Highlights
-
•
DCHR is a rare benign vascular tumor, with the most common symptom being rectal bleeding.
-
•
The main challenge in the surgical management of DCHR lies in the precise resection of distal rectum.
-
•
TaTME appears to be a safe and feasible procedure for patients with DCHR in experienced hands.
-
•
DCHR is a rare benign vascular tumor, with the most common symptom being rectal bleeding.
-
•
The main challenge in the surgical management of DCHR lies in the precise resection of distal rectum.
-
•
TaTME appears to be a safe and feasible procedure for patients with DCHR in experienced hands.
Keywords: Diffuse cavernous hemangioma of the rectum, Transanal total mesorectal excision (TaTME), Natural orifice translumenal endoscopic surgery, Case report
Abstract
Background
The safety and feasibility of transanal total mesorectal excision (TaTME) were demonstrated in the management of rectal cancer. However, its role in the management of patients with diffuse cavernous hemangioma of the rectum (DCHR) has not been evaluated.
Methods
A female patient with DCHR was admitted to our hospital. Colonoscopy, magnetic resonance imaging (MRI), abdominal computed tomography (CT) and arteriography were performed. Lesions were detected in mesorectum and rectal wall extending from the dentate line to 5 cm proximally. TaTME with a protecting loop ileostomy were performed. The research work has been reported in line with the SCARE criteria Agha et al., 2016 [1].
Results
TaTME and a protecting loop ileostomy were safely performed, with an intact mesorectal specimen being harvested. The entire procedure took 348 min. The estimated blood loss was 100 ml. The patient recovered uneventfully. Her symptom of painless rectal bleeding was resolved satisfactorily following the surgery. The histopathological evaluation confirmed the diagnosis of DCHR.
Conclusions
TaTME appears to be a safe and feasible procedure for patients with DCHR in experienced hands.
1. Case report
With the aim of minimally invasive surgery, the feasibility of transanal total mesorectal excision (TaTME) for rectal cancer demonstrates the significant evolution of rectal resection consistent with the concept of natural orifice transluminal endoscopic surgery (NOTES). Compared with open and laparoscopic rectal resection, the specific feature of TaTME is to get access to the rectal lesions through the disease itself, associated with no or significantly smaller abdominal incisions. Owing to the direct and magnified visualization of the operative field, TaTME highlights the precise resection of the local lesion in distal rectum, leading to satisfactory outcomes.
Diffuse cavernous hemangioma of the rectum (DCHR), firstly reported by Phillips in 1839, is a rare benign vascular neoplasm with difficulty in diagnosis and treatment, which mainly affects children and young adults. Complete surgical resection is the preferred therapeutic option when angiographic embolization is not feasible. Traditionally, open surgery was recommended in most case series. Recently, Leal and colleagues showed that laparoscopic-assisted resection might be an alternative for DCHR by reporting on two cases [2]. However, there has been no study in the literature to evaluate the safety and feasibility of TaTME in the treatment of DCHR. Here, we present a female patient who was diagnosed with DCHR and successfully managed by the TaTME procedure. The research work has been reported in line with the SCARE criteria [1].
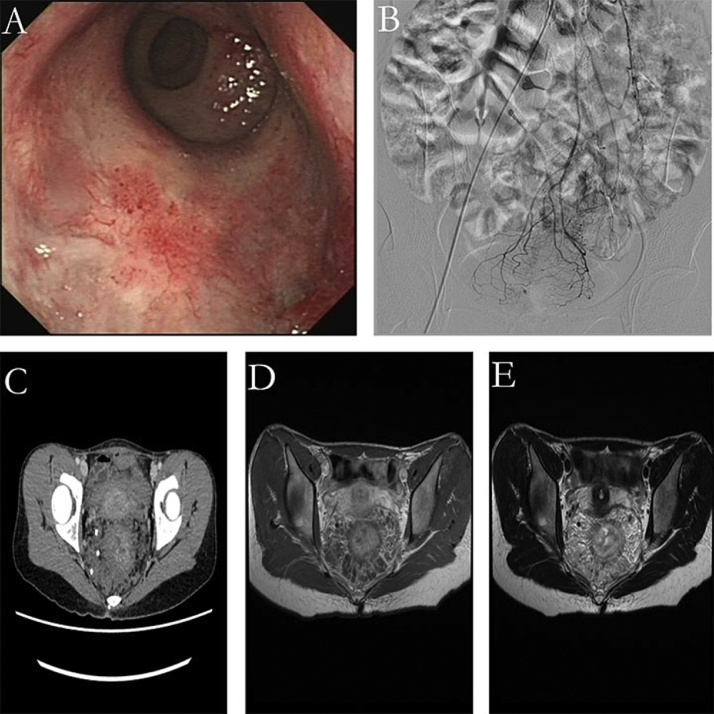
1.1. The patient
A 25-year-old female with a 6-year history of recurrent intermittent painless rectal bleeding was admitted to our hospital in September 2016. She was never transfused despite the fact that her lowest hemoglobin level was 61.0 g/dl. Her past medical history was significant for the diagnosis of hemorrhoids at age 19, when she received a stapled hemorrhoidopexy. Her symptoms of painless rectal bleeding persisted after the surgery. Physical examination revealed pale conjunctivae and the digital rectal examination was abnormal with bright red blood on the glove. Her laboratory test showed a hemoglobin level of 81.0 g/dl, with a mean corpuscular volume (MCV) of 88 fl. Colonoscopy, pelvic magnetic resonance imaging (MRI), abdominal computed tomography (CT) and digital subtraction angiography (DSA) were done subsequently, which confirmed the diagnosis of DCHR, extending from the dentate line to 5 cm proximally (Fig. 1). No other organs were involved.
