Abstract
Purpose:
The aim of this study was to compare the mandibular hard and soft tissue measurements of unilateral and bilateral cleft lip and palate patients with non-cleft individuals.
Materials and Methods:
The study sample comprised of lateral cephalograms of 45 subjects. Sample included 15 non-cleft (NC), 15 unilateral cleft lip and palate (UCLP) and 15 bilateral cleft lip and palate (BCLP) cases whose age were between 15 to 17. 1 angular 13 linear measurements were carried out using Arnett and Gunson soft tissue cephalometric analysis and 4 angular measurements were calculated with Steiner Analysis.
Results:
Mandibular incisor inclinations relative to the occlusal plane (Md1-Md OP) were significantly greater and mandibular incisor projections (Md1-TVL) were significantly retrusive in cleft subjects (p<0.05). Projection values pertaining to lower lip anterior (LLA-TVL), soft tissue B point (B’-TVL), and soft tissue pogonion (Pog’-TVL) were significantly deficient as well in cleft patients (p<0.05). Sagittal position of the maxilla (SNA) (p<0.001) and intermaxillary relation of the jaws (ANB) were significantly deficient in UCLP subjects (p<0.05) and BCLP individuals (p<0.01). LLA-TVL and B’-TVL correlated with SNB in cleft patients (p<0.05).
Conclusion:
Decreased lower lip and chin projection values suggest that mandibular region of cleft patients should be taken into account in forming the treatment plan to improve the esthetic outcome of orthodontic and plastic surgery interventions.
Keywords: Cleft lip and palate, lateral cephalograms, incisor inclination, lower lip projection, chin
Introduction
Orofacial clefts result not only in functional disorders of speech, hearing and occlusion, but in psychological problems as a result of esthetic defects. The primary concerns of clinicians, patients and ordinary people are more concentrated on the soft tissue structure of upper lip and nose region in cleft individuals since no direct impact of cleft deformity or surgical scar from operations is monitored in lower lip area. However indirect consequences of altered or imbalanced function of the orofacial musculature could be observed (1). Despite the abundant number of researches concerning facial profile, upper lip and nose region, relatively small number of studies has been carried out especially related the lower facial area. When the available scarce number of researches is investigated concerning the mandibular soft and hard tissues of cleft patients, contradicting results can be observed. More specifically; the findings regarding the thickness (2, 3, 4), protrusion (3, 5) and length (2, 3) of the lower lip in various studies differ. Therefore, objective measures are needed for the evaluation of the lower lip that will shed a light in providing better treatment outcomes. Cleft patients go through several surgical interventions starting from infancy reaching beyond adulthood of their lives. Orthognathic surgery patients specified the primary reason for resorting to surgery as esthetics among other factors such as occlusion, pronunciation, function, pain and discomfort (6, 7). However it has been pointed out that the ideal esthetic results cannot always be accomplished utilizing conventional cephalometric analysis methods that have been used routinely (8, 9). Moreover the principal factor affecting the esthetics and stability of a treatment are neither the hard tissue considerations nor dental occlusion but soft tissue relations (9). Additionally, it has been pointed out that soft tissue profile analysis is more likely to be able detect differences in outcomes compared to conventional skeletal analysis (10). Thus more soft tissue oriented diagnostic criteria and treatment methods are put to use. Burstone (11), Fish and Epker (12), and most recently Arnett and Gunson (13) can be specified among those who have most frequently practiced soft tissue cephalometric analysis (STCA) today. Hence, the aim of our study was to detail the differences in the hard and soft tissues of mandibular region in unilateral cleft lip and palate (UCLP) and bilateral cleft lip and palate patients (BCLP) and compare these measurements with non-cleft (NC) individuals based on Arnett and Gunson STCA (13). Our null hypothesis were that, (a) mandibular dental parameters of cleft and non-cleft patients are not different due to compensatory mechanisms in play (b) the differences observed pertaining to dental parameters do not show more severity in BCLP patients compared to UCLP patients (c) there was no difference between the mandibular hard and soft tissues of cleft and noncleft individuals with disparities being confined to dental parameters only.
