Abstract
Type 2 diabetes results from defects in both insulin sensitivity and insulin secretion. Elevated cholesterol content within pancreatic β-cells has been shown to reduce β-cell function and increase β-cell apoptosis. Hyperglycemia and dyslipidemia contribute to glucolipotoxicity that leads to type 2 diabetes. Here we examined the capacity of glucolipotoxicity to induce free cholesterol accumulation in human pancreatic islets and the INS-1 insulinoma cell line. Glucolipotoxicity treatment increased free cholesterol in β-cells, which was accompanied by increased reactive oxygen species (ROS) production and decreased insulin secretion. Addition of AAPH, a free radical generator, was able to increase filipin staining indicating a link between ROS production and increased cholesterol in β-cells. We also showed the ability of stigmasterol, a common food-derived phytosterol with anti-atherosclerotic potential, to prevent the increase in both free cholesterol and ROS levels induced by glucolipotoxicity in INS-1 cells. Stigmasterol addition also inhibited early apoptosis, increased total insulin, promoted actin reorganization, and improved insulin secretion in cells exposed to glucolipotoxicity. Overall, these data indicate cholesterol accumulation as an underlying mechanism for glucolipotoxicity-induced defects in insulin secretion and stigmasterol treatment as a potential strategy to protect β-cell function during diabetes progression.
Introduction
As of 2014, an estimated 422 million people have diabetes worldwide, with type 2 diabetes representing approximately 90% of the adult cases1. The number of individuals with diabetes and the chronic nature of the disease pose a serious health and economic challenge. Due to the enormity of this issue, there is an urgent need for strategies to reduce the development of the disease. Given that lifestyle changes can be just as effective as drug interventions2, exploring dietary modifications that may prevent onset of type 2 diabetes is a worthwhile endeavor.
Type 2 diabetes is marked by insulin resistance and pancreatic β-cell dysfunction. As peripheral tissues become insulin resistant, insulin producing β-cells residing in pancreatic islets can compensate by increasing mass and secreting more insulin. Once β-cells fail to compensate for insulin resistance, hyperglycemia and type 2 diabetes ultimately occurs. Several genetic and environmental factors predispose individuals towards type 2 diabetes3, 4. In addition, impaired metabolic states, such as metabolic syndrome and obesity, increase risk for type 2 diabetes5. However, the exact causes leading to type 2 diabetes are still under intensive investigation.
Elevated glucose and non-esterified (free) fatty acids, termed glucolipotoxicity, is a major contributor to the progression of type 2 diabetes after predisposing factors are established6. Glucolipotoxicity is shown in vitro to increase β-cell death and decrease insulin secretion7–9. The effect of glucolipotoxicity may be in part due to changes in lipid partitioning and reactive oxygen species (ROS) production10.
Cholesterol accumulation impairs β-cell function, while removal of excess cholesterol promotes β-cell health11, 12. Glucolipotoxicity may lead to increased cholesterol in β-cells as evidenced by studies performed in mouse and cell lines10, 13, 14. Whether intracellular cholesterol plays a role in glucolipotoxicity is unclear. It has been reported that palmitate alone increases total cholesterol in β-cells, but does not coincide with apoptosis10. Others have reported that apoptosis induced by free fatty acids was due to decreased cholesterol within the ER15.
Due to the link between excess cholesterol and β-cell dysfunction, therapies that reduce β-cell cholesterol may be anti-diabetic. Although statins, which are inhibitors of 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase (HMG-CoA reductase, the rate-limiting enzyme for cholesterol synthesis), are best at reducing serum cholesterol in order to prevent cardiovascular diseases, they present a modestly increased risk for the onset of new diabetes cases16–19. Possible mechanisms include side effects that are independent of statin’s cholesterol-lowering property, such as a statin-specific immune response leading to insulin resistance20. Therefore, alternative ways to reduce cholesterol in β-cells are needed.
Phytosterols are found in plant foods and are analogous to cholesterol in mammals. Phytosterols have been of interest due to their well-documented ability to decrease serum LDL-cholesterol levels in humans21, 22, with the greatest reductions at 2.5 grams of phytosterols per day23. Given that the typical Western diet provides 200–400 milligrams of phytosterols per day24, we may not be consuming phytosterols at a level needed for maximum health benefits. Absorption of phytosterols is regulated by small intestinal ATP-binding cassette transporters that export phytosterols into the lumen25. Although the amount of phytosterols absorbed into serum is low, it can accumulate in tissues. A study by Alhazzaa26 showed that feeding rats phytosterols increases accumulation in all the internal organs measured except the brain.
Commonly consumed dietary phytosterols include stigmasterol, campesterol and sitosterol. Stigmasterol has been widely investigated for its anti-atherosclerotic cholesterol-lowering effects. Stigmasterol increases cholesterol efflux and decreases LDL-induced proinflammatory cytokine secretion, whereas campesterol and sitosterol have no beneficial effects27. The purpose of this study is to assess the capacity for stigmasterol, a common food-derived phytosterol with anti-atherosclerotic potential, to prevent β-cell dysfunction induced by glucolipotoxicity.
Results
Glucolipotoxicity reduces insulin secretion by inducing cholesterol accumulation
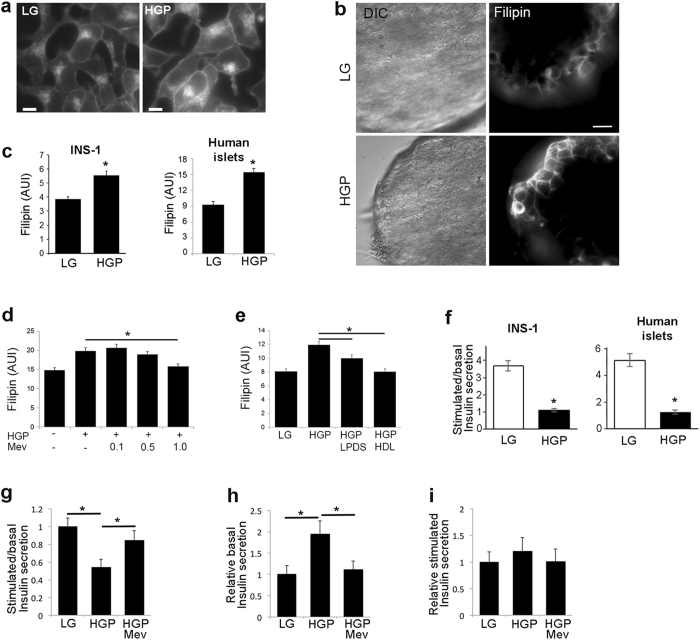
Cholesterol excess is a possible contributing factor to β-cell failure. To determine if glucolipotoxicity treatment can increase free cholesterol within β-cells, INS-1 insulinoma cells and human islets were treated with HGP (30 mM glucose, 0.5 mM palmitate) or normal growth medium (LG) for 72 h. Filipin is a widely used fluorescent probe to measure free cholesterol in cells28. HGP treatment increased filipin staining in INS-1 cells and human islets (Fig. 1a–c). The result from INS-1 cells was consistent with other reports10. To our knowledge, this was the first time the effect of glucolipotoxicity on cholesterol in human islet was examined (Fig. 1b,c). Cholesterol accumulation may occur through increased uptake of LDL, increased biosynthesis, or decreased efflux to acceptors such as HDL. Treatment with mevinolin (Mev), which inhibits the rate-limiting enzyme of cholesterol biosynthesis HMG-CoA reductase, dose-dependently reduced cholesterol accumulation in cells exposed to HGP (Fig. 1d). Similarly, removing LDL as a source for cholesterol uptake by using lipoprotein-deficient serum (LPDS) in place of FBS or adding HDL to LPDS growth medium also inhibited HGP-induced cholesterol accumulation in INS-1 cells (Fig. 1e).
Figure 1.
