Abstract
Study objective
We identify and characterize factors related to subsequent emergency revisits among children hospitalized for asthma.
Methods
This population-based, prospective, observational cohort included children aged 2 to 16 years, hospitalized for asthma at an urban pediatric facility and followed for greater than or equal to 12 months. The primary outcome was asthma-related emergency revisit within 12 months of discharge. Revisits were identified by billing codes, respiratory chief complaints, and medications administered (eg, albuterol, systemic corticosteroids), dispensed, or prescribed. Predictors and covariates include demographic, socioeconomic, access, and environmental exposure variables collected during index admission. Multivariable logistic regression was used to evaluate the association between predictors and odds of asthma-related revisit.
Results
A total of 671 children were enrolled; the majority were boys (65%), aged 4 to 11 years (59%), black (59%), and publicly insured (73%). There were 274 patients (41%) who were treated for asthma-related emergency revisits within 12 months of the index admission. In adjusted models, younger children, black children, children with excellent reported access to primary care, and children with a history of inhaled steroids were more likely to experience emergency revisits. Low income, detectable cotinine levels, and traffic exposure did not independently predict revisit.
Conclusion
Asthma-related emergency revisit is common after hospitalization, with more than 40% of children returning within 12 months. Socioeconomic and exposure-related risk factors typically predictive of asthma morbidity were not independently associated with emergency revisit among children in this cohort.
INTRODUCTION
Asthma is the most common chronic disease in pediatrics, affecting approximately 7 million children in the United States.1 Annually, there are 670,000 emergency department (ED) visits for acute asthma exacerbations for children nationally.2 Reasons for asthma-related ED utilization vary, but children more frequently present to the ED rather than to a primary care provider because of partly controlled or uncontrolled asthma,3,4 caregiver perception of acute severity,5 or lack of access to a medical home.6 Moreover, returning to the ED has been shown to be common after an initial emergency visit for an acute asthma exacerbation.7,8 In fact, asthma is the most common diagnosis for patients with greater than or equal to 4 emergency visits in a 12-month span.9 As many as 37% of children return to the ED within 6 months of their initial ED visit.10,11
Children of minority race and those with public insurance, history of asthma-related ED visit or hospitalization, and suboptimal asthma control are more likely to visit (and revisit) the ED.12–19 However, many studies describing risks related to ED utilization and reutilization have minimal patient-level data beyond these basic factors, elements that may aid in the discovery of modifiable ways to reduce asthma morbidity.20–23 Detailed patient-level predictors, including environmental exposures to tobacco24 or traffic,25 access to primary care,26 and specific financial and social hardships,27 have been shown to affect a patient’s risk of asthma-related rehospitalization after an index hospitalization. The effect of these measures on ED revisit after hospitalization is less clear. Additionally, all patients with ED visits do not have equally urgent symptoms; some could be categorized as truly urgent and others nonurgent.28 Traditional methods for identifying revisits (such as with International Classification of Diseases, Ninth Revision [ICD-9]/ICD-10 codes) do not yield insight into this severity of illness on presentation.
Thus, we first sought to characterize specific patient-level characteristics, including environmental exposures, access to care, and hardships, with risk of subsequent emergency revisits among children with an asthma-related index hospitalization. Second, we sought to describe the type of asthma-related revisit (ie, acute exacerbation versus nonacute asthma related). Finally, given well-documented disparities by race (higher ED utilization by black children), we examined racial differences in frequency of emergency revisits and severity at presentation.
MATERIALS AND METHODS
Study Design and Selection of Participants
The Greater Cincinnati Asthma Risk Study (GCARS) is a prospective population-based cohort study of children hospitalized for asthma and receiving oral steroids and β-agonists at Cincinnati Children’s Hospital Medical Center (CCHMC) between August 2010 and October 2011.27 For children aged 2 to 16 years, we evaluated emergency revisits subsequent to the index admission occurring during the following 12 months. Although GCARS enrolled children aged 1 to 2 years, we included in these analyses only patients older than 2 years to exclude any potential patients with bronchiolitis or nonasthma viral wheeze. Children were excluded from GCARS if the inpatient physician thought a diagnosis other than asthma was more likely and removed them from the asthma clinical pathway. Children were also excluded if they had significant nonasthma respiratory or cardiovascular disease (eg, cystic fibrosis, congenital heart disease), if they resided outside of CCHMC’s 8-county primary service area, or if their primary caregiver did not understand written or spoken English (≈2% of study sample). Further details on GCARS enrollment have been previously published.27 GCARS was approved by the CCHMC institutional review board.
Setting
CCHMC is a tertiary care academic medical center with greater than or equal to 140,000 annual emergency visits to the ED and urgent care sites combined. The locations at which patients may seek emergency care include an urban ED, a suburban ED, and 5 urgent care sites; all sites share a single electronic health record. Initial treatment for asthma at all 7 locations is protocolized and aligned with National Heart, Lung, and Blood Institute recommendations.20 Urgent care patients who require additional treatment are transferred to one of the 2 ED locations for continued outpatient care or admitted to CCHMC for inpatient care.
Outcome Measures
The primary outcome was any asthma-related emergency revisit (to any of the 7 locations) within 12 months of the patient’s index hospitalization. Emergency revisits were included in the outcome if the patient was readmitted or discharged home. Revisits were classified as acute exacerbations or nonacute asthma-related revisits (defined below). We chose a period of 12 months because of the chronicity of asthma, as well as its seasonal variation. Therefore, all patients were at risk for an emergency revisit for an entire year (across all seasons). For patients with multiple asthma-related revisits, the first one was included in this analysis. Secondary outcomes included severity of illness on emergency revisit presentation and the total number of asthma-related emergency visits.
