Abstract
BACKGROUND
There are currently no assessments of the impact of surgical complications on health-related quality of life in gynecology and gynecologic oncology. This is despite complications being a central focus of surgical outcome measurement, and an increasing awareness of the need for patient-reported data when measuring surgical quality.
OBJECTIVE
We sought to measure the impact of surgical complications on health-related quality of life at 1 month postoperatively, in women undergoing gynecologic and gynecologic oncology procedures.
STUDY DESIGN
This is a prospective cohort study of women undergoing surgery by gynecologic oncologists at a tertiary care academic center from October 2013 through October 2014. Patients were enrolled preoperatively and interviewed at baseline and 1, 3, and 6 months postoperatively. Health-related quality of life measures included validated general and disease-specific instruments, measuring multiple aspects of health-related quality of life, including anxiety and depression. The medical record was abstracted for clinical data and surgical complications were graded using validated Clavien-Dindo criteria, and women grouped into those with and without postoperative complications. Bivariate statistics, analysis of covariance, responder analysis, and multivariate modeling was used to analyze the relationship of postoperative complications to change health-related quality of life from baseline to 1 month. Plots of mean scores and change over time were constructed.
RESULTS
Of 281 women enrolled, response rates were 80% (n = 231/281) at baseline, and from that cohort, 81% (n = 187/231), 74% (n = 170/231), and 75% (n = 174/231) at 1, 3, and 6 months, respectively. The primary analytic cohort comprised 185 women with completed baseline and 1-month interviews, and abstracted clinical data. Uterine (n = 84, 45%), ovarian (n = 23, 12%), cervical (n = 17, 9%), vulvar (n = 3, 2%), and other (n = 4, 2%) cancers were represented, along with 53 (30%) cases of benign disease. There were 42 (24%) racial/ethnic minority women. Minimally invasive (n = 115, 63%) and laparotomy (n = 60, 32%) procedures were performed. Postoperative complications occurred in 47 (26%) of patients who experienced grade 1 (n = 12), grade 2 (n = 29), and grade 3 (n = 6) complications. At 1 month, physical (20.6 vs 22.5, P = .04) and functional (15.4 vs 18.3, P = .02) well-being, global physical health (43.1 vs 46.3, P = .02), and work ability (3 vs 7.2, P = .001)were lower in postoperative complication vs non-postoperative complication women. Relative change, however, in most health-related quality of life domains from baseline to 1 month did not differ between postoperative complication and nonpostoperative complication groups. Postoperative complication patients did have increased odds of sustained or worsened anxiety at 1 month vs baseline (odds ratio, 2.5; 95% confidence interval, 1.2–5.0) compared to nonpostoperative complication patients.
CONCLUSION
Collectively, women who experienced postoperative complications after gynecologic and gynecologic oncology procedures did not appear to have differences in most health-related quality of life trends over time compared to those who did not. An exception was anxiety, where postoperative complications were associated with sustained or worsened levels of high anxiety after surgery.
Keywords: gynecologic oncology, postoperative complications, quality of life, surgery
Introduction
Patient-centered outcomes are of increasing importance in medical research. The Affordable Care Act1 provided $150 million in annual funding for the Patient-Centered Outcome Research Institute, an organization expressly committed to addressing the questions and concerns most relevant to patients when comparing treatment strategies.2 Although there is robust research on patient-centered outcomes among patients undergoing medical therapies, research in patient-centered outcomes after surgical procedures is lacking. In January 2015, funding from the Agency for Health Care Quality supported a stakeholder conference on patient-reported outcomes (PRO) in surgery with a major goal of prioritizing PRO research in surgery.3
An area of surgical quality that is under increasing scrutiny is surgical complications.4 However, we are limited in our ability to measure them through our current surgical evaluation systems. The utility of complication data driven purely through administrative claims has been questioned.5 Claims data are a poor source of information regarding symptom burden and functional impairment, however these key aspects of health-related quality of life (HRQOL) can be reliably assessed via PRO measures.
Currently, the impact of surgical complications on patient-reported HRQOL is unknown. We,6 along with others7,8 have previously published on the relationship between preoperative HRQOL domains and postoperative complications. In this study we sought to discover what aspects of HRQOL are affected by adverse surgical outcomes in a new, larger, prospective cohort. The goals of this study were to measure the impact of surgical complications on HRQOL in women undergoing gynecologic and gynecologic oncology procedures, using current commonly used PRO instruments to measure overall and cancer-specific HRQOL. The primary outcome of change in HRQOL scores was measured at 1 month, or 30 days, consistent with the commonly used 30-day window for postoperative complication assessment and postoperative recovery milestones.
