Abstract
Anterior iliac crest bone grafting is a well-established modality in the treatment of alveolar bone deficiencies. However, this procedure may also have considerable postoperative morbidity which is mostly related to general anesthesia. Postoperative pain-related complications can be managed by neuroaxial blockade techniques which provide adequate surgical analgesia and reduce postoperative pain. This clinical report describes the reconstruction of a severely atrophic maxilla with anterior iliac crest bone grafting using combined spinal epidural anesthesia. Neuroaxial blockade techniques may be a useful alternative to eliminate general anesthesia related challenges of anterior iliac crest bone grafting procedures.
Keywords: Bone grafting, iliac crest, neuroaxial blockade, epidural anesthesia, general anesthesia
Introduction
Maxillofacial region is susceptive to the effects of trauma, pathology, developmental deformities and alveolar ridge resorption process subsequent to tooth extraction. Treatment of large bone defects may require the use of extra-oral donor sites (1). Among these, anterior iliac crest is a well-established donor site as the harvested bone possesses excellent osteogenic, osteoconductive and osteoinductive qualities (2, 3). On the other hand, anterior iliac crest has also considerable postoperative morbidity such as chronic pain, disability, hemorrhage, visible scar, contour deformity and sensory loss (4).
Postoperative pain related complications can be managed by neuroaxial blockade (NAB) techniques which provide adequate surgical analgesia and reduce postoperative pain (5, 6). In addition, this technique is considered to be highly effective on the inhibition of vomiting reflex and it improves patient cooperation. Although NABs are complex anesthesia techniques, they can be a useful alternatives to eliminate general anesthesia related challenges of anterior iliac crest bone grafting procedures (7).
This clinical report presents the reconstruction of severe maxillary alveolar bone deficiency with anterior iliac crest bone grafting using combined spinal epidural anesthesia (CSEA) which is a type of NAB technique.
Case Report
A 35 years-old systematically healthy male patient was referred to Istanbul University, Faculty of Dentistry, Department of Oral and Maxillofacial Surgery for the reconstruction of his atrophic maxilla in order to maintain prosthodontics rehabilitation with dental implant supported fixed prosthesis. Following clinical and radiological examinations (Figure 1), it is decided to augment the atrophic maxilla by using autologous bone graft harvested from the anterior iliac crest via CSEA.
Figure 1.
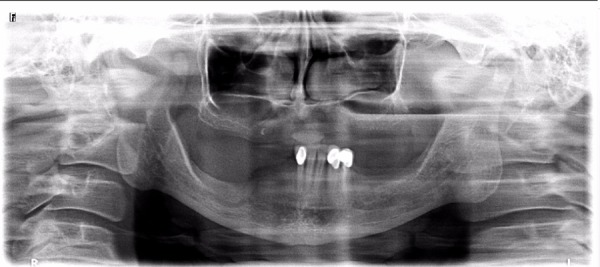
Preoperative panoramic radiography of the patient.
CSEA was administered at the L3–L4 intervertebral disc level (Figure 2) and intravenous sedation was administered in addition to local anesthesia. Initially the patient was turned to lateral decubitus position. The needle-through-needle technique was carried out by introducing a 17-gauge Tuohy needle into the L3 – L4 intervertebral space using a midline approach and the epidural space identified by the loss of resistance to air. Then, an adjustable 27-gauge Whitacre spinal needle (BD Durasafe; Becton-Dickinson, Franklin Lakes, NJ, USA) was inserted into the subarachnoid space via the Tuohy needle. After cerebrospinal fluid was obtained, the subarachnoid block performed by the intrathecal injection of 5.0 mg bupivacaine and 10 μg fentanyl. Following CSEA induction, a 19-gauge multiorificed catheter was placed into the epidural space for the intrathecal medication and the Tuohy needle was removed. Then, the patient was turned into the supine position and anterior iliac crest bone grafting was performed.
Figure 2.
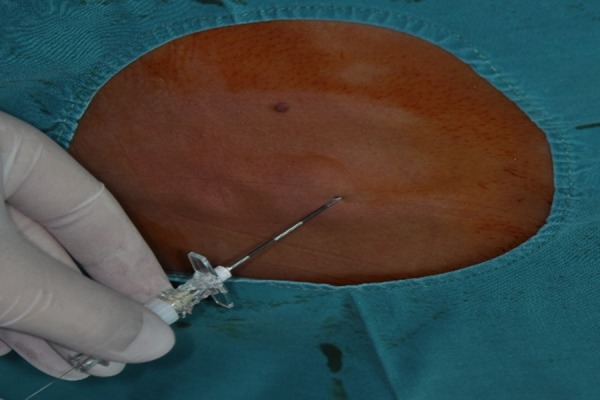
Performing combined spinal epidural anesthesia through L3-L4 intervertebral level.