Revisit data were obtained through a review of the electronic medical record. We examined revisits to determine whether they were asthma related and whether they were acute or nonacute. Revisits with any of the following were examined: ICD-9 code for asthma (493.XX) or wheeze (786.07), respiratory chief complaint, an albuterol order (administered, dispensed, or prescribed), or an order for systemic corticosteroids (administered or prescribed). We defined asthma-related emergency revisits (primary outcome) as those in which medications for asthma (either albuterol or systemic corticosteroids) were administered during the revisit or prescribed at discharge. Other revisits, including those that may have had an ICD-9 code for asthma but had no medications provided for asthma, were considered not asthma related and not included.
Once identified as asthma related, revisits were objectively dichotomized as acute exacerbations or nonacute asthma revisits according to the medications or prescriptions the patients received. Acute exacerbation revisits were defined as those including systemic corticosteroids as part of the treatment plan.29 This approach is consistent with that in previous literature, in which an expert working group defined an asthma exacerbation as “a worsening of asthma requiring the use of systemic corticosteroids to prevent a serious outcome.”29 Patients with documentation of systemic corticosteroids within the preceding 24 hours of the emergency revisit were also included in the acute exacerbation revisit category. Nonacute asthma revisits were defined as those in which the patient received either an albuterol dose or prescription but did not have systemic corticosteroids included as part of the treatment plan. This approach is consistent with previous literature in regard to categorization of an emergency visit as “asthma related” according to documented asthma medications administered or prescribed at the visit.30 Neither parental nor physician subjective impression of symptom severity was a factor in the categorization of revisits.
The range of severity for acute exacerbation revisits was then classified as mild, moderate, or severe to elucidate the necessity or potential preventability of the revisit. Severity was assessed through the first documented respiratory rate, oxygen saturation, and a respiratory score used at CCHMC. The respiratory score ranges from 0 to 8, according to physical examination findings of wheezing, air movement, respiratory rate (adjusted for age), accessory muscle use, and prolongation of expiration.31 Initial respiratory scores of less than or equal to 2 are clinically considered to be absent or mild exacerbations, scores of 3 to 5 are considered moderate exacerbations, and those greater than or equal to 6 are considered severe exacerbations. Standard criteria for discharge to home include respiratory scores less than or equal to 2 after a period of observation after initial treatment for asthma symptoms.
We obtained detailed data on patient characteristics from a face-to-face survey with the primary caregivers for all enrolled patients during the index hospitalization. Caregivers reported basic demographic and socioeconomic information about the patient and family (eg, patient age, sex, insurance, race, caregiver income, educational attainment). Questions also assessed past use of inhaled corticosteroids as a marker of asthma severity, caregiver work or school schedule, and markers of financial and social hardships.27 Perceived access to medical care was evaluated by the access subscale of the Parents’ Perceptions of Primary Care scale.32 We scored the subscale as previously described,26 with an average score corresponding to “always adequate” as perfect (score=100), average score corresponding to “almost always adequate” (score 75 to 99), or average score corresponding to “often/sometimes/never adequate” (score <75). We also collected salivary cotinine to obtain an objective measure of secondhand tobacco exposure in the home or car environment. Salivary cotinine is a metabolite of nicotine with a half-life of approximately 16 hours.33 Details of the collection and processing of specimens have been described previously.24 Finally, traffic-related air pollution was quantified with a land-use regression model that allows estimation of exposure at the patient’s street address.25,34,35
Primary Data Analysis
We used descriptive statistics to illustrate frequencies of asthma-related emergency revisits (total, acute exacerbations, and nonacute revisits). We also classified severity on presentation for the revisits classified as acute. We performed logistic regression analyses to examine the association of patient characteristics with asthma-related emergency revisits. Nearly all predictors and covariates were included in our multivariable analyses. Models did not include the questions about visiting or calling the primary care provider because these were thought to be conceptually related to the Parents’ Perceptions of Primary Care scale. We also did not include source of usual asthma care because a caregiver report of using the ED for asthma seemed less useful. Finally, caregiver work or school schedule was excluded from multivariable analysis because this factor was considered to be exploratory and was not found to be significant in bivariate analysis. We also performed additional sensitivity analyses modeling time to first emergency revisit, using Cox proportional hazards. Given documented racial disparities for ED visitation after hospitalization, we performed bivariate analyses to investigate severity of illness of acute asthma revisits by race. Finally, given the paradoxic relationship between access to care and asthma use, we performed a post hoc descriptive analysis of how access was rated by source of asthma care. All analyses were performed with SAS (version 9.3; SAS Institute, Inc., Cary, NC).
RESULTS
Of the 671 enrolled children, most were aged 4 to 11 years (59%), boys (65%), black (59%), and publicly insured (73%). A total of 62% reported an annual household income of less than $30,000, and 28% reported that they did not have enough money at the end of the month to make ends meet. Most children (58%) had been receiving inhaled corticosteroids at some point in the preceding year. Most children (79%) had detectable levels of salivary cotinine. Finally, 19% of caregivers reported that their children had perfect primary care access (Table 1).
Table 1.