Materials and Methods
Study design, enrollment, and data collection
We conducted a prospective longitudinal cohort study of women enrolled in the Health Registry/Cancer Survivorship Cohort (HR/CSC) at the University of North Carolina. This study was approved by the institutional review board (study no. 13-2367) and enrolled patients from October 2013 through October 2014, with final follow-up through May 2015. Under the HR/CSC protocol, patients were identified and recruited through the University of North Carolina health care oncology outpatient clinics with the following eligibility criteria: age ≥18 years; North Carolina mailing address; and English or Spanish speaking. Patients unable to provide informed consent or participate in interview questionnaires were excluded. For this study, eligibility was further restricted to HR/CSC patients recruited through the gynecologic oncology clinics, with newly diagnosed gynecologic cancer and planned surgical management. Initial exclusion criteria included primary surgery completed or to be completed at an outside institution, previous chemotherapy or radiation therapy, and pregnancy. After the first 10 weeks of enrollment, the exclusion criteria were modified to allow for retention of patients with final benign pathology to allow inclusion of women undergoing surgery for suspicious pelvic masses/suspected ovarian cancer. The exclusion criteria were also modified to include patients with prior, but not active, chemotherapy or radiation treatment to allow inclusion of patients with new recurrences.
Baseline interviews were conducted within 2 weeks of enrollment, prior to surgery, by trained staff using a computer-assisted telephone interview software tool specifically developed for the HR/CSC. Follow-up interviews were conducted at 1, 3, and 6 months after surgery. Patients were included who completed follow-up interviews within a 3-week interval around each targeted time point (1 week prior or up to 2 weeks after the target date [eg, 1, 3, or 6 months postsurgery]). Participants received gift cards as compensation after completion of each interview. Interview questionnaire topics included medical and social histories, and general and cancer-specific HRQOL assessments. The cohort was limited to participants who met all inclusion criteria and completed at least the baseline and 1-month interviews, as this was the primary outcome point of the analysis. As a secondary outcome, the 3- and 6-month data of this cohort were also reported.
The following validated questionnaires were included in this analysis: the Functional Assessment of Cancer Therapy (FACT)-General Population (GP),9 the PRO Measurement Information System (PROMIS) Global Health Short Form v1.0,10 PROMIS Anxiety 4-item Short Form11 and PROMIS Depression 4-item Short Form,11 and the modified Work Ability Index (WAI).12 The FACT-GP version 4 is a 21-item scale that measures 4 HRQOL subscales: physical, functional, emotional, and social well-being. The minimally important difference (MID) for the FACT-GP is 5–7 points, and 2–3 points for each subscale. The FACT-GP covers a wide range of patient experiences (eg, pain, energy levels, social support) and is commonly used in gynecologic oncology clinical trials (Appendix). The PROMIS global is a 10-item scale including questions about fatigue, physical function, pain, emotional distress, and social health that are summarized into measures of physical and mental health. PROMIS scales are scored using T scores (0–100 scale), which are standardized to the US general population and have a mean of 50 and SD of 10. The modified WAI includes a subset of questions from the original scale, designed to assess work ability compared to lifetime best, in relation to mental and physical demands, and sick leave.12 The specific question analyzed for this study was, “Assume that your ability to work at its best has a value of 10 points and 0 means that you cannot currently work at all. How many points would you give your current ability to work?” with a 0–10 scale response.
Patients’ self-reported age, race/ethnicity, marital status, and employment status were obtained from the HR/CSC baseline interview. The electronic medical record was reviewed (physician, nursing, and case management staff documentation) to abstract clinical data at the time of new patient visit (body mass index [BMI], comorbid conditions, cancer site) and during the 30-day postoperative follow-up window (surgical procedure, postoperative complications, and adjuvant treatment plan). Composite variables of major medical comorbidity and postoperative complication were created as reported in previous studies.6,13 The major comorbidity variable included notation in the record for at least 1 of these conditions: diabetes, pulmonary disease (chronic obstructive pulmonary disease, restrictive lung disease, home oxygen requirement), cardiac disease (congestive heart failure, history of myocardial infarction, coronary artery disease), immunocompromised states (HIV, chronic steroid use), and chronic kidney disease. Surgical complications were identified and graded using Clavien-Dindo criteria.14 All medical record abstraction data were limited to encounters at our institution, however patients were asked about outside medical encounters at each follow-up interview session. Those that reported encounters associated with surgical complications (n = 2) were recorded as experiencing a postoperative complication. Insurance status, at the time of the new patient visit, was also abstracted from the medical record. The medical record information was then merged with the HR/CSC demographic and interview data.
Statistical analysis
This study was designed to have 80% power to detect an effect size of 0.47 for comparing mean change in FACT-GP physical well-being scores between women with and without surgical complications at an alpha of 0.05. Change was defined for each woman as the difference in score between 1 month and baseline (ie, 1-month score – baseline score). We planned enrollment of 225 women, assuming 200 would have evaluable baseline and 1-month data and 50 would have surgical complications. Based on our actual number of evaluable women of 187 (47 of whom had complications), we had 80% power to detect an effect size of 0.49.