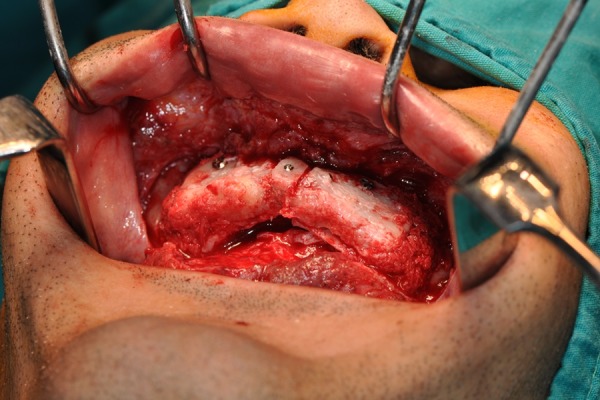
The standard surgical protocol for anterior iliac crest approach was performed and tricortical autonegonus block bone grafts 5 cm x 3 cm x 2 cm in size were harvested. A skin incision approximately 2 cm above the anteriosuperior iliac spine along the anteriosuperior margin of the anterior iliac crest was made by preserving lateral femoral cutaneous nerve. The medial and lateral cortical surfaces of the iliac crest were exposed directly after the subperiosteal dissection of soft tissues covering anterior iliac crest. A micro-saw and chisel were used to harvest a tricortical (corticocancellous) autogenous bone block from the anterior iliac crest (Figure 3). The sharp bone surfaces were smoothed and mini-wac drains were placed on the donor site. Periosteum of the anterior iliac crest was sutured by using 1/0 resorbable polyglactin 910 sutures (Vicryl, Ethicon, Somerville, NJ, USA) . The muscle attachments and subcutaneous layers of the flap were sutured by using 3/0 resorbable polyglactin 910 sutures (Vicryl, Ethicon, Somerville, NJ, USA). The skin was sutured by using 3/0 non-resorbable polypropylene sutures (Prolen; Dogsan Medical Supplies Industry, Trabzon, Turkey). A full thickness mucoperiosteal flap located at the deepest level of the maxillary anterior buccal sulcus was raised after the Le Fort 1 level incision by using needle tip electrocautery. Following flap elevation (Figure 4) the bone graft was modified and fixed to the recipient site by using titanium mini-screws to avoid micromovements of the bone graft during healing period (Figure 5). In addition to block bone grafting, bilateral sinus floor augmentations were performed by using residual bone graft grinded by bone mill. Finally, both the submucosa and the mucous layers were sutured by using 3/0 resorbable polyglactin910 sutures (Vicryl, Ethicon, Somerville, NJ, USA).
Figure 3.
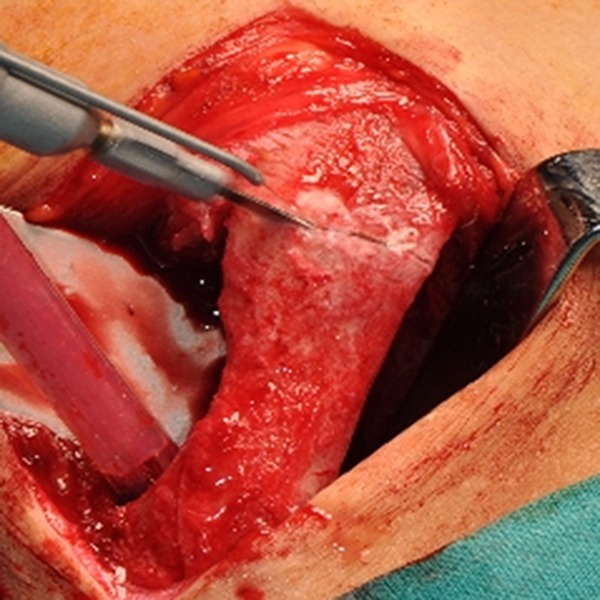
Bicortical autonegonus bone graft harvesting procedure.
Figure 4.
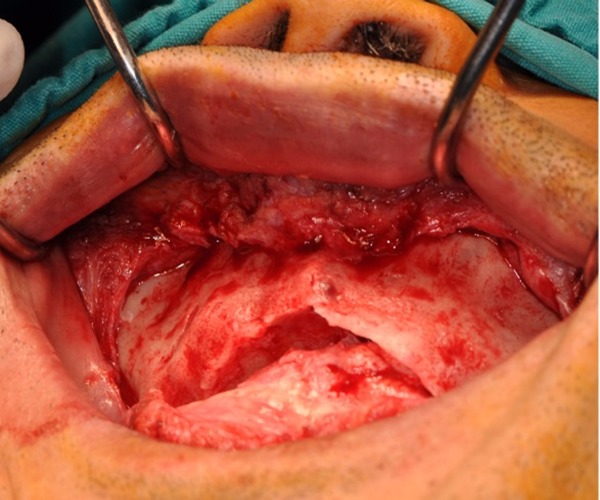
Clinical photograph of the surgical site before bone grafting.