Materials and Methods
Sample selection criteria
The study protocol was approved by the Ethics Committee of the School of Medicine, Ege University, İzmir, Turkey (project no: 14-6.1/10). The lateral cephalograms of 45 subjects (N=45) (8 girls and 7 boys in each group) within the age range of 15 to 17 years constituted the non-syndromic UCLP (n=15), BCLP (n=15) and NC (n=15) groups. The radiographies were gathered from the archives of the Ege University, Orthodontics Department. The lateral cephalograms had been taken with the teeth in occlusion and the lips in repose. Attention was paid to the absence of the following: (1) syndromes, airway infections, (2) nasal obstructions, and (3) pharyngeal pathologies, such as adenoid vegetation and tonsillitis. No orthodontic treatment had been received prior to acquisition of cephalometric films but participants had undergone their primary surgeries. The control group was selected from subjects who presented with Cl I skeletal pattern, with normal vertical dimensions of the face, and no complaints pertaining to the airways. Care was given that included patients had crowding due to dental reasons only, with no skeletal constriction of the maxilla or mandible.
Assessment instruments and measurements
Cephalometric appraisals concerning mandibular region were carried out using Arnett and Gunson STCA (13) by the same researcher. Additionally, 4 angular measurements of Steiner Analysis were also included to have a through interpretation of the results. Since maxillary, nasal and subnasale region of the cleft individuals were reported to be incompetent, subnasale point was omitted for the construction of true vertical line (TVL). Instead a reference line was constructed at a sound region unaffected from the cleft but at the same time staying true to the recommendations of researchers (13) which was through a point 7.5 mm from soft tissue glabella, vertical to the floor with the patients head positioned in natural head position (Figure 1). 5 angular 13 linear measurements were carried out (Figure 2).
Figure 1.
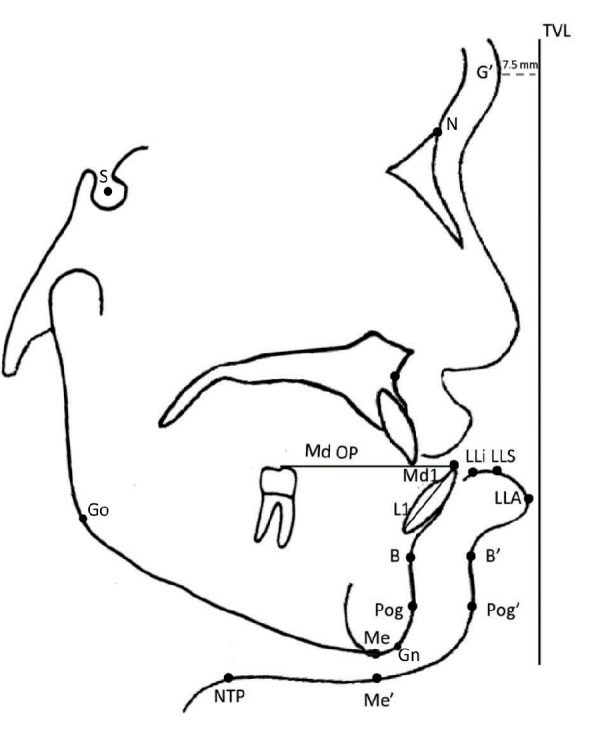
Reference Planes and Landmarks used: TVL, true vertical line constructed 7.5 mm anterior of soft tissue glabella with the head in natural head position; Md OP, mandibular occlusal plane passing from the mesiobuccal cusp of the 41 and incisal tip of 31; L1, long axis of the mandibular central incisor; G’, soft tissue glabella; Md1, mandibular incisor tip; LLS, lower lip superior; Me, hard tissue menton; Me’, soft tissue menton; LLi lower lip inside; LLA, lower lip anterior; Pog, hard tissue pogonion; Pog’, soft tissue pogonion; B, deepest point between alveolar crest and mental process; B’, soft tissue B point; NTP, neck throat point; S, geometric center of sella turcica; A, deepest point between anterior nasal spine and alveolar crest; N, most anterior point of the frontonasal suture; Go, the point of intersection of the ramus plane and the mandibular plane; Gn, the most antero-inferior point on the symphysis of the chin
Figure 2.