Summary statistics were generated using simple frequencies and percentages for categorical variables and mean with SD for continuous variables. Bivariate statistics using Student t tests for continuous data and χ2 tests for categorical data were used to compare baseline characteristics between women with and without complications. Histograms of survey scale responses were constructed to determine normality. The primary outcome, change in mean score from baseline to 1 month, was defined as Δ score = 1-month score – baseline score. Mean scores and mean change in scores of the FACT-GP and subscales, PROMIS global health, and PROMIS anxiety and depression scales were compared using Student t tests accounting for unequal variance. Multivariate linear regression models were constructed and adjusted for age, BMI, and any HRQOL scores that differed significantly at baseline. All other potential covariates were explored and were to be included only if they were associated (P < .05) with both the exposure (complications) and the outcomes (change in specific HRQOL score). No other covariates met these criteria.
To describe how HRQOL domains behaved within each group, we performed responder analyses by categorizing the trend in score change (from baseline to 1 month) into 3 groups: increased, no change, and decreased. This allowed us to examine what fraction of women in each group experienced improvement in a given HRQOL domain, compared to their baseline. Scores had to change in a magnitude greater than the MID for each scale to be categorized as increased or decreased. For example, the MID for the FACT-GP is 5–7. Therefore, only a score that increased by at least 5 points would be in that category. Otherwise, a score that changed by <5 points, in either direction, was grouped under “no change.” A Fisher exact test was used to compare proportions of each category between women with and without surgical complications. For the responder analysis that was statistically significant, the likelihood of increase/no change in score vs decrease was estimated using a multivariate logistic regression model. The question from the modified WAI was analyzed using parametric (Student t test) and nonparametric (Wilcoxon rank-sum test) approaches, given the 0–10 response scale and skewed sample sizes of the responders. For the secondary analysis, graphs of mean score over time, from baseline to 6 months, stratified by complication groups, were constructed.
Results
Study population
Of 281 women who consented for the study, 231 (82%) completed baseline interviews. Of the 50 nonparticipants, 12 were ineligible due to protocol or withdrawal, and 38 did not reply to interview requests. Of the 231 women who completed the baseline interview, 187 completed 1-month interviews, 185 of whom had completed medical record abstraction data. These 185 comprised the final study cohort based on the a priori primary outcome measure. These 185 were 65% (185/281) of the initial enrollment cohort and 80% of those who completed baseline interviews. Subsequent follow-up rates, based on the baseline interview, were 74% (170/231) at 3 months and 75% (174/231) at 6 months for the secondary outcome measures (Figure 1).
FIGURE 1. Study population.
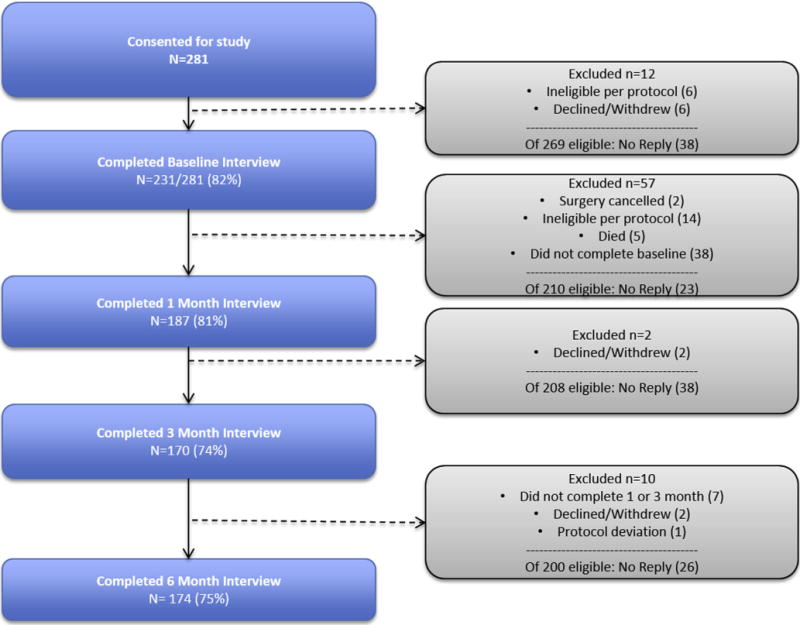
Response rate percentages represent respondents/eligible respondents, as detailed in right-sided bubbles. After completion of baseline interview, participants could miss 1 of 3 follow-up interviews and remain in study. For 1-month primary outcome, 2 patients were missing complete clinical records, yielding final primary cohort of N = 185. Participation rate at 1, 3, and 6 months is based on cohort that completed baseline interview (n = 231).
From the 231 women who completed the baseline interview, responders and nonresponders at 1 month were assessed for differences in baseline characteristics. There was a greater proportion of ovarian cancer in nonresponders (39% vs 12%), with associated greater proportion of debulking procedures (26% vs 10%), and composite postoperative complications (35% vs 25%). These differences were expected as ovarian cancer patients have the highest rate of complication and readmissions among gynecologic cancers, and thus may be the most difficult to follow up for serial interview assessments. Responders and nonresponders were balanced on all other characteristics (Supplemental Table 1).