Glucolipotoxicity increases free cholesterol and decreases insulin secretion. ( a–c) HGP increases free cholesterol. INS-1 cells (a) or human islets (b) were treated for 72 h with control growth medium (LG), or HGP. Filipin per cell, indicating free cholesterol, was quantified from 5 independent experiments (c). DIC, differential interference contrast. AUI, arbitrary unit of intensity. Scale bars, 10 μm. (d) Mevinolin (Mev), an inhibitor of cholesterol synthesis, blocks HGP-induced increase in filipin staining in a dose-dependent manner. Cells were treated with HGP and Mev (μM) in LPDS growth medium for 72 h. (e) LPDS or HDL treatment blocks HGP-induced increase in filipin staining. Cells were treated with LG, HGP, HGP in LPDS medium (HGP + LPDS) or HGP and HDL in LPDS medium (HGP + HDL) for 72 h. (f) HGP decreases GSIS. Static GSIS assays of INS-1 and human islets were performed in cells treated for 72 h with HGP. (g–i) Mev treatment normalizes GSIS (g) by inhibiting HGP-induced basal insulin secretion (h) without affecting stimulated insulin secretion (i). All values are expressed as fold change relative to LG. n = 5 experiments. *p < 0.05.
The increase in cellular free cholesterol was accompanied by reduced glucose-stimulated insulin secretion (GSIS) in both INS-1 cells and human islets treated with HGP (Fig. 1f). Consistent with an inhibitory role of elevated cholesterol in GSIS, GSIS was normalized when HGP-induced cholesterol accumulation was blocked by mevinolin (Fig. 1g). The effect of mevinolin treatment was accomplished through normalization of basal insulin secretion (Fig. 1h), with little effect on stimulated insulin secretion (Fig. 1i).
Oxidative stress increases β-cell cholesterol
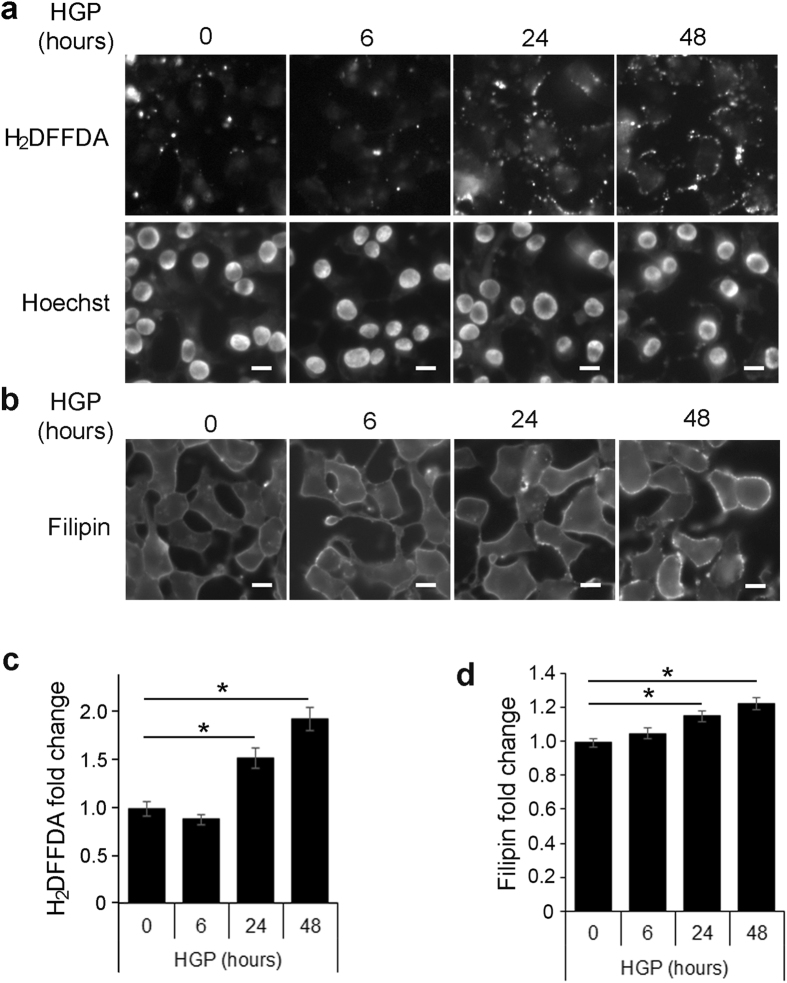
Pancreatic β-cells are particularly susceptible to oxidative stress because they express low levels of intracellular antioxidants29. ROS has been linked to cholesterol accumulation in neurons, vascular smooth muscle cells, and hepatocytes30–32. To determine if ROS may be the underlying cause for HGP-induced cholesterol accumulation, INS-1 cells were incubated with HGP for time periods up to 48 h. As shown in Fig. 2a, HGP increased ROS production as estimated by carboxy-H2DFFDA staining. Carboxy-H2DFFDA becomes fluorescent when oxidized and is used as a general marker of ROS33. The increase in ROS corresponded to a rise in filipin staining (Fig. 2b). The most significant increase in ROS (Fig. 2c) and free cholesterol (Fig. 2d) both took place between 6 and 24 h after HGP treatment, suggesting that the rise in ROS and cholesterol may occur with similar time course.
Figure 2.
Glucolipotoxicity increases ROS in β-cells. (a,b) Timecourse for HGP-induced ROS production (a) and cholesterol accumulation (b). INS-1 cells were incubated for up to 48 h with HGP and imaged using carboxy-H2DFFDA (a) and filipin (b), along with Hoechst stain for cell counting. Scale bars, 10 μm. (c,d) Background-corrected fluorescence was measured for carboxy-H2DFFDA (c) and filipin (d) fluorescence. *p < 0.05.
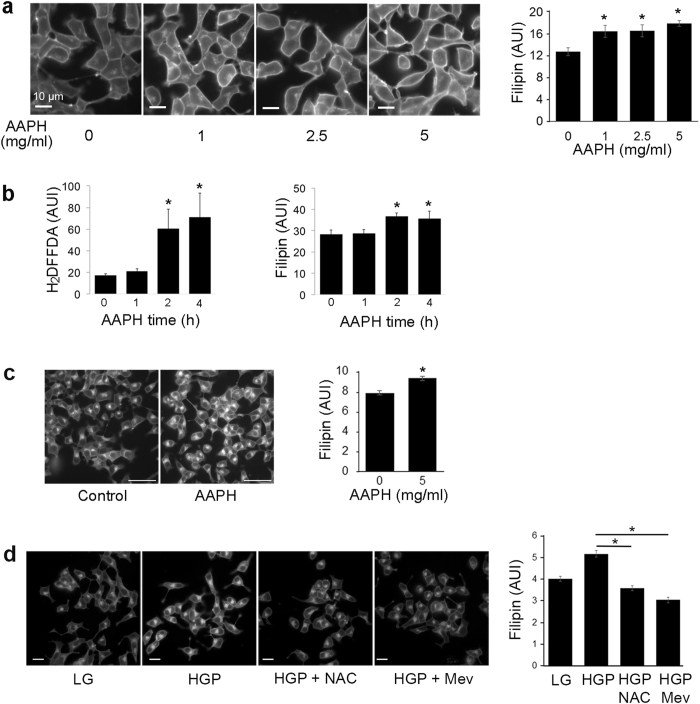
To determine if oxidative stress alone increases cholesterol accumulation in β-cells, INS-1 cells were incubated with AAPH, a water-soluble free radical generator used to produce ROS34, 35 (Supplementary Fig. 1). Cholesterol increased in INS-1 cells treated with varying concentrations of AAPH for 4 h in serum-free media (Fig. 3a). AAPH increased oxidation (H2DFFDA) and filipin staining with a similar temporal pattern, with the most significant rise occurring between one and two hours after AAPH addition (Fig. 3b). At the higher concentration range (5 mg/ml), AAPH was sufficient to increase free cholesterol labeled by filipin staining within 1 h (Fig. 3c). Esterified cholesterol labeled by lipidtox was also increased by AAPH during the same time frame (Supplementary Fig. 2). These data indicate that cholesterol accumulation in β-cells is sensitive to free radical generation. To further determine if ROS is the underlying cause for HGP-induced cholesterol increase in β-cells (Fig. 2), we treated INS-1 cells exposed to HGP with the antioxidant N-acetylcysteine (NAC) to prevent HGP-induced ROS production. Mevinolin (Mev) was included as a positive control of cholesterol depletion. As shown in Fig. 3d, NAC prevented an increase in filipin staining in HGP-treated INS-1 cells. Together with the results from AAPH, these data suggest that ROS stress can raise free cholesterol within β-cells, and the presence of antioxidants can prevent HGP-induced cholesterol increase.
Figure 3.
