Abstract
A four-year-old dachshund presented with a two-week history of pyrexia, depression, and cough. Four months earlier, the owner observed the dog swallow a whole popsicle stick, but the animal showed no clinical signs at that time. Radiography, ultrasonography, and computed tomography confirmed an intrathoracic linear foreign body and pleural effusion in the right thorax. The pleural fluid was bloody and purulent, and contained inflammatory cells and Escherichia coli. The dog was diagnosed with pyothorax induced by a foreign body, and was treated successfully by surgical removal of the foreign body, partial lung lobectomy, thoracic lavage, and antibiotics. The foreign body was identified as a popsicle stick that the dog had eaten.
Keywords: dachshund, extraluminal migration, intrathoracic foreign body, popsicle stick, pyothorax
The presence of intrathoracic foreign bodies, resulting from a penetrating thoracic injury [5, 8, 11, 15, 19, 20], migration of an implant such as a Kirschner wire [6, 10], or migration of a foreign body from the respiratory [2] or gastrointestinal tract [4, 12, 13, 23, 26], is not often reported in small animals. Wooden foreign bodies such as kebab or popsicle sticks are often ingested by dogs because of their palatability, and given their length and sharply pointed ends, can easily migrate from the gastrointestinal tract.
These foreign bodies may be found incidentally, in the absence of any clinical signs [9, 13, 14, 23], or may be found accompanied by severe signs, including a draining tract [3, 15, 16, 27], peritonitis [27], pyothorax [21], pneumothorax, or lameness [12]. The severity of clinical signs associated with a foreign body depends on the duration of penetration, the microenvironment at the site of perforation, the path of migration and the type of foreign body [23, 24]. This report describes a case of pyothorax induced by an extraluminally migrated intrathoracic wooden foreign body in a small dog.
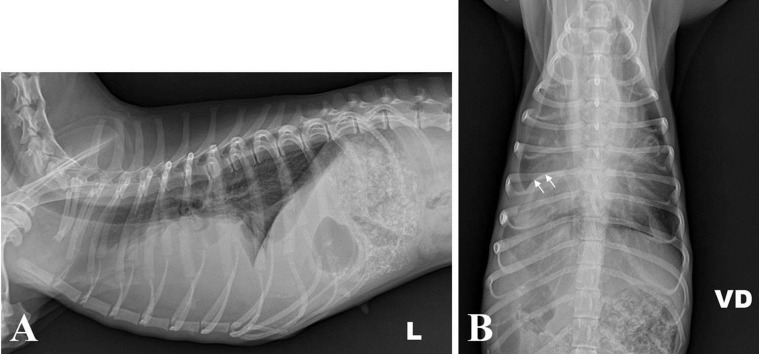
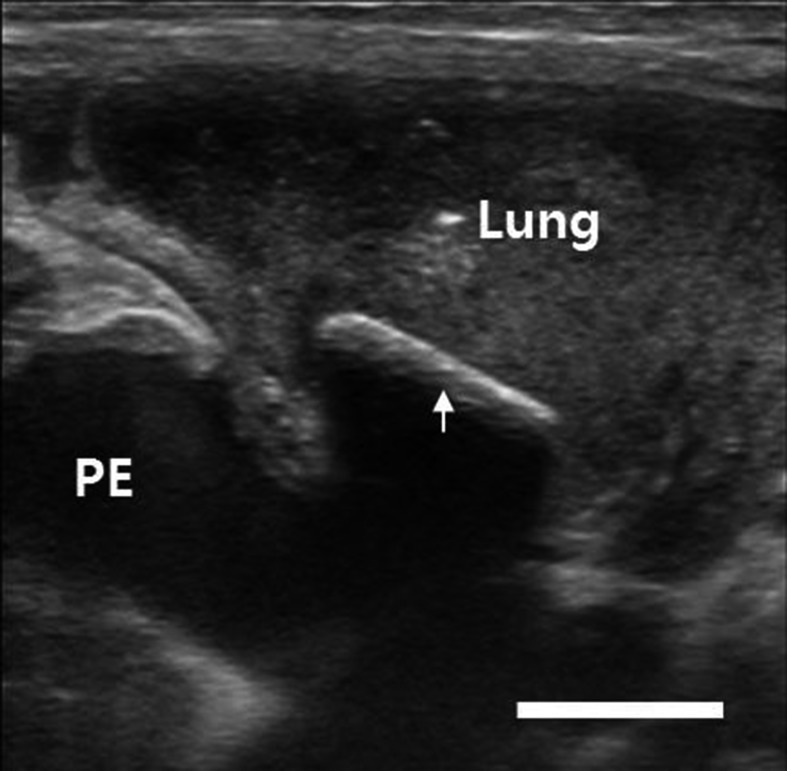
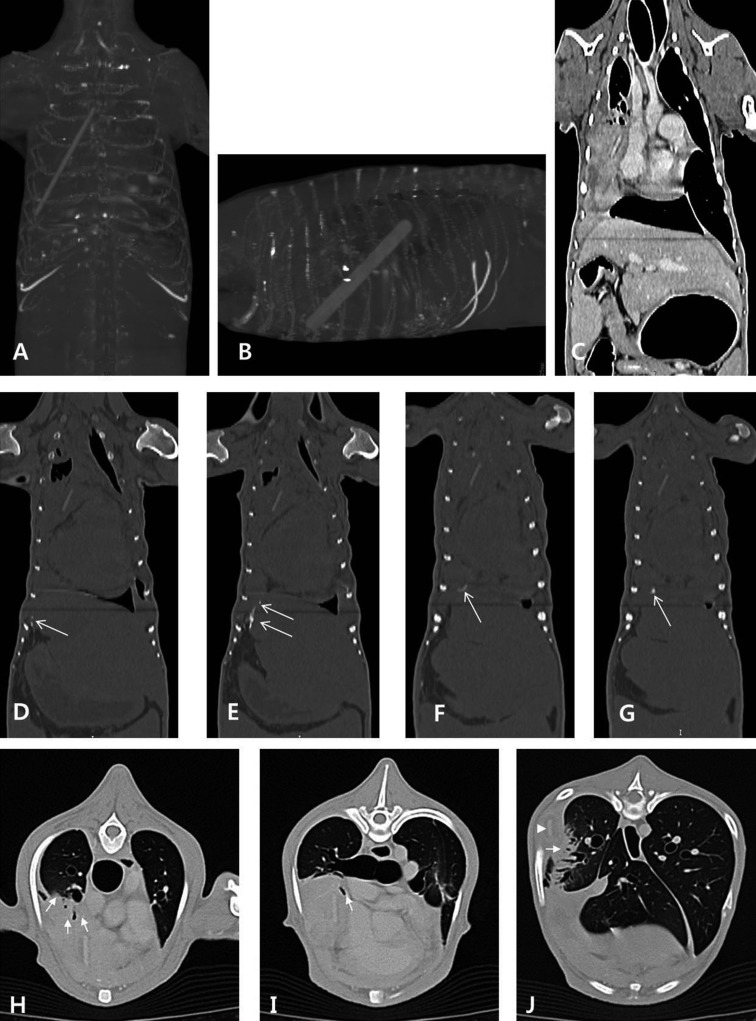