Table 1 details the baseline characteristics of the main study cohort. Due to small numbers, non-white and non-black races were collapsed into an “other” category, which included Asian (n = 2, 1%), Native American (n = 3, 1.6%), and other (n = 5, 2.7%) respondents. There were 8 Hispanic women, 1 who identified as white, 1 as black, and 5 as other. There were 54 women with suspected malignancy who had benign disease on final pathology. These women were kept in the cohort, given they had procedures and therefore associated postoperative risks similar to those with cancer on final pathology. The group of women who experienced a postoperative complication had a larger proportion of ovarian cancer, unemployed status (including retired individuals), laparotomy, debulking surgery, bowel surgery, and adjuvant therapy compared to the women without complications.
TABLE 1.
Baseline characteristics of women undergoing gynecologic oncology surgery, overall and by occurrence of postoperative complicationa
| Characteristics | Overall N = 185 (100) |
No postoperative complications n = 137 (74) |
Any postoperative complication n = 47 (26) |
|---|---|---|---|
| Age, y, mean (SD) [range] | 56.5 (13) [22–93] | 56 (14) [22–93] | 58 (12) [34–82] |
| Race | |||
| White | 143 (77) | 107 (78) | 36 (77) |
| Black | 32 (17) | 24 (18) | 8 (17) |
| Other | 10 (5) | 7 (4) | 3 (6) |
| Insurance | |||
| None | 14 (8) | 11 (8) | 3 (6) |
| Medicare only | 8 (4) | 6 (4) | 2 (4) |
| Medicaid | 7 (4) | 6 (4) | 1 (2) |
| Any private | 156 (84) | 115 (83) | 41 (87) |
| Marital status | |||
| Partnered | 114 (62) | 84 (61) | 30 (64) |
| Single | 51 (28) | 40 (29) | 11 (23) |
| Widowed | 20 (11) | 14 (10) | 6 (13) |
| Employment | |||
| No | 98 (53) | 69 (50) | 29 (62) |
| Yes | 87 (47) | 69 (50) | 18 (38) |
| Cancer site | |||
| Uterine | 84 (45) | 63 (46) | 21 (45) |
| Ovary | 23 (12) | 13 (9) | 10 (21) |
| Cervix | 17 (9) | 14 (10) | 3 (6) |
| Vulva/vaginal | 3 (1.6) | 1 (0.7) | 2 (4) |
| Otherb | 4 (2) | 2 (1.4) | 2 (4) |
| Benign | 54 (29) | 45 (33) | 9 (19) |
| Major comorbidityc | |||
| No | 163 (88) | 124 (90) | 39 (82) |
| Yes | 22 (12) | 14 (10) | 8 (17) |
| BMI, mean (SD) [range] | 32.9 (9) [17–58] | 32 (8.7) [17–56] | 34 (10.2) [19–58] |
| Procedure typed | |||
| MISd | 116 (63) | 95 (69) | 21 (45) |
| Laparotomy | 60 (32) | 38 (28) | 22 (47) |
| Debulking | 20 (10) | 11 (8) | 9 (19) |
| Radical hysterectomy | 13 (7) | 10 (7) | 3 (6) |
| Bowel surgery | 12 (7) | 6 (4) | 6 (13) |
| Adjuvant therapye | |||
| Yes | 77 (42) | 51 (37) | 26 (55) |
| No | 55 (30) | 43 (31) | 12 (26) |
| NAe | 53 (29) | 44 (32) | 9 (19) |
BMI, body mass index; MIS, minimally invasive surgery (including traditional and robotic-assisted laparoscopy); NA, not applicable (benign disease).
All data presented as no. (%) unless otherwise noted;
Includes: 1 patient with gynecologic malignancy, unknown primary, and 3 patients with final pathology of gastrointestinal origin;
Includes: diabetes, history of venous thromboembolism or stroke, chronic renal disease, immunosuppression, or cardiac disease (excluding hypertension);
These are nonexclusive categories of procedures performed and therefore do not add up to 100%;
Includes: chemotherapy, radiation, or hormonal therapy.
There were 47 women with postoperative complications (Supplemental Table 2), of which 12 were grade 1, 29 were grade 2, and 6 were grade 3. Baseline HRQOL scores were compared between women who did and did not have complications (Table 2). At baseline, the surgical complication group had a mean FACT physical well-being score 1.9 points lower (MID 2–3 points), and a PROMIS global physical health score 3.2 points lower (MID 4–7 points) than the noncomplication group.
TABLE 2.