Characteristics of enrolled children and bivariate associations with asthma-related revisits within 12 months.
| Patient Characteristic | Percentage of Overall Cohort Distribution, n=671 | Percentage of Children With an Asthma-Related Revisit in 12 Months, n=274 | Odds Ratio of an Asthma-Related Revisit (95% CI) |
|---|---|---|---|
| Age, y | |||
| 2–3 | 28.8 | 43.5 | 2.07 (1.17–3.64)* |
| 4–11 | 59.2 | 42.3 | 1.97 (1.16–3.34)* |
| ≥12 | 12.1 | 27.2 | 1 [Reference] |
| Sex | |||
| Female | 34.6 | 38.4 | 0.85 (0.62–1.18) |
| Male | 65.4 | 42.1 | 1 [Reference] |
| Race | |||
| White | 32.0 | 30.8 | 1 [Reference] |
| Black | 58.5 | 47.6 | 2.03 (1.43–2.89)* |
| Multiracial/other | 9.4 | 31.8 | 1.04 (0.57–1.91) |
| Health insurance | |||
| Private | 23.3 | 24.0 | 1 [Reference] |
| Public | 73.2 | 46.2 | 2.71 (1.80–4.09)* |
| Self-pay | 3.5 | 26.1 | 1.11 (0.41–3.04) |
| Annual household income, $ | |||
| <14,999 | 33.5 | 46.4 | 1 [Reference] |
| 15,000–29,000 | 28.1 | 44.6 | 0.93 (0.63–1.38) |
| 30,000–44,999 | 14.7 | 42.3 | 0.85 (0.52–1.37) |
| 45,000–59,999 | 6.0 | 35.0 | 0.62 (0.31–1.25) |
| 60,000–89,999 | 10.3 | 32,4 | 0.55 (0.31–0.98)* |
| >90,000 | 7.4 | 12.2 | 0.16 (0.67–0.39)* |
| Caregiver educational attainment | |||
| Less than high school | 15.8 | 54.3 | 2.77 (1.56–4.92)* |
| High school graduate | 28.1 | 41.7 | 1.67 (1.00–2.80) |
| Some college | 28.5 | 39.5 | 1.52 (0.97–2.55) |
| 2-year college | 12.6 | 36.9 | 1.37 (0.74–2.53) |
| 4-year college or above | 15.0 | 30.0 | 1 [Reference] |
| Caregiver marital status | |||
| Single | 61.4 | 45.1 | 1 [Reference] |
| Married | 28.3 | 30.7 | 0.54 (0.37–0.78)* |
| Divorced/widowed/separated | 10.3 | 42.0 | 0.88 (0.53–1.48) |
| Money left over at the end of the month | |||
| Some money left over | 33.4 | 35.0 | 1 [Reference] |
| Just enough money to make ends meet | 38.7 | 43.4 | 1.43 (0.99–2.06) |
| Not enough money to make ends meet | 27.9 | 43.6 | 1.43 (0.96–2.14) |
| Vehicle ownership | |||
| Yes | 72.2 | 37.2 | 1 [Reference] |
| No | 27.8 | 50.3 | 1.71 (1.21–2.40)* |
| Previous inhaled corticosteroids | |||
| Yes | 58.2 | 46.3 | 1.77 (1.28–2.44)* |
| No | 41.8 | 32.7 | 1 [Reference] |
| Source of usual asthma care | |||
| Primary care or clinic provider | 44.5 | 39.5 | 1 [Reference] |
| ED or urgent care | 51.2 | 48.5 | 1.44 (1.02–2.02)* |
| Asthma specialist | 4.2 | 33.3 | 0.77 (0.32–1.85) |
| Visited primary care provider in past week | |||
| Yes | 19.1 | 35.3 | 0.74 (0.50–1.11) |
| No | 80.9 | 42.2 | 1 [Reference] |
| Called primary care provider in past week | |||
| Yes | 31.5 | 38.9 | 0.89 (0.64–1.24) |
| No | 68.6 | 41.7 | 1 [Reference] |
| Caregiver work/school schedule | |||
| Day shift (6 AM–6 PM) | 44.0 | 39.8 | 1 [Reference] |
| Evening shift (2 PM–midnight) | 5.7 | 39.5 | 0.99 (0.49–1.97) |
| Night shift (9 PM–8 AM) | 4.5 | 43.3 | 1.16 (0.54–2.47) |
| Variable (changing shifts) | 16.5 | 34.6 | 0.80 (0.51–1.26) |
| Does not work outside the home | 29.3 | 45.4 | 1.26 (0.87–1.81) |
| Saliva cotinine level above the limit of detection | |||
| Yes | 79.4 | 43.2 | 1 [Reference] |
| No | 20.6 | 28.4 | 0.52 (0.34–0.80)* |
| Traffic pollution greater than median† | |||
| Yes | 49.3 | 44.1 | 1.28 (0.94–1.75) |
| No | 50.7 | 38.1 | 1 [Reference] |
| Access to primary care (P3C score) | |||
| Perfect access (100) | 19.1 | 48.4 | 1.22 (0.80–1.87) |
| Almost always adequate access (75–100) | 44.3 | 35.4 | 0.71 (0.50–1.01) |
| Less than almost always adequate access (<75) | 36.7 | 43.5 | 1 [Reference] |
P3C, Parents’ Perceptions of Primary Care scale.
CIs represent statistical significance.
Measured by emissions attributable to carbon.