A four-year-old female miniature dachshund weighing 4 kg presented with a two-week history of pyrexia, depression and cough. Four months earlier, the owner had witnessed the dog swallow an entire popsicle stick, but the animal showed no clinical signs at that time. On physical examination, the dog was found to be depressed, febrile (39.7°C) and underweight (body condition score 2/5). Auscultation revealed loss of normal breath sounds and crackles on the right side of the thorax. The referring veterinarian identified right pleural effusion on a plain radiograph and referred the dog for further examination. Plain radiographic examination demonstrated a unilateral pleural effusion in the right thoracic cavity representing the interlobar fissure line, and loss of the cardiac and diaphragmatic silhouette on the right side (Fig. 1). An ultrasound confirmed an echogenic pleural effusion and a hyperechoic foreign body with acoustic shadowing in the right thorax. The foreign body was 12.5 mm wide, 3 mm thick, and almost 40 mm long, and was detected between the right third and sixth ribs (Fig. 2). A sample of pleural fluid was obtained by thoracocentesis for cytology, microbial culture and antibiotic susceptibility testing. The pleural fluid was bloody and purulent (hematocrit 11%; total nucleated cell count 92,610 cells/µl; total protein 3.8 g/dl), and cytology revealed numerous toxic neutrophils, macrophages and lymphocytes, which was consistent with purulent inflammation. No bacteria were detected on cytology. Thoracic and abdominal computed tomography (CT) scans (BrightSpeed Elite Select, GE Healthcare, Beijing, China) were obtained under general anesthesia for accurate determination of the size and location of the foreign body. Anesthesia was induced by propofol (6 mg/kg, intravenous [IV]) and maintained with isoflurane and oxygen via tracheal intubation. Contrast medium (350 mg I/ml) at a dose of 770 mg I/kg was then administered and the repeat CT scans were taken. The thoracic CT scan revealed a linear foreign body surrounded by soft tissue and pleural fluid (Fig. 3). The foreign body was long (100.75 mm) and flat with an attenuation of 130 Hounsfield units (HU), which is higher than that of soft tissue (110 HU). The object extended from the third to the ninth rib and was oriented cranioventrally on the midline to caudodorsally on the right side. The right side of the diaphragm was displaced forward, and several hyperattenuating spots were observed cranial to the pylorus leading to the diaphragm (Fig. 3). Focal pulmonary consolidation was observed in the right cranial and caudal lung lobes, and the right middle lung lobe was totally consolidated with complete bronchial obstruction (Fig. 3). The soft tissues in the thoracic wall were thickened and the thoracic lymph nodes were enlarged.
