Abstract
Background
Two decades ago, hypotensive trauma patients requiring emergent laparotomy had a 40% mortality. In the interim, multiple interventions to decrease hemorrhage-related mortality have been implemented but few have any documented evidence of change in outcomes for patients requiring emergent laparotomy. The purpose of this study was to determine current mortality rates for patients undergoing emergent trauma laparotomy.
Methods
A retrospective cohort of all adult, emergent trauma laparotomies performed in 2012–2013 at 12 Level I trauma centers was reviewed. Emergent trauma laparotomy was defined as emergency department (ED) admission to surgical start time in ≤90 minutes. Hypotension was defined as arrival ED systolic blood pressure (SBP) ≤90 mmHg. Cause and time to death was also determined. Continuous data are presented as median [IQR].
Results
1,706 patients underwent emergent trauma laparotomy. The cohort was predominately young (31 years [24, 45]), male (84%), sustained blunt trauma (67%), and with moderate injuries (ISS 19 [10, 33]). The time in ED was 24 minutes [14, 39] and time from ED admission to surgical start was 42 minutes [30, 61]. The most common procedures were enterectomy (23%), hepatorrhaphy (20%), enterorrhaphy (16%), and splenectomy (16%). Damage control laparotomy was utilized in 38% of all patients and 62% of hypotensive patients. The Injury Severity Score for the entire cohort was 19 (IQR 10, 33) and 29 (IQR 18, 41) for the hypotensive group. Mortality for the entire cohort was 21% with 60% of deaths due to hemorrhage. Mortality in the hypotensive group was 46%, with 65% of deaths due to hemorrhage.
Conclusion
Overall mortality rate of a trauma laparotomy is substantial (21%) with hemorrhage accounting for 60% of the deaths. The mortality rate for hypotensive patients (46%) appears unchanged over the last two decades and is even more concerning, with almost half of patients presenting with a SBP ≤ 90 mmHg dying.
Level of Evidence
Level III (retrospective epidemiologcal study with up to two negative criteria)
Keywords: trauma, laparotomy, mortality, hypotension
BACKGROUND
Hemorrhage is a major cause of early death in trauma patients and accounts for the greatest number of preventable trauma deaths.1 Emergent laparotomy is a necessary treatment for intra-abdominal hemorrhage and substantial effort has been expended to streamline the rapid delivery of life-saving interventions.2,3
In a multicenter cohort of patients from 1986–1999, the mortality rate for hypotensive trauma patients undergoing laparotomy was reported to be 40%.4 Since that report, many interventions purported to decrease mortality in these patients have been described, including decreasing time to hemorrhage control, damage control resuscitation, damage control surgery, controlled resuscitation, massive transfusion protocols, bedside ultrasonography, and angioembolization.5,6,7,8
The purpose of this study was to determine the current mortality rate and cause of death for hypotensive trauma patients undergoing emergent laparotomy. We hypothesize that mortality rates in this group would have decreased over the interim years.
METHODS
Twelve Level 1 United States trauma centers participated in this project: the University of Texas McGovern Medical School at Houston (Houston, Texas), the University of Southern California Keck School of Medicine (Los Angeles, California), the Harvard Medical School (Boston, Massachusetts), Mayo Clinic (Rochester, Minnesota), the Baylor College of Medicine (Houston, Texas), the University of Alabama School of Medicine (Birmingham, Alabama), the Rutgers New Jersey Medical School (Newark, New Jersey), the University of Maryland School of Medicine (Baltimore, Maryland), the University of Washington, Harborview Medical Center (Seattle, Washington), the West Virginia University School of Medicine (Morgantown, West Virginia), the Oregon Health & Science University (Portland, Oregon), and the University of Michigan Medical School (Ann Arbor, Michigan).
After each institution obtained Institutional Review Board approval, the trauma registry of each site was queried for adult (age >16), emergency laparotomies from January 1, 2012 through December 31, 2013. Emergent laparotomy was defined as emergency department admission to surgical start in less than or equal to 90 minutes.4 First, a descriptive analysis of all patients was performed. Next, two groups were compared – patients presenting without hypotension (systolic blood pressure >90mmHg) and patients presenting with hypotension (systolic blood pressure ≤90 mmHg).