ROS induces cholesterol accumulation. (a) INS-1 cells were treated with AAPH in concentrations from 0 to 5 mg/ml for 4 h in serum-free media. Free cholesterol was measured using filipin. *p < 0.05 against control (no AAPH). Scale bars, 10 μm. (b) INS-1 cells were treated with 2.5 mg/ml AAPH for the different periods of time. Cellular staining of carboxy-H2DFFDA for ROS content and filipin for free cholesterol content was quantified. *p < 0.05 against control (no treatment). (c) Filipin staining of INS-1 cells incubated for 1 h with 5 mg/ml AAPH in serum free media. Scale bars, 50 μm. Filipin intensity per cell was quantified. *p < 0.05. (d) INS-1 cells were treated with LG, HGP, HGP + NAC (0.5 mM), or HGP + Mev for 48 h. Cells were imaged with filipin to measure free cholesterol. Scale bars, 20 μm. *p < 0.05 against HGP.
Stigmasterol reduces free but not esterified cholesterol
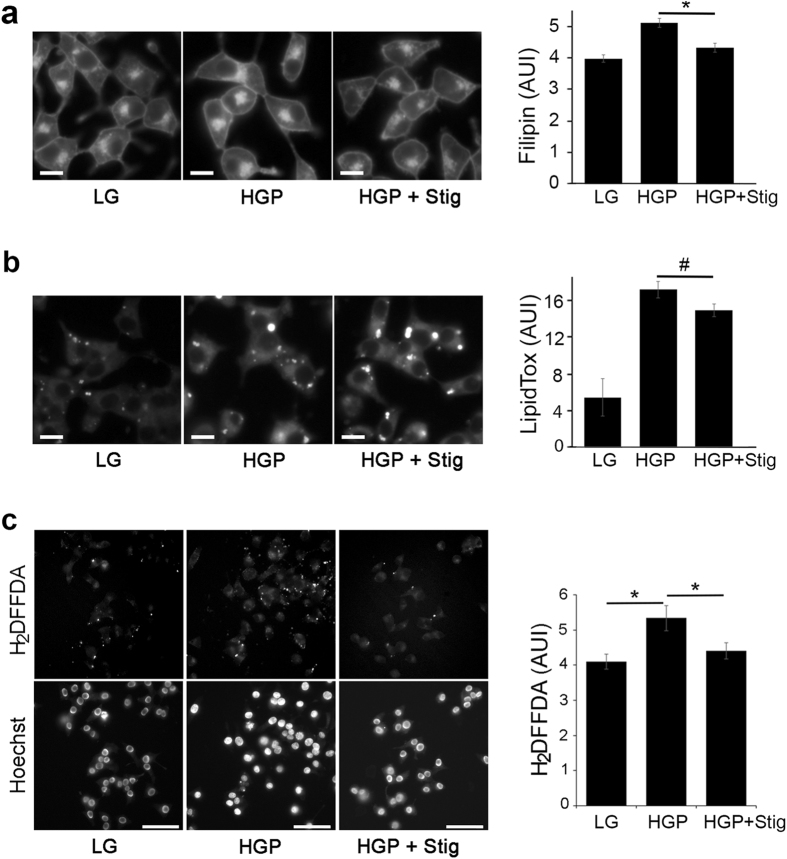
Because glucolipotoxicity increases β-cell cholesterol, which is at least partially responsible for reduced GSIS observed in HGP-treated cells, we next tested whether including stigmasterol with HGP could rescue β-cell function. While there are studies of stigmasterol’s effects on lowering plasma cholesterol levels, how stigmasterol impacts cholesterol pools in cells is not well investigated. Cholesterol is found in either esterified or non-esterified (free) pools within the cell. We utilized filipin to measure free cholesterol and lipidtox to measure neutral lipids in INS-1 cells. As shown in Fig. 4a and b, both filipin and lipidtox staining increased with HGP treatment (HGP vs LG), indicating increased free cholesterol accumulation and conversion to cholesteryl esters. Stigmasterol decreased filipin staining due to HGP treatment (Fig. 4a, HGP + Stig vs HGP). The effect appeared to be specific to free cholesterol, as lipidtox staining, a measure of esterified cholesterol, did not change (Fig. 4b). LPDS treatment, on the hand, reduced both forms of cholesterol in INS-1 cells (Supplementary Fig. 3). At a high concentration, stigmasterol was as effective as LPDS at reducing free cholesterol, but remained ineffective at reducing esterified cholesterol (Supplementary Fig. 3).
Figure 4.
Stigmasterol treatment inhibits HGP-induced increase in free cholesterol and ROS. (a,b) Free cholesterol but not esterified cholesterol was reduced by stigmasterol. INS-1 cells treated for 72 h with LG, HGP, or HGP + stigmasterol (Stig) were stained with filipin (a) and lipidtox (b). Scale bars, 10 μm. *p < 0.05 and #not significant against HGP. (c) ROS is reduced by stigmasterol. INS-1 cells were incubated in LG, HGP, or HGP + stig, and carboxy-H2DFFDA was used to measure ROS production. Carboxy-H2DFFDA fluorescence was quantified by normalizing to cell number (Hoechst staining). Scale bars, 50 μm. *p < 0.05.
Stigmasterol decreases glucolipotoxicity-induced ROS production
Stigmasterol is reported to increase glutathione content in mice, indicating an antioxidative property for stigmasterol36. Because β-cells naturally have low levels of glutathione29, stigmasterol treatment could act by reducing the ROS that accompanies glucolipotoxicity. Increased carboxy-H2DFFDA fluorescence, an indication of elevated ROS, was found in INS-1 cells treated with HGP (Figs 2 and 4c, HGP vs LG). Interestingly, the addition of stigmasterol with HGP decreased the amount of carboxy-H2DFFDA fluorescence, consistent with the idea that stigmasterol could decrease ROS production in β-cells exposed to glucolipotoxicity (Fig. 4c).
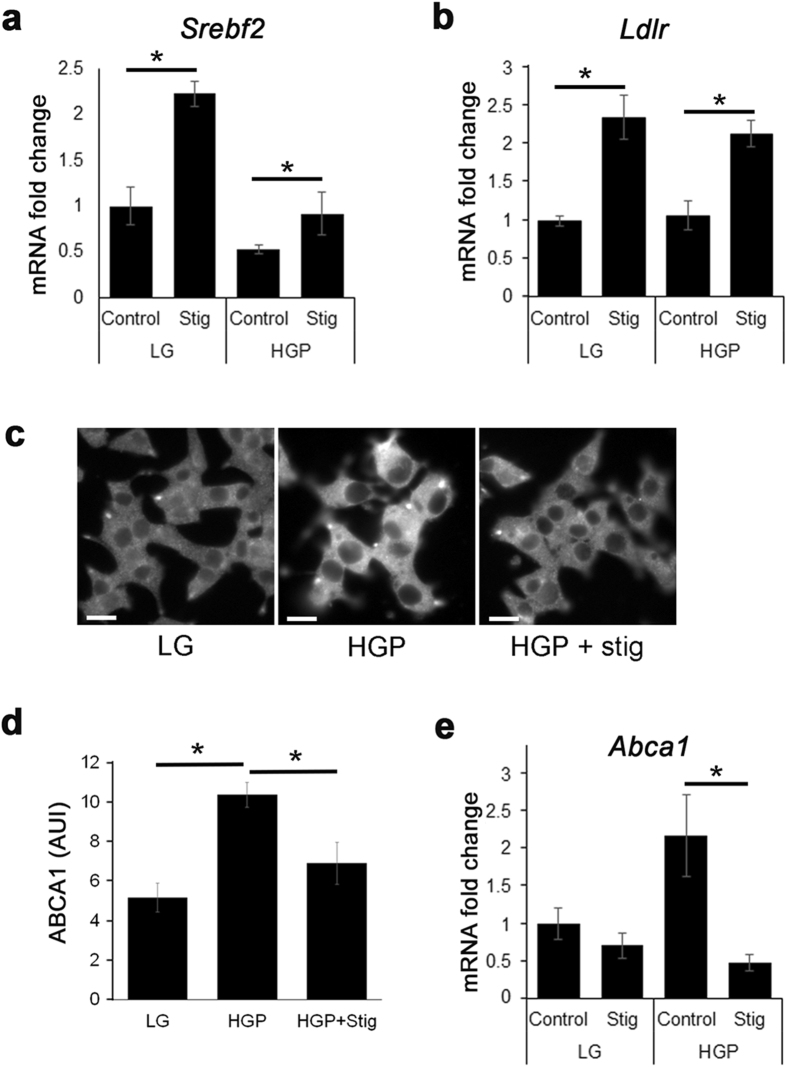
Stigmasterol alters expression of cholesterol homeostasis genes
Because different phytosterols have cell-type specific effects on cholesterol regulatory genes27, we examined whether stigmasterol influences genes associated with cholesterol homeostasis in β-cells. Genes involved in cholesterol regulation are under the control of sterol regulatory element-binding protein 2 (SREBP2). The activation of SREBP2 is well characterized and is highly regulated by intracellular cholesterol levels. Low cholesterol levels are sensed in the ER by SCAP, which chaperones SREBP2 to the Golgi apparatus, where SREBP2 is cleaved by proteases, and is transported to the nucleus. The transcription of the SREBP2 gene Srebf2 is under a feed forward mechanism, where the transcription of Srebf2 is increased by SREBP2 activation37. Stigmasterol has been shown to interfere with SREBP processing38, which may elicit a compensatory response in Srebf2 expression in stigmasterol-treated cells. As shown in Fig. 5a, the addition of stigmasterol to either LG or HGP treated INS-1 cells increased transcription of Srebf2 (Stig vs Control). An SREBP2 target gene Ldlr 39, responsible for cholesterol uptake from LDL, was similarly upregulated (Fig. 5b). HGP + Stig treated cells had decreased cholesterol efflux transporter ABCA1 when compared with HGP treatment at both the protein and transcriptional level (Fig. 5c–e). The exact mechanism that causes cholesterol genes to change in cells loaded with phytosterols is unknown. It has been shown that it is the accumulation of stigmasterol, rather than changes in the cholesterol level, that is responsible for altered expression of cholesterol homeostasis genes38.