Baseline health-related quality-of-life scores by occurrence of surgical complications
| Baseline
|
|||
|---|---|---|---|
| Surgical complication
|
|||
| Survey Mean (SD) | No, n = 137 | Yes, n = 47 | P |
| FACT-GP | 83.0 (18) | 79.0 (22) | .22 |
|
| |||
| Physical | 23.2 (4.8) | 21.3 (7.0) | .04 |
|
| |||
| Functional | 20.6 (6.7) | 18.8 (6.2) | .13 |
|
| |||
| Emotional | 16.4 (6.1) | 16.0 (6.6) | .71 |
|
| |||
| Social | 22.9 (5.2) | 22.9 (6.4) | .98 |
| PROMIS global health | |||
|
| |||
| Physical | 47.8 (8.5) | 44.6 (8.2) | .03 |
|
| |||
| Mental | 50.1 (7.9) | 49.9 (9.3) | .90 |
|
| |||
| PROMIS anxiety | 54.5 (8.7) | 53.1 (9.5) | .35 |
|
| |||
| PROMIS depression | 54.3 (6.6) | 54.0 (6.5) | .79 |
|
| |||
| Currently working, n (%) | 69 (50) | 18 (39) | .20 |
|
| |||
| Work Ability Index | 8.8 (2.3) Median 10 [IQR 9–10] |
7.7 (3.2) Median 9.5 [IQR 5–10] |
.13a |
FACT-GP, Functional Assessment of Cancer Therapy-General Population; IQR, interquartile range; PROMIS, Patient-Reported Outcomes Measurement Information System.
Wilcoxon rank-sum test.
Surgical complications and HRQOL changes
The primary outcome was the effect of surgical complications on the degree of change in mean HRQOL scores from baseline to 1 month (Table 3). There were no statistically significant differences in the magnitude of change in scores between women with and without surgical complications on bivariate testing (not shown). The results of the multivariate linear regression are shown in Table 3. The models were adjusted for age, BMI, and the 2 baseline HRQOL scores that differed significantly between the groups: PROMIS physical health and the physical well-being subscale of the FACT-GP. The point estimates represent the adjusted difference in mean change (from baseline to 1 month), between those who did and did not have surgical complications. For example, for the functional well-being subscale, the mean change in score from baseline to 1-month postoperatively was 2.07 points lower for the group that had complications, compared to the groups that did not (P = .06). Although no results were statistically significant, the largest differences between the groups were in functional well-being, global physical health, and anxiety scores.
TABLE 3.
Multivariate linear regression for change in health-related quality of life scores from baseline to 1 month after surgery, by occurrence of surgical complicationsa
| Survey | Point estimate | 95% CI | P value |
|---|---|---|---|
| Δ FACT-GP | −1.89 | −6.32 to 2.55 | .40 |
| Δ Physical well-being | −1.06 | −2.65 to 0.52 | .19 |
| Δ Functional well-being | −2.07 | −4.19 to 0.06 | .06 |
| Δ Emotional well-being | 0.08 | −1.69 to 1.85 | .93 |
| Δ Social well-being | 0.44 | −1.03 to 1.91 | .55 |
| PROMIS scales | |||
| Δ Global physical health | −1.59 | −3.81 to 0.62 | .16 |
| Δ Global mental health | −1.92 | −4.56 to 0.73 | .15 |
| Δ Anxiety | 2.51 | −0.47 to 5.49 | .10 |
| Δ Depression | 0.48 | −1.68 to 2.63 | .66 |
CI, confidence interval; FACT-GP, Functional Assessment of Cancer Therapy-General Population; PROMIS, Patient-Reported Outcomes Measurement Information System.
Regression model for mean score change in complication group (vs no-complication group) adjusted for age, body mass index, baseline PROMIS physical health score, and baseline physical well-being subscale score. Point estimates are adjusted difference in mean change from baseline, between those who did and did not have surgical complications. Negative estimates indicate greater decrease in scores in complication group.
A trend was noted with the PROMIS anxiety measure, where women without surgical complications had an adjusted mean decrease in anxiety score double that of women with complications (6.1 vs 3.0 points, P = .07). A responder analysis was completed for each survey instrument, by grouping women into those whose scores increased, decreased, or had no change from baseline to 1 month. The proportions of the 3 groups were then compared between those who did and did not have complications. These results were also nonsignificant (not shown), with the exception of the PROMIS anxiety measure.
Women with surgical complications were more likely to have increased or stable anxiety at 1 month after surgery (66%, n = 31), compared to women who did not (44%, n = 61) (P = .03) (Supplemental Table 3). The 4 questions in PROMIS were: anxiety instrument focused on “feeling fearful,” “focusing on anxiety,” “feeling uneasy,” and feeling “worried or overwhelmed.” In the first 3 listed domains (fearful, focus on anxiety, unease), women who experienced a complication had higher mean scores (reflecting more of the feeling) than those who did not. The most notable difference was in the measure of feeling uneasy. In patients who experienced postoperative complications, 72% (n = 34/47) had feelings of unease that were no different or increased from their baseline, preoperative levels, compared to 50% (n = 69/138, P = .021). In a multivariate logistic regression model, adjusting for age, BMI, and baseline PROMIS physical health and physical well-being, patients who experienced a postoperative complication had an odds of stable or increased anxiety 2.6 times that of patients who did not at 1 month after surgery (odds ratio, 2.63; 95% confidence interval, 1.25–5.6). Given that the entire cohort has baseline anxiety above the general population norms, this represents a clinically important effect of postoperative complications.
With regard to work ability, in the complication group, 22% (n = 4/18) of those working at baseline had returned to work at 1 month, compared to 66% (46/69) of those without complications. The WAI question was answered only by those currently working, limiting any further assessment due to small numbers of participants actively working at the 1-month time point.
