Abstract
Fractures in the jaw bones could present themselves differently according to the strength of the force and the bone’s ability to absorb the impact. The location and type of the fracture is important as well as the cause of the fracture (traffic accidents, melee trauma, pathologic changes). Pre-existing pathologic lesions, position of the teeth and the way they are affected by the fracture have a great influence on the prognosis. Whether to extract the teeth in the line of a fracture has always been controversial among dentists. While some researchers advocate that such teeth should be extracted to avoid complications, others believe that retaining these teeth would benefit the patient more. Most clinicians prefer to treat their patients depending on their own previous experiences. This article aims to establish a guideline on assessing whether to retain or extract the teeth in the fracture line.
Keywords: Mandibular fracture, teeth in the line of fracture, healing complications
Introduction
The mandible is the most durable bone in the maxillofacial region (1). Fractures in the mandible are dependent on many factors. Depending on the force of the trauma and the ability of the bone to absorb the shock of the trauma, the resulting fracture may vary between a single hairline fracture and multiple fractures along the mandible. The location and type of the fracture depends on the magnitude of the force, bone density, structurally weak parts of the bone, the state of the soft tissue surrounding the face and the direction in which the mastication muscles pull the fractured bone fragments (2). Clinically significant jaw fractures represent themselves with symptoms such as pain, edema, hematoma, malocclusion, displacement and/or mobility of the fractured segments, facial asymmetry and dysphonia (3).
When the mandibular fractures are evaluated in terms of etiology, traffic accidents which account for 32% of all fractures are the most common cause for injury followed by melee fights with incidence of 32% and 31.6%, respectively. Fractures caused by falls are seen 27% of the time. Fractures that are caused by gunshots, sports accidents and pathologic changes are rarely seen (4, 5). When the fractures are classified by location, condylar fractures take the lead with 36% followed by corpus (21%), angulus (20%) and parasymphesis fractures (14%) (4, 5).
The existing data show that 60% of all the fractures are seen in the toothed area of the mandible and the trauma that caused the fracture often causes damage to the related teeth. The extent of the damage to the teeth in the fracture line may complicate the fracture and the healing process therefore affects the outcome of the treatment. Avulsion, subluxation, root fractures, loss of vitality and preexisting pathologies of the teeth in the fracture line can lead to complications delaying the healing period (4, 6, 7, 8).
When the literature is reviewed it is seen that there is no precise protocol about whether a tooth in the line of a fracture should be extracted or not. Previously, most of the researchers advocated that the teeth in the line of the jaw fractures would be a source of infection in case they were to be left in situ and suggested that these teeth should be extracted. The same researchers believe that the extraction of these teeth prevents the development of osteomyelitis, providing an uncomplicated healing period. They even suggest the extraction of vital teeth in the line of a fracture should avoid infection since they are connected to the oral cavity via periodonsium (4, 9). Some of the researchers believe that the teeth could be retained during the healing of the fracture if a stable splint or osteosynthesis is applied while others suggest prophylactic antibiotics therapy (10).
When a fracture occurs in a tooth bearing area of the mandible, the relation between the fracture line and the teeth may present in many different ways. Samson et al. (11) evaluated the relation of the teeth according to the fracture line in four main groups; (Figure 1).
Figure 1.
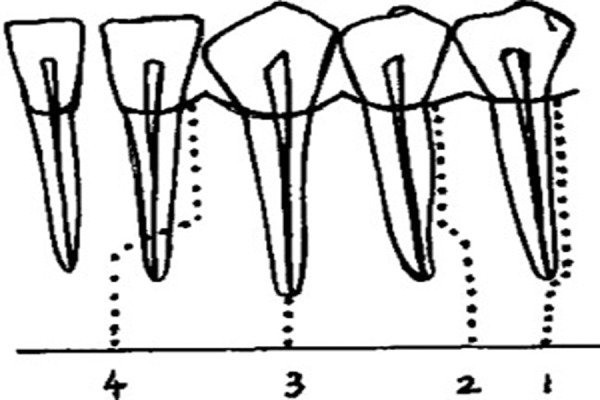
Possible fracture lines around the toothed area.