Figure 5.
Stigmasterol promotes transcriptional changes associated with cholesterol homeostasis. INS-1 cells were incubated in LG or HGP, and treated with or without stigmasterol (Stig). (a,b) Transcription of Srebf-2 (a) and Ldlr (b) measured by RT-PCR. (c-e) Immunohistochemistry (c) and quantification of ABCA1 expression (d) and Abca1 transcription (e) levels under all conditions. Scale bars, 10 μm. *p < 0.05.
Stigmasterol improves β-cell function and reduces β-cell apoptosis
The direct effect of stigmasterol on β-cells is unclear. While Panda and colleagues reported a decrease in serum glucose accompanied by increased circulating insulin when stigmasterol was administered to mice36, others have shown no effect of stigmasterol feeding on glucose tolerance40. Glucolipotoxicity is known to induce β-cell death and reduce β-cell function41. We first examined the effect of stigmasterol on β-cell survival. External phosphatidylserine is a marker of early apoptosis, since phosphatidylserine is normally located on the inner leaflet of the plasma membrane, but is flipped to the outer membrane during apoptosis and necrosis42. Annexin V binds to phosphatidylserine; thus, increased annexin V staining is a measure of cell death. As shown in Fig. 6a, HGP treatment increased annexin V staining in INS-1 cells. The addition of stigmasterol partially blocked the increase in annexin V, indicating that stigmasterol prevents β-cell death due to glucolipotoxicity. Similar results were obtained with Western blotting of active caspase-3 (Supplementary Fig. 4), a marker for apoptosis43.
Figure 6.
Stigmasterol prevents early apoptosis and impaired insulin secretion due to HGP. (a) Annexin V staining of INS-1 cells treated with LG, HGP and HGP + stig, along with Hoechst staining for cell counting. Scale bars, 50 μm. (b) GSIS of INS-1 cells treated with LG, HGP and HGP + stig. Results are presented as the ratio of insulin secretion at 20 mM glucose to insulin secretion at 2 mM glucose. Data are pooled from six different experiments. *p < 0.05. (c) Total insulin from INS-1 cells treated with HGP and varying concentrations of stigmasterol, normalized to cells with no HGP treatment. *p < 0.05, HGP vs. HGP + Stig treatment.
In order to examine the direct effects of stigmasterol on β-cell function, static GSIS assays were performed. Addition of stigmasterol rescued GSIS in cells treated with HGP (Fig. 6b). Under this condition, stigmasterol also exerted a beneficial effect of increasing total insulin in HGP treated INS-1 cells (Fig. 6c). Together these data indicate that stigmasterol treatment can preserve β-cell function and survival in the presence of glucolipotoxicity.
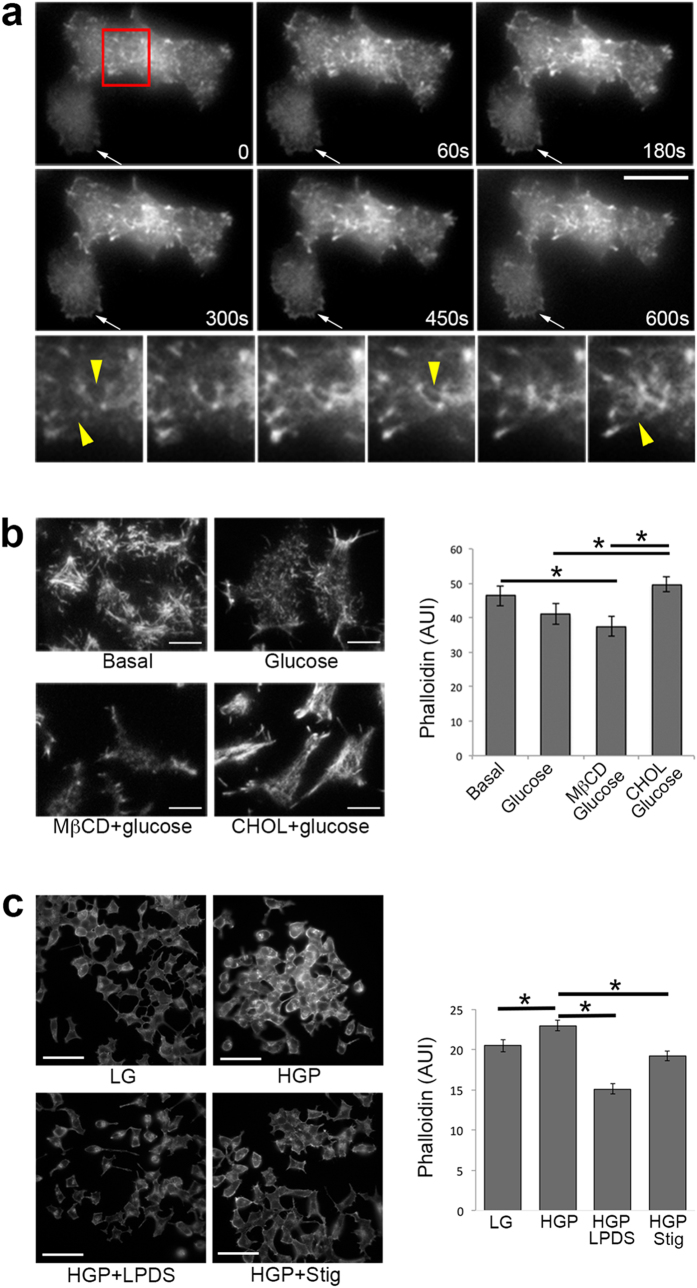
Stigmasterol rescues glucose-stimulated actin reorganization
Actin reorganization plays an essential role in glucose-stimulated insulin secretion. Pancreatic β-cells display a dense actin web below the plasma membrane that may inhibit granule docking. Glucose-stimulated actin reorganization serves to remove the F-actin barrier and permit access of granules to the plasma membrane. When this process is inhibited, GSIS is reduced44, 45. In the next series of experiments, we tested the hypothesis that glucolipotoxicity inhibits GSIS through promoting actin polymerization induced by excess cholesterol and that this process could be prevented by stigmasterol.
