Abstract
Purpose:
To compare the effects of different porcelain surface treatment methods on the shear bond strength (SBS) and fracture mode of orthodontic brackets.
Materials and Methods:
Seventy feldspathic porcelain disk samples mounted in acrylic resin blocks were divided into seven groups (n=10) according to type of surface treatment: I, Diamond bur; II, Orthosphoric acid (OPA); III, hydrofluoric acid (HFA); IV, sandblasted with aluminum oxide (SB); V, SB+HFA; VI, Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser; VII, Erbium:yttrium-aluminum-garnet (Er:YAG) laser. Brackets were affixed to treated all-porcelain surfaces with a silane bonding agent and adhesive resin and subjected to SBS testing. Specimens were evaluated according to the adhesive remnant index (ARI), and failure modes were assessed quantitatively under a stereomicroscope and morphologically under a scanning electron microscope (SEM). Statistical analysis was performed using one-way analysis of variance and the post-hoc Tukey test, with the significance level set at 0.05.
Results:
The highest SBS values were observed for Group V, with no significant difference between Groups V and III. SBS values for Group I were significantly lower than those of all other groups tested. The porcelain/resin interface was the most common site of failure in Group V (40%) and Group III (30%), whereas other groups showed various types of bond failure, with no specific location pre-dominating, but with some of the adhesive left on the porcelain surfaces (ARI scores 2 or 3) in most cases.
Conclusion:
The current findings indicate that a diamond bur alone is unable to sufficiently etch porcelain surfaces for bracket bonding. Moreover, SB and HFA etching used in combination results in a significantly higher shear-bond strength than HFA or SB alone. Finally, laser etching with either an Nd:YAG or Er:YAG laser was found to be more effective and less time-consuming than both HFA acid and SB for the treatment of deglazed feldspathic porcelain.
Keywords: Shear bond strength, sandblasting, Er:YAG, Nd:YAG
Introduction
Increases in the number of adults seeking orthodontic treatment has meant that the orthodontist is often faced with the challenge of effectively bonding orthodontic brackets to porcelain restorations (1, 2, 3). Because conventional orthodontic bonding systems do not guarantee a level of adhesion to porcelain that is sufficient to withstand orthodontic forces (4), a combination of mechanical and/or chemical conditioning methods is needed to increase the bond strength of orthodontic brackets to porcelain restorations (5). Until now, different surface treatment methods have been used, including sandblasting (SB), hydrofluoric acid application (HFA), orthosphoric acid (OPA) and laser etching. There are several advantages and disadvantages to each of these methods (4, 5). HFA etching has been shown to result in clinically acceptable bond-strength values, but the danger of acid burns must be considered. OPA has been found to be less successful in terms of bond strength than HFA due to an inability to erode superficial layers of silicate porcelain (6, 7, 8).
Conversely, diamond burs, which may also be used to roughen the porcelain surface, are known to reduce porcelain integrity. Zachrisson et al.(4) have promoted SB, a procedure that involves blasting aluminium-oxide particles onto the porcelain at high pressure to create a microretentive surface, whereas a combination of HFA and SB was found to be a more time-consuming and material-consuming procedure. Laser irradiation has also been mentioned as a promising technique for the surface treatment of porcelain (6, 9) and a number of studies have investigated the effects of Nd:YAG laser etching and Er:YAG laser etching and compared these to other commonly used etching methods. Poosti et al.(9) demonstrated laser irradiation with an Nd:YAG laser to be an acceptable substitute for HFA, whereas an Er:YAG laser was not considered acceptable due to low bond strengths. Similarly, Topcuoglu (10) reported that Er:YAG laser application could not successfully etch porcelain surfaces, and Pich et al.(11) stated that Er:YAG laser cannot be used with dental porcelain because it does not change the chemical composition of dental porcelain surfaces.
There is currently no consensus in the literature regarding the best surface conditioning method for producing an optimal bond strength between orthodontic brackets and porcelain restorations, with differences in storage conditions one of the critical factors in the confusion among study findings. Therefore, the present study was conducted to identify the outcomes of 7 different surface-conditioning methods (diamond bur, orthosphoric acid, hydrofluoric acid, sandblasting, sandblasting+hydrofluoric acid, Nd:YAG laser, Er:YAG laser) in terms of shear-bond strength (SBS) of metal orthodontic brackets to all porcelain (feldspathic) restorative material and bond failure mode.