Patient demographics, injury characteristics, prehospital vital signs, emergency department vital signs, laboratory values, resuscitation volumes, regional Abbreviated Injury Scores (AIS), Injury Severity Score (ISS), and operative details were recorded. The primary outcome was in-hospital mortality. Secondary outcomes included cause of death, time to death, and hospital-free days. Hospital-free days were defined as days alive and not admitted to the hospital (30 – total hospital days = hospital-free days). For those that died prior to 30 days and had no days free of the hospital, this was recorded as 0. For those that had lengths of stay longer than 30 days, this was recorded as 0.
Continuous data are presented as medians with 25th to 75th interquartile range (IQR). Categorical data are presented as numbers with percentages. Variables were analyzed using Wilcoxon rank sum, Chi Square, and Fisher’s Exact test for continuous, binary, and sparse binary variables, respectively. All calculations were performed using STATA statistical software (version 13.1; Stata Corporation, College Station, TX).
RESULTS
Over the two year period, 74,048 patients were admitted to the twelve trauma centers (5,238 admits, range 2,197 – 13,171 admits). Of those trauma patients, 3,117 (4%) underwent laparotomy during their hospitalization: 1,706 underwent emergent laparotomy who made up the study cohort, 1,404 underwent laparotomy greater than 90 minutes from emergency department admission, and 7 had unknown times to operating room. Of the 1,706 undergoing emergent laparotomy, 1,253 had a presenting blood pressure above 90 mmHg, 394 had a presenting blood pressure less than or equal to 90 mmHg, and 59 had a missing presenting systolic blood pressure.
Patient demographics are summarized in Table 1. The median pre-hospital time was 46 minutes (IQR 30, 75) in the entire cohort and 51 minutes (IQR 31, 85) in the hypotensive group. The cohort was young, mostly male who primarily suffered blunt trauma. The rate of penetrating trauma was significantly greater in the hypotensive group compared to the normotensive group (47% versus 27%, p<0.001). A higher percentage of patients in the hypotensive group were female (23% versus 14%, p<0.001).
Table 1.
Demographics and Emergency Department Vital Signs, Laboratory Values, Resuscitation, and Times
| Emergency Department | All Patients (n=1,706) | ED SBP >90 (n=1,253) | ED SBP ≤90 (n=394) | p value |
|---|---|---|---|---|
|
| ||||
| Demographics | ||||
|
| ||||
| Age, years | 31 (24, 45) | 30 (23, 43) | 34 (24, 52) | <0.001 |
|
| ||||
| Gender | ||||
| Male | 1427 (84%) | 1,072 (86%) | 304 (77%) | <0.001 |
| Female | 278 (16%) | 180 (14%) | 90 (23%) | |
|
| ||||
| Race | ||||
| White | 543 (32%) | 381 (30%) | 149 (38%) | 0.001 |
| Black | 634 (37%) | 498 (40%) | 113 (29%) | |
| Hispanic | 339 (20%) | 239 (19%) | 83 (21%) | |
| Other | 187 (11%) | 133 (11%) | 48 (12%) | |
|
| ||||
| Mechanism | ||||
| Blunt | 1145 (67%) | 915 (73%) | 209 (53%) | <0.001 |
| Penetrating | 561 (33%) | 338 (27%) | 185 (47%) | |
|
| ||||
| Admission Vital Signs and Labs | ||||
|
| ||||
| Glasgow Coma Scale | 15 (3, 15) | 15 (12, 15) | 6 (3, 15) | <0.001 |
|
| ||||
| Temperature, F | 97.7 (96.9, 98.2) | 97.8 (97, 98.2) | 97.0 (96.0, 98.0) | <0.001 |
|
| ||||
| Systolic blood pressure, mmHg | 119 (92, 139) | 128 (113, 144) | 71 (40, 84) | <0.001 |
|
| ||||
| Pulse, bpm | 99 (82, 119) | 99 (84, 117) | 101 (69, 125) | 0.416 |
|
| ||||