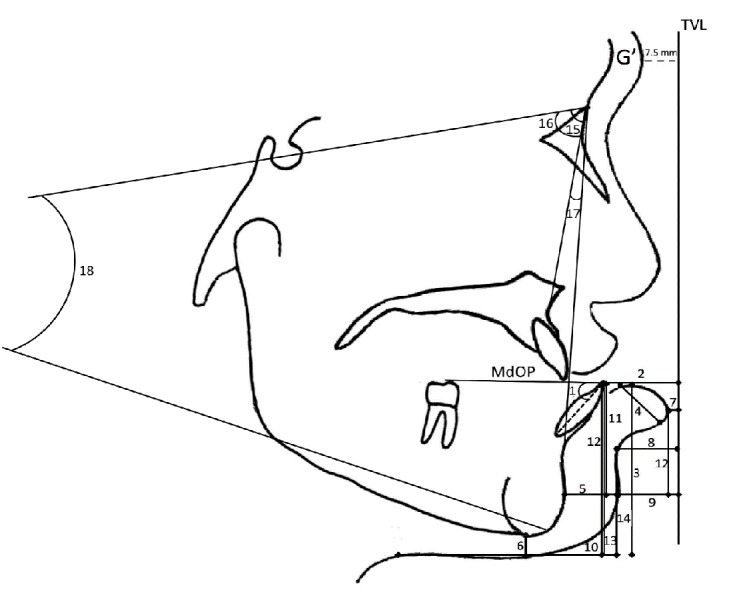
Angular and linear measurements used in Arnett and Gunson STCA concerning mandible: 1, Md1-Md OP angle; 2, Md1-TVL distance; 3, LLS-Me’ distance; 4, LLi-LLA distance; 5, Pog-Pog’ distance; 6, Me-Me’ distance; 7, LLA-TVL distance; 8, B’-TVL distance; 9, Pog’-TVL distance; 10, NTP-Pog’ distance; 11, Md1-Pog’ distance; 12, LLA-Pog’ distance; 13, Md1-Me’ distance; 14, B’-Pog’ distance; 15, SNA angle; 16, SNB angle; 17, ANB angle; 18, SNGoGn angle
Statistical analysis
According to the power analysis with 0.05 level and 80% power (based on a 1.22-mm standard deviation and a 1.37-mm detectable difference for lower lip protrusion) (3), the needed minimum sample size was 14 for each group. Statistical analysis of the cephalometric data was carried out with the SPSS for Windows program (version 20.0, SPSS, Chicago, IL, USA). Data were tested for normality through the Shapiro-Wilk test. The data was normally distributed; therefore, parametric tests were used. Descriptive statistics were reported for each parameter as minimum, maximum, mean and standard deviation. Analysis of variance (ANOVA) with post-hoc tests was used for statistical comparisons.
To evaluate the relationship between the parameters of Arnett and Gunson Analysis and sagittal and vertical parameters of the cleft patients, Pearson’s correlation coefficients were calculated. The statistical significance was determined at p<0.05 level. For the assessment of the method error, 10 randomly selected cephalograms were retraced and remeasured, and method errors were calculated, as recommended by Dahlberg (14).
Results
The errors varied from 0.20 to 0.70 mm in linear measurements, and ranged between 0.16-0.72 for the angular measurements. The study was conducted on 24 female and 21 male subjects within the age range of 15-17. Cephalograms of 15 UCLP (mean age 15.53±0.74 years), 15 BCLP (mean age 15.4±0.61 years), and 15 NC (mean age 15.93±0.79 years) individuals were used in the evaluation of mandibular soft and hard tissue parameters. The means, standard deviations, minimum and maximum values of the evaluated data are presented in Table 1
Table 1.
Means, standard deviations, minimum and maximum values of each group (UCLP: Unilateral Cleft Lip and Palate, BCLP: Bilateral Cleft Lip and Palate, NC: Non-Cleft).
| Variable | Group | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Md1-Md OP | UCLP | 70.64 | 2.04 | 67.40 | 73.80 |
| BCLP | 71.03 | 5.85 | 58.30 | 76.40 | |
| NC | 65.75 | 3.41 | 62.10 | 74.20 | |
| Md1-TVL | UCLP | -17.62 | 2.34 | -21.23 | -15.04 |
| BCLP | -17.87 | 2.07 | -20.45 | -14.29 | |
| NC | -15.09 | 1.90 | -18.60 | -11.60 | |
| LLS-Me' | UCLP | 53.84 | 2.67 | 49.90 | 59.10 |
| BCLP | 53.82 | 8.90 | 45.70 | 76.20 | |
| NC | 47.59 | 2.41 | 44.10 | 50.20 | |
| LLi-LLA | UCLP | 10.33 | 1.77 | 8.00 | 12.70 |
| BCLP | 10.84 | 1.27 | 8.90 | 12.90 | |
| NC | 11.72 | 1.13 | 10.70 | 13.70 | |
| Pog-Pog' | UCLP | 10.89 | 1.95 | 8.40 | 13.90 |
| BCLP | 11.22 | 4.10 | 6.90 | 20.60 | |
| NC | 12.05 | 1.57 | 9.70 | 15.60 | |
| Me-Me' | UCLP | 10.02 | 3.25 | 5.80 | 16.60 |
| BCLP | 7.27 | 2.09 | 4.90 | 11.00 | |
| NC | 8.59 | 2.38 | 5.90 | 13.10 | |
| LLA-TVL | UCLP | -2.82 | 1.47 | -5.97 | -0.62 |
| BCLP | -3.22 | 1.41 | -6.23 | -1.28 | |
| NC | -0.94 | 1.97 | -3.20 | 2.90 | |