Materials and Methods
Specimen Preparation
70 feldspathic porcelain discs (Noritake super porcelain EX-3, Noritake Co., Inc., Nagoya, Japan) with a diameter of 6 mm and a thickness of 3 mm were fabricated and glazed according to the manufacturer’s recommendations (Figure 1). Discs were viewed under a stereomicroscope (EMZTR, Meji Techno Co.,Ltd.,Japan) at 20x magnification to ensure that the flattened surfaces were free from defects such as cracks, pits and fissures. Discs were randomly divided into seven groups (n=10) according to surface conditioning methods, as follows: Group I (DB): Mechanical roughening and deglazing was performed with a cylindrical diamond bur (30 m, Brasseler, Lemgo, Germany) rotated at 40,000 rpm for 3 seconds with the shaft parallel to the sample. Samples were rinsed thoroughly to remove debris and air-dried. Group II (OPA): After roughening and deglazing the porcelain surfaces with a diamond bur as described above, samples were then etched for 2 minutes with 37% orthophosphoric acid (OPA, etching solution, ORMCO, Orange, CA, USA), washed under water for 20 seconds and air-dried. Group III (HFA): After roughening and deglazing the porcelain surfaces with a diamond bur as described above, samples were then etched for 2 minutes with 9.6% hydrofluoric acid gel (HFA, 9.6%, Vita Ceram Etch, Bad Sackingen, Germany) washed under water for 20 seconds and air-dried. Group IV (SB): Samples were sandblasted with a micro-etcher (Micro-Etcher ERC II, Danville Engineering, San Ramon, California, USA) using 50 μm aluminium oxide particles at 60 psi for 3 seconds, with the sandblasting apparatus (Microetcher II, Danville Engineering, San Ramon, California, USA) directed perpendicular to the porcelain surface at a distance of 10 mm. Samples were then washed with water for 20 seconds and air-dried. Group V (SB+HFA): Sandblasting was performed (as described above), followed by HFA etching (as described above). Group VI (Nd:YAG): After roughening and deglazing the porcelain surfaces with a diamond bur as described above, samples were irradiated using an Nd:YAG laser, (Figure 2, Fotona, Ljubljana, Slovenia) with a wavelength of 1064nm (300 μm fiber), 2W power and frequency of 10 Hz for 10 seconds in pulse mode (100μs) using a sweeping motion at approximately 2mm distance from the porcelain surfaces (Figure 3). Group VII (Er.YAG): Samples were treated with laser irradiation as described above for Group VI, but with an Er:YAG laser (2W, 10 Hz, 10 seconds. 2mm (Figure 3).
Figure 1, 2 and 3.

From left to right: An example of porcelain disc, the laser system used in the study and laser treatment of porcelain surface.
Bonding Procedure
Porcelain samples were embedded in acrylic resin blocks, with the smooth surfaces left exposed for bonding. Stainless steel brackets (Rocky Mountain Denver, CO, USA) with approximately the same shape and adhesion area (height: 2mm, base area: 3.5x2.0 mm) as those used for maxillary premolars were used in this study. A silane bonding agent was applied to the exposed porcelain surfaces (Ortho Solo Sealant, Ormco, Orange, CA, USA) and air-thinned, after which an adhesive resin (Enlight Light Cure Adhesive, Ormco, Orange, CA, USA) was prepared and applied to the porcelain surfaces according to the manufacturer’s instructions. Excess resin was removed with an explorer. Samples were light cured for 40s (Demetron LC, SDS Kerr; light output: 400 mW/cm2), stored in deionized water at 37°C for 24 hours, and thermocycled in water baths at 5°C and 55°C (30-second cycles, total 500 cycles) to simulate temperature and humidity conditions of the oral cavity. Samples were then stored at room temperature in distilled water for 1 week until SBS testing.
Shear Bond Strength Testing
Shear bond strength was evaluated using a universal testing machine (Shimadzu AG-X, Tokyo, Japan) operating at a speed of 0.5 mm/min. A knifeedged shearing blade was secured on the crosshead with the direction of force parallel to the labial surface and the bracket interface, and the shearing blade struck flush against the edge of the base without touching the porcelain. Values obtained in Newtons (N) were converted into megapascals (MPa) by dividing the value of N by the surface area of the bracket base. After debonding, each sample was examined under a stereomicroscope (Olympus SZ61; Olympus Optical Co, Tokyo, Japan) at 10x magnification to identify the location of bond failure. The residual composite remaining on the premolar was assessed using the Adhesive Remnant Index (ARI), which scores each sample according to the amount of material remaining on the porcelain surface, as follows: 0, no adhesive remaining; 1, less than 50% of the adhesive remaining; 2, more than 50% of the adhesive remaining; 3, all of the adhesive remaining on the porcelain surface, with a distinct impression of the bracket base.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences, Windows v. 10.0.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics including means, standard deviations and minimum and maximum values were calculated for each group. A Kolmogorov-Smirnov normality test was applied and showed normality of distribution; thus, one-way analysis of variance (ANOVA) and post-hoc Tukey tests were used to identify differences in SBS among groups with the level of significance set at p<0.05.