In the first group, the fracture line passed through the periodontium along the root unilaterally whereas in the second group it only passed through the upper ¾ of the root. In the third group the fracture line is limited to the apex of the tooth. In the fourth group the fracture line encircles the root bilaterally and then continues into the alveolalar bone. The worst prognosis is seen in the first group while the best is seen in the third group.
Andreassen et al.(12) studied 492 root fractures in 432 trauma patients and found out that 66% of 50 teeth that were fractured close to the cementoenamel junction were lost within the first 10 years due to infection.
Malanchuk and Kopchak (13) determined the risk factors for infection in patients with mandibular fractures located in the tooth-bearing area as delayed medical care, multiple and comminuted fractures, accompanying pathological disorders, and the type of antibiotic used. They found out that older patients were more susceptible to infection during the course of treatment. They also stated that the infection rate was 55% in patients older than 60 and there is no significant difference between angular and comminuted fractures. According to Malanchuk and Kopchak (13), a tooth in the fracture line had no significant influence on the infection rate, which was 25% among the patients with a tooth in the fracture line vs. 22% in the others. The data obtained in his study suggests that use of antibiotics decreases the incidence of infection even when there is a tooth in the fracture line and he concluded infection is not only caused by a tooth in the fracture line but also by bacteria that can penetrate into the fracture zone via lacerations and mucosal ruptures.
Ellis (14) concluded that the risk of infection was a little higher if a tooth was present in the fracture line but the differences were not statistically significant. Furthermore, the risk of postoperative infection was not reduced when the tooth was removed.
Rai and Pradhan (5) studied 54 patients with angular fractures where a third molar was present in the fracture line. They divided the patients into two groups; in the first 30 patients the third molar was retained whereas in the second group the third molar was extracted. Patients were then evaluated in terms of infection and occlusal discrepancy. In the first group, the incidence of infection and occlusal discrepancy was 13.33%. In the second group, the incidence of infection and occlusal discrepancy was 2.5%1 and 16.66%, respectively.
Samson et al. (11) studied 62 mandibular fractures in 50 patients in 2010. The patients were sorted by the location and the displacement of the fracture and the response to the vitality test. The teeth of 3 out of 4 patients that responded negative to the preoperative vitality test were extracted due to infection. The fourth patient exhibited symptoms of infection after a 1 year follow-up. The rate of infection was determined to be 6.5%.
Bobrowski et al. (15) studied a series of 1542 mandibular angle fractures. Of 788 cases where the tooth was removed, a postoperative infection occurred in 84 cases, of 754 cases where the tooth was retained, postoperative infection also occurred in 84 cases. They concluded that there was no significant statistical difference between removing or retaining the tooth in the line of fracture and the occurrence of postoperative infection.
The fate of primary tooth buds may vary in children with mandibular fractures. The age of the patient, the developmental stage of the tooth and the magnitude of the trauma are the factors that affect the prognosis. The complications may manifest as interruption of development of the tooth root, fusion and anomalies in the morphology. Teeth that are in the stage of crown calcification are less affected than those that are in the stage of root formation. Tooth buds that are in the line of a fracture usually (82%) erupt normally, however in 18% of cases delayed eruption or impaction may be seen. As long as there is no sign of infection, tooth buds should be retained and should not become damaged during the course of treatment (16).
Discussion
When treating maxillofacial trauma patients, the general principles of bone fracture treatment should always be remembered. These principles are the correct anatomical reduction of bone fragments, protecting the occlusal plane, using the right fixation technique which will hold the bone fragments immobilized in a functional position while maintaining occlusion until the end of the treatment, and the prevention of infection (17). Because the teeth in the fracture line have influence over these four principles, it is in the best interest of the patient that the surgeon determines a course of treatment after a careful examination. While a tooth in the fracture line enhances stabilization between bone fragments and facilitates the reduction of these fragments, the risk of infection is the most important disadvantage. Extracting the teeth in the angle region where the mandible is anatomically thinner further decreases the surface area between bone fragments and complicates the immobilization of the bone fragments (18, 19). It is often seen that in the literature the teeth with a certain indication for extraction are always extracted and they are not included in the study. The results are achieved after these teeth are excluded. When deciding whether to extract a tooth in the fracture line, dentists should remember the table below and decide on a treatment plan individually for every patient (Table 1).
