Abstract
Background and Aims
Research has shown that internet interventions can be effective for dependent users of various substances. However, less is known about the effects of these interventions on users of opioids, cocaine and amphetamines than for other substances. We aimed to investigate the effectiveness of internet interventions in decreasing the usage of these types of substances.
Methods
We conducted a systematic literature search in the databases of PubMed, PsycINFO, Embase and the Cochrane Library to identify randomized controlled trials examining the effectiveness of internet interventions compared with control conditions in reducing the use of opioids, cocaine and amphetamines. No setting restrictions were applied. The risk of bias of the included studies was examined according to the Cochrane Risk of Bias assessment tool. The primary outcome was substance use reduction assessed through toxicology screening, self‐report or both at post‐treatment and at the follow‐up assessment.
Results
Seventeen studies with 2836 adult illicit substance users were included. The risk of bias varied across the included studies. Internet interventions decreased significantly opioid [four studies, n = 606, g = 0.36; 95% confidence interval (CI) = 0.20–0.53, P < 0.001] and any illicit substance use (nine studies, n = 1749, g = 0.35; 95% CI = 0.24–0.45, P < 0.001) at post‐treatment. Conversely, the effect of internet intervention for stimulant users was small and non‐significant (four studies, n = 481, P = 0.164). Overall, internet interventions decreased substance significantly use at post‐treatment (17 studies, n = 2836, g = 0.31; 95% CI = 0.23–0.39, P < 0.001) and at the follow‐up assessments (nine studies, n = 1906, g = 0.22; 95% CI = 0.07–0.37; P = 0.003).
Conclusions
Internet interventions demonstrate small but significant effects in decreasing substance use among various target populations at post‐treatment and at the follow‐up assessment. However, given the small number of available studies for certain substances, the findings should be interpreted with caution.
Keywords: Internet interventions, meta‐analysis, opioid, stimulant, substance use, web‐based
Introduction
Illicit substance use is a major health issue associated with serious physical, psychological and social harm 1. Approximately 187 000 of 27 million illicit substance users die annually due to drug‐related deaths 2. Causes of death include drug overdoses and delayed or chronic drug‐related medical consequences, including infections, fatal liver diseases, respiratory and cardiovascular diseases. The most widely used illicit substances are cannabis (although recently decriminalized/legalized in various countries) opioids, amphetamines and cocaine, of which the global use estimates are 3.9, 0.7, 0.7 and 0.4%, respectively 2. Moreover, previous findings indicate that regardless of the primary substance, illicit substance abuse and dependence, referred to currently as substance use disorder, accounts for approximately 20 million disability‐adjusted life years (DALYs) lost every year world‐wide 3. This is a substantial amount given that, for example, other serious disorders, such as dementia, account for approximately only 11 million DALYs 4. Consequently, illicit substance use imposes a significant societal and economic burden 5, 6, 7.
Pharmacological interventions are not yet available for amphetamine and cocaine users 8. Moreover, the literature indicates mixed results for opioid users 9. However, several meta‐analyses have shown that psychosocial and behavioural treatments are effective in reducing illicit substance use 10, 11, 12, 13, 14, 15. Unfortunately, only 20% of individuals with a substance use disorder utilize mental health and addiction services 16. This phenomenon can be attributed to a variety of reasons, such as lack of availability of treatment services, available but overcrowded programmes, time conflicts, financial barriers, fear of stigma and the requirement of abstinence as a goal 17, 18, 19. Internet interventions might be a novel approach to overcoming these obstacles 20 by increasing the number of people receiving standardized evidence‐based treatments, minimizing therapists' time and decreasing treatment costs 21.
Two distinct internet‐based approaches are applied commonly in the substance use literature, unguided stand‐alone internet interventions and internet interventions as an add‐on to treatment as usual (TAU). These approaches offer distinct advantages: unguided stand‐alone internet interventions are capable of supporting numerous substance users simultaneously with a low threshold for accessibility 22, 23, 24, 25. Conversely, add‐on internet interventions that are combined with face‐to‐face support are more intensive treatment in which the support of a mental health professional and the high level of convenience and flexibility of internet interventions are combined. Both approaches have demonstrated encouraging effects for nicotine, alcohol and cannabis users in previous meta‐analyses 22, 23, 26.