| Base excess | −5 (−10, −2) | −4 (−8, −1) | −9 (−14, −5) | <0.001 |
|
| ||||
| Hemoglobin | 12.9 (11.3, 14.2) | 13.4 (11.9, 14.5) | 11.5 (10.0, 12.9) | <0.001 |
|
| ||||
| Platelet level | 223 (180, 264) | 227 (191, 270) | 193 (138, 251) | <0.001 |
|
| ||||
| Emergency Department Resuscitation | ||||
|
| ||||
| Crystalloid, mL | 0 (0, 2000) | 200 (0, 2000) | 0 (0, 1000) | 0.034 |
|
| ||||
| Red blood cells, units | 2 (0, 4) | 1 (0, 2) | 3 (2, 4) | <0.001 |
|
| ||||
| Plasma, units | 0 (0, 2) | 0 (0, 1) | 2 (0, 3) | <0.001 |
|
| ||||
| Emergency Department Times | ||||
|
| ||||
| Time in ED, minutes | 24 (14, 39) | 23 (14, 40) | 22 (15, 38) | 0.275 |
|
| ||||
| Time from ED to surgical start, minutes | 42 (30, 61) | 45 (33, 63) | 36 (27, 54) | <0.001 |
ED – emergency department; OR – operating room
Continuous variables: median (IQR)
The entire cohort spent a median of 24 minutes (IQR 14, 39) in the emergency department (Table 1). Of note, while the time spent in the emergency department was not significantly different between the two groups, the time from emergency department admission to surgical start was shorter in the hypotensive group (36 minutes [IQR 27, 54] versus 45 [IQR 33, 63], p<0.001).
The hypotensive group had worse chest and abdominal injuries: chest AIS 3 (IQR 0, 4) versus 0 (IQR 0, 3) for the normotensive group (p<0.001); abdomen AIS 4 (3, 4) versus 3 (IQR 2, 4) for the normotensive group (p<0.001). The ISS for the hypotensive group also significantly higher: 29 (IQR 18, 41) versus 17 (IQR 9, 27) (p<0.001).
Data for operative procedures were available for 1,038 of the 1,706 patients (Table 2). In the entire cohort, the most common procedures were enterectomy (23%), hepatorrhaphy (20%), and enterorrhaphy (16%), and splenectomy (16%). Not surprisingly, operative control of hemorrhage involving hepatorraphy, splenectomy, major vascular repair, major vascular ligation, and thoracotomy/sternotomy was significantly more common in the hypotensive group.
Table 2.
Operating Room Procedures and Indications for Damage Control Laparotomy
| Operating Room | All Patients (n=1,038) | ED SBP >90 (n=739) | ED SBP ≤90 (n=241) | p value |
|---|---|---|---|---|
| Enterrorrhaphy | 164 (16%) | 123 (17%) | 31 (13%) | 0.164 |
| Enterectomy | 240 (23%) | 175 (24%) | 50 (21%) | 0.352 |
| Colorrhaphy | 137 (13%) | 106 (14%) | 26 (11%) | 0.160 |
| Colectomy | 154 (15%) | 108 (15%) | 38 (16%) | 0.662 |
| Hepatorrhaphy | 210 (20%) | 138 (19%) | 62 (26%) | 0.018 |
| Nephrectomy | 42 (4%) | 25 (3%) | 14 (6%) | 0.094 |
| Splenectomy | 163 (16%) | 89 (12%) | 67 (28%) | <0.001 |
| Diaphragm repair | 155 (15%) | 119 (16%) | 25 (10%) | 0.029 |
| Gastrorrhaphy | 112 (11%) | 90 (12%) | 16 (7%) | 0.016 |
| Major vascular repair | 91 (9%) | 53 (7%) | 31 (13%) | 0.007 |
| Major vascular ligation | 111 (11%) | 67 (9%) | 34 (14%) | 0.027 |
| Thoractomy/sternotomy | 131 (13%) | 53 (7%) | 64 (26%) | <0.001 |
The rate of damage control laparotomy was 38% (388/1,027) in the cohort, with the most common indications being need for intra-abdominal packing (31%), planned second look (20%), and hemodynamic instability (20%) (Table 3). The individual institutional rate of damage control laparotomy ranged from 24% to 53%. Although damage control laparotomy was utilized at a significantly greater rate in hypotensive patients (62% [129/207] versus 31% [236/769], p<0.001), the indications for damage control were similar: packing (38%), hemodynamic instability (23%), and planned second look (12%).
