 41.Gerhard W, Yewdell J, Frankel ME, Webster R. Antigenic structure of influenza virus haemagglutinin defined by hybridoma antibodies. Nature. 1981;290:713–7. doi: 10.1038/290713a0. [DOI] [PubMed] [Google Scholar]
- 42.Wiley DC, Wilson IA, Skehel JJ. Structural identification of the antibody-binding sites of Hong Kong influenza haemagglutinin and their involvement in antigenic variation. Nature. 1981;289:373–8. doi: 10.1038/289373a0. [DOI] [PubMed] [Google Scholar]
- 43.Skehel JJ, Stevens DJ, Daniels RS, Douglas AR, Knossow M, Wilson IA, et al. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc Natl Acad Sci U S A. 1984;81:1779–83. doi: 10.1073/pnas.81.6.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wiley DC, Skehel JJ. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu Rev Biochem. 1987;56:365–94. doi: 10.1146/annurev.bi.56.070187.002053. [DOI] [PubMed] [Google Scholar]
- 45.Bush RM, Bender CA, Subbarao K, Cox NJ, Fitch WM. Predicting the evolution of human influenza A. Science. 1999;286:1921–5. doi: 10.1126/science.286.5446.1921. [DOI] [PubMed] [Google Scholar]
- 46.Wang X, Ilyushina NA, Lugovtsev VY, Bovin NV, Couzens LK, Gao J, et al. Amino acids in hemagglutinin antigenic site B determine antigenic and receptor binding differences between A(H3N2)v and ancestral seasonal H3N2 influenza viruses. J Virol. 2017:91. doi: 10.1128/JVI.01512-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Popova L, Smith K, West AH, Wilson PC, James JA, Thompson LF, et al. Immunodominance of antigenic site B over site A of hemagglutinin of recent H3N2 influenza viruses. PLoS One. 2012;7:e41895. doi: 10.1371/journal.pone.0041895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koel BF, Burke DF, Bestebroer TM, van der Vliet S, Zondag GC, Vervaet G, et al. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science. 2013;342:976–9. doi: 10.1126/science.1244730. [DOI] [PubMed] [Google Scholar]
- 49.Guarnaccia T, Carolan LA, Maurer-Stroh S, Lee RT, Job E, Reading PC, et al. Antigenic drift of the pandemic 2009 A(H1N1) influenza virus in A ferret model. PLoS Pathog. 2013;9:e1003354. doi: 10.1371/journal.ppat.1003354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li C, Hatta M, Burke DF, Ping J, Zhang Y, Ozawa M, et al. Selection of antigenically advanced variants of seasonal influenza viruses. Nat Microbiol. 2016;1:16058. doi: 10.1038/nmicrobiol.2016.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun S, Wang Q, Zhao F, Chen W, Li Z. Glycosylation site alteration in the evolution of influenza A (H1N1) viruses. PLoS One. 2011;6:e22844. doi: 10.1371/journal.pone.0022844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blackburne BP, Hay AJ, Goldstein RA. Changing selective pressure during antigenic changes in human influenza H3. PLoS Pathog. 2008;4:e1000058. doi: 10.1371/journal.ppat.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cherry JL, Lipman DJ, Nikolskaya A, Wolf YI. Evolutionary dynamics of N-glycosylation sites of influenza virus hemagglutinin. PLoS Curr. 2009;1:RRN1001. doi: 10.1371/currents.RRN1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tate MD, Job ER, Deng YM, Gunalan V, Maurer-Stroh S, Reading PC. Playing hide and seek: how glycosylation of the influenza virus hemagglutinin can modulate the immune response to infection. Viruses. 2014;6:1294–316. doi: 10.3390/v6031294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Das SR, Puigbo P, Hensley SE, Hurt DE, Bennink JR, Yewdell JW. Glycosylation focuses sequence variation in the influenza A virus H1 hemagglutinin globular domain. PLoS Pathog. 2010;6:e1001211. doi: 10.1371/journal.ppat.1001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang M, Gaschen B, Blay W, Foley B, Haigwood N, Kuiken C, et al. Tracking global patterns of N-linked glycosylation site variation in highly variable viral glycoproteins: HIV, SIV, and HCV envelopes and influenza hemagglutinin. Glycobiology. 2004;14:1229–46. doi: 10.1093/glycob/cwh106. [DOI] [PubMed] [Google Scholar]
- 57.Igarashi M, Ito K, Kida H, Takada A. Genetically destined potentials for N-linked glycosylation of influenza virus hemagglutinin. Virology. 2008;376:323–9. doi: 10.1016/j.virol.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 58.Lee PS, Ohshima N, Stanfield RL, Yu W, Iba Y, Okuno Y, et al. Receptor mimicry by antibody F045-092 facilitates universal binding to the H3 subtype of influenza virus. Nat Commun. 2014;5:3614. doi: 10.1038/ncomms4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abe Y, Takashita E, Sugawara K, Matsuzaki Y, Muraki Y, Hongo S. Effect of the addition of oligosaccharides on the biological activities and antigenicity of influenza A/H3N2 virus hemagglutinin. J Virol. 2004;78:9605–11. doi: 10.1128/JVI.78.18.9605-9611.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schulze IT. Effects of glycosylation on the properties and functions of influenza virus hemagglutinin. J Infect Dis. 1997;176(Suppl 1):S24–8. doi: 10.1086/514170. [DOI] [PubMed] [Google Scholar]