Fig. 1.
(A) Flat bluish sub-mucosal serpentine vessels on colonoscopy. (B) Normal superior rectal artery and slight lamellar tumor stain on angiography. (C) Enhanced thickened rectal wall and serpentine enlarged vessels in the rectal mesentery with multiple calcification in pelvic on CTV. (D) T1W axial. (E) T2W axial. Thickening of the rectal wall with serpentine enlarged vessels in the rectal mesentery intermediate signal intensity on T1W and significantly hyperintense on T2W image.
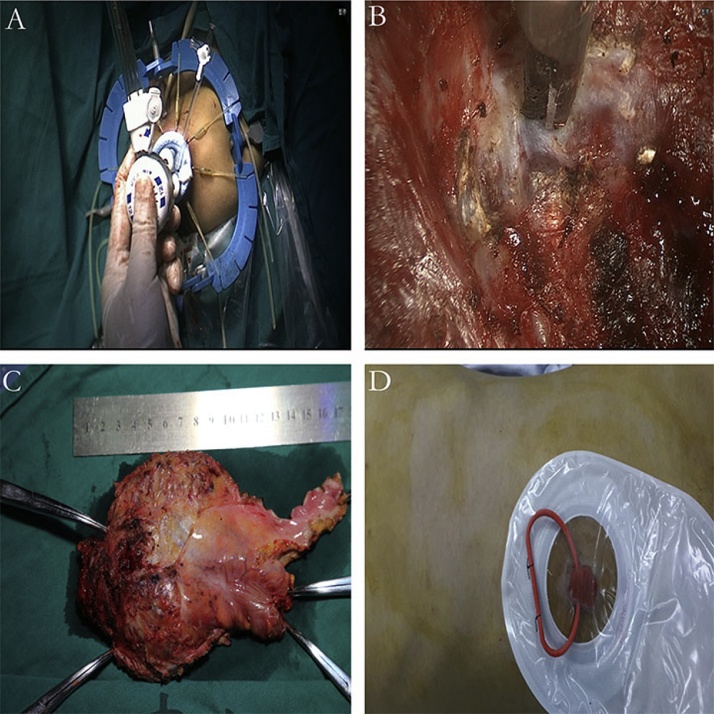
The patient was taken to the operating room for the management of DCHR. TaTME with a stapled coloanal anastomosis which was located at 2.0 cm above the anal verge were done. A loop ileostomy was also constructed for the protection of the anastomosis (Fig. 2). The entire procedure took 348 min. The estimated intraoperative blood loss was 100 ml. No intraoperative blood transfusion was required. The patient continued to recover well from the surgery. Enteral nutrition was tolerated on postoperative day 3 when bowel function returned. She was discharged on postoperative day 8. The histopathological features of excised specimen, the mesorectum of which was classified as complete, were an increased amount of dilated, thin-walled blood vessels in the submucosa, muscular layer, serosa and mesorectum (Fig. 2). No complaint of rectal bleeding was reported at the follow-up 3 months later after the surgery, when her stoma was reversed uneventfully.
Fig. 2.
(A) Transanal single-incision laparoscopic surgery port (Covidien, Mansfield, MA). (B) Transanal total mesorectal posterior dissection. (C) Surgical specimen with complete mesorectum. (D) A protecting ileostomy.
2. Discussion
As a rare benign vascular tumor, the most common symptom of DCHR is rectal bleeding, which is a general clinical problem attributed to multiple causes, leading to a dilemma in diagnosis. Wang et al. revealed that the mean delay time between initial symptom and final diagnosis was 17.63 years and most patients were misdiagnosed as hemorrhoids, colitis, polypus, and rectal varicosis caused by portal hypertension [3]. Being essential to the diagnosis of DCHR and evaluation of the extent of the lesion, colonoscopy was significant for multiple flat bluish submucosal serpentine vessels in this case. But endoscopic biopsy should be prohibited because of the high risk of severe hemorrhage. Regardless of the intrinsic insensitivity of MRI for spotting calcification, MRI is superior to CT for the diagnosis of DCHR, including the accurate evaluation of the extent of the lesion and the possible involvement of other organs [4]. They were significant for enhanced thickened rectal wall and serpentine enlarged vessels in the rectal mesentery with multiple calcification in pelvic in this case. Regardless of low sensitivity, selective inferior mesenteric angiography can help to visualize the lesion and identify a vessel for embolization. Since only slight lamellar tumor stain in the rectal wall was identified using selective inferior mesenteric angiography in this case, the embolization technique was not feasible as no large caliber vessel was available for the procedure. Histopathologic examination generally is significant for dilated, thin-walled blood vessels in the submucosa or muscular layer, serosa, and mesorectum, originated from the dentate line.