| B'- TVL | UCLP | -8.89 | 1.66 | -10.78 | -5.50 |
| BCLP | -9.27 | 2.16 | -13.84 | -6.48 | |
| NC | -6.74 | 2.63 | -9.90 | -5.00 | |
| Pog-TVL | UCLP | -9.95 | 2.04 | -13.47 | -6.80 |
| BCLP | -9.85 | 2.01 | -12.88 | -6.92 | |
| NC | -7.16 | 2.72 | -12.40 | -3.90 | |
| NTP-Pog' | UCLP | 47.50 | 5.94 | 37.30 | 54.60 |
| BCLP | 48.75 | 4.37 | 40.40 | 53.60 | |
| NC | 52.99 | 5.25 | 44.90 | 63.30 | |
| Md1-Pog' | UCLP | 9.75 | 1.98 | 6.40 | 12.70 |
| BCLP | 9.27 | 3.27 | 3.50 | 12.90 | |
| NC | 8.63 | 2.52 | 5.20 | 14.50 | |
| LLA-Pog | UCLP | 2.06 | 3.02 | -4.50 | 5.30 |
| BCLP | 4.74 | 3.23 | 0.10 | 9.30 | |
| NC | 4.65 | 2.57 | -0.20 | 8.70 | |
| Md1-Me' | UCLP | 47.73 | 4.18 | 39.30 | 52.70 |
| BCLP | 46.92 | 3.62 | 43.10 | 54.70 | |
| NC | 45.05 | 2.66 | 41.00 | 48.60 | |
| B'-Pog' | UCLP | 2.24 | 1.07 | 0.60 | 4.60 |
| BCLP | 2.58 | 0.77 | 1.10 | 3.70 | |
| NC | 2.94 | 1.01 | 1.00 | 4.10 | |
| SNA | UCLP | 77.15 | 1.71 | 75.00 | 80.00 |
| BCLP | 76.01 | 0.67 | 75.30 | 77.18 | |
| NC | 80.47 | 1.80 | 78.11 | 83.36 | |
| SNB | UCLP | 76.86 | 1.37 | 75.10 | 78.96 |
| BCLP | 76.52 | 1.45 | 74.01 | 78.03 | |
| NC | 77.93 | 0.97 | 76.57 | 79.23 | |
| ANB | UCLP | 0.29 | 2.58 | -3.31 | 4.90 |
| BCLP | -0.51 | 1.36 | -2.60 | 1.56 | |
| NC | 2.54 | 1.71 | 1.02 | 5.56 | |
| SNGoGn | UCLP | 38.61 | 2.73 | 31.95 | 41.84 |
| BCLP | 37.14 | 2.06 | 33.10 | 40.64 | |
| NC | 36.38 | 1.14 | 34.08 | 37.74 |
First hypothesis was rejected. Dental parameters, namely, mandibular incisor inclination (Md1-Md OP) and mandibular incisor projection to TVL (Md1-TVL) showed significant differences among cleft and NC subjects (p<0.05). Second hypothesis was accepted since there were no significant differences among UCLP and BCLP patients in terms of severity of the evaluated variables. The final hypothesis was partially rejected since various mandibular soft tissue and skeletal characteristics of cleft and NC individuals did indeed show disparities.
Projections of lower lip anterior (LLA-TVL), soft tissue B’ point (B’-TVL), and soft tissue pogonion (Pog’-TVL) displayed significant differences among cleft and NC patients (p<0.05) with no difference between UCLP and BCLP patients. Lower lip length (LLS-Me’), chin height (Md1-Me’), incisor tip to chin (Md1-Pog’), lower lip anterior to chin (LLAPog’), chin contour (B’- Pog’), thickness of soft tissue pogonion (Pog-Pog’), thickness of soft tissue menton (Me-Me’), lower lip thickness (LLi-LLA), throat length (NTA-Pog’), vertical dimensions of the face (SNGoGn) and sagittal position of the mandible did not show any intergroup differences. Sagittal position of the maxilla (SNA) was significantly retrognathic in cleft patients compared to controls (p<0.001). When intermaxillary relation of the jaws is considered (ANB), significant deficiencies of in UCLP subjects (p<0.05) and BCLP individuals (p<0.01) were observed, but no intergroup difference was detected (Table 2). In UCLP patients a moderate, positive correlation was present between LLA-TVL and SNB (r= 0.46, p=0.006), and B’-TVL and SNB (r=0.39, p=0.030). Also moderate, positive correlations were present between LLA-TVL and SNB (r= 0.54, p=0.002), and B’-TVL and SNB (r=0.41, p=0.006) in BCLP individuals. No correlations were detected among SNA, ANB, SNGoGn and variables in Arnett and Gunson Analysis concerning the mandible.