Another point to consider is deciding the time of extraction of a tooth located in the fracture line because extraction increases the risk of infection and displacement of bone fragments (20, 21). Therefore some researchers believe that the non-urgent extractions such as non-symptomatic third molars could be postponed after the 4-6 week treatment period (22).
Some researchers think that performing a vitality test is beneficial before deciding whether to extract a tooth in the fracture line. However there seems to be no consensus in the literature on the role of a vitality test in treatment planning. As a matter of fact in many cases the teeth on a fracture line may respond with a false positive on vitality test due to acute apical periodontitis. While some researchers believe that those which respond negative to the test should be extracted right away, others advocate the long term follow-up would be more suitable. Especially the teeth that have not completed the apexification may become vital once more through revascularization (4).
Deciduous teeth that are not highly mobile, infected and fractured should be retained if possible. Permanent teeth of children that are in the line of fracture should be retained intact whenever possible and their prognosis should closely observed. Tooth buds that are not infected should also be retained and not be damaged during the course of treatment (23).
Table 1.
| Absolute indications for extraction | Relative indications for extraction | Relative contraindications for extraction |
|---|---|---|
| Teeth with vertical root fractures | Teeth with advanced periodontitis | Teeth that are essential for anatomical reduction |
| Highly mobile teeth | Non-functional teeth (3rd molars) | Teeth that act as a occlusal stopper |
| Teeth with periapical pathologies | Roots that have horizontal and/or oblique fractures | |
| Decayed and/or fractured teeth that cannot be restorated | ||
| Presence of acute infection in the fracture line | ||
| Teeth that may cause acute pericoronitis | ||
| Teeth that have root fractures near the cemento-enamel junction |
Conclusion
Dentists should be more conservative towards the teeth that are in the fracture line. In a one year period after treatment the risk of complication varies between 6%-25% for teeth in the fracture line. Although with the use of antibiotics, the prophylactic extraction of non-symptomatic teeth are no longer necessary, close observation and one year radiological and clinical follow up are advised.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Patrocinio LG, Patrocinio JA, Borba BH, Bonatti Bde S, Pinto LF, Vieira JV, Costa JM. Mandibular fracture: analysis of 293 patients treated in the Hospital of Clinics, Federal University of Uberlandia. Braz J Otorhinolaryngol. 2005;71(5):560–565. doi: 10.1016/S1808-8694(15)31257-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metin M, Sener I, Tek M. Impacted teeth and mandibular fracture. Eur J Dent. 2007;1(1):18–20. [PMC free article] [PubMed] [Google Scholar]
- 3.Thapliyal GK, Sinha R, Menon PS, Chakranarayan A. Management of mandibular fractures. MJAFI. 2008;64(3):218–220. doi: 10.1016/S0377-1237(08)80096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamboozia AH, Punnia-Moorthy A. The fate of teeth in mandibular fracture lines. A clinical and radiographic follow-up study. Int J Oral Maxillofac Surg. 1993;22(2):97–101. doi: 10.1016/s0901-5027(05)80811-2. [DOI] [PubMed] [Google Scholar]
- 5.Rai S, Pradhan R. Tooth in the line of fracture: its prognosis and its effects on healing. Indian J Dent Res. 2011;22(3):495–496. doi: 10.4103/0970-9290.87083. [DOI] [PubMed] [Google Scholar]
- 6.Wolujevicz MA. Fractures of the mandible involving the impacted third molar tooth: an analysis of 47 cases. Br J Oral Surg. 1980;18(2):125–131. doi: 10.1016/0007-117x(80)90028-1. [DOI] [PubMed] [Google Scholar]