Exploratory results by complication grade are also presented. Although very limited by a sample size of 6, among the grade 3 group, complications appear to have a greater impact on change in overall physical and mental HRQOL domains in multiple scales. This is shown graphically in Figure 2 where trends from baseline to 6 months post-operatively are shown. Figure 2, A, demonstrates the difference in score trend in FACT-GP among women without complications, those with grade 1–2 complications, and the severe grade 3 subgroup. It may be thought that the HRQOL trend in this small subgroup of severe complications simply reflects an increased likelihood of more complex surgery or chemotherapy toxicity. Therefore, for comparison sake, Figure 2, B, shows the FACT-GP trend among patients experiencing these other significant events of adjuvant chemotherapy and complex surgery, alongside the patients with severe complications.
FIGURE 2. Health-related quality of life score trends.
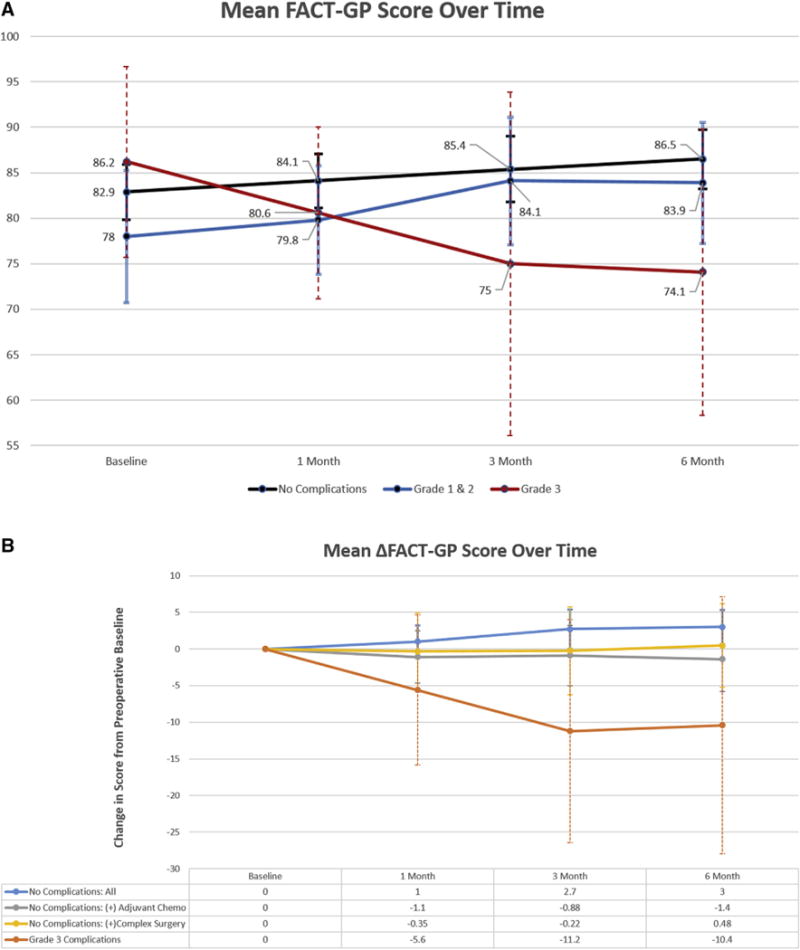
Health-related quality of life score trends: from baseline to 6 months postoperatively. A, Mean scores of women with no complications (n = 137), grade 1 and 2 complications (n = 41), and severe grade 3 complications (n = 6). B, Change in mean scores from baseline values, comparing those with severe grade 3 complications vs other postoperative groups without complications: women undergoing adjuvant chemotherapy (n = 51) and those who required complex surgery (n = 23).
Comment
In a cohort of women undergoing gynecologic and gynecologic oncology procedures, we found that the magnitude of change between preoperative and postoperative HRQOL did not differ significantly by the occurrence of surgical complications, with the exception of anxiety. Women who had surgical complications had greater odds of stable or increased anxiety at 1 month after surgery, compared to women who did not experience a complication. Absolute preoperative and postoperative scores on physical well-being and functional well-being (as measured by the FACT-GP), global physical health (as measured by the PROMIS global health), and work ability (as measured by the WAI) are lower in women who experience post-operative complications, consistent with prior studies.6–8 This is among the few studies designed to prospectively test the impact of composite postoperative complications on HRQOL, and the first, to our knowledge, in gynecologic and gynecologic oncology patients.