We previously showed that cholesterol overloading induces actin polymerization, leading to membrane protrusion, membrane ruffling, and cell expansion in cultured β-cells, suggesting a role of cholesterol in regulating cortical F-actin46. Here we extended our previous actin studies of fixed cells to live cell total internal reflection fluorescence microscopy (TIRFM) studies of real-time cortical actin dynamics in β-cells expressing actin-GFP. TIRFM was used to ensure that the focus was on cortical F-actin at the plasma membrane where insulin granule exocytosis took place. Within minutes after adding soluble cholesterol, formation of actin filaments was seen in both cells in Fig. 7a. Rapid actin polymerization occurred in the lower cell, evidenced especially by the thick actin ring around the rim (arrows). Enlarged images of the upper cell are presented in the bottom panels, which show that long actin filaments appeared from what were previously smaller fragments (arrowheads). This set of images provides evidence for a direct involvement of excess cholesterol in actin polymerization in cultured β-cells.
Figure 7.
Stigmasterol reverses HGP-mediated actin polymerization. (a) Real-time polymerization of actin-GFP at the plasma membrane in MIN6 cells exposed to cholesterol loading. TIRFM images were taken every 2 s. The time points refer to the time after adding soluble cholesterol (CHOL). The lower panels show enlarged images of the red-boxed region indicated in the first frame. The arrow points to a cell in which rapid actin polymerization took place, especially around the cell periphery. Scale bars, 10 μm. (b) Fluorescence imaging and quantification of F-actin labeled with phalloidin in cholesterol treated cells. “Basal” cells were starved in 2 mM glucose for 2 h; “Glucose” cells were incubated with 20 mM glucose for 15 min, “MβCD” cells were incubated with 5 mM MβCD at 37 °C for 1 h, and “CHOL” cells were incubated with 5 mM CHOL for 1 h at 37 °C. 20 mM glucose was added to the last 15 min of cholesterol treatment. Scale bars, 10 μm. *p < 0.05. (c) Fluorescence imaging and quantification of F-actin labeled with phalloidin in HGP treated cells. INS-1 cells were treated for 72 h with LG, HGP, HGP + LPDS or HGP + Stig. Scale bars, 50 μm. *p < 0.05.
To further confirm that cholesterol regulates actin reorganization upon glucose stimulation, a process that is critical for GSIS, cells were first cholesterol depleted (by MβCD) or overloaded (by soluble cholesterol, “CHOL”), then stimulated with 20 mM glucose, fixed and stained using phalloidin, a probe specific for polymerized F-actin47 (Fig. 7b). Compared with basal unstimulated cells, glucose-stimulated cells displayed slightly less F-actin staining, consistent with the idea that glucose stimulates actin reorganization to remove the F-actin barrier and thus to facilitate insulin release44, 45. Cholesterol overloaded cells stimulated with glucose (“CHOL”), on the other hand, had a mesh-like layer of F-actin network and significantly increased amount of F-actin, compared with untreated cells stimulated with glucose. Quantification of F-actin content under the four conditions is presented in Fig. 7b. These data show that cholesterol is actively involved in the actin reorganization process during glucose stimulation.
Finally, we examined phalloidin staining in HGP-treated cells with or without stigmasterol. HGP treatment significantly increased F-actin in INS-1 cells, which was normalized by stigmasterol treatment (Fig. 7c). Cholesterol depletion by LPDS, serving as a positive control for cholesterol-mediated actin dynamics, also reduced polymerized actin. The results from Fig. 7 support a model that the crucial step of glucose-stimulated actin depolymerization in GSIS is inhibited by glucolipotoxicity-induced cholesterol accumulation and that stigmasterol rescues GSIS at least partially by increasing actin dynamics in β-cells.
Discussion
The study presented here shows that stigmasterol protects pancreatic β-cells from glucolipotoxicity by preventing accumulation of free cholesterol and ROS, improving insulin secretion, increasing insulin content and decreasing markers for early apoptosis. We provide evidence that glucolipotoxicity stimulates ROS production, and that free radicals in turn promote cholesterol accumulation within β-cells. Stigmasterol treatment can normalize cellular cholesterol levels by reducing ROS production from glucolipotoxicity in β-cells. Indeed, stigmasterol can serve as a mild antioxidant or pro-oxidant to lipid peroxidation depending on the substrate48. Intraperitoneal injection of stigmasterol decreases lipid peroxidation and increases scavenger proteins in the livers of Ehrlich Ascites Carcinoma mice49. Stigmasterol did not increase Abca1 expression in INS-1 cells, indicating that stigmasterol may work differently in β-cells than in macrophages27.
It has long been recognized that Type 2 diabetes is associated with disordered lipid homeostasis, including increased VLDL and decreased HDL50. Thus, perturbations in circulating cholesterol may be a predisposing factor for type 2 diabetes. In agreement with these clinical findings, excess cholesterol and disrupted cholesterol export can promote β-cell dysfunction12, 51, 52. HMG-CoA reductase inhibitors (statins) are widely used to decrease serum cholesterol to prevent cardiovascular diseases. Several meta-analyses indicate, however, that statins may actually increase diabetes risk16–19. In vitro studies also suggest that statin treatment can negatively affect β-cells. Statins increase basal insulin secretion in MIN-6 cells, lowering the fold change in insulin secretion upon glucose stimulation53. Atorvastatin decreased insulin content in rat islets and INS-1 cells54. It should be noted that these in vitro studies were performed in systems with normal cholesterol levels. Cholesterol extraction using MβCD from LDLR−/− islets with elevated cholesterol reported an improvement in insulin secretion55. Therefore, depletion of β-cell cholesterol may be beneficial during times of cholesterol excess.
Studies on the link between statin usage and increased diabetes risk caution us against relying on statins to reduce cholesterol as a means to improve β-cell function under glucolipotoxicity. Few studies have focused on the effect of phytosterols on diabetes. Db/db mice represent a widely used animal model for obesity-induced diabetes. When they were fed Aloe Vera, they displayed decreased fasting blood glucose and HbA1c levels (a marker of blood glucose control) which were attributable to the phytosterol containing extracts56. Similarly, Zucker diabetic fatty rats exhibited increased glucose tolerance and decreased HbA1c levels when Aloe Vera derived phytosterols were administered orally57. Patients fed a phytosterol-enriched spread displayed a small, but significant, decrease in HbA1c levels58. One study looking at the effects of phytosterols on high fat fed mice reported that phytosterols did not improve glucose and insulin tolerance40, although β-cell function was not measured.
Cortical F-actin is dramatically increased in cholesterol-overloaded cells (Fig. 7), which could inhibit insulin granule exocytosis by several mechanisms. It may present a physical barrier, which impairs the ability of insulin granules to dock at the plasma membrane and reduces the size of the readily releasable pool of insulin granules. Indeed, an increase in the readily releasable pool of insulin granules has been suggested in cholesterol depleted cells59 and cholesterol overloading reduces the number of insulin granules docked at the plasma membrane60. Dense F-actin could restrict syntaxin 4 accessibility, which is required for insulin exocytosis61. Disruption of F-actin increases syntaxin 4 accessibility to VAMP2 by promoting dissociation of syntaxin 4 from F-actin, leading to increased GSIS62. Because cholesterol overloading results in cortical F-actin polymerization, it is likely that cholesterol alteration would interfere with the interaction between syntaxin 4 and F-actin, thereby affecting the required function of syntaxin 4 in GSIS. One potential mechanism for the involvement of stigmasterol in rescuing GSIS from HGP-treated β-cells is reducing the detrimental effect of excess cholesterol on glucose-stimulated actin reorganization.
In conclusion, our study shows beneficial effects of stigmasterol treatment on diabetic β-cells. Further studies will be needed to determine if oral intake of stigmasterol prevents β-cell dysfunction in diabetes.
Methods
Cell culture
INS-1 832/13 (INS-1) cells63 were cultured in RPMI-1640 supplemented with 10% fetal bovine serum (FBS), 100 U/ml penicillin, 100 μg/ml streptomycin, 10 mM HEPES, 2 mM L-glutamine, 1 mM sodium pyruvate, and 50 μM mercaptoethanol, at 37 °C in 5% CO2. MIN6 cells were grown in DMEM supplemented with 100 U/ml Penicillin, 100 µg/ml Streptomycin, 10% FBS, 2 mM L-glutamine and 50 µM 2-mercaptoethanol, at 37 °C in 5% CO2. Unless otherwise indicated, all experiments were performed using INS-1 cells. For cell culture treatments, INS-1 cells or human islets were incubated in normal growth media with 0.5% BSA (LG), growth media supplemented to a final concentration of 30 mM glucose, 0.5 mM palmitate-BSA complex (HGP), or HGP supplemented with stigmasterol (HGP + stig) for 72 h. For stigmasterol supplementation, stigmasterol stocks were made from stigmasterol powder (95%, Sigma) dissolved in 100% ethanol at a final concentration of 5 mg/ml. Unless otherwise stated, 50 μg/ml stigmasterol was used. Where indicated, 2,2′-Azobis(2-amidinopropane) dihydrochloride (AAPH) was dissolved in FBS-free RPMI media to indicated concentrations. Human islets were commercially obtained from InSphero (Zurich, Switzerland) and cultured according to manufacturer instructions.