- 61.Medina RA, Stertz S, Manicassamy B, Zimmermann P, Sun X, Albrecht RA, et al. Glycosylations in the globular head of the hemagglutinin protein modulate the virulence and antigenic properties of the H1N1 influenza viruses. Sci Transl Med. 2013;5:187ra70. doi: 10.1126/scitranslmed.3005996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Job ER, Deng YM, Barfod KK, Tate MD, Caldwell N, Reddiex S, et al. Addition of glycosylation to influenza A virus hemagglutinin modulates antibody-mediated recognition of H1N1 2009 pandemic viruses. J Immunol. 2013;190:2169–77. doi: 10.4049/jimmunol.1202433. [DOI] [PubMed] [Google Scholar]
- 63.Tsuchiya E, Sugawara K, Hongo S, Matsuzaki Y, Muraki Y, Li ZN, et al. Effect of addition of new oligosaccharide chains to the globular head of influenza A/H2N2 virus haemagglutinin on the intracellular transport and biological activities of the molecule. J Gen Virol. 2002;83:1137–46. doi: 10.1099/0022-1317-83-5-1137. [DOI] [PubMed] [Google Scholar]
- 64.Tsuchiya E, Sugawara K, Hongo S, Matsuzaki Y, Muraki Y, Li ZN, et al. Antigenic structure of the haemagglutinin of human influenza A/H2N2 virus. J Gen Virol. 2001;82:2475–84. doi: 10.1099/0022-1317-82-10-2475. [DOI] [PubMed] [Google Scholar]
- 65.Das SR, Hensley SE, David A, Schmidt L, Gibbs JS, Puigbo P, et al. Fitness costs limit influenza A virus hemagglutinin glycosylation as an immune evasion strategy. Proc Natl Acad Sci U S A. 2011;108:E1417–22. doi: 10.1073/pnas.1108754108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim JI, Lee I, Park S, Hwang MW, Bae JY, Lee S, et al. Genetic requirement for hemagglutinin glycosylation and its implications for influenza A H1N1 virus evolution. J Virol. 2013;87:7539–49. doi: 10.1128/JVI.00373-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alymova IV, York IA, Air GM, Cipollo JF, Gulati S, Baranovich T, et al. Glycosylation changes in the globular head of H3N2 influenza hemagglutinin modulate receptor binding without affecting virus virulence. Sci Rep. 2016;6:36216. doi: 10.1038/srep36216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chambers BS, Parkhouse K, Ross TM, Alby K, Hensley SE. Identification of hemagglutinin residues responsible for H3N2 antigenic drift during the 2014–2015 influenza season. Cell Rep. 2015;12:1–6. doi: 10.1016/j.celrep.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ekiert DC, Kashyap AK, Steel J, Rubrum A, Bhabha G, Khayat R, et al. Cross-neutralization of influenza A viruses mediated by a single antibody loop. Nature. 2012;489:526–32. doi: 10.1038/nature11414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yoshida R, Igarashi M, Ozaki H, Kishida N, Tomabechi D, Kida H, et al. Cross-protective potential of a novel monoclonal antibody directed against antigenic site B of the hemagglutinin of influenza A viruses. PLoS Pathog. 2009;5:e1000350. doi: 10.1371/journal.ppat.1000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee PS, Yoshida R, Ekiert DC, Sakai N, Suzuki Y, Takada A, et al. Heterosubtypic antibody recognition of the influenza virus hemagglutinin receptor binding site enhanced by avidity. Proc Natl Acad Sci U S A. 2012;109:17040–5. doi: 10.1073/pnas.1212371109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ohshima N, Iba Y, Kubota-Koketsu R, Asano Y, Okuno Y, Kurosawa Y. Naturally occurring antibodies in humans can neutralize a variety of influenza virus strains, including H3, H1, H2, and H5. J Virol. 2011;85:11048–57. doi: 10.1128/JVI.05397-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krause JC, Tsibane T, Tumpey TM, Huffman CJ, Albrecht R, Blum DL, et al. Human monoclonal antibodies to pandemic 1957 H2N2 and pandemic 1968 H3N2 influenza viruses. J Virol. 2012;86:6334–40. doi: 10.1128/JVI.07158-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xu R, Krause JC, McBride R, Paulson JC, Crowe JE, Jr, Wilson IA. A recurring motif for antibody recognition of the receptor-binding site of influenza hemagglutinin. Nat Struct Mol Biol. 2013;20:363–70. doi: 10.1038/nsmb.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Whittle JR, Zhang R, Khurana S, King LR, Manischewitz J, Golding H, et al. Broadly neutralizing human antibody that recognizes the receptor-binding pocket of influenza virus hemagglutinin. Proc Natl Acad Sci U S A. 2011;108:14216–21. doi: 10.1073/pnas.1111497108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hong M, Lee PS, Hoffman RM, Zhu X, Krause JC, Laursen NS, et al. Antibody recognition of the pandemic H1N1 Influenza virus hemagglutinin receptor binding site. J Virol. 2013;87:12471–80. doi: 10.1128/JVI.01388-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Krause JC, Tsibane T, Tumpey TM, Huffman CJ, Basler CF, Crowe JE., Jr A broadly neutralizing human monoclonal antibody that recognizes a conserved, novel epitope on the globular head of the influenza H1N1 virus hemagglutinin. J Virol. 2011;85:10905–8. doi: 10.1128/JVI.00700-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee PS, Wilson IA. Structural characterization of viral epitopes recognized by broadly cross-reactive antibodies. Curr Top Microbiol Immunol. 2015;386:323–41. doi: 10.1007/82_2014_413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Barbey-Martin C, Gigant B, Bizebard T, Calder LJ, Wharton SA, Skehel JJ, et al. An antibody that prevents the hemagglutinin low pH fusogenic transition. Virology. 2002;294:70–4. doi: 10.1006/viro.2001.1320. [DOI] [PubMed] [Google Scholar]