Table 3.
Indications for Damage Control Laparotomy
| Indications for Damage Control | All Damage Control Patients (n=388) | ED SBP >90 (n=236) | ED SBP ≤90 (n=129) | p value |
|---|---|---|---|---|
|
| ||||
| Packing | 121 (31%) | 68 (29%) | 49 (38%) | 0.111 |
| Planned second look | 76 (20%) | 56 (24%) | 15 (12%) | |
| HD Instability | 76 (20%) | 40 (17%) | 30 (23%) | |
| Expedite IR | 8 (2%) | 5 (2%) | 2 (2%) | |
| Expedite CT/ICU | 30 (8%) | 17 (7%) | 10 (8%) | |
| Coagulopathy | 38 (10%) | 25 (11%) | 11 (9%) | |
| ACS Prophylaxis | 4 (1%) | 3 (1%) | 1 (1%) | |
| Contamination | 1 (0%) | 1 (0%) | 0 (0%) | |
| Unknown | 34 (9%) | 21 (9%) | 11 (9%) | |
HD = hemodynamic; IR = interventional radiology; CT = computed tomography; ICU = intensive care unit; ACS = abdominal compartment syndrome
The mortality rate for the entire cohort was 21% (Table 4). The most common cause of death was hemorrhage (60%) and the median time to death was 4 hours (IQR 2, 33). Seventy-six percent of deaths in the entire cohort occurred in the first day, with over 50% of these occurring within the first 2 hours of arrival to the emergency department. In the entire group, the mortality rate for patients with blunt and penetrating mechanism of injury was significantly different (blunt 12% versus 37% penetrating, p<0.001).
Table 4.
Outcomes
| Outcomes | All Patients (n=1,706) | ED SBP >90 (n=1,253) | ED SBP ≤90 (n=394) | p value |
|---|---|---|---|---|
|
| ||||
| Deaths | 350 (21%) | 145 (11%) | 182 (46%) | <0.001 |
|
| ||||
| Time to death, hours | 4 (2, 33) | 5 (2, 83) | 3 (1, 8) | <0.001 |
|
| ||||
| Cause of death: | ||||
| Hemorrhage | 210 (60%) | 77 (53%) | 119 (65%) | 0.016 |
| Traumatic brain injury | 56 (16%) | 22 (15%) | 31 (17%) | |
| Multi-organ failure | 28 (8%) | 16 (11%) | 11 (6%) | |
| Cardiac arrest | 12 (3%) | 4 (3%) | 8 (4%) | |
| Respiratory failure | 12 (3%) | 9 (6%) | 3 (2%) | |
| Sepsis | 3 (1%) | 3 (2%) | 0 (0%) | |
| Other/unknown | 29 (8%) | 14 (10%) | 10 (5%) | |
|
| ||||
| Hospital free days | 15 (0, 23) | 19 (1, 24) | 0 (0, 12) | <0.001 |
Continuous variables: median (IQR)
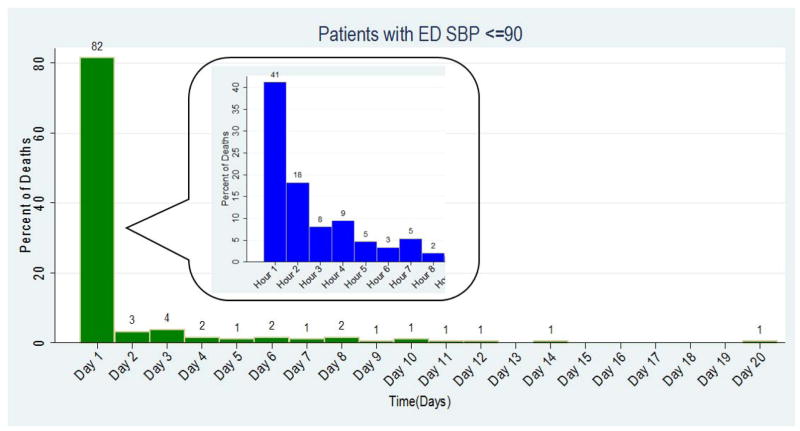
In the hypotensive group, the mortality rate was 46%. The most common cause of death in the hypotensive group was hemorrhage (65%) and the median time to death was 3 hours (IQR 1, 8). Eighty-two percent of all deaths in the hypotensive group occurred within the first day and 59% occurred within the first two hours of arrival (Figure 1). In the hypotensive group, the significant difference in mortality rate by mechanism was no longer apparent (blunt 43% versus penetrating 49%, p=0.191).