Materials
Alexa546-phalloidin, lipidTOX red, actin-GFP and carboxy-H2DFFDA were from Thermo Fisher Scientific. AAPH was from Cayman Chemical. Rabbit anti-ABCA1 was from Novus Biologicals. Antibodies to active Caspase-3 and GAPDH were from Abcam. Filipin, mevinolin, N-acetyl-l-cysteine (NAC), MβCD, water-soluble cholesterol (CHOL) and all other chemicals were from Sigma. KRBH buffer (128.8 mM NaCl, 4.8 mM KCl, 1.2 mM KH2PO4, 1.2 mM MgSO4, 2.5 mM CaCl2, 5 mM NaHCO3, 10 mM HEPE, pH 7.4) was used for all experiments.
Palmitate/BSA complex preparation
Palmitate solution was prepared as described previously64 by making a 20 mM palmitate stock in 0.1 M NaOH and heating to 70 °C for 30 min. Palmitate stock was added to 10% BSA in RPMI-1640 for a final concentration of 4 mM palmitate complex and heated at 55 °C for 30 min with occasional shaking.
Cholesterol manipulation
Cholesterol depletion using methyl-β-cyclodextrin (MβCD) was done by incubating cells with 5 mM MβCD at 37 °C for 1 h; to cholesterol overload, cells were incubated with 5 mM soluble cholesterol (CHOL, 1 g contains approximately 40 mg cholesterol) at 37 °C for 1 h. LPDS treatment was done by culturing cells in normal growth medium with 10% FBS replaced by lipoprotein deficient serum (LPDS medium). Mevinolin treatment was done by including 1 μM mevinolin in LPDS medium. HDL treatment was done by including 50 μg/ml HDL in LPDS growth medium.
Glucose stimulated insulin secretion
Static glucose stimulated insulin secretion was measured as previously described65. Briefly, INS-1 cells were incubated in glucose-free RPMI-1640 culture medium for 2 h. Cells were starved for 1 h in glucose-free KRBH buffer. INS-1 cells were incubated in 2 mM glucose in KRBH for 1 h (basal samples), followed by 1 h in 20 mM glucose in KRBH (glucose-stimulated samples). Incubations were performed at 37 °C in an air incubator. Total insulin samples were taken after 1% Triton X-100 extraction. To measure the basal and stimulated insulin secretion separately, secreted insulin was normalized to total protein. Insulin samples were measured by insulin ELISA kits (Alpco Diagnostics).
Fluorescence Microscopy
Cells were grown in imaging dishes similar to MatTek dishes. Wide-field fluorescence microscopy utilized a Leica DMIRB microscope (Leica Mikroscopie und Systeme GmbH, 35578 Wetzlar, Germany) equipped with a Princeton Instruments (Princeton, NJ, USA) cooled charge coupled device (CCD) using MetaMorph Imaging System software (Molecular Devices). Images were acquired using an oil-immersion objective (×40). For filipin and lipidtox staining, INS-1 cells were fixed in 1% paraformaldehyde for 20 minutes then incubated in filipin (50 μg/ml) or lipidtox (1:1000 dilution) for 45 min. Filipin and lipidtox images were captured using UV and rhodamine filters, respectively. Details of filipin staining and imaging are described previously66. For carboxy-H2DFFDA fluorescence, INS-1 cells were incubated in 20 μM carboxy-H2DFFDA for 1 h. Cells were washed and counterstained with Hoechst 33342 to label the nuclei for cell counting. For phalloidin staining, cells were fixed with 4% paraformaldehyde for 20 min, permeabilized with 0.1% Triton X-100 for 5 min, and stained with Alexa 546-phalloidin. All staining was done at room temperature.
RT-PCR
Total RNA from INS-1 cells was extracted from tissues using the Purelink® RNA kit (Thermo Fisher Scientific). Total RNA (1 µg) was reverse transcribed using the SuperScript® Reverse Transcription system (Thermo Fisher Scientific). Real time PCR was performed on the cDNA on a Bio-Rad iCycler using SYBR green mastermix (Thermo Fisher Scientific). Thermal cycling conditions were: 95 °C for 5 min, (30 seconds 95 °C, 30 seconds 60 °C, 1 minute 52 °C) for 40 cycles, followed by a melt curve. Gene expression was expressed as the ratio between the expression of the target gene and GAPDH using the ΔΔCt method. Primers (Integrated DNA Technologies) used: Gapdh (forward 5′-actcccactcttccaccttc-3′, reverse 5′-tcttgctcagtgtccttgc-3′), Abca1 (forward 5′-aacagtttgtggcccttttg-3′, reverse 5′-agttccaggctggggtactt-3′), Ldlr (forward 5′-cagcctagaggggtaaactg-3′, reverse 5′-tagcataccatcagggcaag-3′), Srebf-2 (forward 5′-cgaactgggcgatggatgag-3′, reverse 5′-gacaaactgtagcatctcgtcg-3′).
TIRFM
Transient transfections were performed with Lipofectamine 2000 (Thermo Fisher Scientific) according to the manufacturer’s protocol and cells were cultured for 48 h prior to microscopy. Actin-GFP-expressing MIN6 cells grown in MatTek dishes were kept in an Air-therm (WPI) temperature-regulated environmental box at 37 °C throughout the imaging experiments. Cells were imaged for 2 min to establish basal baseline. A 10 × concentrated stock of soluble cholesterol (CHOL) was then added to the edge of the MatTek dish on the microscope stage. TIRFM was performed using an Olympus objective-type IX-70 inverted microscope fitted with a 60×/1.45 NA TIRFM lens (Olympus), controlled by Andor iQ software (Andor Technologies), and detected with a back-illuminated Andor iXon 897 EMCCD camera (512 × 512, 14 bit; Andor Technologies). The depth of the evanescent field was calculated to be 98 nm67.
Western blotting
Total cell lysates were prepared, and protein concentration was determined by BCA (Thermo Scientific). Samples were immunoblotted against active caspase 3 (1:1000) and GAPDH (1:2000) at 4 °C overnight. Secondary antibodies conjugated with HRP were incubated for 1 h at room temperature. The membranes were then developed by ECL (Thermo Scientific), according to the manufacturer’s instructions.
Image quantification and statistics
All images were analyzed using MetaMorph software (Molecular Devices). Images were background subtracted and either quantified as individual cells or whole fields normalized to cell counts. Unless otherwise indicated, each data point represents the average of three independent experiments. Data are presented as the mean ± SEM. Statistical significance was analyzed using unpaired Student’s t tests for comparison between two groups and one-way repeated measures ANOVA with Post-hoc comparisons using the Tukey HSD test for data from more than two groups, with p-values less than 0.05 deemed significant.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Electronic supplementary material
Acknowledgements
We would like to thank Frederik Lund for his help with the statistical analysis. This research was supported by funds from the United States Department of Agriculture grant 2016–67012–25207.
Author Contributions
M.G.W. and M.H. conceived the project, analyzed the data and wrote the manuscript. M.G.W., V.C.B., G.L. and M.H. performed the experiments. All authors reviewed the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-10209-0
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Global report on diabetes. Geneva (2016).