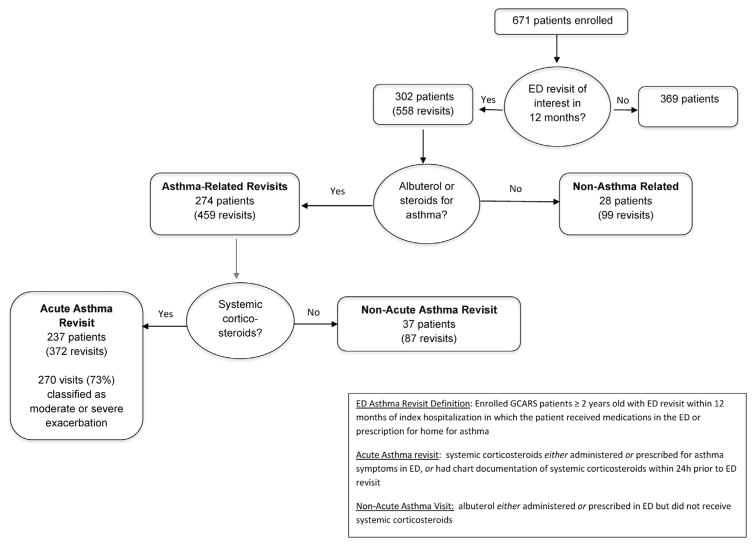
Within 12 months of discharge, there were a total of 558 emergency revisits from 302 enrolled children. After further review, 459 (82%) of these visits were found to be consistent with visits in which children received care consistent with treatment for asthma. The remaining visits were for different concerns (eg, broken arm), but asthma was included in billing codes. The majority of asthma-related revisits (n=372; 81%) were classified as acute exacerbations according to our a priori definition (receiving systemic corticosteroids) (Figure 1). No revisits were planned. Of the 372 emergency revisits classified as acute, the majority (73%) were classified as moderate to severe exacerbation (Figure 1).
Figure 1.
Emergency revisits within 12 months of index hospitalization (≥2 years).
A 25% subsample of all patients enrolled was contacted by telephone approximately 12 months after the index admission to assess potential loss to follow-up or ED utilization at non-CCHMC sites.27 Of patients who reported using the ED, 7 of 49 revisits were to non-CCHMC sites.
Multiple factors had a bivariate association with asthma-related emergency revisit in the patient-level analysis (Table 1). For example, black children were significantly more likely to experience an emergency revisit, with an odds ratio of 2.03 (95% confidence interval [CI] 1.43 to 2.89). Similarly, patients with public insurance had increased odds of an emergency revisit (odds ratio 2.71; 95% CI 1.80 to 4.09). Younger children, lower caregiver educational attainment, and no vehicle ownership were also more likely to mean an asthma-related emergency visit. Families who reported higher income had lower odds of readmission. Increased odds of emergency revisit were also observed for children who had been receiving inhaled corticosteroids and those who reported using the ED as their usual source of asthma care. Finally, tobacco smoke exposure (ie, detectable salivary cotinine levels) showed an association with revisit in the expected direction.
In multivariable logistic regression analyses, younger children (2 to 3 years) had the highest odds of an asthma-related revisit compared with children aged 12 years or older (adjusted odds ratio 2.24; 95% CI 1.16 to 4.32) (Table 2). Black children had higher odds of revisit compared with white children (adjusted odds ratio 1.67; 95% 1.04 to 2.66). Children who had not been receiving inhaled corticosteroids in the past year had lower odds of revisit compared with those who had been receiving inhaled corticosteroids (adjusted odds ratio 0.56; 95% CI 0.38 to 0.82). Contrary to what was hypothesized, however, children who reported perfect access to primary care had higher odds of revisitation compared with those with suboptimal access (adjusted odds ratio 1.89; 95% CI 1.11 to 3.21). The time-to-event sensitivity analysis revealed similar results, with age, previous steroid use, primary care access, and lower income showing significant relationships with time to first revisit.
Table 2.
Adjusted odds ratios for asthma-related revisits within 12 months in multivariable logistic regression.*
| Patient Characteristic | Adjusted Odds Ratio | 95% CI |
|---|---|---|
| Age, y | ||
| 2–3 | 2.24 | (1.16–4.32) |
| 4–11 | 2.20 | (1.20–4.02) |
| ≥12 | 1 [Reference] | 1 [Reference] |
| Race | ||
| White | 1 [Reference] | 1 [Reference] |
| Black | 1.67 | (1.04–2.66) |
| Multiracial/other | 0.78 | (0.38–1.59) |
| Previous inhaled steroids | ||
| Yes | 1 [Reference] | 1 [Reference] |
| No | 0.56 | (0.38–0.82) |
| Access to primary care (Parents’ Perceptions of Primary Care scale) | ||
| 100 (perfect) | 1.89 | (1.11–3.21) |
| 75–99 | 0.89 | (0.60–1.34) |
| <75 | 1 [Reference] | 1 [Reference] |
Model includes sex, insurance, income, caregiver education, caregiver marital status, money left over at the end of the month, vehicle ownership, salivary cotinine level, and traffic pollution.