- 7.Luz JG, Moraes RB, D’Ávila RP, Yamamoto MK. Factors contributing to the surgical retreatment of mandibular fractures. Braz Oral Res. 2013;27(3):258–265. doi: 10.1590/S1806-83242013005000007. [DOI] [PubMed] [Google Scholar]
- 8.Chrcanovic BR. Factors influencing the incidence of maxillofacial fractures. Oral Maxillofac Surg. 2012;16(1):3–17. doi: 10.1007/s10006-011-0280-y. [DOI] [PubMed] [Google Scholar]
- 9.Chrcanovic BR. Teeth in the line of mandibular fractures. Oral Maxillofac Surg. 2014;18(1):7–24. doi: 10.1007/s10006-012-0369-y. [DOI] [PubMed] [Google Scholar]
- 10.Chuong R, Donoff RB, Guralnick WC. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg. 1983;41(5):305–309. doi: 10.1016/0278-2391(83)90297-5. - 309. [DOI] [PubMed] [Google Scholar]
- 11.Samson J, John R, Jayakumar S. Teeth in the line of fracture: to retain or remove? Craniomaxillofac Trauma Reconstr. 2010;3(4):177–184. doi: 10.1055/s-0030-1268512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreasen Jens O, Ahrensburg SS, Tsilingaridis G. Root fractures: the influence of type of healing and location of fracture on tooth survival rates - an analysis of 492 cases. Dent Traumatol. 2012 Mar 23;28(5):404–409. doi: 10.1111/j.1600-9657.2012.01132.x. [DOI] [PubMed] [Google Scholar]
- 13.Malanchuk VO, Kopchak AV. Risk factors for development of infection in patients with mandibular fractures located in the tooth-bearing area. J Craniomaxillofac Surg. 2007 Feb 12;35(1):57–62. doi: 10.1016/j.jcms.2006.07.865. [DOI] [PubMed] [Google Scholar]
- 14.Ellis E., 3rd Outcomes of patients with teeth in the line of mandibular angle fractures treated with stable internal fixation. J Oral Maxillofac Surg. 2002;60(8):863–865. doi: 10.1053/joms.2002.33852. [DOI] [PubMed] [Google Scholar]
- 15.Bobrowski AN, Sonego CL, Chagas OL. Postoperative infection associated with mandibular angle fracture treatment in the presence of teeth on the fracture line: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2013 Apr 25;42(9):1041–1048. doi: 10.1016/j.ijom.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 16.Koenig WR, Olsson AB, Pensler JM. The fate of developing teeth in facial trauma: tooth buds in the line of mandibular fractures in children. Ann Plast Surg. 1994;32(5):503–505. doi: 10.1097/00000637-199405000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Berg S, Pape HD. Teeth in the fracture line. Int J Oral Maxillofac Surg. 1992;21(3):145–146. doi: 10.1016/s0901-5027(05)80781-7. [DOI] [PubMed] [Google Scholar]
- 18.Spinnato G, Alberto PL. Teeth in the line of mandibular fractures. Atlas Oral Maxillofac Surg Clin North Am. 2009;17(1):15–18. doi: 10.1016/j.cxom.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Gerbino G, Tarello F, Fasolis M, Gioanni PP. Rigid fixation with teeth in the line of mandibular fractures. Int J Oral Maxillofac Surg. 1997;26(3):182–186. doi: 10.1016/s0901-5027(97)80816-8. [DOI] [PubMed] [Google Scholar]
- 20.Iizuka T, Lindqvist C, Hallikainen D, Paukku P. Infection after rigid internal fixation of mandibular fractures: a clinical and radiologic study. J Oral Maxillofac Surg. 1991;49(6):585–593. doi: 10.1016/0278-2391(91)90340-r. - 593. [DOI] [PubMed] [Google Scholar]
- 21.Amaratunga NA. The effect of teeth in the line of mandibular fractures on healing. J Oral Maxillofac Surg. 1987;45(4):312–314. doi: 10.1016/0278-2391(87)90350-8. [DOI] [PubMed] [Google Scholar]
- 22.Neal DC, Wagner WF, Alpert B. Morbidity associated with teeth in the line of mandibular fractures. J Oral Surg. 1978;36(11):859–862. [PubMed] [Google Scholar]
- 23.Suei Y, Mallick PC, Nagasaki T, Taguchi A, Fujita M, Tanimoto K. Radiographic evaluation of the fate of developing tooth buds on the fracture line of mandibular fractures. J Oral Maxillofac Surg. 2006;64(1):94–99. doi: 10.1016/j.joms.2005.10.005. [DOI] [PubMed] [Google Scholar]