Fig. 1.
On plain radiography, unilateral pleural effusion is identified in the right thoracic cavity, representing the interlobar fissure line (arrows); loss of cardiac and diaphragmatic silhouette on the right side is visible.
Fig. 2.
A linear hyperechoic foreign body (arrow) between the right third and sixth ribs is detected on ultrasonography. The foreign body is 12.5 mm wide and 3 mm thick, and the acoustic shadow is readily identified in the transverse plane. The foreign body borders the lung and is surrounded by pleural effusion (PE). The scale bar represents 10 mm.
Fig. 3.
Thoracic and abdominal computed tomography scans. A–G: Intrathoracic foreign body and evidence of its extraluminal migration path are detected. A, B. The linear hyperattenuating foreign body is located in the right thoracic cavity between the third and ninth ribs. The length is 100.75 mm, and it extends in the caudodorsal direction from a cranioventral origin. C. The right diaphragm is displaced forward. D–G. Dorsal computed tomographic view in a bone window shows several hyperattenuating spots thought to be calcified (arrows) cranial to the gastric pylorus leading to the diaphragm. H–J: Right-side pulmonary consolidations are observed. H. The ventral part of the right cranial lung lobe is partially consolidated (arrows). I. The right middle lung lobe is collapsed with complete bronchial obstruction (arrow). J. Partial consolidation (arrow) is detected in the right caudal lung lobe near the foreign body (arrowhead).
Neutrophilic leukocytosis (18,910 white cells/µl with 16,000 neutrophils/µl), normochromic and normocytic anemia (hematocrit 25.41%), and hypoalbuminemia (2.4 g/dl) were detected on a complete blood count and biochemical examination. Microbial culture revealed Escherichia coli susceptible to cephalosporin, amikacin, imipenem and azithromycin.
The dog was diagnosed with pyothorax induced by an intrathoracic foreign body and the owner opted for surgery to remove the foreign body and treat the pyothorax.
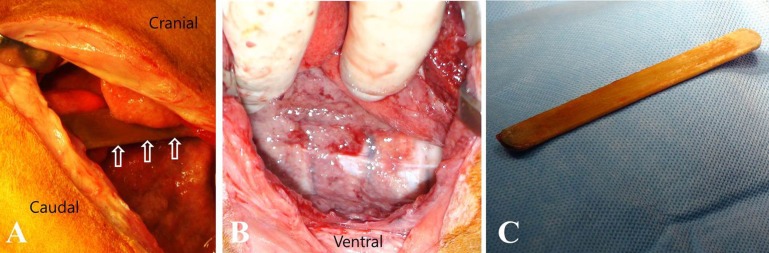
A right fifth intercostal thoracotomy was performed. The dog was premedicated with butorphanol (0.2 mg/kg, IV) followed by induction with propofol (6 mg/kg, IV). After tracheal intubation, anesthesia was maintained with isoflurane and oxygen. After opening the thoracic cavity, the foreign body was identified and easily removed, as it was floating in the thoracic cavity without any adhesions (Fig. 4). There was no surrounding granulation tissue or capsule wrapping the foreign body. Bloody, purulent pleural effusion and severe inflammation of the visceral and parietal pleura were identified. The right middle lung lobe was completely consolidated and the distal third of the right cranial and caudal lung lobes were partially consolidated. There was some adhesion between the lung lobes and the inflamed parietal pleura. After removal of the foreign body, the severely inflamed fibrous tissue was carefully debrided and detached from the lobe. During this procedure, the distal ends of the right cranial and caudal lung lobes were damaged and some bubbles were found in the lobes during thoracic lavage. After copious lavage with warm saline, a partial lobectomy of the damaged lung lobes was performed.