Because other therapies, in most case to date, fail to resolve rectal bleeding, most investigations in treatment for DCHR favor an open surgical resection, with a main challenge in the precise resection of distal rectum, since lesion is often originated from the dentate line. Wang et al. reported the results of 13 patients with an open surgical resection, showing that the median operative time was 295 min, the median amount of intraoperative blood loss was 793 ml and the median amount of intraoperative blood transfusion was 1013 ml [3]. Although laparoscopy provides better visualization and facilitates mobilization of the rectum, only a few studies of laparoscopic surgery for DCHR were reported. Leal et al. presented two cases of laparoscopic-assisted bowel resection for DCHR, where both patients recovered uneventfully and rectal bleeding completely resolved following the surgery [2]. Considering the difficulty of TME surgery for DCHR in resecting completely the lesion in distal rectum, TaTME might stand for an alternative surgical procedure to improve surgical quality, in which the rectum and mesorectum are excised through the avascular plane between the visceral and parietal pelvic fascia.
The feasibility and short-term outcomes of TaTME for rectal cancer have been previously demonstrated. Zhang et al. reported on a rectal cancer patient who underwent transanal single-port laparoscopic total mesorectal excision [5]. Recently, surgeons tended to consider it more feasible to perform TaTME in a hybrid approach with conventional laparoscopic assistance. On the contrast, other scholars demonstrated the safety of pure-TaTME [6], performed as transanal single-port laparoscopic TME. Realizing the goal of minimally invasive surgery, TaTME gains access to the rectal disease through the disease itself, without abdominal incisions or only significantly smaller ones so as to positively decrease incisional pain, bleeding and length of hospital stay. In this case, the patient with DCHR recovered satisfactorily from the TaTME procedure, with an acceptable amount of intraoperative blood loss and an uneventful recovery process from the surgery. Despite this case shows that TaTME appears to be an effective technique in the management of DCHR, the feasibility and safety of the procedure for DCHR needs to be evaluated in further studies with large sample sizes. Due to the learning curve, TaTME for DCHR should only be performed strictly in selective patients by experienced hands.
Conflicts of interest
All authors are aware of and agree to the content of the paper and don’t have any financial and personal conflict.
Funding
The case report doesn’t be supported by any sources of funding. All authors of this paper have directly participated in the planning, execution, and analysis of the study.
Ethical approval
Approval has been given.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contribution
All authors of this paper have directly participated in the planning, execution, and analysis of the study.
Ping Lan: Concept and design of study, revision, approval of final manuscript.
Liang Kang: Concept and design of study, data collection, revision, approval of final manuscript.
Xian-rui Wu and Wei-wen Liang: Writing the paper; data collection, revision, approval of final manuscript.
Xing-wei Zhang: revision, image editing and approval of final manuscript.
Guarantor
Lan Ping.
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Leal R.F. Laparoscopic-assisted bowel resection with construction of a colonic reservoir for cavernous hemangioma of the rectum: report of two cases. Tech. Coloproctol. 2011;15(2):205–207. doi: 10.1007/s10151-011-0685-5. [DOI] [PubMed] [Google Scholar]
- 3.Wang H.T. Diagnosis and treatment of diffuse cavernous hemangioma of the rectum: report of 17 cases. World J. Surg. 2010;34(10):2477–2486. doi: 10.1007/s00268-010-0691-1. [DOI] [PubMed] [Google Scholar]
- 4.Kandpal H. Diffuse cavernous haemangioma of colon: magnetic resonance imaging features. Report of two cases. Australas. Radiol. 2007;51:B147–B151. doi: 10.1111/j.1440-1673.2007.01837.x. Spec No.: [DOI] [PubMed] [Google Scholar]
- 5.Zhang H. Transanal single-port laparoscopic total mesorectal excision in the treatment of rectal cancer. Tech. Coloproctol. 2013;17(1):117–123. doi: 10.1007/s10151-012-0882-x. [DOI] [PubMed] [Google Scholar]
- 6.Kang L. Transanal total mesorectal excision for rectal cancer: a preliminary report. Surg. Endosc. 2016;30(6):2552–2562. doi: 10.1007/s00464-015-4521-2. [DOI] [PubMed] [Google Scholar]