- 80.Schmidt AG, Xu H, Khan AR, O’Donnell T, Khurana S, King LR, et al. Preconfiguration of the antigen-binding site during affinity maturation of a broadly neutralizing influenza virus antibody. Proc Natl Acad Sci U S A. 2013;110:264–9. doi: 10.1073/pnas.1218256109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fleury D, Wharton SA, Skehel JJ, Knossow M, Bizebard T. Antigen distortion allows influenza virus to escape neutralization. Nat Struct Biol. 1998;5:119–23. doi: 10.1038/nsb0298-119. [DOI] [PubMed] [Google Scholar]
- 82.Schmidt AG, Therkelsen MD, Stewart S, Kepler TB, Liao HX, Moody MA, et al. Viral receptor-binding site antibodies with diverse germline origins. Cell. 2015;161:1026–34. doi: 10.1016/j.cell.2015.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gamblin SJ, Haire LF, Russell RJ, Stevens DJ, Xiao B, Ha Y, et al. The structure and receptor binding properties of the 1918 influenza hemagglutinin. Science. 2004;303:1838–42. doi: 10.1126/science.1093155. [DOI] [PubMed] [Google Scholar]
- 84.Xu R, McBride R, Nycholat CM, Paulson JC, Wilson IA. Structural characterization of the hemagglutinin receptor specificity from the 2009 H1N1 influenza pandemic. J Virol. 2012;86:982–90. doi: 10.1128/JVI.06322-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lin YP, Xiong X, Wharton SA, Martin SR, Coombs PJ, Vachieri SG, et al. Evolution of the receptor binding properties of the influenza A(H3N2) hemagglutinin. Proc Natl Acad Sci U S A. 2012;109:21474–9. doi: 10.1073/pnas.1218841110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Connor RJ, Kawaoka Y, Webster RG, Paulson JC. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology. 1994;205:17–23. doi: 10.1006/viro.1994.1615. [DOI] [PubMed] [Google Scholar]
- 87.Glaser L, Stevens J, Zamarin D, Wilson IA, Garcia-Sastre A, Tumpey TM, et al. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol. 2005;79:11533–6. doi: 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, et al. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol. 2006;355:1143–55. doi: 10.1016/j.jmb.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 89.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–9. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 90.Matrosovich MN, Gambaryan AS, Teneberg S, Piskarev VE, Yamnikova SS, Lvov DK, et al. Avian influenza A viruses differ from human viruses by recognition of sialyloligosaccharides and gangliosides and by a higher conservation of the HA receptor-binding site. Virology. 1997;233:224–34. doi: 10.1006/viro.1997.8580. [DOI] [PubMed] [Google Scholar]
- 91.Rogers GN, Paulson JC, Daniels RS, Skehel JJ, Wilson IA, Wiley DC. Single amino acid substitutions in influenza haemagglutinin change receptor binding specificity. Nature. 1983;304:76–8. doi: 10.1038/304076a0. [DOI] [PubMed] [Google Scholar]
- 92.Peng W, de Vries RP, Grant OC, Thompson AJ, McBride R, Tsogtbaatar B, et al. Recent H3N2 viruses have evolved specificity for extended, branched human-type receptors, conferring potential for Increased avidity. Cell Host Microbe. 2017;21:1–12. doi: 10.1016/j.chom.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Moules V, Terrier O, Yver M, Riteau B, Moriscot C, Ferraris O, et al. Importance of viral genomic composition in modulating glycoprotein content on the surface of influenza virus particles. Virology. 2011;414:51–62. doi: 10.1016/j.virol.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 94.Wasilewski S, Calder LJ, Grant T, Rosenthal PB. Distribution of surface glycoproteins on influenza A virus determined by electron cryotomography. Vaccine. 2012;30:7368–73. doi: 10.1016/j.vaccine.2012.09.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Klein JS, Bjorkman PJ. Few and far between: how HIV may be evading antibody avidity. PLoS Pathog. 2010;6:e1000908. doi: 10.1371/journal.ppat.1000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sauter NK, Bednarski MD, Wurzburg BA, Hanson JE, Whitesides GM, Skehel JJ, et al. Hemagglutinins from two influenza virus variants bind to sialic acid derivatives with millimolar dissociation constants: a 500-MHz proton nuclear magnetic resonance study. Biochemistry. 1989;28:8388–96. doi: 10.1021/bi00447a018. [DOI] [PubMed] [Google Scholar]