Fig. 4.
On right intercostal thoracotomy, a popsicle stick was found in the right thoracic cavity. A. The popsicle stick floated freely in the thoracic cavity without adhesion or embedding (arrows). B. Severe inflammation of the parietal and visceral pleura was observed. C. The popsicle stick was surgically removed.
A thoracostomy tube was placed during surgery for removal of the pleural effusion postoperatively and for thoracic lavage. After closure of the thorax, an endoscopy was performed to examine the esophagus and stomach for evidence of foreign body migration. No perforation or scar tissue was found.
Microbial culture of the removed stick and fibrous tissue was performed, and the result was the same as that for the previous pleural fluid culture.
Postoperative treatment included antibiotics, analgesics, and thoracic lavage. Cefotaxime (30 mg/kg IV, twice a day and metronidazole (15 mg/kg, IV, twice a day) were administered for the first 7 days; then the patient received cephalexin (20 mg/kg, PO, twice a day) and metronidazole (15 mg/kg, PO, twice a day) for 14 days. For management of postoperative pain, a constant-rate infusion of fentanyl (0.004 mg/kg/hr) and lidocaine (1 mg/kg/hr) was administered for the initial 24 hr, followed by tramadol (3 mg/kg, PO, three times a day) and carprofen (2.2 mg/kg, PO, twice a day) for 7 days. The dog was also treated with famotidine (0.5 mg/kg, PO, twice a day). Thoracic lavage was performed once daily using 50 ml of warm physiologic saline via a thoracostomy tube. The tube was removed 5 days after surgery when the aspirated fluid was grossly transparent and the volume aspirated was below 2 ml/kg/day.
The dog was discharged 7 days after surgery and had recovered fully by 18 days postoperatively without any abnormal signs, including pleural effusion, anemia, leukocytosis or hypoalbuminemia. On follow-up 3 years later, the dog remains healthy with no recurrence.
Wooden kebab and popsicle sticks are very attractive to dogs because of their palatability [27]. Dogs usually swallow this type of wooden sticks whole, without chewing [27]. Due to its length and shape, it is almost impossible for such a long, sharp-pointed wooden stick to pass through the digestive tract without causing perforation. In previous reports on migration of ingested wooden sticks, migration was extraluminal in all cases, and the stick was found inside the thoracic or abdominal cavity, where it was causing inflammation in a specific area [1, 3, 12, 15,16,17, 27, 29]. Our dog swallowed the popsicle stick whole, and the stick was found in the thoracic cavity. The stick was too long to pass through the digestive tract of a small dog weighing 4 kg, and its sharp edge could perforate the digestive tract easily. Popsicle sticks are not sharp-pointed like kebab sticks, but they do have one end with a sharp edge that can perforate the gastrointestinal tract if a stick is ingested, as shown in previous reports [3, 12, 29].
Imaging methods such as radiography, ultrasound, CT and magnetic resonance imaging are needed to identify foreign bodies in the body cavity. In particular, a wooden foreign body is almost invisible on conventional radiography due to its radiolucency, but it is commonly identified as a hyperechoic foreign body with uniform acoustic shadowing on ultrasound [27]. However, there are some limitations with ultrasound: it can be difficult to identify the acoustic shadow of the wooden stick in a longitudinal plane rather than in a transverse plane, and wooden sticks can become less echogenic, and therefore less indistinguishable from surrounding inflammatory tissue, over time [27]. Because of this, a CT scan may be necessary to identify the wooden foreign body accurately; CT is an effective tool for identification of wooden foreign bodies in human medicine [20]. On CT images, wooden sticks show increased attenuation due to their high inherent density and fluid absorption; therefore, their linear shape, size, and location can be accurately identified on CT [27]. In this case, the stick was identified on both ultrasound and CT. On ultrasound, a hyperechoic foreign body was detected, but it was difficult to evaluate the exact size and extent. On CT imaging, the shape, size, and location of the foreign body were accurately determined. Furthermore, information of the surrounding tissue was obtained.