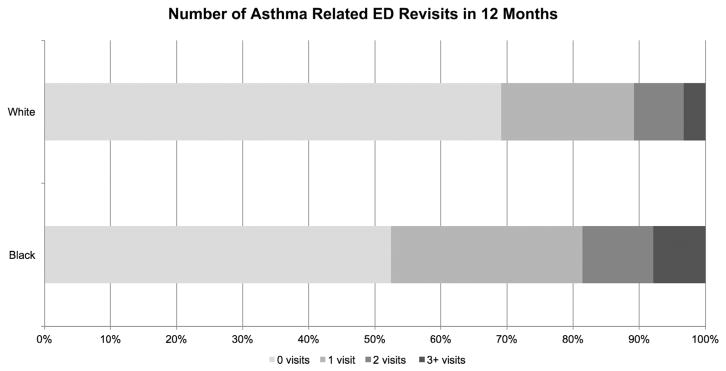
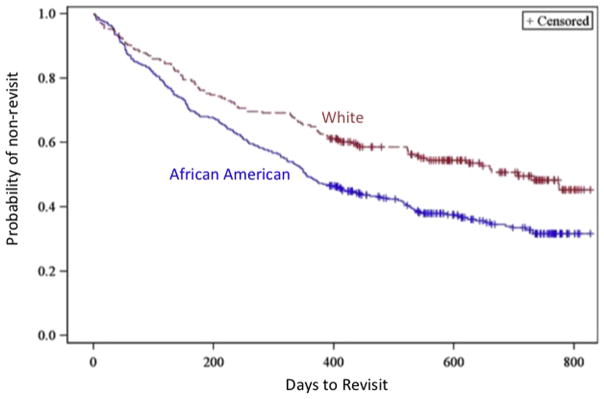
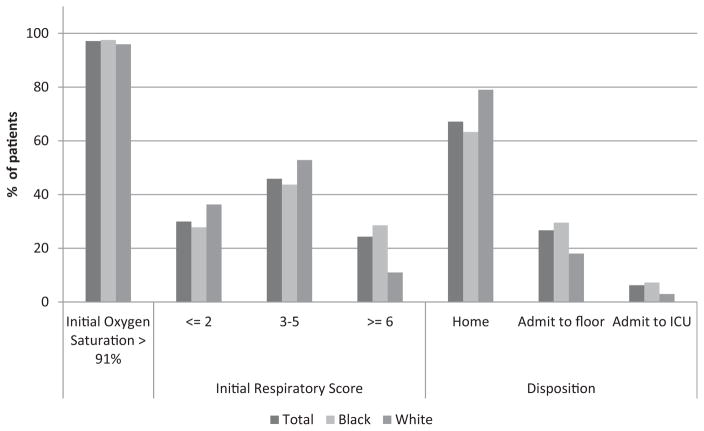
Black children were more likely to have greater than or equal to 2 revisits within 12 months of the index hospitalization than whites (18.6% versus 10.8%) (Figure 2). Black children revisited earlier than white children (Figure 3). Hypoxia on presentation (oxygen saturation ≤91%) was similar between white and black children (overall, 3% were hypoxic). Presenting respiratory score (proxy for acute severity) differed by race, with 44% of visits for black children in the moderate range and 29% in the severe category compared with 53% of visits for white children in the moderate range and 11% in the severe range (P<.01). Black children were more frequently admitted to the floor (30%) or ICU (7%) than white children (floor 18%; ICU 3%; P<.05) (Figure 4).
Figure 2.
Number of asthma-related ED revisits by race.
Figure 3.
Time to asthma-related ED revisit by race.
Figure 4.
Severity of illness on presentation for asthma-related ED revisits.
Given the paradoxic relationship between access to care and revisits, we examined the relationship between access to care and source of care. Of the caregivers who stated their usual source of asthma care to be the ED, 14% rated their access as perfect, 38% rated it as almost always adequate, and 47% rated their access as often, sometimes, or never adequate. In contrast, of the caregivers who stated their usual source of asthma care is their primary care provider, 23% rated their access as perfect, 52% rated it as almost always adequate, and 25% rated their access as often, sometimes, or never adequate.
LIMITATIONS
Our study should be considered in the context of several limitations. First, our outcome data are limited to emergency revisits in the CCHMC system; therefore, some children may have been lost to follow-up. In our 12-month follow-up, 7 of 49 people who used the ED reported using other EDs; still, our institution dominates the pediatric emergency and hospital market locally. Second, although our caregiver surveys used previously developed questions, given the face-to-face administration of the survey, caregivers’ responses were subject to social desirability bias. We expect this to have been nondifferential across groups who did or did not revisit the ED. Additionally, although our respiratory scoring system is widely deployed and has been routinely used across CCHMC for more than a decade, formal validity testing has not been performed; therefore, our severity-of-illness assessments are limited to clinical care assessments. Third, the use of logistic regression yields information on correlation and not causation.
DISCUSSION
Asthma-related emergency revisits are common after hospitalization for an asthma exacerbation; more than 4 in 10 children within our cohort returned within 1 year. The majority of asthma-related revisits were for acute exacerbations necessitating treatment with systemic corticosteroids and not for nonurgent complaints. Indeed almost 3 in 4 children revisiting an emergency care site for an acute exacerbation after a hospitalization were moderately or severely ill on presentation. In multivariable analyses, young age, black race, better primary care access, and previous inhaled corticosteroid use were associated with increased odds of emergency care revisit. Surprisingly, variables including low income, detectable cotinine level, and traffic-related air pollution exposure were not found to be independently associated with our outcome.
Black children were more likely to have emergency revisits compared with white children. This finding is consistent with our previous work assessing relationships between index hospitalization and asthma-related rehospitalization.27,36 Moreover, bivariate analyses suggest that black children are more likely than white ones to return for asthma-related revisits multiple times. Although black children were more likely to have multiple asthma-related revisits than white children, this does not appear to be related to overuse or misuse of the emergency setting (ie, children presenting when not ill). In fact, black children on revisits had significantly higher respiratory scores on presentation and were more likely to be admitted than white children.