However, to the best of our knowledge, no previous meta‐analysis has examined the effectiveness of internet interventions regarding substance use reduction in users of opioids, cocaine, amphetamines and any illicit substances 27. The present meta‐analysis aimed to examine to what extent internet interventions are effective in reducing the use of opioids, cocaine, amphetamines and any illicit substances in adults compared to controls. By the term ‘any illicit substance users’, we refer to individuals who use at least one illicit substance and are included in transdiagnostic interventions targeting various substances at once.
Methods
Identification of studies
We conducted a systematic literature search up to January 2016 on the following databases: PubMed, PsycINFO, EMBASE and Cochrane Central Register of Controlled Trials. We used various combinations of key and index terms covering the concepts of substances (drug abuse, addiction, drug dependence, polydrug, heroin, cocaine, crack, opioid, benzodiazepine, ecstasy, amphetamine, methamphetamine) and internet interventions (internet, web, online, computer, mobile) (the full search string for PubMed is given in Supporting information, Appendix S1). Furthermore, we applied a filter for randomized controlled trials (RCTs) in these databases. We conducted additional searches by checking references of the included studies 28. Our initial selection was based on titles and abstracts. Subsequently, full texts of studies possibly meeting inclusion criteria were retrieved and evaluated. No language restrictions were applied. All searches and screenings were performed independently by two of the authors (N.B.) and (E.K.), and disagreements were resolved through discussion. The identified interventions were either web‐based or computerized; however, for the sake of clarity, we will refer to the included interventions as ‘internet interventions’.
Eligibility criteria
We included RCTs that compared internet or computerized interventions with active [e.g. TAU, motivational interviewing (MI), brief intervention (BI), psychoeducation] or non‐active (e.g. waiting‐list, assessment‐only) control conditions. The RCTs had to focus upon adult current users of illicit substances, such as cocaine, amphetamines, opioids or any illicit substances. By ‘users of any illicit substances’, we describe individuals who use at least one illicit substance. Transdiagnostic interventions, targeting those users of any illicit substances, screen for the most common substances, including opioids, cocaine, stimulants, cannabis and alcohol. Furthermore, studies had to include a measurement of substance use of the participants' at post‐test, measured through self‐report, toxicology screening or both. No distinction was made between use and abuse or dependence. Studies that did not focus on protocolized interventions but on the internet as a communication medium (e.g. by e‐mail, chat or video consultation) were excluded (see Fig. 1).
Figure 1.
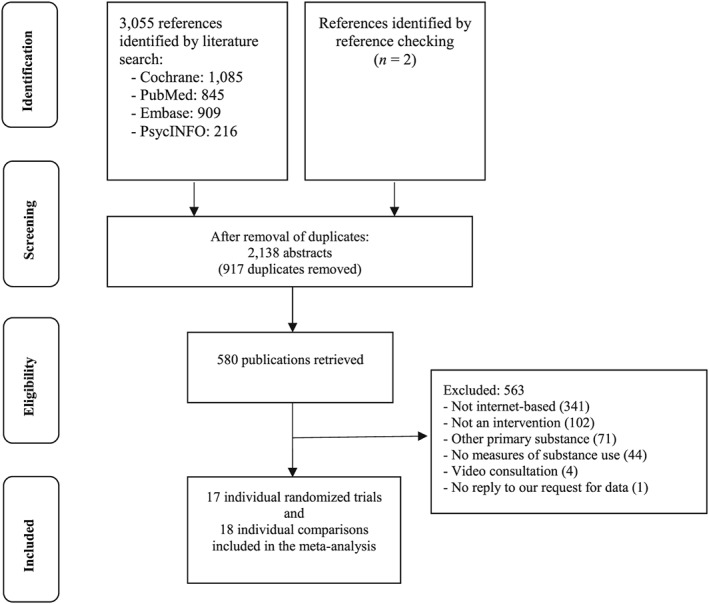
Flowchart of inclusion of studies
Quality assessment
The validity of the included studies was assessed according to the criteria of the Cochrane risk of bias assessment tool 29. We tested (1) adequacy of allocation sequence generation, (2) concealment of the allocation to the particular conditions, (3) blinding of the participants and personnel, (4) blinding of the outcome assessors, (5) appropriate handling of incomplete outcome data by applying an intention‐to‐treat design, (6) selective outcome reporting, and finally (7) other potential threats to validity, such as early cessation of the trial or extreme baseline imbalances. Two authors (N.B. and E.K.) assessed the risk of bias, and disagreements were resolved by discussion.