The perforated area may or may not be identified. However, evidence of perforation is identified in most cases, and may include adhesion or embedding of the foreign body in the perforated area, a draining tract following the migration path, or scar tissue on the perforated organ [3, 4, 12, 13, 23, 27]. In our case, there was no strong evidence of perforation.
This case represented unique features of the migration of the wooden stick; the stick floated freely in the thoracic cavity with no adhesion or draining tract, and no visible scar tissue was found in the esophagus or stomach on endoscopy. However, several unusual findings were detected on the CT scans, including cranial displacement of the right side of the diaphragm and several hyperattenuating spots cranial to the pylorus on the right side of the diaphragm. These spots represented similar attenuation to the bone in a bone window of CT; therefore, they could be regarded as calcified soft tissues. Based on these findings, stick was thought to have perforated the right side of the stomach and pushed the ipsilateral diaphragm cranially while slowly migrating into the thorax. During this process, soft tissue around the perforated stomach could be inflamed and calcified.
Symptoms of gastrointestinal perforation vary according to the duration of penetration, the site of perforation and the migration path [23]. When the penetration period is longer, more bacteria accumulate at the perforation site and cause more severe inflammation [23, 27]. The location of the foreign body after migration determines which of the various possible complications may occur, such as a draining tract [3, 12, 15,16,17, 27]; periosteal reaction of the ribs [12], vertebral body [1], and ilium [12]; pyuria [29]; peritonitis [12, 27]; mediastinitis [27]; pulmonary abscess [27]; and pneumothorax [12]. In this case, the stick migrated into the thoracic cavity and induced severe inflammation, but there was no peritoneal inflammation related to gastric perforation. It is believed that most of the stick was located in the thoracic cavity rather than in the abdominal cavity because the foreign body penetrated the diaphragm immediately after gastric perforation. In addition, the perforated stomach was thought to have healed spontaneously without excessive leakage of gastric contents due to adhesion of the surrounding tissues. These are the likely reasons why there was no severe peritoneal inflammation.
The type of foreign body ingested also affects the clinical symptoms. In all reports, ingested wooden foreign bodies caused severe inflammation after extraluminal migration, whereas ingestion of sewing needles was often asymptomatic [9, 13, 14, 23]. It is thought that a wooden foreign body, especially when ingested, has more bacteria attached and causes more severe infection and inflammation than a metal foreign body such as a sewing needle.
Pyothorax can be treated medically with or without surgery. Selection of the best treatment method remains controversial in both human and veterinary medicine, and no prospective study has evaluated the effects of the various treatment options [28]. The first choice for treatment is drainage of exudates, thoracic lavage and antibiotic treatment [22, 28]. If this treatment is not effective, surgery, including pleural debridement, subtotal pericardiectomy and lung lobectomy, may be needed to remove the inflamed fibrous tissue and restore function of the thoracic organs [22]. If the cause of pyothorax is a foreign body, surgery is necessary to prevent recurrence [22]. Surgical methods include conventional thoracotomy and thoracoscopy. A median or lateral thoracotomy may be performed depending on whether the lesion is unilateral or bilateral. Recently, thoracoscopy was introduced as a minimally invasive method [21, 25]. Although it is advantageous for minimization of the complications associated with conventional thoracotomy, which include high morbidity, wound complications, a long recovery time and postoperative pain, its use is still limited due to the increased operating time, need for special equipment, difficulty of the technique and inadequate visibility in the presence of extensive adhesions [18, 21]. There is little evidence that thoracoscopy is more effective than conventional thoracotomy for pyothorax [7, 25, 28].
Our patient was diagnosed with unilateral pyothorax caused by a foreign body, and was treated by a conventional method that included surgical removal of the foreign body and a partial lung lobectomy via lateral thoracotomy, thoracic lavage and antibiotics. The dog had fully recovered by 18 days after surgery and there has been no recurrence of the pyothorax.
In conclusion, ingested wooden foreign bodies, especially long, sharp-edged sticks, can migrate easily from the gastrointestinal tract and can be found in the thoracic cavity. A wooden foreign body is easily contaminated with bacteria and may cause severe infection and inflammation. In this case, the intrathoracic wooden stick caused pyothorax; peritoneal inflammation was minimal even though moderate to severe gastrointestinal perforation was presumed. For the treatment of pyothorax induced by the wooden stick, surgical removal of the stick and a partial lung lobectomy, thoracic lavage and antibiotics are conventional protocols, but are still effective.