- 2.Diabetes Prevention Program Research Group Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sladek R, et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature. 2007;445:881–885. doi: 10.1038/nature05616. [DOI] [PubMed] [Google Scholar]
- 4.Morris AP, et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44:981–990. doi: 10.1038/ng.2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guh DP, et al. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health. 2009;9 doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poitout V, Robertson RP. Glucolipotoxicity: fuel excess and beta-cell dysfunction. Endocr Rev. 2008;29:351–366. doi: 10.1210/er.2007-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buteau J, et al. Glucagon-like peptide-1 prevents beta cell glucolipotoxicity. Diabetologia. 2004;47:806–815. doi: 10.1007/s00125-004-1379-6. [DOI] [PubMed] [Google Scholar]
- 8.Erion KA, Berdan CA, Burritt NE, Corkey BE, Deeney JT. Chronic Exposure to Excess Nutrients Left-shifts the Concentration Dependence of Glucose-stimulated Insulin Secretion in Pancreatic beta-Cells. J Biol Chem. 2015;290:16191–16201. doi: 10.1074/jbc.M114.620351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kondegowda NG, et al. Lactogens protect rodent and human beta cells against glucolipotoxicity-induced cell death through Janus kinase-2 (JAK2)/signal transducer and activator of transcription-5 (STAT5) signalling. Diabetologia. 2012;55:1721–1732. doi: 10.1007/s00125-012-2501-9. [DOI] [PubMed] [Google Scholar]
- 10.El-Assaad W, et al. Glucolipotoxicity alters lipid partitioning and causes mitochondrial dysfunction, cholesterol, and ceramide deposition and reactive oxygen species production in INS832/13 ss-cells. Endocrinology. 2010;151:3061–3073. doi: 10.1210/en.2009-1238. [DOI] [PubMed] [Google Scholar]
- 11.Brunham LR, et al. Beta-cell ABCA1 influences insulin secretion, glucose homeostasis and response to thiazolidinedione treatment. Nat Med. 2007;13:340–347. doi: 10.1038/nm1546. [DOI] [PubMed] [Google Scholar]
- 12.Hao M, Head WS, Gunawardana SC, Hasty AH. & Piston, D. W. Direct Effect of Cholesterol on Insulin Secretion: A Novel Mechanism for Pancreatic β-Cell Dysfunction. Diabetes. 2007;56:2328–2338. doi: 10.2337/db07-0056. [DOI] [PubMed] [Google Scholar]
- 13.Malmgren S, et al. Coordinate changes in histone modifications, mRNA levels, and metabolite profiles in clonal INS-1 832/13 beta-cells accompany functional adaptations to lipotoxicity. J Biol Chem. 2013;288:11973–11987. doi: 10.1074/jbc.M112.422527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peyot ML, et al. Beta-cell failure in diet-induced obese mice stratified according to body weight gain: secretory dysfunction and altered islet lipid metabolism without steatosis or reduced beta-cell mass. Diabetes. 2010;59:2178–2187. doi: 10.2337/db09-1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boslem E, et al. Alteration of endoplasmic reticulum lipid rafts contributes to lipotoxicity in pancreatic beta-cells. J Biol Chem. 2013;288:26569–26582. doi: 10.1074/jbc.M113.489310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones M, Tett S, Peeters GM, Mishra GD, Dobson A. New-Onset Diabetes After Statin Exposure in Elderly Women: The Australian Longitudinal Study on Women’s Health. Drugs Aging. 2017;34:203–209. doi: 10.1007/s40266-017-0435-0. [DOI] [PubMed] [Google Scholar]
- 17.Preiss D, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011;305:2556–2564. doi: 10.1001/jama.2011.860. [DOI] [PubMed] [Google Scholar]
- 18.Rajpathak SN, et al. Statin therapy and risk of developing type 2 diabetes: a meta-analysis. Diabetes Care. 2009;32:1924–1929. doi: 10.2337/dc09-0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sattar N, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010;375:735–742. doi: 10.1016/S0140-6736(09)61965-6. [DOI] [PubMed] [Google Scholar]
- 20.Henriksbo BD, et al. Fluvastatin causes NLRP3 inflammasome-mediated adipose insulin resistance. Diabetes. 2014;63:3742–3747. doi: 10.2337/db13-1398. [DOI] [PubMed] [Google Scholar]
- 21.Lau VW, Journoud M, Jones PJ. Plant sterols are efficacious in lowering plasma LDL and non-HDL cholesterol in hypercholesterolemic type 2 diabetic and nondiabetic persons. Am J Clin Nutr. 2005;81:1351–1358. doi: 10.1093/ajcn/81.6.1351. [DOI] [PubMed] [Google Scholar]
- 22.Thompson GR, Grundy SM. History and development of plant sterol and stanol esters for cholesterol-lowering purposes. Am J Cardiol. 2005;96:3d–9d. doi: 10.1016/j.amjcard.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 23.Abumweis, S. S., Barake, R. & Jones, P. J. Plant sterols/stanols as cholesterol lowering agents: A meta-analysis of randomized controlled trials. Food Nutr Res52 (2008). [DOI] [PMC free article] [PubMed]
- 24.Jones PJ, MacDougall DE, Ntanios F, Vanstone CA. Dietary phytosterols as cholesterol-lowering agents in humans. Can J Physiol Pharmacol. 1997;75:217–227. doi: 10.1139/y97-011. [DOI] [PubMed] [Google Scholar]
- 25.Fernandez ML, Vega-Lopez S. Efficacy and safety of sitosterol in the management of blood cholesterol levels. Cardiovasc Drug Rev. 2005;23:57–70. doi: 10.1111/j.1527-3466.2005.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 26.Alhazzaa R, Oen JJJ, Sinclair AJ. Dietary phytosterols modify the sterols and fatty acid profile in a tissue-specific pattern. J Funct Foods. 2013;5:829–837. doi: 10.1016/j.jff.2013.01.030. [DOI] [Google Scholar]
- 27.Sabeva NS, et al. Phytosterols differentially influence ABC transporter expression, cholesterol efflux and inflammatory cytokine secretion in macrophage foam cells. J Nutr Biochem. 2011;22:777–783. doi: 10.1016/j.jnutbio.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Behnke O, Tranum-Jensen J, van Deurs B. Filipin as a cholesterol probe. II. Filipin-cholesterol interaction in red blood cell membranes. Eur J Cell Biol. 1984;35:200–215. [PubMed] [Google Scholar]
- 29.Robertson RP, Harmon J, Tran PO, Tanaka Y, Takahashi H. Glucose toxicity in beta-cells: type 2 diabetes, good radicals gone bad, and the glutathione connection. Diabetes. 2003;52:581–587. doi: 10.2337/diabetes.52.3.581. [DOI] [PubMed] [Google Scholar]
- 30.Cutler RG, et al. Involvement of oxidative stress-induced abnormalities in ceramide and cholesterol metabolism in brain aging and Alzheimer’s disease. Proc Natl Acad Sci U S A. 2004;101:2070–2075. doi: 10.1073/pnas.0305799101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gesquiere L, Loreau N, Minnich A, Davignon J, Blache D. Oxidative stress leads to cholesterol accumulation in vascular smooth muscle cells. Free Radic Biol Med. 1999;27:134–145. doi: 10.1016/S0891-5849(99)00055-6. [DOI] [PubMed] [Google Scholar]
- 32.Pallottini V, et al. Age-related HMG-CoA reductase deregulation depends on ROS-induced p38 activation. Mech Ageing Dev. 2007;128:688–695. doi: 10.1016/j.mad.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Zawada AM, et al. SuperSAGE evidence for CD14 + + CD16 + monocytes as a third monocyte subset. Blood. 2011;118:e50–61. doi: 10.1182/blood-2011-01-326827. [DOI] [PubMed] [Google Scholar]
- 34.Takenaka Y, Miki M, Yasuda H, Mino M. The effect of alpha-tocopherol as an antioxidant on the oxidation of membrane protein thiols induced by free radicals generated in different sites. Arch Biochem Biophys. 1991;285:344–350. doi: 10.1016/0003-9861(91)90370-X. [DOI] [PubMed] [Google Scholar]