Data extraction
We extracted a set of outcome variables measuring the same construct; namely, substance use reduction. This practice enabled us to summarize available findings adequately. In case the studies reported more than one relevant outcome, we aggregated the means of these variables to yield an overall mean effect size for each study. These variables included: (a) mean maximum number of days or weeks abstinent throughout treatment, (b) number of positive urine samples, (c) consumption within previous weeks or months and (d) post‐treatment and follow‐up scores based on self‐report scales. Data were extracted for both post‐treatment and the longest follow‐up (6 months post‐randomization and beyond) outcomes available, and these were analysed separately. Additional aspects of the studies were coded, including participant characteristics (primary substance, recruitment method, setting, medication); intervention characteristics (type of intervention, format, duration, type of assessment, inclusion and exclusion criteria, number of sessions, attrition); control characteristics; length of the follow‐up period; and the country in which the trial was carried out (see Table 1). In cases where eligible studies did not report the necessary data to conduct quantitative analyses, we attempted to contact the first author to gain the necessary data 30, 31, 32. In the event of no reply, the studies were not included in the present systematic review 30.
Table 1.
Selected characteristics of included studies.
| Study | Primary substancea | Measureb | Recruiting | Inclusion criteria | Internet format | Intervention | Comparison | Duration | NSession | Medic. | Overallattrition | Average age & SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bickel, 2008 | Opioids | U | Community | M/F, DSM‐IV opioid dependence | ADD | CRA + CM | TAU | 23 W | 72 | Bupren. | 40% | 28.6 ± 9.1 |
| Christensen, 2014 | Opioids | U | Community | M/F, DSM‐IV opioid dependence | ADD | CRA + CM + TAU | CM + TAU | 12 W | 36 | Bupren. | 27% | 34.4 ± 9.9 |
| Chopra, 2009 | Opioids | U | Community | M/F, DSM‐IV opioid dependence | ADD | CRA + CM + TAU | TAU | 12 W | 48 | Bupren. | 27% | 31.8 ± 10.2 |
| Marsch, 2014 | Opioids | U | Out‐patient clinic | M/F, DSM‐IV opioid dependence | ADD | CRA + TAU | TAU | 52 W | 30 | Meth. | 61% | 40.7 ± 9.8 |
| Brooks, 2010 | Stimulants | S,U | Out‐patient clinic | M/F, DSM‐IV cocaine abuse/ dependence | ADD | CRA + CM + TAU | TAU | 8 W | 48 | NR | 8% | 43.1 ± 9.4 |
| Carrol, 2014 | Stimulants | U | Out‐patient clinic | M/F, DSM‐IV cocaine dependence | ADD | CBT + TAU | TAU | 8 W | 8 | Meth. | 26% | 42 ± 9.6 |
| Schaub, 2012 | Stimulants | S | Community | M/F, cocaine use ≥ 3 times past 30 days | SA | CBT | EDUC. | 6 W | 8 | NO | 85% | 34.2 ± 8.8 |
| Tait, 2014 | Stimulants | S, | Community | M/F, ATS use in past 90 days | SA | CBT | WLC | 12 W | 3 | NO | 50% | 22.4 ± 6.3 |
| Campbell, 2014 | Any | U | Out‐patient clinic | M/F illicit substance use past 60 days | ADD | CRA + CM + TAU | TAU | 12 W | 48 | NO | 56% | 34.9 ± 10.9 |
| Carrol, 2008 | Any | S,U | Out‐patient clinic | M/F, any DSM‐IV substance dependence disorder | ADD | CBT + TAU | TAU | 8 W | 6 | NR | 34% | 41.6 ± 10.2 |
| Fals‐Stewart, 2010 | Any | S,U | Residential center | M/F, any DSM‐IV substance dependence disorder | ADD | CR + TAU | TAU + TT | 8 W | 24 | NR | 8% | 32.8 ± 6.9 |
| Christoff, 2015 | Any | S | Community | M/F, ASSIST between 4 and 26 | SA | MI | MI | 1D | 1 | NR | NA | 24 ± 5.4 |
| Schwartz, 2014 | Any | S,H | Hospital | M/F, ASSIST between 4 and 26 | SA | BI | BI | 1D | 1 | NR | NA | 36.1 ± 14.7 |
| Ondersma, 2005 | Any | S | Hospital | F, any illicit drug use 30 days prior pregnancy | SA | MI | AO | 1D | 1 | NR | NA | 23.4 ± 4.9 |
| Ondersma, 2007 | Any | S,U,H | Hospital | F, any illicit drug use 30 days prior pregnancy | SA | MI | AO | 1D | 1 | NR | NA | 25.1 ± 5.6 |
| Ondersma, 2014 | Any | S,U,H | Hospital | F, any illicit drug use 30 days prior pregnancy | SA | MI | AO | 1D | 1 | NR | NA | 26.6 ± 6 |
| Sinadinovic, 2012 | Any | S | Community | M/F, DUDIT over zero | SA | MI | AO | 1D | 1 | NR | 66% | 32.6 ± NR |