Results
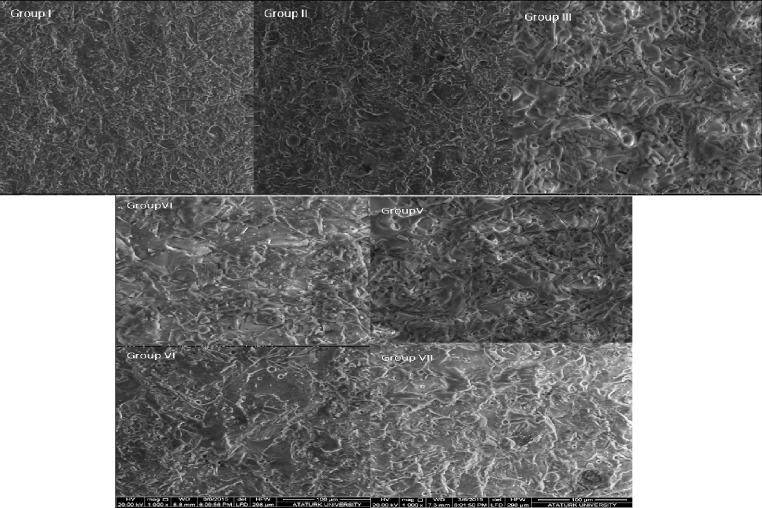
Group V (SB+HFA) showed the highest SBS values, and Group I (DB) showed the lowest SBS values (Figure 4). ARI scores were: 0, indicating no adhesive; 1, less than half of the adhesive; 2, more than half of the adhesive; and 3, all the adhesive. Mean shear test values for each group were as follows: I, 3.49±0.75; II, 6.18±1.98; III, 11.19±0.92; IV, 10.75±1.61; V, 12.27±1.63; VI,9.48±1.16 VII, 7.82±1.49 (Table 1). One-way analysis of variance showed significant differences among groups (Table 2; p<0.05). Multiple paired comparisons (Tukey test) showed Groups III (HFA) and V to have significantly higher bond strengths than the other groups and Group I to have statistically lower bond strengths than the other groups. No significant differences were found between the SBS values of Groups II and VII; Groups VI and VII; Groups VI and IV; Groups III and IV; or Groups III and V (p>0.05). The distribution of failure modes, as expressed by ARI scores, is given in Table 3. The porcelain/resin interface was the most common site of failure in Groups V (40%) and III (30%), whereas the other groups showed a range of failures, most of which involved some or all of the adhesive remaining on the porcelain surfaces (ARI Scores 2 or 3). SEM evaluation of debonded samples showed differences in the surface characteristics of the porcelain disks by treatment group (Figure 5), which may be described as follows: Group I (DB): uniform peeling or erosion, with deep grooves in the porcelain surface; Group II (OPA): relatively smooth surfaces with little or no damage; Group III (HFA): a relatively homogenous pattern with small fissures, micro-cracks, and profound penetration of HFA, removal of the crystalline phase and glass matrix; Group IV (SB): shallow surface erosion; Group V (SB+HPA): visibly rougher surfaces than the other groups, with greater penetration and undercuts; Group VI (Nd:YAG): rough, umbilicate, craterlike structures; Group VII (Er:YAG): rough, umbilicate, craterlike structures.
Figure 4.
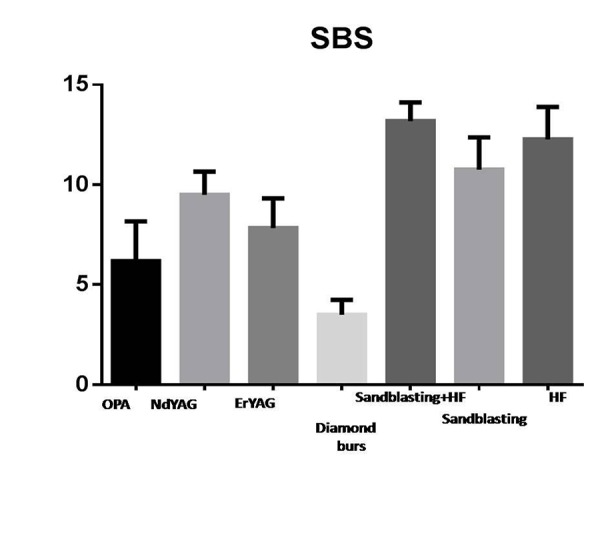
Shear Bond Strengths (SBS) values for groups.
Table 1.
Descriptive statistics for groups.
| 95% Confidence Interval for Mean | |||||||
|---|---|---|---|---|---|---|---|
| SBS(MPa) | n | Mean±Std.Dev. | Std. Error | Lower Bound | Upper Bound | Min.(MPa) | Max.(MPa) |
| Group I | 10 | 3.498±0.75 | .7516 | 2.960 | 4.036 | 1.62 | 4.32 |
| Group II | 10 | 6.182±1.98 | .6264 | 4.765 | 7.599 | 3.71 | 10.73 |
| Group III | 10 | 11.19±0.92 | .2940 | 12.52 | 13.85 | 11.89 | 14.53 |
| Group IV | 10 | 10.75±1.61 | .5101 | 9.596 | 11.90 | 7.89 | 13.01 |
| Group V | 10 | 12.27±1.63 | .5159 | 11.10 | 13.44 | 9.89 | 14.08 |
| Group VI | 10 | 9.489±1.16 | .3695 | 8.653 | 10.32 | 7.61 | 11.25 |
| Group VII | 10 | 7.829±1.49 | .4718 | 6.762 | 8.896 | 5.96 | 10.40 |
Table 2.