Table 2.
Significance levels of investigated parameters among the groups (UCLP: Unilateral Cleft Lip and Palate, BCLP: Bilateral Cleft Lip and Palate, NC: Non-Cleft).
| Variable | Group | Group | Significance |
|---|---|---|---|
| Md1-Md OP | UCLP | NC | 0.037 |
| BCLP | 0.975 | ||
| BCLP | NC | 0.022 | |
| Md1-TVL | UCLP | NC | 0.037 |
| BCLP | 0.963 | ||
| BCLP | NC | 0.020 | |
| LLS-Me' | UCLP | NC | 0.054 |
| BCLP | 0.998 | ||
| BCLP | NC | 0.055 | |
| LLi-LLA | UCLP | NC | 0.111 |
| BCLP | 0.984 | ||
| BCLP | NC | 0.529 | |
| Pog-Pog' | UCLP | NC | 0.623 |
| BCLP | 0.962 | ||
| BCLP | NC | 0.783 | |
| Me-Me' | UCLP | NC | 0.698 |
| BCLP | 0.679 | ||
| BCLP | NC | 0.809 | |
| LLA-TVL | UCLP | NC | 0.047 |
| BCLP | 0.847 | ||
| BCLP | NC | 0.013 | |
| B'- TVL | UCLP | NC | 0.036 |
| BCLP | 0.889 | ||
| BCLP | NC | 0.012 | |
| Pog'-TVL | UCLP | NC | 0.028 |
| BCLP | 0.957 | ||
| BCLP | NC | 0.028 | |
| NTP-Pog' | UCLP | NC | 0.066 |
| BCLP | 0.855 | ||
| BCLP | NC | 0.184 | |
| Md1-Pog' | UCLP | NC | 0.621 |
| BCLP | 0.915 | ||
| BCLP | NC | 0.854 | |
| LLA-Pog' | UCLP | NC | 0.181 |
| BCLP | 0.157 | ||
| BCLP | NC | 0.997 | |
| Md1-Me' | UCLP | NC | 0.866 |
| BCLP | 0.306 | ||
| BCLP | NC | 0.744 | |
| B'-Pog' | UCLP | NC | 0.344 |
| BCLP | 0.711 | ||
| BCLP | NC | 0.683 | |
| SNA | UCLP | NC | 0.001 |
| BCLP | 0.214 | ||
| BCLP | NC | 0.001 | |
| SNB | UCLP | NC | 0.062 |
| BCLP | 0.820 | ||
| BCLP | NC | 0.051 | |
| ANB | UCLP | NC | 0.041 |
| BCLP | 0.636 | ||
| BCLP | NC | 0.005 | |
| SNGoGn | UCLP | NC | 0.068 |
| BCLP | 0.367 | ||
| BCLP | NC | 0.962 |
Discussion
Our first impression of people and the inferences about their characters is based on their facial appearances (15). When considered that CLP individuals content many surgical interventions for esthetic reasons, it is the utmost importance to provide the correct diagnosis to get the most out of surgeries with minimum number of interventions. Due to the relatively greater severity of the midfacial deformation, attention is subjectively directed to midfacial area and upper lip with lower lip usually omitted. However objective measures for evaluating facial disharmony in cleft individuals will lead to better treatment planning hence bring about improved surgical and orthodontic outcomes.
One integral observation of the current study was that the mean values of NC individuals were within the normative values reported by Tancan et al. (16) concerning Arnett appraisals for Turkish young adults. This implied that control group was representative of the ideal norms determined for Turkish individuals; hence intergroup comparisons would not be biased by deviations deriving from hard and soft tissues other than cleft anomaly. Furthermore, the proportion of female to male subjects was identical among groups to rule out the effect of sexual dimorphism on craniofacial growth and size.