ADD = add‐on intervention; ASSIST = Alcohol, Smoking and Substance Involvement Screening Test; ATS = amphetamine‐type stimulants; BI = brief intervention; Bupren. = buprenorphine; CBT = cognitive–behavioural therapy; CM = contingency management; CR= cognitive rehabilitation; CRA = community reinforcement approach; D = day; DUDIT = Drug Use Disorders Identification Test; F = female; M = male; Medic. = medication; Meth. = methadone; MI = motivational interviewing; NR = not reported; EDUC = psychoeducation; SA = standalone intervention; SD = standard deviation; TAU = treatment as usual; TT = typing tutorial; W = week; WLC = waiting list control; NA = not available.
By the term ‘any illicit substances’ we describe individuals that use at least one illicit substance and are included in transdiagnostic interventions targeting various substances at once.
By the term ‘measure’ we describe the primary outcome variable. This column also indicates which study provided multiple measures to our analyses; H = hair analyses; S = self‐report; U = urine analyses.
Meta‐analyses
We chose to calculate Hedges' g as the effect size indicating the difference for each comparison between an internet intervention and a control condition. The effect size for small sample bias was corrected according to the procedures suggested by Hedges & Olkin 33. Given that there is no gold standard of how to report results in the substance use literature 34, we expected to encounter a great variety of outcome reporting styles. The computer program Comprehensive Meta‐Analysis (CMA, version 3.3.070) was used for all analyses. Effect sizes were calculated by (a) subtracting the average post‐treatment score of the intervention group from the mean score of the control group and dividing the result by the pooled standard deviations of the two groups 35, (b) transforming test statistics (e.g. t, F, r) into the standardized mean difference 36, (c) transforming odds ratios into the standardized mean difference 37; and (d) transforming medians and interquartile range into means and standard deviations 38. Effect sizes of approximately 0.8 can be considered large, 0.5 as moderate and 0.2 small 35. When studies included two or more intervention conditions, we split the control condition into two or more groups and divided the sample size by that number 39. Consequently, intervention groups were compared separately with the relevant control conditions. If the author reported results separately for certain subgroups (e.g. gender or occupational status), the subgroups were combined and compared as one group with the relevant control condition 39, 40. As we expected heterogeneity among the studies, we decided to calculate mean effect sizes using a random‐effects model. This model assumes that the included studies were drawn from populations of studies that differed systematically from one another 41. We calculated the I 2 statistic as an indicator of heterogeneity in percentages to test the homogeneity of effect sizes. A value of 0% suggests no observed heterogeneity, while 25, 50 and 75% suggest low, moderate and high heterogeneity, respectively. Furthermore, we estimated 95% confidence intervals (CI) around I 2 42, using the non‐central χ2‐based approach within the HETEROGI module for Stata 43. Publication bias was tested by inspecting the funnel plot visually. Furthermore, Egger's linear regression test of the intercept was applied to examine if the bias captured by the funnel plot was significant 44. We also used Duval & Tweedie's trim‐and‐fill procedure 45, which produces an imputed estimate of the effect size accounting for missing studies. We investigated the presence of outliers by examining whether effect sizes and 95% CI of each study overlapped with the 95% CI of the pooled effect size; if an outlying effect size was identified, it was excluded to examine the extent to which it affects the results. Factors that, according to the literature, may have led to heterogeneity and differences between the results of individual studies were investigated through subgroup analyses. Various subgroup analyses were conducted (see Table 3, Supporting information, Appendix S2), according to the mixed‐effects model 41. In this model, studies within subgroups are pooled with the random‐effects model, whereas analyses for significant differences between subgroups are conducted with the fixed‐effects model. Given the similar behavioural and physiological effects of cocaine and amphetamines 46 and the low number of available studies for each substance, we decided to combine the RCTs targeting these populations in the subgroup analyses creating a combined group; namely, stimulant users. Finally, we conducted three univariable meta‐regression analyses to assess the association of the effect size of the internet interventions on substance use reduction (as reported at post‐test) with (a) the duration, (b) the number of sessions and (c) the risk of bias of the assessed studies. In a meta‐regression analysis, the outcome variable is being predicted according to explanatory variables. The resulting regression coefficient describes how the outcome variable changes with a unit increase in the explanatory variable 47.