Figure 1.
Timing of death for hypotensive group.
Histogram shows percent of death in the hypotensive group by day. The insert shows the percent deaths by hour in the first 8 hours after arrival.
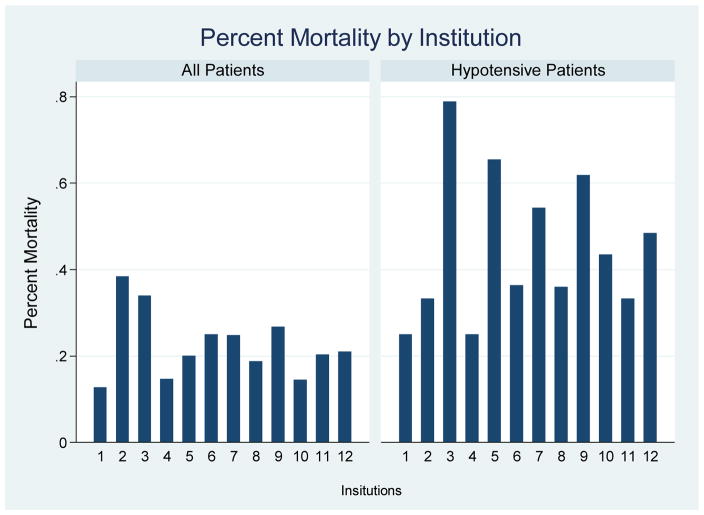
Significant variability in mortality was observed when stratifying the entire cohort by institution (Figure 2). This variability was also observed when only evaluating the hypotensive group.
Figure 2.
Mortality by institution.
The histogram shows the percent mortality for all patients and the hypotensive group by institution.
DISCUSSION
In this multicenter, retrospective study of hypotensive trauma patients undergoing emergent laparotomy, the mortality rate was 46% and hemorrhage was the most common cause of death (65%). In 2002, Clarke et al published data from 1986–1999 reporting a mortality rate of 40% for hypotensive trauma patients undergoing laparotomy within 90 minutes of arrival.4 Despite the many interventions implemented to decrease mortality in this severely injured subset, there appears to have been no decrease in mortality compared to two decades ago.
The results of this study are in stark contrast to the mortality rates recently published by Joseph et al, who reported an 11% mortality rate in patients undergoing trauma laparotomy from 2010–2013.9 The difference in mortality between this study and those data appears to be due to fundamentally different patient populations. That study excluded patients who died within 30 minutes of surgical start and the data reported here included only patients whose time from ED to surgical start was ≤90 minutes.