Patient anxiety is not a benign condition. Anxiety in patients with cancer impacts levels of fatigue15 exacerbates chemotherapy-related nausea and vomiting,16 and is a predictor of dose delays and reductions.17 And, critically important within the postoperative, pre-adjuvant treatment window, anxiety is related to less effective medical decision making.18,19 Why some patients have more anxiety at baseline than others is poorly understood. Our results point to a possible mechanism, especially for cancer patients whose care often begins with surgery. It makes sense that an unexpected adverse event after surgery, no matter how minor, can contribute to feelings of unease and anxiety about health and further treatment. Surgical complications are often thought of as temporary events that are quickly resolved. If complications increase patient anxiety however, this suggests a mechanism for a longer term impact of even minor surgical complications than what is currently considered. It also reemphasizes the need for true baseline preoperative HRQOL measures in all oncology trials where surgery is a component of care. A systematic review of longitudinal anxiety in ovarian cancer patients, published in 20 1 5,20 featured 7 studies with labeled “pretreatment” baseline anxiety levels, only 1 of which actually reported preoperative baseline anxiety, and consisted of 27 patients total.21
Our secondary outcomes of HRQOL trends over 3 and 6 months did not have substantive differences between the complication and noncomplication groups, with the exception of the small subset of 6 patients with grade 3 complications. These are hypothesisgenerating data that support the role of a larger study that focuses on long-term HRQOL trends among women with grade ≥3 surgical complications.
Our study has important limitations to note. It is a single-institution study and therefore the results may not be generalizable in a broader population. We cannot comment on nonparticipation bias, as we do not have abstracted clinical information on the 38 women who were enrolled, remained eligible, but did not complete baseline and/or 1-month interviews. Although patients were asked at the 1-month interview about care received at outside institutions and possible complications, we may still be underestimating the complication rate due to lack of medical record data from other institutions. Unlike clinical trials, the proportion of black women (17%) in our study was representative of the larger state population (22%),22 however, we had under-representation of Hispanic women (3.4%) compared to the state (8%).22 This may in part be due to the relatively young median age of Hispanics in the state (33 years)23 compared to the median age of gynecologic oncology patients (49–68 years).24 We also had an overrepresentation of patients with private insurance (84%) compared to the state population of women age > 18 years (68%).22 This may be a population of higher socioeconomic status that in turn has greater ability to withstand the insult of postoperative complications, limiting the effect seen in our data. Our first postoperative assessment was at 1 month and each interview asked the patient to recall experiences over the past 7 days. This schedule may have missed early 1–3 week experiences in surgical recovery, or in the intervening follow-up weeks, that may have resulted in changes in survey scores. Given the study design and power, we are unable to distinguish which kind of complications resulted in greater or lesser changes in HRQOL. In addition, we included multiple different procedure types that may inherently affect HRQOL differently, independent of complication. With regard to this, however, we used the same scales used in surgical randomized trials, where these scores were not found to differ by procedure type such as laparoscopy vs laparotomy or sphincter sparing surgery vs abdominoperineal repair.25,26 Finally, the results are not adjusted for multiple testing (9 hypothesis tests) where more conservative P values could be employed. These results need replication in larger sample groups of cancer patients to assure sufficient statistical power for the anticipated effect size.
Our study has many unique aspects and strengths. We had a high response rate (>70%) at each assessment interval through the 6-month interviews, adding robustness to the follow-up data. The interviews were performed by independent trained administrators in person or over the telephone, limiting bias with literacy skills. Our assessments included standardized instruments to measure multiple aspects of HRQOL including depression and anxiety.
Our results have important implications for the selection of HRQOL measures in surgical trails. Although randomized controlled trials of surgery are rare, in essence they are performed to compare such outcomes as surgical complication and HRQOL between 2 techniques. The FACT-GP is a commonly used HRQOL measure in gynecologic oncology trials. Yet, the ability of this tool to discriminate the impact of surgical complications on HRQOL was never tested. Although we cannot answer this definitely with our study design, our results suggest that the FACT-GP may have some reactivity to severe (grade ≥3) complications, but not the more minor complications. One may argue this level of sensitivity is reasonable, because minor complications are not important. However, in the current era of an emphasis on the patient experience, that may be a faulty assumption. Using a HRQOL instrument that fails to detect the impact of minor complications assumes these events are not important to a patient’s quality of life. The truth is that these events may matter greatly to some patients and not at all to others. We should have HRQOL measures designed for a surgical population, to allow patients to participate in shared decision making around surgery, with complete data.
PRO data are critically needed in surgical literature, especially in nonclinical trial populations and in patients with benign and malignant gynecologic disease, to facilitate decision making and treatment evaluation. Therefore, we need more survey measures that are specific to the surgical recovery experience for cancer patients, beyond the FACT-GP. We also need greater awareness and intervention methods for addressing the anxiety that may be a lasting effect of temporary surgical complications. The Society of Gynecologic Oncology, along with many others, is working to define the concepts of “value” and “quality” in surgical care. In addition to considering complication rates, we need to incorporate the impact of such complications, major and minor, on HRQOL.
Supplementary Material
Acknowledgments
The research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health (NIH) under award R25CA116339 and the North Carolina University Cancer Research Fund. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors report no conflict of interest.
Presented at the 47th Annual Meeting on Women’s Cancer of the Society of Gynecologic Oncology, San Diego, CA, March 19-22, 2016.
References
- 1.Patient Protection and Affordable Care Act. Public Law 111-148. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm. Accessed April 28, 2014.
- 2.Patient Centered Outcomes Research Institute. Available at: www.pcori.org/about-us. Accessed Dec. 9, 2015.