- 97.Yang H, Chen LM, Carney PJ, Donis RO, Stevens J. Structures of receptor complexes of a North American H7N2 influenza hemagglutinin with a loop deletion in the receptor binding site. PLoS Pathog. 2010;6:e1001081. doi: 10.1371/journal.ppat.1001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Suarez DL, Garcia M, Latimer J, Senne D, Perdue M. Phylogenetic analysis of H7 avian influenza viruses isolated from the live bird markets of the Northeast United States. J Virol. 1999;73:3567–73. doi: 10.1128/jvi.73.5.3567-3573.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ekiert DC, Bhabha G, Elsliger MA, Friesen RH, Jongeneelen M, Throsby M, et al. Antibody recognition of a highly conserved influenza virus epitope. Science. 2009;324:246–51. doi: 10.1126/science.1171491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sui J, Hwang WC, Perez S, Wei G, Aird D, Chen LM, et al. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat Struct Mol Biol. 2009;16:265–73. doi: 10.1038/nsmb.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dreyfus C, Laursen NS, Kwaks T, Zuijdgeest D, Khayat R, Ekiert DC, et al. Highly conserved protective epitopes on influenza B viruses. Science. 2012;337:1343–8. doi: 10.1126/science.1222908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dreyfus C, Ekiert DC, Wilson IA. Structure of a classical broadly neutralizing stem antibody in complex with a pandemic H2 influenza virus hemagglutinin. J Virol. 2013;87:7149–54. doi: 10.1128/JVI.02975-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Okuno Y, Isegawa Y, Sasao F, Ueda S. A common neutralizing epitope conserved between the hemagglutinins of influenza A virus H1 and H2 strains. J Virol. 1993;67:2552–8. doi: 10.1128/jvi.67.5.2552-2558.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kashyap AK, Steel J, Oner AF, Dillon MA, Swale RE, Wall KM, et al. Combinatorial antibody libraries from survivors of the Turkish H5N1 avian influenza outbreak reveal virus neutralization strategies. Proc Natl Acad Sci U S A. 2008;105:5986–91. doi: 10.1073/pnas.0801367105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kallewaard NL, Corti D, Collins PJ, Neu U, McAuliffe JM, Benjamin E, et al. Structure and function analysis of an antibody recognizing all influenza A subtypes. Cell. 2016;166:596–608. doi: 10.1016/j.cell.2016.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Henry Dunand CJ, Leon PE, Kaur K, Tan GS, Zheng NY, Andrews S, et al. Preexisting human antibodies neutralize recently emerged H7N9 influenza strains. J Clin Invest. 2015;125:1255–68. doi: 10.1172/JCI74374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ekiert DC, Friesen RH, Bhabha G, Kwaks T, Jongeneelen M, Yu W, et al. A highly conserved neutralizing epitope on group 2 influenza A viruses. Science. 2011;333:843–50. doi: 10.1126/science.1204839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Throsby M, van den Brink E, Jongeneelen M, Poon LL, Alard P, Cornelissen L, et al. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+ memory B cells. PLoS One. 2008;3:e3942. doi: 10.1371/journal.pone.0003942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Friesen RH, Lee PS, Stoop EJ, Hoffman RM, Ekiert DC, Bhabha G, et al. A common solution to group 2 influenza virus neutralization. Proc Natl Acad Sci U S A. 2014;111:445–50. doi: 10.1073/pnas.1319058110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wu Y, Cho M, Shore D, Song M, Choi J, Jiang T, et al. A potent broad-spectrum protective human monoclonal antibody crosslinking two haemagglutinin monomers of influenza A virus. Nat Commun. 2015;6:7708. doi: 10.1038/ncomms8708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Corti D, Voss J, Gamblin SJ, Codoni G, Macagno A, Jarrossay D, et al. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science. 2011;333:850–6. doi: 10.1126/science.1205669. [DOI] [PubMed] [Google Scholar]
- 112.Fu Y, Zhang Z, Sheehan J, Avnir Y, Ridenour C, Sachnik T, et al. A broadly neutralizing anti-influenza antibody reveals ongoing capacity of haemagglutinin-specific memory B cells to evolve. Nat Commun. 2016;7:12780. doi: 10.1038/ncomms12780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nakamura G, Chai N, Park S, Chiang N, Lin Z, Chiu H, et al. An in vivo human-plasmablast enrichment technique allows rapid identification of therapeutic influenza A antibodies. Cell Host Microbe. 2013;14:93–103. doi: 10.1016/j.chom.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 114.Avnir Y, Tallarico AS, Zhu Q, Bennett AS, Connelly G, Sheehan J, et al. Molecular signatures of hemagglutinin stem-directed heterosubtypic human neutralizing antibodies against influenza A viruses. PLoS Pathog. 2014;10:e1004103. doi: 10.1371/journal.ppat.1004103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhou T, Lynch RM, Chen L, Acharya P, Wu X, Doria-Rose NA, et al. Structural repertoire of HIV-1-neutralizing antibodies targeting the CD4 supersite in 14 donors. Cell. 2015;161:1280–92. doi: 10.1016/j.cell.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lerner RA. Rare antibodies from combinatorial libraries suggests an S.O.S. component of the human immunological repertoire. Mol Biosyst. 2011;7:1004–12. doi: 10.1039/c0mb00310g. [DOI] [PubMed] [Google Scholar]
- 117.Lerner RA. Combinatorial antibody libraries: new advances, new immunological insights. Nat Rev Immunol. 2016;16:498–508. doi: 10.1038/nri.2016.67. [DOI] [PubMed] [Google Scholar]