Multiple comparison testing for groups.
| SBS(MPa) | Group I | Group II | Group III | Group IV | Group V | Group VI | Group VII |
|---|---|---|---|---|---|---|---|
| Group I | - | *** | **** | **** | **** | **** | **** |
| Group II | *** | - | **** | **** | **** | **** | ns |
| Group III | **** | **** | - | ** | ns | **** | **** |
| Group IV | **** | **** | ** | - | ns | ns | **** |
| Group V | **** | **** | ns | ns | - | *** | **** |
| Group VI | **** | **** | **** | ns | *** | - | ns |
| Group VII | **** | ns | **** | **** | **** | ns | - |
ns:Not significant, ***: p<0.001, ****:p<0.0001
Table 3.
Frequency distribution and the results of the ARI scores.
| Groups | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| I | 1 | 7 | 2 | - |
| II | 1 | 6 | 3 | - |
| III | - | 4 | 3 | 3 |
| IV | - | 4 | 4 | 2 |
| V | - | 3 | 3 | 4 |
| VI | - | 2 | 6 | 2 |
| VII | - | 3 | 5 | 2 |
ARI scores were: 0, indicating no adhesive; 1, less than half of the adhesive; 2, more than half of the adhesive; and 3, all the adhesive.
Figure 5.
Scanning electron photomicrographs of seven groups.
Discussion
As the demand for adult orthodontic treatment increases and the popularity of esthetic dentistry grows, orthodontists are often faced with the challenge of bonding attachments on teeth that have been restored with porcelain restorations (11, 12). Not only does bond strength need to be high enough to resist accidental debonding during treatment, it must also be low enough so that debonding at the end of orthodontic treatment requires minimal force to avoid harming restorations, which generally remain in the mouth after orthodontic treatment is complete (8).
Deglazing of porcelain before orthodontic bonding remains a controversial issue. Whereas studies have shown that a satisfactory bond strength can be achieved with glazed ceramic, several studies have advocated removal of the glaze to allow for better mechanical retention by the adhesive agent (13, 14, 15). Zachrisson et al.(4) have explained that felspathic porcelains may sometimes have an alumina overglaze that is difficult to identify, but which renders silane ineffective, as it is only able to enhance bonding to porcelains containing significant amounts of silica. In such cases, careful removal of the glaze in the area of the bonding will increase the surface area available for both chemical and mechanical retention. Deglazing has also been shown to enable laser light to produce microscopic porosities through a process of thermomechanical ablation, thereby increasing micromechanical retention between the resin composite and the porcelain surface (13, 14). In this study, the porcelain surfaces were deglazed in order to increase micromechanical retention.
Roughening of the porcelain surface may reduce the strength of the porcelain restoration and increase the rate of plaque accumulation, causing gingival inflammation and other adverse soft-tissue reactions (8). Some surface-treatment methods currently recommended for porcelain are both time-consuming and potentially harmful to soft tissue (16). Because restorations ordinarily remain in the mouth following orthodontic treatment, roughening during surface treatment needs to be kept to a minimum (17); however, some degree of mechanical or chemical roughening is required to obtain a viable bond between bracket and porcelain (8, 17, 18). For these reasons, this study examined the effects of seven different types of porcelain surface treatment methods on bracket bond strength. With the exception of Group I, which had SBS values of 3.12±0.67 MPa, indicating mechanical roughening with a diamond bur to be unable to produce SBS values suitable for clinical usage, all the surface preparation techniques evaluated in the current study resulted in SBS values that were clinically acceptable (6.182±1.98 - 12.27±1.63 MPa).
In fact, the literature includes few scientifically based recommendations for minimum orthodontic bracket shear bond strength. Whitlock et al.(7) suggested that 6-8 MPa was strong enough to maintain orthodontic attachments through the course of treatment, but weak enough to preserve the integrity of the porcelain restoration following bracket removal. Thurmond et al.(18) reported that increasing the SBS to 13 MPa increased the probability of cohesive fractures in the porcelain substrate. In the present study, all SBS values were below 13 MPa, and no porcelain fractures were observed. Findings regarding failure modes were in line with those of bond-strength testing in that increased resistance to debonding decreased the likelihood of bond failure at the toothadhesive interface and increased the likelihood of failure at the bracket-adhesive interface. Thus, HFA etching combined with sandblasting (Group V), which resulted in a higher SBS than both HFA and laser etching alone, also left more adhesive remaining on the tooth surface (as expressed by higher ARI scores) than the use of a diamond bur, acid etching, and laser etching alone.