- 3.Plastic Surgery Foundation. Patient-reported outcomes in surgery conference. Available at: http://www.thepsf.org/training/pros-conference.htm. Accessed Dec. 9, 2015.
- 4.Pierce O, Allen M. Assessing surgeon-level risk of patient harm during elective surgery for public reporting. 2015 Available at: https://www.propublica.org/article/surgery-risks-patient-safety-surgeon-matters. Accessed October 10, 2015.
- 5.Rosenbaum L. Scoring no goal-further adventures in transparency. N Engl J Med. 2015;373:1385–8. doi: 10.1056/NEJMp1510094. [DOI] [PubMed] [Google Scholar]
- 6.Doll KM, Snavely AC, Kalinowski A, et al. Preoperative quality of life and surgical outcomes in gynecologic oncology patients: A new predictor of operative risk? Gynecol Oncol. 2014;133:546–51. doi: 10.1016/j.ygyno.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ihemelandu CU, McQuellon R, Shen P, Stewart JH, Votanopoulos K, Levine EA. Predicting postoperative morbidity following cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CS+HIPEC) with preoperative FACT-C (Functional Assessment of Cancer Therapy) and patient-rated performance status. Ann Surg Oncol. 2013;20:3519–26. doi: 10.1245/s10434-013-3049-8. [DOI] [PubMed] [Google Scholar]
- 8.Baker J, Janda M, Gebski V, et al. Lower preoperative quality of life increases post-operative risk of adverse events in women with endometrial cancer: results from the LACE trial. Gynecol Oncol. 2015;137:102–5. doi: 10.1016/j.ygyno.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 10.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res. 2009;18:873–80. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): depression, anxiety, and anger. Assessment. 2011;18:263–83. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilmarinen J. The Work Ability Index. Occup Med. 2007;57:160. [Google Scholar]
- 13.Doll KM, Kalinowski AK, Snavely AC, et al. Obesity is associated with worse quality of life in women with gynecologic malignancies: an opportunity to improve patient-centered outcomes. Cancer. 2015;121:395–402. doi: 10.1002/cncr.29061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Long NH, Thanasilp S, Thato R. A causal model for fatigue in lung cancer patients receiving chemotherapy. Eur J Oncol Nurs. 2016;21:242–7. doi: 10.1016/j.ejon.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Andrykowski MA. The role of anxiety in the development of anticipatory nausea in cancer chemotherapy: a review and synthesis. Psychosom Med. 1990;52:458–75. doi: 10.1097/00006842-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Greer JA, Pirl WF, Park ER, Lynch TJ, Temel JS. Behavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. J Psychosom Res. 2008;65:549–52. doi: 10.1016/j.jpsychores.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Traeger L, Greer JA, Fernandez-Robles C, Temel JS, Pirl WF. Evidence-based treatment of anxiety in patients with cancer. J Clin Oncol. 2012;30:1197–205. doi: 10.1200/JCO.2011.39.5632. [DOI] [PubMed] [Google Scholar]
- 19.Latini DM, Hart SL, Knight SJ, et al. The relationship between anxiety and time to treatment for patients with prostate cancer on surveillance. J Urol. 2007;178:826–31. doi: 10.1016/j.juro.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 20.Watts S, Prescott P, Mason J, McLeod N, Lewith G. Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2015;5:e007618. doi: 10.1136/bmjopen-2015-007618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sukegawa A, Miyagi E, Asai-Sato M, et al. Anxiety and prevalence of psychiatric disorders among patients awaiting surgery for suspected ovarian cancer. J Obstet Gynaecol Res. 2008;34:543–51. doi: 10.1111/j.1447-0756.2008.00738.x. [DOI] [PubMed] [Google Scholar]
- 22.Hess C, Hegewisch A, Yi Y, Williams C. The status of women in North Carolina. Washington (DC): Institute for Women’s Policy Research; 2013. [Google Scholar]
- 23.Demographic profile of Hispanics in North Carolina, 2011. Washington (DC): Pew Research Center; 2013. Available at: http://www.pewhispanic.org/states/state/nc/. Accessed June 3, 2016. [Google Scholar]
- 24.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2011. National Cancer Institute; Available from: http://seer.cancer.gov/csr/1975_2011/. Accessed Aug. 1, 2014. [Google Scholar]
- 25.Russell MM, Ganz PA, Lopa S, et al. Comparative effectiveness of sphincter-sparing surgery versus abdominoperineal resection in rectal cancer: patient-reported outcomes in National Surgical Adjuvant Breast and Bowel Project randomized trial R-04. Ann Surg. 2015;261:144–8. doi: 10.1097/SLA.0000000000000594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kornblith AB, Huang HQ, Walker JL, Spirtos NM, Rotmensch J, Cella D. Quality of life of patients with endometrial cancer undergoing laparoscopic International Federation of Gynecology and Obstetrics staging compared with laparotomy: a Gynecologic Oncology Group study. J Clin Oncol. 2009;27:5337–42. doi: 10.1200/JCO.2009.22.3529. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