Power calculation
As we expected to find only a limited number of studies for each primary substance, we conducted a power calculation to investigate the necessary amount of studies that would have to be included to have sufficient statistical power to determine relevant post‐treatment and follow‐up effects 41. Assuming a small effect size of g = 0.30, with a moderate level of between‐study variance (τ 2), a statistical power of 0.80 and an alpha of 0.05, we estimated that five studies with a mean of 60 participants per condition would be required, or 10 studies with 30 participants per condition. Alternatively, we would need 10 studies with 17 participants per condition to detect an effect size of g = 0.4, or five studies with 34 participants per condition.
Results
Selection and inclusion of studies
From the 3057 abstracts (2138 after removal of duplicates), we retrieved 580 full‐text papers for possible inclusion in the present systematic review, 563 of which were excluded because they did not meet the inclusion criteria. The flowchart describing the inclusion process is presented in Fig. 1. We included in the analysis a total of 17 individual studies with 18 individual comparisons that met all the inclusion criteria.
Characteristics of included studies
Selected characteristics of the included studies are presented in Table 1. In the present meta‐analysis, 17 studies with a total of 2836 participants were included (n = 1461 in the intervention condition; n = 1375 in the control condition). Eight studies included participants based on a DSM‐IV diagnosis, six studies included individuals according to a cut‐off score based on self‐reported substance use, two studies included individuals with an elevated substance score on the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) 48 and one study included participants who scored more than zero at the Drug Use Disorders Identification Test (DUDIT) 49—indicating at least minimal illicit substance use. Three target populations were addressed in these trials; namely, opioid users (n = 4), stimulant users (n = 4) and users of any illicit substances (n = 9). By ‘users of any illicit substances’, we describe individuals who use at least one illicit substance. RCTs, which target users of any illicit substances, screen for the most common substances, including opioids, cocaine, stimulants, cannabis and alcohol, and provide transdiagnostic interventions. The majority of the studies included recruited the participants from a clinical setting (out‐patient facility n = 5, hospital n = 4, residential centre n = 1), whereas the remaining seven studies recruited their participants from the community. Gender was distributed equally between the intervention and control conditions. The overall study attrition varied substantially, ranging from 8 to 89%. Five of the included studies provided medication to the patients 32, 39, 50, 51, 52, three specifically excluded patients receiving medication 31, 53, 54, and the remaining studies did not report the proportion of patients on medication 40, 55, 56, 57, 58, 59, 60, 61, 62. Nine trials applied an add‐on intervention, whereas eight trials applied an unguided standalone intervention. Three of the nine studies that included users of any illicit substances compared unguided standalone internet interventions with non‐active controls, three compared add‐on interventions with TAU only and three compared unguided standalone internet interventions with other types of active controls (MI, BI, psychoeducation). The four opioid primary substance studies compared add‐on interventions with TAU only. Of the four studies on stimulant users, two compared add‐on interventions with TAU only and two compared an unguided standalone intervention with a non‐active control.