The main reason behind the use of HFA etching is to improve the shear bond strength of brackets to porcelain. When treated with HFA, feldspathic porcelain surfaces exhibit uniformly distributed pores and shallow irregularities caused by the preferential reaction between the HFA and the silica component of the porcelain (1). While HFA etching has been presented as an effective surface treatment method that offers ease of chair-side usage in addition to its satisfactory SBS results (8), many clinicians prefer not to use HFA because of the great care required during intraoral application to avoid soft-tissue damage (19).
As one of the most commonly used methods for dissolving superficial layers of porcelain, HFA etching is frequently used when comparing bond strengths of different porcelain surface-treatment methods (8). This study found the bond strength of SB (10.75±1.61 MPa) to be comparable to that of HFA etching (11.19±0.92 MPa); moreover, the combination of SB and HFA yielded a higher bond strength (12.27±1.63 MPa) than HFA etching alone, although the difference was not statistically significant (p>0.05). Kocadereli et al.(20) found porcelain surface preparation with HFA etching followed by the application of a silane bonding agent resulted in higher tensile bond strengths, and the same study as well as several others (7, 20, 21, 22, 23, 24, 25) reported higher shear bond strengths with HFA etching followed by the application of a silane bonding agent when compared to sandblasting and HFA used without silane. In contrast, Schmage et al.(26) found no significant difference in bond strengths between HFA used with silane and HFA alone. Two previous studies (27, 28) found sandblasting prior to HFA and silane application did not significantly increase bond strengths. Moreover, Zachrisson (8) reported brackets applied to sandblasted porcelain after silane application had bond strengths that were not clinically acceptable and suggested abandoning this technique. Harari et al.(22) reported considerably higher tensile bond strength with HFA than microetching with aluminium oxide particles. The contradictory results may be explained by differences in storage conditions, bonding agents and porcelain types among studies.
The present study found higher bond strengths with HFA than with 37% OPA. This is in line with some previous studies (17, 29, 30, 31, 32, 33, 34); however, others have reported no significant differences in bond strength between HFA and OPA (29, 30, 31, 34). Importantly, despite the good bond strength produced with HFA, in clinical practice, great care is required to ensure adequate isolation in order to protect oral tissue from HFA’s toxic effects.
Although the use of lasers in etching enamel surfaces has been previously reported (35), the effect of laser etching on porcelain surfaces has been less extensively examined (36, 37). Er: YAG and Nd:YAG lasers have been suggested as possible alternatives to HFA application for porcelain treatment for a number of reasons (38, 39, 40). Whereas HFA acid needs to remain on the porcelain surface for a relatively long time (about 2 min) and requires extreme care to avoid soft-tissue irritation, lasers are applied for a relatively short time (10 s) and require no rinsing and drying of surfaces and no rubber dam for isolation (although procedures should be performed with standard safety equipment, such as protective glasses). However, the high energy required for surface modification with Nd:YAG laser etching may produce cracks throughout the porcelain surfaces that can decrease fracture resistance (9, 12, 15, 38).
Previous studies have shown 9.6% HFA and Nd:YAG laser treatment to produce SBS in an acceptable range for orthodontic treatment (9, 41). Li et al.(41) conditioned porcelain with Nd:YAG at 0.6, 0.9 and 1.2W and concluded this type of laser used in combination with light-curing composite promotes acceptable bond strength to porcelain. Poosti et al.(9) showed Nd:YAG laser to be an acceptable substitute for HFA, while Er:YAG laser at the power and duration tested was not a suitable option (9). In contrast, Yassae et al.(42) found Er:YAG laser (1.6 W, 7.88 MPa) was an appropriate choice for bonding brackets to porcelain surfaces, with acceptable bond strength and minimal surface damage when compared to other conditioning methods such as 9.6% HF, and Er:YAG lasers of 2 and 3.2 W, respectively. Sohn (43) and Akova et al.(44) showed that the conventional techniques of HFA and silane, sandblasting and silane, OPA and silane, and HFA alone had higher bond strength than laser etching and silane. However, in line with the present study, bond strength following laser treatment was significantly higher than following OPA treatment. CO2 laser irradiation (2W/20-second superpulse) has also been found to provide acceptable bond strength of metal brackets to porcelain surfaces (44). In the present study, both Nd:YAG and Er:YAG laser treatment (Groups VI,VII) resulted in SBS values that were acceptable for clinical usage, and no cracks were observed in the porcelain surfaces, most likely because of the relatively low output power used (2W).
This study has a number of limitations worth mentioning. First, a major drawback common to all in vitro bond strength studies is the difficulty in simulating the complex nature of the oral environment in the laboratory. Factors such as variations in temperature, stresses, humidity, acidity and plaque all have an affect on bond strength in a way that is impossible to reproduce in vitro. Second, the present study was conducted with a small sample size. Future studies are required with larger sample sizes and different types of lasers.