Figure 5.
Bone blocks harvested from the anterior iliac crest were positioned along the contour of the maxillary arch.
The patient was mobilized after the effects of the CSEA on the lower extremities wore off. Fifteen mg bupivacaine and 50 μg fentanyl were administered via his epidural catheter for pain management during the hospitalization period. Postsurgical medications including; antibiotics for 7 days starting on the day of the operation (1,000 mg of amoxicillin and clavulanic acid administered twice daily), analgesics (600 mg ibuprofen as needed every 6 hours) and 0.2% chlorhexidine mouthwash twice daily for 2 weeks starting on the day after the operation were prescribed. Dexamethasone (4 mg daily) was administered for 2 days to control the postoperative edema. The patient was discharged one day after the surgery without epidural catheter and mini-wac drain and detailed written postoperative instructions were provided. Both the sutures of the donor and the recipient sites were removed 10 days after surgery and the recovery period was uneventful.
The positions of the autogenous bone grafts and augmented sinuses were controlled by panoramic radiography (Figure 6). After 3 months of graft integration period, for maxilla; 8 4.6 mm diameter, 12 mm length, for mandible;, 2 4,6 mm diameter, 9.5mm length, 2 4.6mm diameter, 12 mm length and 2 4.6 mm diameter 15 mm length Biohorizons RBT (Biohorizons Birmingham, AL, USA) dental implants were placed. After the osseointegration period of dental implants, the patient was referred to the prosthodontics clinic for the fabrication of implant supported fixed prosthesis (Figure 7).
Figure 6.
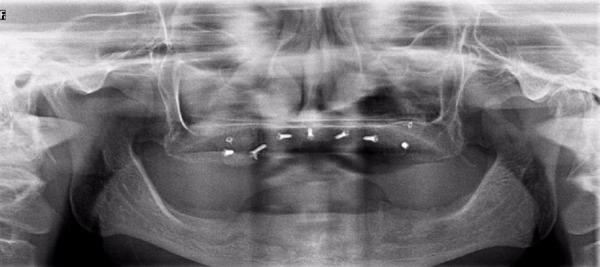
Postoperative panoramic radiography after anterior iliac crest bone grafting and bilateral sinus lifting procedure.
Figure 7.
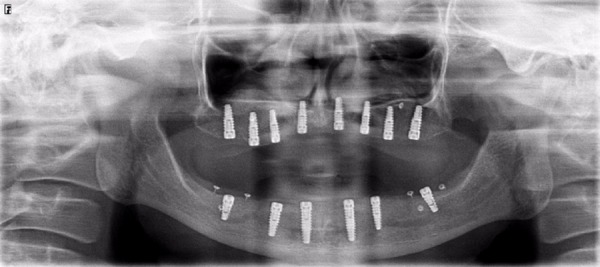
Postoperative panoramic radiography after dental implant operation.
Discussion
Autogenous bone is still considered one of the most popular graft materials for preprosthetic augmentation procedures. The anterior or the posterior aspect of the iliac crest remains the most preferred donor site which provides good quantities of cortical and cancellous bone with adequate volume and dimension for reconstruction of bone defects as well as placement of osseointegrated dental implants for complete aesthetic and functional rehabilitation (8). The implant survival rate in anterior iliac bone grafts has been reported to be 92.4% after a follow-up period of 5 years (9).
However, bone harvesting from an extraoral donor site may have considerable postoperative morbidity which is mostly related to general anesthesia. There are some clinical studies which have pointed that NABs have a lower effect on eventual morbidity and mortality risks compared to general anesthesia by reducing cardiac complication incidence, hemorrhage, respiratory depression, malign hyperthermia, postoperative anxiety, wake up delay and redistribution risk of drugs (5, 6).
It is essential to keep postoperative morbidities as low as possible and to get back the patient to daily routine as early as possible. The results of several studies about iliac bone grafting procedures documented that the patients were able to return to normal activities including sports within 4–6 weeks (4, 10). In present case, the patient was mobilized immediately after the effects of CSEA wore off. The length of stay in hospital was reported in similar variations with 2–8 days and it may be concluded that an outpatient iliac crest bone-grafting protocol provides patients with the opportunity to recover in the familiar home environment.