- 118.Chai N, Swem LR, Reichelt M, Chen-Harris H, Luis E, Park S, et al. Two escape mechanisms of influenza A virus to a broadly neutralizing stalk-binding antibody. PLoS Pathog. 2016;12:e1005702. doi: 10.1371/journal.ppat.1005702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tharakaraman K, Subramanian V, Cain D, Sasisekharan V, Sasisekharan R. Broadly neutralizing influenza hemagglutinin stem-specific antibody CR8020 targets residues that are prone to escape due to host selection pressure. Cell Host Microbe. 2014;15:644–51. doi: 10.1016/j.chom.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Impagliazzo A, Milder F, Kuipers H, Wagner MV, Zhu X, Hoffman RM, et al. A stable trimeric influenza hemagglutinin stem as a broadly protective immunogen. Science. 2015;349:1301–6. doi: 10.1126/science.aac7263. [DOI] [PubMed] [Google Scholar]
- 121.Yassine HM, Boyington JC, McTamney PM, Wei CJ, Kanekiyo M, Kong WP, et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat Med. 2015;21:1065–70. doi: 10.1038/nm.3927. [DOI] [PubMed] [Google Scholar]
- 122.Valkenburg SA, Mallajosyula VV, Li OT, Chin AW, Carnell G, Temperton N, et al. Stalking influenza by vaccination with pre-fusion headless HA mini-stem. Sci Rep. 2016;6:22666. doi: 10.1038/srep22666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fleishman SJ, Whitehead TA, Ekiert DC, Dreyfus C, Corn JE, Strauch EM, et al. Computational design of proteins targeting the conserved stem region of influenza hemagglutinin. Science. 2011;332:816–21. doi: 10.1126/science.1202617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Whitehead TA, Chevalier A, Song Y, Dreyfus C, Fleishman SJ, De Mattos C, et al. Optimization of affinity, specificity and function of designed influenza inhibitors using deep sequencing. Nat Biotechnol. 2012;30:543–8. doi: 10.1038/nbt.2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fowler DM, Fields S. Deep mutational scanning: a new style of protein science. Nat Methods. 2014;11:801–7. doi: 10.1038/nmeth.3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Doud MB, Hensley SE, Bloom JD. Complete mapping of viral escape from neutralizing antibodies. PLoS Pathog. 2017;13:e1006271. doi: 10.1371/journal.ppat.1006271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wu NC, Xie J, Zheng T, Nycholat CM, Grande G, Paulson JC, et al. Diversity of functionally permissive sequences in the receptor-binding site of influenza hemagglutinin. Cell Host Microbe. 2017;21:742–53. doi: 10.1016/j.chom.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhu X, Guo YH, Jiang T, Wang YD, Chan KH, Li XF, et al. A unique and conserved neutralization epitope in H5N1 influenza viruses identified by an antibody against the A/Goose/Guangdong/1/96 hemagglutinin. J Virol. 2013;87:12619–35. doi: 10.1128/JVI.01577-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ha Y, Stevens DJ, Skehel JJ, Wiley DC. H5 avian and H9 swine influenza virus haemagglutinin structures: possible origin of influenza subtypes. EMBO J. 2002;21:865–75. doi: 10.1093/emboj/21.5.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Herrler G, Durkop I, Becht H, Klenk HD. The glycoprotein of influenza C virus is the haemagglutinin, esterase and fusion factor. J Gen Virol. 1988;69(Pt 4):839–46. doi: 10.1099/0022-1317-69-4-839. [DOI] [PubMed] [Google Scholar]
- 131.Herrler G, Klenk HD. Structure and function of the HEF glycoprotein of influenza C virus. Adv Virus Res. 1991;40:213–34. doi: 10.1016/S0065-3527(08)60280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rosenthal PB, Zhang X, Formanowski F, Fitz W, Wong CH, Meier-Ewert H, et al. Structure of the haemagglutinin-esterase-fusion glycoprotein of influenza C virus. Nature. 1998;396:92–6. doi: 10.1038/23974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Herrler G, Rott R, Klenk HD, Muller HP, Shukla AK, Schauer R. The receptor-destroying enzyme of influenza C virus is neuraminate-O-acetylesterase. EMBO J. 1985;4:1503–6. doi: 10.1002/j.1460-2075.1985.tb03809.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lee J, Boutz DR, Chromikova V, Joyce MG, Vollmers C, Leung K, et al. Molecular-level analysis of the serum antibody repertoire in young adults before and after seasonal influenza vaccination. Nat Med. 2016;22:1456–64. doi: 10.1038/nm.4224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.DiLillo DJ, Tan GS, Palese P, Ravetch JV. Broadly neutralizing hemagglutinin stalk-specific antibodies require FcγR interactions for protection against influenza virus in vivo. Nat Med. 2014;20:143–51. doi: 10.1038/nm.3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mullarkey CE, Bailey MJ, Golubeva DA, Tan GS, Nachbagauer R, He W, et al. Broadly neutralizing hemagglutinin stalk-specific antibodies induce potent phagocytosis of immune complexes by neutrophils in an Fc-dependent manner. MBio. 2016:7. doi: 10.1128/mBio.01624-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cox F, Kwaks T, Brandenburg B, Koldijk MH, Klaren V, Smal B, et al. HA antibody-mediated FcγRIIIa activity is both dependent on FcR engagement and interactions between HA and sialic acids. Front Immunol. 2016;7:399. doi: 10.3389/fimmu.2016.00399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Francis T. On the doctrine of original antigenic sin. Proc Am Philos Soc. 1960;104:572–8. [Google Scholar]