Children with public insurance and those with a previous prescription for inhaled corticosteroids had higher odds of emergency care revisit in multivariable logistic regression. Also, contrary to previous findings on asthma hospital readmission,26 children with perfect primary care access scores actually had higher odds of emergency revisit in adjusted analyses. These findings may be related to severity of underlying disease. In previous work, children with “not well-controlled” asthma (as reflected by validated asthma control test scores) had an approximately 5-fold greater risk for asthma-related primary care ill visits, as well as ED visits, compared with those with well-controlled asthma.4 Here, children who have been receiving inhaled corticosteroids in the past have higher odds of emergency revisitation; these children likely also have more severe disease, representing a type of confounding by indication. Similarly, caregivers of children who are prone to frequent emergency exacerbations may seek out easily accessible primary care providers; thus, rating of access may, too, be partially capturing asthma severity. Additionally, the Parents’ Perceptions of Primary Care metric asks families to consider “the person your child sees for health care….”32 Some patients preferentially use the ED as their source of asthma care. These caregivers may rate their access as excellent (because the ED is always open and accessible). This would be in line with our post hoc finding that 14% of children who use the ED as their source of asthma rated their access as perfect.
Our data confirm that emergency care revisits after asthma hospitalizations are common.8 Given the movement to episode-based payments (ie, a single payment for a period of care regardless of cost accrued during that period), it is worth considering and evaluating strategies to decrease such revisits. Educating caregivers about pediatric asthma has been shown to decrease the mean number of hospitalizations and ED visits.37 Qualitative interviews with patients and caregivers have revealed opportunities for improvement in ED discharge instructions, including use of simplified language and increased visual learning (with opportunity for demonstrations and “teach-back”).38
There are also documented cost-effective successes within communities to improve health outcomes and decrease emergency visits for asthma,39 yet these interventions are frequently labor and time intensive, complicating their implementation on a large scale. Hospital-based discharge interventions, which include enhanced education for children with asthma, have shown mixed effects (ie, some show no difference in revisitation, some show decreased revisits, and one showed increased revisits).40 Furthermore, increased asthma knowledge has been shown to be associated with increased odds of readmission after an asthma discharge.41 Thus, it is unclear whether asthma education is the best intervention or whether during a severe acute illness (requiring a hospitalization or ED visit) is the best time for that education.42 Another potential strategy to decrease emergency care visits after hospitalization may be to increase prescribing and dispensing of inhaled corticosteroids at hospital (or ED) discharge. Such a strategy has already been shown to be cost-effective in the ED setting,43 yet in the hectic emergency environment, the additional tasks of categorizing the patient’s chronic asthma control level and appropriately prescribing an inhaled corticosteroid, coupled with provision of an updated written asthma action plan, can be challenging.7,44–46
Locally, we have a broad ongoing asthma quality improvement collaborative to increase dispensing inhaled corticosteroids for home use in the inpatient setting when the patient is prescribed steroids.47 Additionally, physicians are prompted to ask about long-term level of control for all children admitted with asthma.48 Further work in ensuring that all children who would benefit from inhaled corticosteroids are prescribed them at discharge may prevent posthospital emergency health care use. Continued targeted efforts within these identified specific subpopulations (eg, those of younger age) at high risk for revisits may also be warranted, given the lack of decline of ED visits during the past decade, coupled with the high rate of revisits for asthma.49
Emergency revisits for asthma exacerbations are common after an asthma-related hospitalization. The majority of children who revisit the ED and urgent care sites for acute asthma symptoms are experiencing exacerbations and are moderately to severely ill. Young children, black children, and those receiving inhaled steroids are at increased odds of any asthma-related emergency revisitation. Finally, socioeconomic and exposure-related risk factors typically predictive of asthma morbidity were not independently associated with emergency revisit among children in this cohort.
Editor’s Capsule Summary
-
What is already known on this topic
Most studies examining emergency department (ED) utilization for asthma are retrospective and do not have patient-level and environmental data.
-
What question this study addressed
What factors are associated with ED and urgent care utilization after an asthma hospitalization?
-
What this study adds to our knowledge
In this study of 671 children, socioeconomic status, access to primary care, and exposure-related risk factors typically predictive of asthma morbidity were not associated ED revisit utilization.
-
How this is relevant to clinical practice
ED visits for asthma after hospitalization are common and may be related to severity of disease.
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. The Greater Cincinnati Asthma Risk Study was funded by a grant from the National Institutes of Health (NIH) to Dr. Kahn (1R01AI88116). Dr. Beck received funding from the NIH through a career development award (1K23AI112916).
Footnotes
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author contributions: LHJ, AFB, RSK, BH, PHR, and KAA conceived the study. AFB and RSK obtained funding. LHJ, RSK, and BH supervised the data collection and managed the data, including quality control. BH and PHR provided statistical advice on study design. BH analyzed data. LHJ and KAA drafted the article, and all authors contributed substantially to its revision. LHJ takes responsibility for the paper as a whole.