After bone harvesting from the anterior iliac crest, patients complained about persistent pain, superficial skin sensitivity, gait disturbance, the need for the use of crutches, bleeding, infection, pelvic fractures (4, 7). Immediate pain is the most disturbing postoperative morbidity to the patient after iliac bone grafting. In order to overcome the problem of prolonged pain, several technical modifications and the use of bupivacaine have been suggested (11). Epidural analgesia is more efficient to control postoperative acute pain and it does not require any other operative intervention such as psoas sheath block and administration of intravenous opioids or long acting local anesthetics (12). We assume that CSEA decreases opioid and non-steroidal anti-inflammatory drugs need significantly via epidural administration of local anesthetics. On the other hand, extended duration of surgery has been identified as an independent risk factor of infection, cerebrovascular accidents and intraoperative hypotension rates (13). In the present case, although preoperative preparation and administration of neuraxial anesthesia elongated the planned operation time, postoperative complications were not observed.
Conclusion
Neuroaxial blockade techniques may be a useful alternative to eliminate general anesthesia related challenges of anterior iliac crest bone grafting procedures. This case report emphasizes that the combined spinal-epidural anesthesia could effectively achieve the patient cooperation during anterior iliac bone grafting surgery, postoperative mobilization and immediate pain management.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Mertens C, Decker C, Seeberger R, Hoffmann J, Sander A, Freier K. Early bone resorption after vertical bone augmentation--a comparison of calvarial and iliac grafts. Clin Oral Implants Res. 2013;24(7):820–825. doi: 10.1111/j.1600-0501.2012.02463.x. [DOI] [PubMed] [Google Scholar]
- 2.Kahnberg KE, Vannas-Lofqvist L. Maxillary osteotomy with an interpositional bone graft and implants for reconstruction of the severely resorbed maxilla: A clinical report. Int J Oral Maxillofac Implants. 2005;20(6):938–945. [PubMed] [Google Scholar]
- 3.Nystrom E, Ahlqvist J, Gunne J, Kahnberg K E. 10-year follow-up of onlay bone grafts and implants in severely resorbed maxillae. Int J Oral Maxillofac Surg. 2004;33(3):258–262. doi: 10.1006/ijom.2003.0512. [DOI] [PubMed] [Google Scholar]
- 4.Swan MC, Goodacre TE. Morbidity at the iliac crest donor site following bone grafting of the cleft alveolus. Br J Oral Maxillofac Surg. 2006;44(2):129–133. doi: 10.1016/j.bjoms.2005.04.. [DOI] [PubMed] [Google Scholar]
- 5.Ballantyne JC, Carr DB, deFerranti S, Suarez T, Lau J, Chalmers TC, Angelillo IF, Mosteller F. The comparative effects of postoperative analgesic therapies on pulmonary outcome: Cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86(3):598–612. doi: 10.1213/00000539-199803000-00032. [DOI] [PubMed] [Google Scholar]
- 6.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trials. BMJ. 2000;321(7275):1493. doi: 10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beirne JC, Barry HJ, Brady FA, Morris VB. Donor site morbidity of the anterior iliac crest following cancellous bone harvest. Int J Oral Maxillofac Surg. 1996;25(4):268–271. doi: 10.1016/S0901-5027(06)80053-6. [DOI] [PubMed] [Google Scholar]
- 8.Myeroff C, Archdeacon M. Autogenous bone graft: Donor sites and techniques. J Bone Joint Surg Am. 2011;93(23):2227–2236. doi: 10.2106/JBJS.J.01513. [DOI] [PubMed] [Google Scholar]
- 9.Wiltfang J, Schultze-Mosgau S, Nkenke E, Thorwarth M, Neukam FW, Schlegel KA. Onlay augmentation versus sinuslift procedure in the treatment of the severely resorbed maxilla: A 5-year comparative longitudinal study. Int J Oral Maxillofac Surg. 2005;34(8):885–889. doi: 10.1016/j.ijom.2005.04.026. [DOI] [PubMed] [Google Scholar]
- 10.O'Neill KR, Lockney DT, Bible JE, Crosby CG, Devin CJ. Bupivacaine for pain reduction after iliac crest bone graft harvest. Orthopedics. 2014;37(5):e428–e434. doi: 10.3928/01477447-20140430-52. [DOI] [PubMed] [Google Scholar]
- 11.Joshi A, Kostakis GC. An investigation of post-operative morbidity following iliac crest graft harvesting. Br Dent J. 2004;196(3):167–171. doi: 10.1038/sj.bdj.4810945. [DOI] [PubMed] [Google Scholar]
- 12.Racle JP, Benkhadra A, Poy JY, Gleizal B, Gaudray A. comparative study of general and spinal anesthesia in elderly women in hip surgery. Ann Fr Anesth Reanim. 1986;5(1):24–30. doi: 10.1016/s0750-7658(86)80118-6. [DOI] [PubMed] [Google Scholar]
- 13.Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999;230(2):251–259. doi: 10.1097/00000658-199908000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]