- 139.Worobey M, Han GZ, Rambaut A. Genesis and pathogenesis of the 1918 pandemic H1N1 influenza A virus. Proc Natl Acad Sci U S A. 2014;111:8107–12. doi: 10.1073/pnas.1324197111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gostic KM, Ambrose M, Worobey M, Lloyd-Smith JO. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science. 2016;354:722–6. doi: 10.1126/science.aag1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Luk J, Gross P, Thompson WW. Observations on mortality during the 1918 influenza pandemic. Clin Infect Dis. 2001;33:1375–8. doi: 10.1086/322662. [DOI] [PubMed] [Google Scholar]
- 142.Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Shanks GD, Brundage JF. Pathogenic responses among young adults during the 1918 influenza pandemic. Emerg Infect Dis. 2012;18:201–7. doi: 10.3201/eid1802.102042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gagnon A, Miller MS, Hallman SA, Bourbeau R, Herring DA, Earn DJ, et al. Age-specific mortality during the 1918 influenza pandemic: unravelling the mystery of high young adult mortality. PLoS One. 2013;8:e69586. doi: 10.1371/journal.pone.0069586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lessler J, Riley S, Read JM, Wang S, Zhu H, Smith GJ, et al. Evidence for antigenic seniority in influenza A (H3N2) antibody responses in southern China. PLoS Pathog. 2012;8:e1002802. doi: 10.1371/journal.ppat.1002802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kohler I, Scherrer AU, Zagordi O, Bianchi M, Wyrzucki A, Steck M, et al. Prevalence and predictors for homo- and heterosubtypic antibodies against influenza a virus. Clin Infect Dis. 2014;59:1386–93. doi: 10.1093/cid/ciu660. [DOI] [PubMed] [Google Scholar]
- 147.Gioia C, Castilletti C, Tempestilli M, Piacentini P, Bordi L, Chiappini R, et al. Cross-subtype immunity against avian influenza in persons recently vaccinated for influenza. Emerg Infect Dis. 2008;14:121–8. doi: 10.3201/eid1401.061283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Corti D, Suguitan AL, Jr, Pinna D, Silacci C, Fernandez-Rodriguez BM, Vanzetta F, et al. Heterosubtypic neutralizing antibodies are produced by individuals immunized with a seasonal influenza vaccine. J Clin Invest. 2010;120:1663–73. doi: 10.1172/JCI41902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ding H, Tsai C, Zhou F, Buchy P, Deubel V, Zhou P. Heterosubtypic antibody response elicited with seasonal influenza vaccine correlates partial protection against highly pathogenic H5N1 virus. PLoS One. 2011;6:e17821. doi: 10.1371/journal.pone.0017821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tang JW, Ngai KL, Chan PK. Lack of cross-immune reactivity against influenza H5N1 from seasonal influenza vaccine in humans. J Med Virol. 2008;80:1992–6. doi: 10.1002/jmv.21321. [DOI] [PubMed] [Google Scholar]
- 151.Wrammert J, Koutsonanos D, Li GM, Edupuganti S, Sui J, Morrissey M, et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J Exp Med. 2011;208:181–93. doi: 10.1084/jem.20101352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Andrews SF, Huang Y, Kaur K, Popova LI, Ho IY, Pauli NT, et al. Immune history profoundly affects broadly protective B cell responses to influenza. Sci Transl Med. 2015;7:316ra192. doi: 10.1126/scitranslmed.aad0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hoa le NM, Mai le Q, Bryant JE, Thai PQ, Hang Nle K, Yen NT, et al. Association between hemagglutinin stem-reactive antibodies and influenza A/H1N1 virus infection during the 2009 pandemic. J Virol. 2016;90:6549–56. doi: 10.1128/JVI.00093-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Krammer F, Margine I, Hai R, Flood A, Hirsh A, Tsvetnitsky V, et al. H3 stalk-based chimeric hemagglutinin influenza virus constructs protect mice from H7N9 challenge. J Virol. 2014;88:2340–3. doi: 10.1128/JVI.03183-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Margine I, Krammer F, Hai R, Heaton NS, Tan GS, Andrews SA, et al. Hemagglutinin stalk-based universal vaccine constructs protect against group 2 influenza A viruses. J Virol. 2013;87:10435–46. doi: 10.1128/JVI.01715-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Krammer F, Hai R, Yondola M, Tan GS, Leyva-Grado VH, Ryder AB, et al. Assessment of influenza virus hemagglutinin stalk-based immunity in ferrets. J Virol. 2014;88:3432–42. doi: 10.1128/JVI.03004-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Steel J, Lowen AC, Wang TT, Yondola M, Gao Q, Haye K, et al. Influenza virus vaccine based on the conserved hemagglutinin stalk domain. MBio. 2010:1. doi: 10.1128/mBio.00018-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hai R, Krammer F, Tan GS, Pica N, Eggink D, Maamary J, et al. Influenza viruses expressing chimeric hemagglutinins: globular head and stalk domains derived from different subtypes. J Virol. 