Mandibular incisor inclinations were increased with respect to the occlusal plane in cleft patients with retrusive projection values relative to the TVL. In agreement with the findings of the present study, there is consensus in the literature on the retrusive position of the mandibular incisors (17, 18, 19, 20, 21) which is compensation to retroclined maxillary incisors due to the pressure exerted by the taut repaired lip. Also, the pressure exerted by the retroclined premaxilla could play a part in this retrusion since SNA angle was significantly lower in both of our cleft groups compared to the controls.
Lower lip length, chin height, incisor tip to chin, and lower lip anterior to chin measurements were similar between the groups coherent with the literature. (5) Mandibular projection values, including lower incisors, soft tissue B point and Pogonion showed retrusive values relative to the TVL when compared with the NC individuals. Some studies (2, 3, 5) indicated protrusive values for lower lip. Hasanzadeh et al. (2) and Liu et al. (3) used E-line (22) as a reference plane. However flatter nose tip in cleft individuals leading to reduced nasal projection affects the location of E-plane, forming the impression of protrusive lower lip whereas it is actually normal or retrusive. Similarly Moreira et al. (5) used sn’ point in constructing the reference plane, yet, the subnasale region of cleft individuals are already altered significantly with reduced maxillary height and depth, deficient nasal, upper lip and maxillary morphology as a result of surgical scars and tissue deficiencies with deviated anterior nasal spine (18, 23, 24, 25). Hence an erroneous fiducial line would bias the results. Therefore, a TVL which was constructed independent of the facial deformity was chosen in the current study to give the true extend of the deficiency.
As for the observed deficient mandibular projection values (projection of lower lip, soft tissue B point and soft tissue pogonion), the reason could either be the insufficiency of soft tissue thicknesses, skeletal inadequacies, lower lip exerting pressure during function or backwards rotation of the mandible. Mandibular soft tissue thickness at Pogonion and Menton as well as the thickness of the lower lip did not differ among the groups.
The forementioned soft tissue thicknesses measured were consistent with findings of the other authors (2, 3, 4, 18) hinting similar lip and soft tissue chin developments among cleft and NC individuals. Furthermore, mandibular soft tissue harmony values (LLA’-Pog and B’-Pog’) were similar among the groups. Therefore it would be erroneous to ground the retrusive projection values on soft tissue thickness inadequacies. Throat length (NTA-Pog’) hinting about mandibular corpus length was also comparable between cleft and NC individuals. Additionally, similar chin height measurements (Md1- Me’) indicated essentially non-deficient mandibular anterior skeletal morphology. To further look into the causes of these deficient mandibular projection values, supplementary measurements from Steiner Analysis were used.
The mean values of SNB measurements were less for cleft patients compared to NC individuals. Although these values failed to present a significant difference statistically, the p values calculated were on the verge of reaching a significance level. Furthermore, slight but non-significant increase was detected in vertical skeletal dimensions in cleft individuals. Hence when these data are evaluated coherently with the literature that point out similar mandibular morphologies between cleft and NC individuals (26, 27, 28) but report significantly lower sagittal parameters for cleft patients (29, 30, 31), backwards rotation of the mandible with retrognathic sagittal position (19, 32, 33) appears to be responsible for the deficient projection values. Likewise, although statistically significant correlations between SNB and projection values of LLA and B’ were detected, the correlation coefficients were relatively weak hence it will not be possible to make precise predictions concerning Arnett and Gunson soft tissue parameters based on skeletal parameters.
As for the limitations of this study, it was not possible to standardize the surgical protocols among subjects, due to different operation timings, operator identities and surgical interventions preferred. In retrospective studies, confounding variables (operations undergone) may go unrecognized due to inadequate knowledge of how they interrelate with the outcome (34). Furthermore, retrospective studies relies on others for reliability and accuracy of recordkeeping.
Conclusion
Though mandibular soft and hard tissue parameters displayed essentially the same values among BCLP and UCLP subjects, some disparities were present between cleft and NC individuals. Hence, it is important to make thorough consideration including the lower lip region also, to improve the esthetic outcome of orthodontic and plastic surgery interventions.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
This study has been presented as a poster in 2014 at the 1st Cleft Lip and Palate Congress, Kapadokya, Nevşehir, Turkey.