References
- 1.Bloom B, Jones LI, Freeman G. Summary health statistics for US children: National Health Interview Survey, 2012. Vital Health Stat 10. 2013;258:1–81. [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. Natl Health Stat Report. 2011;32:1–14. [PubMed] [Google Scholar]
- 3.Gold LS, Smith N, Allen-Ramey FC, et al. Associations of patient outcomes with level of asthma control. Ann Allergy Asthma Immunol. 2012;109:260–265. doi: 10.1016/j.anai.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Guilbert TW, Garris C, Jhingran P, et al. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J Asthma. 2011;48:126–132. doi: 10.3109/02770903.2010.535879. [DOI] [PubMed] [Google Scholar]
- 5.Still L, Dolen WK. The perception of asthma severity in children. Curr Allergy Asthma Rep. 2016;16:50. doi: 10.1007/s11882-016-0629-2. [DOI] [PubMed] [Google Scholar]
- 6.Costet Wong A, Claudet I, Sorum P, et al. Why do parents bring their children to the emergency department? a systematic inventory of motives. Int J Family Med. 2015;2015:1–10. doi: 10.1155/2015/978412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwok MY, Walsh-Kelly CM, Gorelick MH, et al. National Asthma Education and Prevention Program severity classification as a measure of disease burden in children with acute asthma. Pediatrics. 2006;117:S71–S77. doi: 10.1542/peds.2005-2000D. [DOI] [PubMed] [Google Scholar]
- 8.Tolomeo C, Savrin C, Heinzer M, et al. Predictors of asthma-related pediatric emergency department visits and hospitalizations. J Asthma. 2009;46:829–834. [PubMed] [Google Scholar]
- 9.Alpern ER, Clark AE, Alessandrini EA, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21:365–373. doi: 10.1111/acem.12347. [DOI] [PubMed] [Google Scholar]
- 10.Spurrier NJ, Staugas R, Sawyer MG, et al. Health-service use by children with asthma over a 6-month period. J Paediatr Child Health. 2003;39:15–21. doi: 10.1046/j.1440-1754.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 11.To T, Wang C, Dell S, et al. Risk factors for repeat adverse asthma events in children after visiting an emergency department. Ambul Pediatr. 2008;8:281–287. doi: 10.1016/j.ambp.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Butz AM, Eggleston P, Alexander C, et al. Outcomes of emergency room treatment of children with asthma. J Asthma. 1991;28:255–264. doi: 10.3109/02770909109073382. [DOI] [PubMed] [Google Scholar]
- 13.Ducharme FM, Kramer MS. Relapse following emergency treatment for acute asthma: can it be predicted or prevented? J Clin Epidemiol. 1993;46:1395–1402. doi: 10.1016/0895-4356(93)90139-r. [DOI] [PubMed] [Google Scholar]
- 14.Emerman CL, Woodruff PG, Cydulka RK, et al. Prospective multicenter study of relapse following treatment for acute asthma among adults presenting to the emergency department. MARC Investigators. Multicenter Asthma Research Collaboration. Chest. 1999;115:919–927. doi: 10.1378/chest.115.4.919. [DOI] [PubMed] [Google Scholar]
- 15.Guttmann A, Zagorski B, Austin PC, et al. Effectiveness of emergency department asthma management strategies on return visits in children: a population-based study. Pediatrics. 2007;120:e1402–e1410. doi: 10.1542/peds.2007-0168. [DOI] [PubMed] [Google Scholar]
- 16.Stevens MW, Gorelick MH. Short-term outcomes after acute treatment of pediatric asthma. Pediatrics. 2001;107:1357–1362. doi: 10.1542/peds.107.6.1357. [DOI] [PubMed] [Google Scholar]
- 17.To T, Dick P, Feldman W, et al. A cohort study on childhood asthma admissions and readmissions. Pediatrics. 1996;98:191–195. [PubMed] [Google Scholar]
- 18.Walsh-Kelly CM, Kelly KJ, Drendel AL, et al. Emergency department revisits for pediatric acute asthma exacerbations: association of factors identified in an emergency department asthma tracking system. Pediatr Emerg Care. 2008;24:505–510. doi: 10.1097/PEC.0b013e318180fdcb. [DOI] [PubMed] [Google Scholar]
- 19.Wasilewski Y, Clark NM, Evans D, et al. Factors associated with emergency department visits by children with asthma: implications for health education. Am J Public Health. 1996;86:1410–1415. doi: 10.2105/ajph.86.10.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Heart, Lung, and Blood Institute (NHLBI) Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 21.Diedhiou A, Probst JC, Hardin JW, et al. Relationship between presence of a reported medical home and emergency department use among children with asthma. Med Care Res Rev. 2010;67:450–475. doi: 10.1177/1077558710367735. [DOI] [PubMed] [Google Scholar]
- 22.Kim H, Kieckhefer GM, Greek AA, et al. Health care utilization by children with asthma. Prev Chronic Dis. 2009;6:A12. [PMC free article] [PubMed] [Google Scholar]
- 23.Christakis DA, Mell L, Koepsell TD, et al. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107:524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 24.Howrylak JA, Spanier AJ, Huang B, et al. Cotinine in children admitted for asthma and readmission. Pediatrics. 2014;133:e355–e362. doi: 10.1542/peds.2013-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newman NC, Ryan PH, Huang B, et al. Traffic-related air pollution and asthma hospital readmission in children: a longitudinal cohort study. J Pediatr. 2014;164:1396–1402. doi: 10.1016/j.jpeds.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Auger KA, Kahn RS, Davis MM, et al. Medical home quality and readmission risk for children hospitalized with asthma exacerbations. Pediatrics. 2013;131:64–70. doi: 10.1542/peds.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AF, Huang B, Simmons JM, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133:431–439. doi: 10.1542/peds.2013-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stanley R, Zimmerman J, Hashikawa C, et al. Appropriateness of children’s nonurgent visits to selected Michigan emergency departments. Pediatr Emerg Care. 2007;23:532–536. doi: 10.1097/PEC.0b013e318128f84a. [DOI] [PubMed] [Google Scholar]