2012;86:5774–81. doi: 10.1128/JVI.00137-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wohlbold TJ, Nachbagauer R, Margine I, Tan GS, Hirsh A, Krammer F. Vaccination with soluble headless hemagglutinin protects mice from challenge with divergent influenza viruses. Vaccine. 2015;33:3314–21. doi: 10.1016/j.vaccine.2015.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mallajosyula VV, Citron M, Ferrara F, Lu X, Callahan C, Heidecker GJ, et al. Influenza hemagglutinin stem-fragment immunogen elicits broadly neutralizing antibodies and confers heterologous protection. Proc Natl Acad Sci U S A. 2014;111:E2514–23. doi: 10.1073/pnas.1402766111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mallajosyula VV, Citron M, Ferrara F, Temperton NJ, Liang X, Flynn JA, et al. Hemagglutinin sequence conservation guided stem immunogen design from influenza A H3 subtype. Front Immunol. 2015;6:329. doi: 10.3389/fimmu.2015.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bommakanti G, Lu X, Citron MP, Najar TA, Heidecker GJ, ter Meulen J, et al. Design of Escherichia coli-expressed stalk domain immunogens of H1N1 hemagglutinin that protect mice from lethal challenge. J Virol. 2012;86:13434–44. doi: 10.1128/JVI.01429-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Webster RG, Laver WG, Kilbourne ED. Reactions of antibodies with surface antigens of influenza virus. J Gen Virol. 1968;3:315–26. doi: 10.1099/0022-1317-3-3-315. [DOI] [PubMed] [Google Scholar]
- 164.Mitnaul LJ, Castrucci MR, Murti KG, Kawaoka Y. The cytoplasmic tail of influenza A virus neuraminidase (NA) affects NA incorporation into virions, virion morphology, and virulence in mice but is not essential for virus replication. J Virol. 1996;70:873–9. doi: 10.1128/jvi.70.2.873-879.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Westgeest KB, de Graaf M, Fourment M, Bestebroer TM, van Beek R, Spronken MI, et al. Genetic evolution of the neuraminidase of influenza A (H3N2) viruses from 1968 to 2009 and its correspondence to haemagglutinin evolution. J Gen Virol. 2012;93:1996–2007. doi: 10.1099/vir.0.043059-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sandbulte MR, Westgeest KB, Gao J, Xu X, Klimov AI, Russell CA, et al. Discordant antigenic drift of neuraminidase and hemagglutinin in H1N1 and H3N2 influenza viruses. Proc Natl Acad Sci U S A. 2011;108:20748–53. doi: 10.1073/pnas.1113801108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Colman PM, Tulip WR, Varghese JN, Tulloch PA, Baker AT, Laver WG, et al. Three-dimensional structures of influenza virus neuraminidase-antibody complexes. Philos Trans R Soc Lond B Biol Sci. 1989;323:511–8. doi: 10.1098/rstb.1989.0028. [DOI] [PubMed] [Google Scholar]
- 168.Laver WG, Webster RG, Colman PM. Crystals of antibodies complexed with influenza virus neuraminidase show isosteric binding of antibody to wild-type and variant antigens. Virology. 1987;156:181–4. doi: 10.1016/0042-6822(87)90451-x. [DOI] [PubMed] [Google Scholar]
- 169.Colman PM, Laver WG, Varghese JN, Baker AT, Tulloch PA, Air GM, et al. Three-dimensional structure of a complex of antibody with influenza virus neuraminidase. Nature. 1987;326:358–63. doi: 10.1038/326358a0. [DOI] [PubMed] [Google Scholar]
- 170.Malby RL, Tulip WR, Harley VR, McKimm-Breschkin JL, Laver WG, Webster RG, et al. The structure of a complex between the NC10 antibody and influenza virus neuraminidase and comparison with the overlapping binding site of the NC41 antibody. Structure. 1994;2:733–46. doi: 10.1016/s0969-2126(00)00074-5. [DOI] [PubMed] [Google Scholar]
- 171.Wan H, Yang H, Shore DA, Garten RJ, Couzens L, Gao J, et al. Structural characterization of a protective epitope spanning A(H1N1)pdm09 influenza virus neuraminidase monomers. Nat Commun. 2015;6:6114. doi: 10.1038/ncomms7114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Venkatramani L, Bochkareva E, Lee JT, Gulati U, Graeme Laver W, Bochkarev A, et al. An epidemiologically significant epitope of a 1998 human influenza virus neuraminidase forms a highly hydrated interface in the NA-antibody complex. J Mol Biol. 2006;356:651–63. doi: 10.1016/j.jmb.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 173.Gulati U, Hwang CC, Venkatramani L, Gulati S, Stray SJ, Lee JT, et al. Antibody epitopes on the neuraminidase of a recent H3N2 influenza virus (A/Memphis/31/98) J Virol. 2002;76:12274–80. doi: 10.1128/JVI.76.23.12274-12280.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Webster RG, Air GM, Metzger DW, Colman PM, Varghese JN, Baker AT, et al. Antigenic structure and variation in an influenza virus N9 neuraminidase. J Virol. 1987;61:2910–6. doi: 10.1128/jvi.61.9.2910-2916.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wan H, Gao J, Xu K, Chen H, Couzens LK, Rivers KH, et al. Molecular basis for broad neuraminidase immunity: conserved epitopes in seasonal and pandemic H1N1 as well as H5N1 influenza viruses. J Virol. 