Conclusion
Within the limitations of this study, the following conclusions can be drawn: 1) A diamond bur alone is incapable of etching porcelain surfaces for successful bonding to orthodontic brackets; 2) Treating porcelain surfaces with a combination of sandblasting and hydrofluoric acid etching results in a significantly higher shear bond strength than hydrofluoric acid etching or sandblasting alone; 3)Etching of deglazed feldspathic porcelain with either Nd:YAG or Er:YAG lasers is a more effective and time-saving alternative to hydrofluoric acid or sandblasting alone. Further studies are required to determine the efficacy of lasers in preparing other types of porcelain for composite. Other aspects of laser-etching that need clarification through additional research include the amount of heat absorbed by underlying tissue and the durability of the bond after long-term water storage and thermocycling.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Al-Hity R, Gustin MP, Bridel N, Morgon L, Grosgogeat B. In vitro orthodontic bracket bonding to porcelain. Eur J Orthod. 2012;34(4):505–511. doi: 10.1093/ejo/cjr043. [DOI] [PubMed] [Google Scholar]
- 2.Bishara SE, VonWald L, Olsen ME, Laffoon JF. Effect of time on the shear bond strength of glass ionomer and composite orthodontic adhesives. Am J Orthod Dentofacial Orthop. 1999;116(6):616–620. doi: 10.1016/s0889-5406(99)70195-2. [DOI] [PubMed] [Google Scholar]
- 3.Pannes DD, Bailey DK, Thompson JY, Pietz DM. Orthodontic bonding to porcelain: A comparison of bonding systems. J Prosthet Dent. 2003;89(1):66–69. doi: 10.1067/mpr.2003.63. [DOI] [PubMed] [Google Scholar]
- 4.Zachrisson BU. Orthodontic bonding to artificial tooth surfaces: Clinical versus laboratory findings. Am J Orthod Dentofacial Orthop. 2000;117(5):592–594. doi: 10.1016/s0889-5406(00)70211-3. [DOI] [PubMed] [Google Scholar]
- 5.Gillis I, Redlich M. The effect of different porcelain conditioning techniques on shear bond strength of stainless steel brackets. Am J Orthod Dentofacial Orthop. 1998;114(4):387–392. doi: 10.1016/s0889-5406(98)70183-0. [DOI] [PubMed] [Google Scholar]
- 6.Bourke BM, Rock WP. Factors affecting the shear bond strength of orthodontic brackets to porcelain. Br J Orthod. 1999;26(4):285–290. doi: 10.1093/ortho/26.4.285. [DOI] [PubMed] [Google Scholar]
- 7.Whitlock 3rd BO, Eick JD, Ackerman RJ, Glaros AG, Chappell RP. Shear strength of ceramic brackets bonded to porcelain. Am J Orthod Dentofacial Orthop. 1994;10(4):358–364. doi: 10.1016/S0889-5406(94)70056-7. [DOI] [PubMed] [Google Scholar]
- 8.Zachrisson YO, Zachrisson BU, Buyukyilmaz T. Surface preparation for orthodontic bonding to porcelain. Am J Orthod Dentofacial Orthop. 1996;109(4):420–430. doi: 10.1016/S0889-5406(96)70124-5. [DOI] [PubMed] [Google Scholar]
- 9.Poosti M, Jahanbin A, Mahdavi P, Mehrnoush S. Porcelain conditioning with nd:Yag and er:Yag laser for bracket bonding in orthodontics. Lasers Med Sci. 2012;27(2):321–324. doi: 10.1007/s10103-010-0878-6. [DOI] [PubMed] [Google Scholar]
- 10.Topcuoglu T, Oksayan R, Topcuoglu S, Coskun ME, Isman NE. Effect of er:Yag laser pulse duration on shear bond strength of metal brackets bonded to a porcelain surface. Photomed Laser Surg. 2013;31(6):240–246. doi: 10.1089/pho.2012.3463. [DOI] [PubMed] [Google Scholar]
- 11.Pich O, Franzen R, Gutknecht N, Wolfart S. Laser treatment of dental ceramic/cement layers: Transmitted energy, temperature effects and surface characterisation. Lasers Med Sci. 2015;30(2):591–597. doi: 10.1007/s10103-013-1340-3. [DOI] [PubMed] [Google Scholar]
- 12.Nattrass C, Sandy JR. Adult orthodontics-a review. Br J Orthod. 1995;22(4):331–337. doi: 10.1179/bjo.22.4.331. [DOI] [PubMed] [Google Scholar]