REFERENCES
- 1.Beischer D. A., Robins G. M.1993. Vertebral osteomyelitis, ataxia and paraparesis caused by a satay stick. Aust. Vet. Pract. 23: 7–10. [Google Scholar]
- 2.Brennan K. E., Ihrke P. J.1983. Grass awn migration in dogs and cats: a retrospective study of 182 cases. J. Am. Vet. Med. Assoc. 182: 1201–1204. [PubMed] [Google Scholar]
- 3.Brennan S. F., Connery N., Tobin E., Mooney C. T., Jones B. R.2004. Gastrocutaneous fistula as a result of migration of a foreign body in a dog. J. Small Anim. Pract. 45: 304–306. doi: 10.1111/j.1748-5827.2004.tb00240.x [DOI] [PubMed] [Google Scholar]
- 4.Calvo I., Weilland L., Pratschke K.2011. Traumatic myocardial laceration as a result of suspected cranial migration of a sewing needle from the stomach of a dog. Aust. Vet. J. 89: 444–446. doi: 10.1111/j.1751-0813.2011.00847.x [DOI] [PubMed] [Google Scholar]
- 5.Costa A., Lahmers S., Barry S. L., Stanton J., Stern J. A.2014. Fungal pericarditis and endocarditis secondary to porcupine quill migration in a dog. J. Vet. Cardiol. 16: 283–290. doi: 10.1016/j.jvc.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Crosara S., Zabarino S., Morello E., Iussich S., Buracco P., Borgarelli M.2008. Migration of a Kirschner wire to the heart in a Yorkshire terrier. J. Small Anim. Pract. 49: 100–102. doi: 10.1111/j.1748-5827.2007.00426.x [DOI] [PubMed] [Google Scholar]
- 7.Davies H. E., Davies R. J., Davies C. W., BTS Pleural Disease Guideline Group2010. Management of pleural infection in adults: British thoracic society pleural disease guideline 2010. Thorax 65Suppl 2: ii41–ii53. doi: 10.1136/thx.2010.137000 [DOI] [PubMed] [Google Scholar]
- 8.Elliott J. M., Mayhew P. D.2011. Diagnostic challenges and treatment options of a suspected pericardial metallic projectile foreign body in a dog. J. Vet. Emerg. Crit. Care (San Antonio) 21: 684–691. [DOI] [PubMed] [Google Scholar]
- 9.Feng Q. Z., Wang J., Sun H.2009. A sewing needle in liver: a case report and review of the literature. Cases J. 2: 6520. doi: 10.1186/1757-1626-2-6520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grand J. G., Bureau S. C.2011. Video-assisted thoracoscopic surgery for pneumothorax induced by migration of a K-wire to the chest. J. Am. Anim. Hosp. Assoc. 47: 268–275. doi: 10.5326/JAAHA-MS-5648 [DOI] [PubMed] [Google Scholar]
- 11.Guevara J. L., Holmes E. S., Reetz J., Holt D. E.2015. Porcupine quill migration in the thoracic cavity of a German shorthaired pointer. J. Am. Anim. Hosp. Assoc. 51: 101–106. doi: 10.5326/JAAHA-MS-6093 [DOI] [PubMed] [Google Scholar]
- 12.Hunt G. B., Worth A., Marchevsky A.2004. Migration of wooden skewer foreign bodies from the gastrointestinal tract in eight dogs. J. Small Anim. Pract. 45: 362–367. doi: 10.1111/j.1748-5827.2004.tb00249.x [DOI] [PubMed] [Google Scholar]
- 13.Hunt G. B., Bellenger C. R., Allan G. S., Malik R.1991. Suspected cranial migration of two sewing needles from the stomach of a dog. Vet. Rec. 128: 329–330. doi: 10.1136/vr.128.14.329 [DOI] [PubMed] [Google Scholar]
- 14.Ikenberry S. O., Jue T. L., Anderson M. A., Appalaneni V., Banerjee S., Ben-Menachem T., Decker G. A., Fanelli R. D., Fisher L. R., Fukami N., Harrison M. E., Jain R., Khan K. M., Krinsky M. L., Maple J. T., Sharaf R., Strohmeyer L., Dominitz J. A., ASGE Standards of Practice Committee 2011. Management of ingested foreign bodies and food impactions. Gastrointest. Endosc. 73: 1085–1091. doi: 10.1016/j.gie.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 15.Jackson A. H., Degner D. A.2002. Cutaneopulmonary fistula in a dog caused by migration of a toothpick. J. Am. Anim. Hosp. Assoc. 38: 545–547. doi: 10.5326/0380545 [DOI] [PubMed] [Google Scholar]