- 29.Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129:S34–S48. doi: 10.1016/j.jaci.2011.12.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nelson KA, Garbutt JM, Wallendorf MJ, et al. Primary care visits for asthma monitoring over time and association with acute asthma visits for urban Medicaid-insured children. J Asthma. 2014;51:907–912. doi: 10.3109/02770903.2014.927483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Acute Asthma Guideline, Cincinnati Children’s Hospital Medical Center. Evidence-based care guideline for management of acute asthma exacerbation in children. Asthma Exacerbation in Children Pediatric Evidence Base Care Guidelines, Cincinnati Children’s Hospital Medical Center, Guideline. 2010 Sep 16;4:1–35. [Google Scholar]
- 32.Seid M, Varni JW, Bermudez LO, et al. Parents’ Perceptions of Primary Care: measuring parents’ experiences of pediatric primary care quality. Pediatrics. 2001;108:264–270. doi: 10.1542/peds.108.2.264. [DOI] [PubMed] [Google Scholar]
- 33.Benowitz NL. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol Rev. 1996;18:188–204. doi: 10.1093/oxfordjournals.epirev.a017925. [DOI] [PubMed] [Google Scholar]
- 34.Ryan PH, Lemasters GK, Biswas P, et al. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect. 2007;115:278–284. doi: 10.1289/ehp.9480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryan PH, Lemasters GK, Levin L, et al. A land-use regression model for estimating microenvironmental diesel exposure given multiple addresses from birth through childhood. Sci Total Environ. 2008;404:139–147. doi: 10.1016/j.scitotenv.2008.05.051. [DOI] [PubMed] [Google Scholar]
- 36.Beck AF, Huang B, Auger KA, et al. Explaining racial disparities in child asthma readmission using a causal inference approach. JAMA Pediatr. 2016;170:695–703. doi: 10.1001/jamapediatrics.2016.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coffman JM, Cabana MD, Halpin HA, et al. Effects of asthma education on children’s use of acute care services: a meta-analysis. Pediatrics. 2008;121:575–586. doi: 10.1542/peds.2007-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samuels-Kalow M, Hardy E, Rhodes K, et al. “Like a dialogue”: teach-back in the emergency department. Patient Educ Couns. 2016;99:549–554. doi: 10.1016/j.pec.2015.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woods ER, Bhaumik U, Sommer SJ, et al. Community asthma initiative: evaluation of a quality improvement program for comprehensive asthma care. Pediatrics. 2012;129:465–472. doi: 10.1542/peds.2010-3472. [DOI] [PubMed] [Google Scholar]
- 40.Auger KA, Kenyon CC, Feudtner C, et al. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review. J Hosp Med. 2014;9:251–260. doi: 10.1002/jhm.2134. [DOI] [PubMed] [Google Scholar]
- 41.Auger KA, Kahn RS, Davis MM, et al. Pediatric asthma readmission: asthma knowledge is not enough? J Pediatr. 2015;166:101–108. doi: 10.1016/j.jpeds.2014.07.046. [DOI] [PubMed] [Google Scholar]
- 42.Boyd M, Lasserson TJ, McKean MC, et al. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev. 2009;(2):CD001290. doi: 10.1002/14651858.CD001290.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Andrews AL, Teufel RJ, 2nd, Basco WT, Jr, et al. A cost-effectiveness analysis of inhaled corticosteroid delivery for children with asthma in the emergency department. J Pediatr. 2012;161:903–907. doi: 10.1016/j.jpeds.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 44.Garro AC, Asnis L, Merchant RC, et al. Frequency of prescription of inhaled corticosteroids to children with asthma in US emergency departments. Acad Emerg Med. 2011;18:767–770. doi: 10.1111/j.1553-2712.2011.01117.x. [DOI] [PubMed] [Google Scholar]
- 45.Lovinsky S, Rastogi D. Prescription habits for preventative medications among pediatric emergency department physicians at an inner-city teaching hospital. J Asthma. 2010;47:1011–1014. doi: 10.1080/02770903.2010.491138. [DOI] [PubMed] [Google Scholar]
- 46.Ly CD, Dennehy CE. Emergency department management of pediatric asthma at a university teaching hospital. Ann Pharmacother. 2007;41:1625–1631. doi: 10.1345/aph.1K138. [DOI] [PubMed] [Google Scholar]
- 47.McCarthy D, Cohen A. The Cincinnati Children’s Hospital Medical Center’s Asthma Improvement Collaborative: enhancing quality and coordination of care. [Accessed November 23, 2015];Case study: innovations in care transitions. 2013 Available at: http://www.commonwealthfund.org/~/media/Files/Publications/Case%20Study/2013/Jan/1660_McCarthy_care_transitions_Cincinnati_case_study_v2.pdf.
- 48.Beck AF, Sauers HS, Kahn RS, et al. Improved documentation and care planning with an asthma-specific history and physical. Hosp Pediatr. 2012;2:194–201. doi: 10.1542/hpeds.2012-0016. [DOI] [PubMed] [Google Scholar]
- 49.Nath JB, Hsia RY. Children’s emergency department use for asthma, 2001–2010. Acad Pediatr. 2015;15:225–230. doi: 10.1016/j.acap.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]