References
- 1.Proff P, Weingartner J, Koppe T, Fanghanel J, Mack F, Gedrange T. Morphofunctional changes of orofacial muscles in patients with unilateral or bilateral cleft lip, alveolus and palate. Ann Anat. 2007;189(2):203–207. doi: 10.1016/j.aanat.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Hasanzadeh N, Majidi MR, Kianifar H, Eslami N. Facial soft-tissue morphology of adolescent patients with nonsyndromic bilateral cleft lip and palate. J Craniofac Surg. 2014;25(1):314–317. doi: 10.1097/SCS.0000000000000446. [DOI] [PubMed] [Google Scholar]
- 3.Liu RK, Wamalwa P, Lu DW, Li CH, Hu HK, Zou S. Soft-tissue characteristics of operated unilateral complete cleft lip and palate patients in mixed dentition. J Craniofac Surg. 2011;22(4):1275–1279. doi: 10.1097/SCS.0b013e31821c6a96. [DOI] [PubMed] [Google Scholar]
- 4.Toygar TU, Akcam MO, Arman A. A cephalometric evaluation of lower lip in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2004;41(5):485–489. doi: 10.1597/03-115.1. [DOI] [PubMed] [Google Scholar]
- 5.Moreira I, Suri S, Ross B, Tompson B, Fisher D, Lou W. Soft-tissue profile growth in patients with repaired complete unilateral cleft lip and palate: A cephalometric comparison with normal controls at ages 7, 11, and 18 years. Am J Orthod Dentofacial Orthop. 2014;145(3):341–358. doi: 10.1016/j.ajodo.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham SJ. The psychology of facial appearance. Dent Update. 1999;26(10):438–443. doi: 10.12968/denu.1999.26.10.438. [DOI] [PubMed] [Google Scholar]
- 7.Yu D, Wang F, Wang X, Fang B, Shen SG. Presurgical motivations, self-esteem, and oral health of orthognathic surgery patients. J Craniofac Surg. 2013;24(3):743–747. doi: 10.1097/SCS.0b013e318285d5a4. [DOI] [PubMed] [Google Scholar]
- 8.Ackerman JL, Proffit WR, Sarver DM. The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res. 1999;2(2):49–52. doi: 10.1111/ocr.1999.2.2.49. [DOI] [PubMed] [Google Scholar]
- 9.Proffit WR. The soft tissue paradigm in orthodontic diagnosis and treatment planning: A new view for a new century. J Esthet Dent. 2000;12(1):46–49. [PubMed] [Google Scholar]
- 10.Molsted K, Asher-McDade C, Brattstrom V, Dahl E, Mars M, McWilliam J, Plint DA, Prahl-Andersen B, Semb G, Shaw WC. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 2. Craniofacial form and soft tissue profile. Cleft Palate Craniofac J. 1992;29(5):398–404. doi: 10.1597/1545-1569(1992)029<0398:ASCISO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36(4):269–277. [PubMed] [Google Scholar]
- 12.Fish LC, Epker BN. Dentofacial deformities related to midface deficiencies. Integrated orthodontic-surgical correction. J Clin Orthod. 1987;21(9):654–664. [PubMed] [Google Scholar]
- 13.Arnett GW, Gunson MJ. Facial planning for orthodontists and oral surgeons. Am J Orthod Dentofacial Orthop. 2004;126(3):290–295. doi: 10.1016/S0889540604005232. [DOI] [PubMed] [Google Scholar]
- 14.Dahlberg G. Statistical methods for medical and biological students. London: Allen; 1940. [Google Scholar]
- 15.Todorov A, Olivola CY, Dotsch R, Mende-Siedlecki P. Social attributions from faces: Determinants, consequences, accuracy, and functional significance. Annu Rev Psychol. 2015;66(3):519–545. doi: 10.1146/annurev-psych-113011-143831. [DOI] [PubMed] [Google Scholar]
- 16.Uysal T, Yagci A, Basciftci FA, Sisman Y. Standards of soft tissue arnett analysis for surgical planning in turkish adults. Eur J Orthod. 2009;31(4):449–456. doi: 10.1093/ejo/cjn123. [DOI] [PubMed] [Google Scholar]
- 17.Capelozza Filho L, Normando AD, da Silva Filho OG. Isolated influences of lip and palate surgery on facial growth: Comparison of operated and unoperated male adults with uclp. Cleft Palate Craniofac J. 1996;33(1):51–56. doi: 10.1597/1545-1569(1996)033<0051:IIOLAP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Celikoglu M, Buyuk SK, Sekerci AE, Ersoz M, Celik S, Sisman Y. Facial soft-tissue thickness in patients affected by bilateral cleft lip and palate: A retrospective cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2014;146(5):573–578. doi: 10.1016/j.ajodo.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Corbo M, Dujardin T, de Maertelaer V, Malevez C, Glineur R. Dentocraniofacial morphology of 21 patients with unilateral cleft lip and palate: A cephalometric study. Cleft Palate Craniofac J. 2005;42(6):618–624. doi: 10.1597/03-129.1. [DOI] [PubMed] [Google Scholar]