- 16.Lamb C. R., White R. N., McEvoy F. J.1994. Sinography in the investigation of draining tracts in small animals: retrospective review of 25 cases. Vet. Surg. 23: 129–134. doi: 10.1111/j.1532-950X.1994.tb00457.x [DOI] [PubMed] [Google Scholar]
- 17.Matteucci M. L., Spaulding K., Dassler C., Lee D.1999. Ultrasound diagnosis: intra-abdominal wood foreign body. Vet. Radiol. Ultrasound 40: 513–516. doi: 10.1111/j.1740-8261.1999.tb00384.x [DOI] [PubMed] [Google Scholar]
- 18.McCarthy T. C., Monnet E.2005. Diagnostic and operative thoracoscopy. pp. 229–278. In: Veterinary Endoscopy for the small animal practitioner. (McCarthy T. C. ed.), Elsevier Saunders, St. Louis. [Google Scholar]
- 19.Moon S. J., Lee J. H., Jeong S. W., Kim J. W., Park H. M.2012. Chronic bronchocutaneous fistula caused by toothpick foreign body in a Maltese dog. J. Vet. Med. Sci. 74: 651–655. doi: 10.1292/jvms.11-0376 [DOI] [PubMed] [Google Scholar]
- 20.Nielsen C., Todd J. M., Cronk D. E., Anderson K. L.2005. What is your diagnosis? A wood fragment was detected within the mediastinum, penetrating the cranial aspect of the pericardial sac and in contact with the right auricle. J. Am. Vet. Med. Assoc. 226: 1055–1056. doi: 10.2460/javma.2005.226.1055 [DOI] [PubMed] [Google Scholar]
- 21.Peláez M. J., Jolliffe C.2012. Thoracoscopic foreign body removal and right middle lung lobectomy to treat pyothorax in a dog. J. Small Anim. Pract. 53: 240–244. doi: 10.1111/j.1748-5827.2011.01175.x [DOI] [PubMed] [Google Scholar]
- 22.Piek C. J., Robben J. H.2000. Pyothorax in nine dogs. Vet. Q. 22: 107–111. doi: 10.1080/01652176.2000.9695035 [DOI] [PubMed] [Google Scholar]
- 23.Pratt C. L., Reineke E. L., Drobatz K. J.2014. Sewing needle foreign body ingestion in dogs and cats: 65 cases (2000-2012). J. Am. Vet. Med. Assoc. 245: 302–308. doi: 10.2460/javma.245.3.302 [DOI] [PubMed] [Google Scholar]
- 24.Ryan W. W., Greene R. W.1975. The conservative management of esophageal foreign bodies and their complications: a review of 66 cases in dogs and cats. J. Am. Anim. Hosp. Assoc. 11: 243–249. [Google Scholar]
- 25.Scott J., Singh A., Monnet E., Coleman K. A., Runge J. J., Case J. B., Mayhew P. D.2017. Video-assisted thoracic surgery for the management of pyothorax in dogs: 14 cases. Vet. Surg. 29: [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Smith K. R.1994. Acquired caudal vena cava occlusion and high protein ascites in a dog. J. Small Anim. Pract. 35: 261–265. doi: 10.1111/j.1748-5827.1994.tb03277.x [DOI] [Google Scholar]
- 27.Stander N., Kirberger R. M.2011. Diagnostic imaging of migrating kebab (sosatie) sticks--a review of 8 cases. J. S. Afr. Vet. Assoc. 82: 160–165. doi: 10.4102/jsava.v82i3.62 [DOI] [PubMed] [Google Scholar]
- 28.Stillion J. R., Letendre J. A.2015. A clinical review of the pathophysiology, diagnosis, and treatment of pyothorax in dogs and cats. J. Vet. Emerg. Crit. Care (San Antonio) 25: 113–129. doi: 10.1111/vec.12274 [DOI] [PubMed] [Google Scholar]
- 29.Wyatt K. M., Marchevsky A. M., Kelly A.1999. An enterovesical foreign body in a dog. Aust. Vet. J. 77: 27–29. doi: 10.1111/j.1751-0813.1999.tb12420.x [DOI] [PubMed] [Google Scholar]