2013;87:9290–300. doi: 10.1128/JVI.01203-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Doyle TM, Hashem AM, Li C, Van Domselaar G, Larocque L, Wang J, et al. Universal anti-neuraminidase antibody inhibiting all influenza A subtypes. Antiviral Res. 2013;100:567–74. doi: 10.1016/j.antiviral.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 177.Sandbulte MR, Jimenez GS, Boon AC, Smith LR, Treanor JJ, Webby RJ. Cross-reactive neuraminidase antibodies afford partial protection against H5N1 in mice and are present in unexposed humans. PLoS Med. 2007;4:e59. doi: 10.1371/journal.pmed.0040059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Marcelin G, DuBois R, Rubrum A, Russell CJ, McElhaney JE, Webby RJ. A contributing role for anti-neuraminidase antibodies on immunity to pandemic H1N1 2009 influenza A virus. PLoS One. 2011;6:e26335. doi: 10.1371/journal.pone.0026335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Couch RB, Atmar RL, Franco LM, Quarles JM, Wells J, Arden N, et al. Antibody correlates and predictors of immunity to naturally occurring influenza in humans and the importance of antibody to the neuraminidase. J Infect Dis. 2013;207:974–81. doi: 10.1093/infdis/jis935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Monto AS, Petrie JG, Cross RT, Johnson E, Liu M, Zhong W, et al. Antibody to influenza virus neuraminidase: an independent correlate of protection. J Infect Dis. 2015;212:1191–9. doi: 10.1093/infdis/jiv195. [DOI] [PubMed] [Google Scholar]
- 181.Memoli MJ, Shaw PA, Han A, Czajkowski L, Reed S, Athota R, et al. Evaluation of antihemagglutinin and antineuraminidase antibodies as correlates of protection in an influenza A/H1N1 virus healthy human challenge model. MBio. 2016;7:e00417–16. doi: 10.1128/mBio.00417-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Wohlbold TJ, Krammer F. In the shadow of hemagglutinin: a growing interest in influenza viral neuraminidase and its role as a vaccine antigen. Viruses. 2014;6:2465–94. doi: 10.3390/v6062465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Rudneva IA, Sklyanskaya EI, Barulina OS, Yamnikova SS, Kovaleva VP, Tsvetkova IV, et al. Phenotypic expression of HA-NA combinations in human-avian influenza A virus reassortants. Arch Virol. 1996;141:1091–9. doi: 10.1007/BF01718612. [DOI] [PubMed] [Google Scholar]
- 184.Xu R, Zhu X, McBride R, Nycholat CM, Yu W, Paulson JC, et al. Functional balance of the hemagglutinin and neuraminidase activities accompanies the emergence of the 2009 H1N1 influenza pandemic. J Virol. 2012;86:9221–32. doi: 10.1128/JVI.00697-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kaverin NV, Gambaryan AS, Bovin NV, Rudneva IA, Shilov AA, Khodova OM, et al. Postreassortment changes in influenza A virus hemagglutinin restoring HA-NA functional match. Virology. 1998;244:315–21. doi: 10.1006/viro.1998.9119. [DOI] [PubMed] [Google Scholar]
- 186.Mitnaul LJ, Matrosovich MN, Castrucci MR, Tuzikov AB, Bovin NV, Kobasa D, et al. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J Virol. 2000;74:6015–20. doi: 10.1128/jvi.74.13.6015-6020.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hughes MT, Matrosovich M, Rodgers ME, McGregor M, Kawaoka Y. Influenza A viruses lacking sialidase activity can undergo multiple cycles of replication in cell culture, eggs, or mice. J Virol. 2000;74:5206–12. doi: 10.1128/jvi.74.11.5206-5212.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kaverin NV, Matrosovich MN, Gambaryan AS, Rudneva IA, Shilov AA, Varich NL, et al. Intergenic HA-NA interactions in influenza A virus: postreassortment substitutions of charged amino acid in the hemagglutinin of different subtypes. Virus Res. 2000;66:123–9. doi: 10.1016/s0168-1702(99)00131-8. [DOI] [PubMed] [Google Scholar]
- 189.Ginting TE, Shinya K, Kyan Y, Makino A, Matsumoto N, Kaneda S, et al. Amino acid changes in hemagglutinin contribute to the replication of oseltamivir-resistant H1N1 influenza viruses. J Virol. 2012;86:121–7. doi: 10.1128/JVI.06085-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Squires RB, Noronha J, Hunt V, Garcia-Sastre A, Macken C, Baumgarth N, et al. Influenza research database: an integrated bioinformatics resource for influenza research and surveillance. Influenza Other Respir Viruses. 2012;6:404–16. doi: 10.1111/j.1750-2659.2011.00331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bohne-Lang A, von der Lieth CW. GlyProt: in silico glycosylation of proteins. Nucleic Acids Res. 2005;33:W214–9. doi: 10.1093/nar/gki385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Tsibane T, Ekiert DC, Krause JC, Martinez O, Crowe JE, Jr, Wilson IA, et al. Influenza human monoclonal antibody 1F1 interacts with three major antigenic sites and residues mediating human receptor specificity in H1N1 viruses. PLoS Pathog. 2012;8:e1003067. doi: 10.1371/journal.ppat.1003067. [DOI] [PMC free article] [PubMed] [Google Scholar]