- 13.Kao EC, Boltz KC, Johnston WM. Direct bonding of orthodontic brackets to porcelain veneer laminates. Am J Orthod Dentofacial Orthop. 1988;94(6):458–468. doi: 10.1016/0889-5406(88)90003-0. [DOI] [PubMed] [Google Scholar]
- 14.Lacy AM, LaLuz J, Watanabe LG, Dellinges M. Effect of porcelain surface treatment on the bond to composite. J Prosthet Dent. 1988;60(3):288–291. doi: 10.1016/0022-3913(88)90270-3. [DOI] [PubMed] [Google Scholar]
- 15.Smith GA, McInnes-Ledoux P, Ledoux WR, Weinberg R. Orthodontic bonding to porcelain--bond strength and refinishing. Am J Orthod Dentofacial Orthop. 1988;94(3):245–252. doi: 10.1016/0889-5406(88)90034-0. [DOI] [PubMed] [Google Scholar]
- 16.Hayakawa T, Horie K, Aida M, Kanaya H, Kobayashi T, Murata Y. The influence of surface conditions and silane agents on the bond of resin to dental porcelain. Dent Mater. 1992;8(4):238–240. doi: 10.1016/0109-5641(92)90092-Q. [DOI] [PubMed] [Google Scholar]
- 17.Cochran D, O’Keefe KL, Turner DT, Powers JM. Bond strength of orthodontic composite cement to treated porcelain. Am J Orthod Dentofacial Orthop. 1997;111(3):297–300. doi: 10.1016/S0889-5406(97)70188-4. [DOI] [PubMed] [Google Scholar]
- 18.Thurmond JW, Barkmeier WW, Wilwerding TM. Effect of porcelain surface treatments on bond strengths of composite resin bonded to porcelain. J Prosthet Dent. 1994;72(4):355–359. doi: 10.1016/0022-3913(94)90553-3. [DOI] [PubMed] [Google Scholar]
- 19.Barbosa VL, Almeida MA, Chevitarese O, Keith O. Direct bonding to porcelain. Am J Orthod Dentofacial Orthop. 1995;107(2):159–164. doi: 10.1016/s0889-5406(95)70131-1. [DOI] [PubMed] [Google Scholar]
- 20.Kocadereli I, Canay S, Akca K. Tensile bond strength of ceramic orthodontic brackets bonded to porcelain surfaces. Am J Orthod Dentofacial Orthop. 2001;119(6):617–620. doi: 10.1067/mod.2001.113655. [DOI] [PubMed] [Google Scholar]
- 21.Chung CH, Brendlinger EJ, Brendlinger DL, Bernal V, Mante FK. Shear bond strengths of two resin-modified glass ionomer cements to porcelain. Am J Orthod Dentofacial Orthop. 1999;115(5):533–535. doi: 10.1016/S0889-5406(99)70275-1. [DOI] [PubMed] [Google Scholar]
- 22.Harari D, Shapira-Davis S, Gillis I, Roman I, Redlich M. Tensile bond strength of ceramic brackets bonded to porcelain facets. Am J Orthod Dentofacial Orthop. 2003;123(5):551–554. doi: 10.1067/mod.2003.S0889540602569134. [DOI] [PubMed] [Google Scholar]
- 23.Huang TH, Kao CT. The shear bond strength of composite brackets on porcelain teeth. Eur J Orthod. 2001;23(4):433–439. doi: 10.1093/ejo/23.4.433. [DOI] [PubMed] [Google Scholar]
- 24.Kao EC, Johnston WM. Fracture incidence on debonding of orthodontic brackets from porcelain veneer laminates. J Prosthet Dent. 1991;66(5):631–637. doi: 10.1016/0022-3913(91)90443-Z. [DOI] [PubMed] [Google Scholar]
- 25.Wood DP, Jordan RE, Way DC, Galil KA. Bonding to porcelain and gold. Am J Orthod. 1986;89(3):194–205. doi: 10.1016/0002-9416(86)90032-1. [DOI] [PubMed] [Google Scholar]
- 26.Schmage P, Nergiz I, Herrmann W, Ozcan M. Influence of various surface-conditioning methods on the bond strength of metal brackets to ceramic surfaces. Am J Orthod Dentofacial Orthop. 2003;123(5):540–546. doi: 10.1067/mod.2003.S0889540602569110. [DOI] [PubMed] [Google Scholar]
- 27.Jochen DG. Repair of fractured porcelain denture teeth. J Prosthet Dent. 1973;29(21):228–230. doi: 10.1016/0022-3913(73)90119-4. [DOI] [PubMed] [Google Scholar]
- 28.Moore PA, Manor RC. Hydrofluoric acid burns. J Prosthet Dent. 1982;47(3):338–339. doi: 10.1016/0022-3913(82)90165-2. [DOI] [PubMed] [Google Scholar]
- 29.Ahmad Akhoundi M, Rahmati Kamel M, Hooshmand T, Harririan I, Kharazi Fard M, Noroozi H. Assessment of bond strength between metal brackets and non-glazed ceramic in different surface treatment methods. J Dent (Tehran) 2010;7(2):64–70. [PMC free article] [PubMed] [Google Scholar]