- 20.Lisson JA, Hanke I, Trankmann J. Vertical changes in patients with complete unilateral and bilateral cleft lip, alveolus and palate. J Orofac Orthop. 2004;65(3):246–258. doi: 10.1007/s00056-004-0332-0. [DOI] [PubMed] [Google Scholar]
- 21.Liu R, Lu D, Wamalwa P, Li C, Hu H, Zou S. Craniofacial morphology characteristics of operated unilateral complete cleft lip and palate patients in mixed dentition. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6):e16–e25. doi: 10.1016/j.tripleo.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Ricketts RM. Esthetics, environment, and the law of lip relation. Am J Orthod. 1968;54(4):272–289. doi: 10.1016/s0002-9416(68)90278-9. [DOI] [PubMed] [Google Scholar]
- 23.Ferrario VF, Sforza C, Dellavia C, Tartaglia GM, Sozzi D, Caru A. A quantitative three-dimensional assessment of abnormal variations in facial soft tissues of adult patients with cleft lip and palate. Cleft Palate Craniofac J. 2003;40(5):544–549. doi: 10.1597/1545-1569(2003)040<0544:AQTAOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Kilpelainen PV, Laine-Alava MT, Lammi S. Palatal morphology and type of clefting. Cleft Palate Craniofac J. 1996;33(6):477–482. doi: 10.1597/1545-1569(1996)033<0477:PMATOC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Shi B, Song QG, Zuo H, Zheng Q. Effects of lip repair on maxillary growth and facial soft tissue development in patients with a complete unilateral cleft of lip, alveolus and palate. J Craniomaxillofac Surg. 2006;34(6):355–361. doi: 10.1016/j.jcms.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Abad-Santamaria L, Lopez-de-Andres A, Jimenez-Trujillo I, Ruiz C, Romero M. Effect of unilateral posterior crossbite and unilateral cleft lip and palate on vertical mandibular asymmetry. Ir J Med Sci. 2014;183(3):357–362. doi: 10.1007/s11845-013-1020-0. [DOI] [PubMed] [Google Scholar]
- 27.Kyrkanides S, Richter L. Mandibular asymmetry and antigonial notching in individuals with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2002;39(1):30–35. doi: 10.1597/1545-1569(2002)039<0030:MAAANI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Laspos CP, Kyrkanides S, Tallents RH, Moss ME, Subtelny JD. Mandibular asymmetry in noncleft and unilateral cleft lip and palate individuals. Cleft Palate Craniofac J. 1997;34(5):410–416. doi: 10.1597/1545-1569(1997)034<0410:MAINAU>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Abuhijleh E, Aydemir H, Toygar-Memikoglu U. Three-dimensional craniofacial morphology in unilateral cleft lip and palate. J Oral Sci. 2014;56(2):165–172. doi: 10.2334/josnusd.56.165. [DOI] [PubMed] [Google Scholar]
- 30.Jahanbin A, Eslami N, Hoseini Zarch H, Kobravi S. Comparative evaluation of cranial base and facial morphology of cleft lip and palate patients with normal individuals in cone beam computed tomography. J Craniofac Surg. 2015;26(3):785–788. doi: 10.1097/SCS.0000000000001361. [DOI] [PubMed] [Google Scholar]
- 31.Semb G. A study of facial growth in patients with bilateral cleft lip and palate treated by the oslo clp team. Cleft Palate Craniofac J. 1991;28(1):22–39. doi: 10.1597/1545-1569(1991)028<0022:ASOFGI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Oosterkamp BC, Remmelink HJ, Pruim GJ, Hoekema A, Dijkstra PU. Craniofacial, craniocervical, and pharyngeal morphology in bilateral cleft lip and palate and obstructive sleep apnea patients. Cleft Palate Craniofac J. 2007;44(1):1–7. doi: 10.1597/05-175. [DOI] [PubMed] [Google Scholar]
- 33.Wermker K, Jung S, Joos U, Kleinheinz J. Nasopharyngeal development in patients with cleft lip and palate:a retrospective case-control study. J Otolaryngol. 2012 doi: 10.1155/2012/458507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ward RA, Brier ME. Retrospective analyses of large medical databases: What do they tell us. J Am Soc Nephrol. 1999;10(2):429–432. doi: 10.1681/ASN.V102429. [DOI] [PubMed] [Google Scholar]