There are many potential reasons why a decrease in mortality was not observed. First, the patients described in this paper may be systematically different from patients described previously.4 With increasing utilization of angioembolization and non-operative management of solid organ injuries, the patients undergoing laparotomy in this time period may represent a more physiologically deranged and severely injured cohort of trauma patients than prior decades. Additionally, improvements in prehospital care may result in sicker patients arriving alive to the trauma center. This observation of reduced transport time and increased mortality has seen in patients presenting with abdominal vascular injuries.10
Second, time to the operating room still appears to matter.11 Vast resources in trauma systems and at trauma centers are utilized to expedite transport (aeromedical evacuation, scoop and run), resuscitation (massive transfusion protocols), and surgery (in-house trauma surgeon, direct to operating room protocols) to rapidly achieve hemostasis in bleeding patients. Despite these investments, we may still not be fast enough in many instances. Faster transport to the operating room with control of hemorrhage may not be feasible. Novel interventions in the field or emergency department may be critical adjuncts to lengthen that critical window to allow greater time to operative hemorrhage control.12,13
Lastly, there are few large, or even small, prospective observational or interventional clinical trials of trauma laparotomy to identify and guide best practices. Impediments, including limited funding and regulatory difficulties, have resulted in the reliance on retrospective data, which introduces known and unknown biases into any conclusions. Such studies result in tradition-driven, suboptimal clinical care.14,15 The relatively unexpected differences in mortality by center may be due to factors and biases that are unaccounted for in this study.
The limitations of the study include its retrospective nature, though as a descriptive study bias is minimal. Additionally, though the desire to have granular data of procedures for all patients, the difficulty in performing such a large, multicenter study resulted in missing data for operative procedures. Lastly, there may be important but unknown differences between the group of patients described here both between the 12 centers and in aggregate compared to others in the literature. For example, time from injury to emergency department was not known in this study, while the Injury Severity Score and resuscitation volumes were not reported in the series from Clarke et al.
In conclusion, the mortality rate for hypotensive trauma patients undergoing emergent laparotomy was 46% in 2012–2013 at 12 Level 1 trauma centers across the United States. There does not appear to have been a decrease in mortality for this group of critically ill patients compared to two decades ago despite many advances in trauma surgery.
Acknowledgments
Source of Funding – Dr. Harvin’s is supported by a KL2 grant from the Center for Clinical and Translational Sciences, which is funded by National Institutes of Health Clinical and Translational Award KL2 TR000370 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
We would like to thank Dr. David T. Martin for his contributions to this study.
Footnotes
This paper was presented in oral form at the 47th Annual Meeting of the Western Trauma Association, March 10, 2017 in Snowbird, Utah.
Author Contributions:
Study design, data analysis, data interpretation – JAH, KI, DRK, MDZ, SRT, JDK, DHL, DMS, EMB, AW, MAS, HBA, JBH
Data collection – JAH, TM, MAMA, AJC, SA, RLG, JAB, KC, LC, AW, VJUP, JRCP
Critical Revision - JAH, TM, KI, MAMA, DRK, AJC, MDZ, SA, SRT, RLG, JDK, JAB, DHL, KC, DMS, LC, EMB, AW, VJUP, MAS, JRCP, HBA, JBH
References
- 1.Cothren CC, Moore EE, Hedegaard HB, Meng K. Epidemiology of Urban Trauma Deaths: a Comprehensive Reassessment 10 Years Later. World J Surg. 2007 Jul;31(7):1507–11. doi: 10.1007/s00268-007-9087-2. [DOI] [PubMed] [Google Scholar]