- 35.Wang CC, Chen F, Kim E, Harrison LE. Thermal sensitization through ROS modulation: a strategy to improve the efficacy of hyperthermic intraperitoneal chemotherapy. Surgery. 2007;142:384–392. doi: 10.1016/j.surg.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 36.Panda S, Jafri M, Kar A, Meheta BK. Thyroid inhibitory, antiperoxidative and hypoglycemic effects of stigmasterol isolated from Butea monosperma. Fitoterapia. 2009;80:123–126. doi: 10.1016/j.fitote.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J Clin Invest. 2002;109:1125–1131. doi: 10.1172/JCI0215593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang C, et al. Disruption of cholesterol homeostasis by plant sterols. J Clin Invest. 2004;114:813–822. doi: 10.1172/JCI22186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horton JD, et al. Activation of cholesterol synthesis in preference to fatty acid synthesis in liver and adipose tissue of transgenic mice overproducing sterol regulatory element-binding protein-2. J Clin Invest. 1998;101:2331–2339. doi: 10.1172/JCI2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calpe-Berdiel L, Escola-Gil JC, Rotllan N, Blanco-Vaca F. Phytosterols do not change susceptibility to obesity, insulin resistance, and diabetes induced by a high-fat diet in mice. Metabolism. 2008;57:1497–1501. doi: 10.1016/j.metabol.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Maedler K, et al. Distinct effects of saturated and monounsaturated fatty acids on beta-cell turnover and function. Diabetes. 2001;50:69–76. doi: 10.2337/diabetes.50.1.69. [DOI] [PubMed] [Google Scholar]
- 42.Vermes I, Haanen C, Steffens-Nakken H, Reutelingsperger C. A novel assay for apoptosis. Flow cytometric detection of phosphatidylserine expression on early apoptotic cells using fluorescein labelled Annexin V. J Immunol Methods. 1995;184:39–51. doi: 10.1016/0022-1759(95)00072-I. [DOI] [PubMed] [Google Scholar]
- 43.Nicholson DW, et al. Identification and inhibition of the ICE/CED-3 protease necessary for mammalian apoptosis. Nature. 1995;376:37–43. doi: 10.1038/376037a0. [DOI] [PubMed] [Google Scholar]
- 44.Thurmond DC, Gonelle-Gispert C, Furukawa M, Halban PA, Pessin JE. Glucose-stimulated insulin secretion is coupled to the interaction of actin with the t-SNARE (target membrane soluble N-ethylmaleimide-sensitive factor attachment protein receptor protein) complex. Mol Endocrinol. 2003;17:732–742. doi: 10.1210/me.2002-0333. [DOI] [PubMed] [Google Scholar]
- 45.Wilson JR, Ludowyke RI, Biden TJ. A redistribution of actin and myosin IIA accompanies Ca(2+)-dependent insulin secretion. FEBS Lett. 2001;492:101–106. doi: 10.1016/S0014-5793(01)02241-4. [DOI] [PubMed] [Google Scholar]
- 46.Hao M, Bogan JS. Cholesterol regulates glucose-stimulated insulin secretion through phosphatidylinositol 4,5-bisphosphate. J Biol Chem. 2009;284:29489–29498. doi: 10.1074/jbc.M109.038034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang ZJ, Haugland RP, You WM, Haugland RP. Phallotoxin and actin binding assay by fluorescence enhancement. Anal Biochem. 1992;200:199–204. doi: 10.1016/0003-2697(92)90299-M. [DOI] [PubMed] [Google Scholar]
- 48.Yoshida Y, Niki E. Antioxidant effects of phytosterol and its components. J Nutr Sci Vitaminol (Tokyo) 2003;49:277–280. doi: 10.3177/jnsv.49.277. [DOI] [PubMed] [Google Scholar]
- 49.Ghosh T, Maity TK, Singh J. Evaluation of antitumor activity of stigmasterol, a constituent isolated from Bacopa monnieri Linn aerial parts against Ehrlich Ascites Carcinoma in mice. Orient Pharm Exp Med. 2011;11:41–49. doi: 10.1007/s13596-011-0001-y. [DOI] [Google Scholar]
- 50.Reaven GM. Non-insulin-dependent diabetes mellitus, abnormal lipoprotein metabolism, and atherosclerosis. Metabolism. 1987;36:1–8. doi: 10.1016/0026-0495(87)90193-4. [DOI] [PubMed] [Google Scholar]
- 51.Ishikawa M, et al. Cholesterol accumulation and diabetes in pancreatic beta-cell-specific SREBP-2 transgenic mice: a new model for lipotoxicity. J Lipid Res. 2008;49:2524–2534. doi: 10.1194/jlr.M800238-JLR200. [DOI] [PubMed] [Google Scholar]
- 52.Kruit JK, et al. Loss of both ABCA1 and ABCG1 results in increased disturbances in islet sterol homeostasis, inflammation, and impaired beta-cell function. Diabetes. 2012;61:659–664. doi: 10.2337/db11-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ishikawa M, et al. Distinct effects of pravastatin, atorvastatin, and simvastatin on insulin secretion from a beta-cell line, MIN6 cells. J Atheroscler Thromb. 2006;13:329–335. doi: 10.5551/jat.13.329. [DOI] [PubMed] [Google Scholar]
- 54.Sun H, et al. Atorvastatin inhibits insulin synthesis by inhibiting the Ras/Raf/ERK/CREB pathway in INS-1 cells. Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000004906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Souza JC, et al. Cholesterol reduction ameliorates glucose-induced calcium handling and insulin secretion in islets from low-density lipoprotein receptor knockout mice. Biochim Biophys Acta. 2013;1831:769–775. doi: 10.1016/j.bbalip.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 56.Tanaka M, et al. Identification of five phytosterols from Aloe vera gel as anti-diabetic compounds. Biol Pharm Bull. 2006;29:1418–1422. doi: 10.1248/bpb.29.1418. [DOI] [PubMed] [Google Scholar]
- 57.Misawa E, et al. Administration of phytosterols isolated from Aloe vera gel reduce visceral fat mass and improve hyperglycemia in Zucker diabetic fatty (ZDF) rats. Obes Res Clin Pract. 2008;2:I–ii. doi: 10.1016/j.orcp.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 58.Lee YM, Haastert B, Scherbaum W, Hauner H. A phytosterol-enriched spread improves the lipid profile of subjects with type 2 diabetes mellitus–a randomized controlled trial under free-living conditions. Eur J Nutr. 2003;42:111–117. doi: 10.1007/s00394-003-0401-y. [DOI] [PubMed] [Google Scholar]
- 59.Xia F, et al. Disruption of pancreatic beta-cell lipid rafts modifies Kv2.1 channel gating and insulin exocytosis. J Biol Chem. 2004;279:24685–24691. doi: 10.1074/jbc.M314314200. [DOI] [PubMed] [Google Scholar]
- 60.Bogan JS, Xu Y, Hao M. Cholesterol accumulation increases insulin granule size and impairs membrane trafficking. Traffic. 2012;13:1466–1480. doi: 10.1111/j.1600-0854.2012.01407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Spurlin BA, Thurmond DC. Syntaxin 4 facilitates biphasic glucose-stimulated insulin secretion from pancreatic beta-cells. Mol Endocrinol. 2006;20:183–193. doi: 10.1210/me.2005-0157. [DOI] [PubMed] [Google Scholar]
- 62.Jewell JL, Luo W, Oh E, Wang Z, Thurmond DC. Filamentous actin regulates insulin exocytosis through direct interaction with Syntaxin 4. J Biol Chem. 2008;283:10716–10726. doi: 10.1074/jbc.M709876200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hohmeier HE, et al. Isolation of INS-1-derived cell lines with robust ATP-sensitive K + channel-dependent and -independent glucose-stimulated insulin secretion. Diabetes. 2000;49:424–430. doi: 10.2337/diabetes.49.3.424. [DOI] [PubMed] [Google Scholar]
- 64.Cousin SP, et al. Free fatty acid-induced inhibition of glucose and insulin-like growth factor I-induced deoxyribonucleic acid synthesis in the pancreatic beta-cell line INS-1. Endocrinology. 2001;142:229–240. doi: 10.1210/endo.142.1.7863. [DOI] [PubMed] [Google Scholar]
- 65.Gunawardana SC, Rocheleau JV, Head WS. & Piston, D. W. Mechanisms of time-dependent potentiation of insulin release: involvement of nitric oxide synthase. Diabetes. 2006;55:1029–1033. doi: 10.2337/diabetes.55.04.06.db05-1532. [DOI] [PubMed] [Google Scholar]
- 66.Maxfield FR, Wustner D. Analysis of cholesterol trafficking with fluorescent probes. Methods Cell Biol. 2012;108:367–393. doi: 10.1016/B978-0-12-386487-1.00017-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu Y, et al. Dual-mode of insulin action controls GLUT4 vesicle exocytosis. J Cell Biol. 2011;193:643–653. doi: 10.1083/jcb.201008135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).