- 30.Aida M, Hayakawa T, Mizukawa K. Adhesion of composite to porcelain with various surface conditions. J Prosthet Dent. 1995;73(5):464–470. doi: 10.1016/s0022-3913(05)80076-9. [DOI] [PubMed] [Google Scholar]
- 31.Kussano CM, Bonfante G, Batista JG, Pinto JH. Evaluation of shear bond strength of composite to porcelain according to surface treatment. Braz Dent J. 2003 Oct 3;14(2):132–135. doi: 10.1590/S0103-64402003000200011. [DOI] [PubMed] [Google Scholar]
- 32.Nebbe B, Stein E. Orthodontic brackets bonded to glazed and deglazed porcelain surfaces. Am J Orthod Dentofacial Orthop. 1996;109(4):431–436. doi: 10.1016/S0889-5406(96)70125-7. [DOI] [PubMed] [Google Scholar]
- 33.Newman SM, Dressler KB, Grenadier MR. Direct bonding of orthodontic brackets to esthetic restorative materials using a silane. Am J Orthod. 1984;86(6):503–506. doi: 10.1016/s0002-9416(84)90356-7. [DOI] [PubMed] [Google Scholar]
- 34.Shahverdi S, Canay S, Sahin E, Bilge A. Effects of different surface treatment methods on the bond strength of composite resin to porcelain. J Oral Rehabil. 1998;2(9):699–705. doi: 10.1046/j.1365-2842.1998.00299.x. [DOI] [PubMed] [Google Scholar]
- 35.Walsh LJ, Abood D, Brockhurst PJ. Bonding of Brackets bonded to porcelain resin composite to carbon dioxide laser-modified human enamel. Dent Mater. 1994;10(3):162–166. doi: 10.1016/0109-5641(94)90026-4. [DOI] [PubMed] [Google Scholar]
- 36.Ariyaratnam MT, Wilson MA, Mackie IC, Blinkhorn AS. A comparison of surface roughness and composite/enamel bond strength of human enamel following the application of the nd:Yag laser and etching with phosphoric acid. Dent Mater. 1997;13(1):51–55. doi: 10.1016/s0109-5641(97)80008-5. [DOI] [PubMed] [Google Scholar]
- 37.Martinez-Insua A, Da Silva Dominguez L, Rivera FG, Santana-Penin UA. Differences in bonding to acid-etched or er:Yag-laser-treated enamel and dentin surfaces. J Prosthet Dent. 2000;84(3):280–288. doi: 10.1067/mpr.2000.108600. [DOI] [PubMed] [Google Scholar]
- 38.da Silva Ferreira S, Hanashiro FS, de Souza-Zaroni WC, Turbino ML, Youssef MN. Influence of aluminum oxide sandblasting associated with nd:Yag or er:Yag lasers on shear bond strength of a feldspathic ceramic to resin cements. Photomed Laser Surg. 2010;28(4):471–475. doi: 10.1089/pho.2009.2528. [DOI] [PubMed] [Google Scholar]
- 39.Kara HB, Dilber E, Koc O, Ozturk AN, Bulbul M. Effect of different surface treatments on roughness of ips empress 2 ceramic. Lasers Med Sci. 2012;27(2):267–272. doi: 10.1007/s10103-010-0860-3. [DOI] [PubMed] [Google Scholar]
- 40.Kara HB, Ozturk AN, Aykent F, Koc O, Ozturk B. The effect of different surface treatments on roughness and bond strength in low fusing ceramics. Lasers Med Sci. 2011;26(5):599–604. doi: 10.1007/s10103-010-0806-9. [DOI] [PubMed] [Google Scholar]
- 41.Li R, Ren Y, Han J. Effects of pulsed nd:Yag laser irradiation on shear bond strength of composite resin bonded to porcelain. Hua Xi Kou Qiang Yi Xue Za Zhi. 2000;18(6):377–379. [PubMed] [Google Scholar]
- 42.Yassaei S, Moradi F, Aghili H, Kamran MH. Shear bond strength of orthodontic brackets bonded to porcelain following etching with Er:YAG laser versus hydrofluoric acid. Orthodontics (Chic.) 2013;14(1) doi: 10.11607/ortho.856. [DOI] [PubMed] [Google Scholar]
- 43.Sohn DS, An KM. The effect of using laser for ceramic bracket bonding of porcelain surfaces. Korean J Orthod. 2008;38(4):275–282. doi: 10.4041/kjod.2008.38.4.275. [DOI] [Google Scholar]
- 44.Akova T, Yoldas O, Toroglu MS, Uysal H. Porcelain surface treatment by laser for bracket porcelain bonding. Am J Orthod Dentofacial Orthop. 2005;128(5):630–637. doi: 10.1016/j.ajodo.2004.02.021. [DOI] [PubMed] [Google Scholar]