- 2.Hoyt DB, Shackford SR, McGill T, Mackersie R, Davis J, Hansbrough J. The Impact of In-House Surgeons and Operating Room Resuscitation on Outcomes of Traumatic Injuries. Arch Surg. 1989 Aug;124(8):906–09. doi: 10.1001/archsurg.1989.01410080036005. [DOI] [PubMed] [Google Scholar]
- 3.Steele JT, Hoyt DB, Simons RK, Winchell RJ, Garcia J, Fortlage BA. Is Operating Room Resuscitation a Way to Save Time? Am J Surg. 1997 Dec;174(6):683–87. doi: 10.1016/s0002-9610(97)00194-3. [DOI] [PubMed] [Google Scholar]
- 4.Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CL. Time to Laparotomy for Intra-Abdominal Bleeding form Trauma Does Affect Survival for Delays up to 90 Minutes. J Trauma. 2002;52(3):420–425. doi: 10.1097/00005373-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of Errors Contributing to Trauma Mortality. Ann Surg. 2006 Sep;244(3):371–380. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cotton BA, Reddy N, Hatch QM, LeFebvre E, Wade CE, Kozar RA, Gill BS, Albarado R, McNutt MK, Holcomb JB. Damage Control Resuscitation is Associated with a Reduction in Resuscitation Volumes and Improvement in Survival in 390 Damage Control Laparotomy Patients. Ann Surg. 2011 Oct;254(4):598–605. doi: 10.1097/SLA.0b013e318230089e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rotondo MF, Schwab CW, McGonigal MD, Phillips GR, Fruchterman TM, Kauder DR, Latenser BA, Angood PA. ‘Damage Control’: an Approach for Improved Survival in Exsanguinating Penetrating Abdominal Trauma. J Trauma. 1993 Sep;35(3):375–382. [PubMed] [Google Scholar]
- 8.Niles SE, McLaughlin DF, Perkins JG, Wade CE, Li Y, Spinella PC, Holcomb JB. Increase Mortality Associated with the Early Coagulopathy of Trauma in Combat Casualties. J Trauma. 2008 Jun;64(6):1459–65. doi: 10.1097/TA.0b013e318174e8bc. [DOI] [PubMed] [Google Scholar]
- 9.Joseph B, Azim A, Zangbar B, Bauman ZM, O’Keefe T, Ibraheem K, Kulvatunyou N, Tang A, Latifi R, Rhee P. Improving Mortality in Trauma Laparotomy trhough the Evolution of Damage Control Resucitation. Analysis of 1,030 Consecutive Trauma Laparotomies. J Trauma Acute Care Surg. doi: 10.1097/TA.0000000000001273. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.Ball CG, Williams BH, Tallah C, Salomone JP, Feliciano DV. The Impact of Shorter Prehospital Transport Times on Outcomes in Patients with Abdominal Vascular Injuries. J Trauma Manag Outcomes. 2013 Dec;7(1):11. doi: 10.1186/1752-2897-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meizoso JP, Ray JJ, Karcutskie CA, Allen CJ, Zakrison TL, Pust GD, Koru-Sengul T, Ginzburg E, Pizano LR, Schulman CI, et al. Effect of Time to Operation on Mortality for Hypotensive Patients with Gunshot Wounds to the Torso: the Golden 10 Minutes. J Trauma Acute Care Surg. 2016 Oct;81(4):685–91. doi: 10.1097/TA.0000000000001198. [DOI] [PubMed] [Google Scholar]
- 12.Moore LJ, Brenner M, Kozar RA, Pasley J, Wade CE, Baraniuk MS, Scalea T, Holcomb JB. Implementation of Resuscitative Endovascular Balloon Occlusion of the Aorta as an Alternative to Resuscitative Thoracotomy for Noncompressible Truncal Hemorrhage. J Trauma Acute Care Surg. 2015 Oct;79(4):523–30. doi: 10.1097/TA.0000000000000809. [DOI] [PubMed] [Google Scholar]
- 13.Rago A, Duggan MJ, Marini J, Beagle J, Velmahos G, DeMoya MA, Sharma U, Hwabejire J, King DR. Self-Expanding Foam Improves Survival Following a Lethal, Exsanguinating Iliac Artery Injury. J Trauma Acute Care Surg. 2014 Jul;77(1):73–7. doi: 10.1097/TA.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 14.Holcomb JB, Hoyt DB. Comprehensive Injury Research. JAMA. 2015 Apr;313(14):1463–4. doi: 10.1001/jama.2014.16802. [DOI] [PubMed] [Google Scholar]
- 15.Davis KA, Fabian TC, Cioffi WG. The Toll of Death and Disability from Traumatic Injury in the United States – the “Neglected Disease” of Modern Society, Still Neglected after 50 Years. JAMA Surg. doi: 10.1001/jamasurg.2016.4625. Epub ahead of print. [DOI] [PubMed] [Google Scholar]