The interventions applied varied according to the target population (interventions were defined as described in Table 2). The community reinforcement approach (CRA) was applied for opioid users, whereas cognitive behaviour therapy (CBT) was the prevailing approach for stimulant users. Internet interventions targeting users of any illicit substances varied considerably in terms of treatment approach and number of sessions, with MI being the dominant approach. Of the 17 studies in total, some studies employed more than one type of assessment. Specifically, 12 employed measures based on toxicology screenings, such as urine or hair analyses, and 11 studies employed self‐report measures, such as the ASSIST, the DUDIT and through online questionnaires that measured number of days using. The studies were carried out in five different countries (Australia n = 1, Brazil n = 1, Sweden n = 1, Switzerland n = 1, and the United States n = 13).
Table 2.
Definitions of internet interventions for illicit substance users.
| Conditions | Definition | Nst | Np |
|---|---|---|---|
| Treatment as usual (TAU) | TAU may vary to some extend depending on the facility; however, the majority of the facilities employ individual and group counselling that focuses largely on patients’ compliance with programme rules and rehabilitation. The counsellor might focus on assisting patients with current problems (e.g. employment, recent arrests, illness, housing) and current treatment progress (attendance, urine test results). Patients often also receive HIV educational materials 66, 67 | 9 | 1366 |
| Community reinforcement approach (CRA) |
CRA is a comprehensive behavioural programme that assists individuals to discover and adopt the fact that a healthy life‐style is more rewarding than a deleterious Life‐style filled with substance use. Consequently, it employs social, recreational, vocational and familial incentives to change the environment of substance‐misusing individuals 68 |
6 | 569 |
| Contingency management (CM) | In CM patients’ behaviour is reinforced by rewards according to the level to which they adhere in their treatment plan (e.g. negative urine screenings). Incentives usually include vouchers with monetary value that can be exchanged for goods and services. The value of these incentives typically increase gradually after each negative urine screening 69 | 5 | 567 |
| Motivational interviewing (MI) | MI is a client‐centred approach that seeks to elicit and reinforce the clients motivation for change. MI assumes that support from a therapist in the context of an egalitarian relationship enhances the likelihood of positive behaviour change, while a directive approach might inhibit such change. However, fully self‐guided internet interventions are restricted when delivering certain components of MI, such as providing a therapeutic rapport and might, therefore, not be appropriate in all cases 70. Key components of MI include acceptance, empathy, collaborative partnership, compassion, direction and evocation of client motivation 71 | 5 | 470 |
| Cognitive behaviour therapy (CBT) | CBT targets individual and social triggers for relapse via functional analysis of substance use behaviour and coping skills training to support the individual to abandon habits associated with substance use by substituting them with healthier alternative habits 72 | 4 | 261 |
| Brief intervention (BI) | BIs are concise, solution focused interventions that focus on specific measurable outcomes. They rely upon the assumption that guidance from experts can promote change and provide personalized feedback according to general practitioners or patient population data 73 | 1 | 360 |
| Cognitive rehabilitation (CR) | The rationale for this approach lies in the fact that previous findings have shown that substance users often demonstrate various deficits in cognitive skills. Thus, addressing these critical aspects of cognitive function might be a novel strategy for increasing treatment effects and decreasing substance use. CR interventions consist of various exercises intended to enhance cognitive skills such as problem‐solving, attention, memory and abstract reasoning 74 | 1 | 80 |
| Internet interventions | Internet interventions are standardized interventions that are delivered via the internet. Due to this delivery method, a wide variety of advantages become possible, such as the widespread dissemination of information to individuals who face various barriers including economical ones, stigma, transportation or other obstacles that might limit access to traditional treatments 75 | 6 | 862 |
| Computerized interventions | Computer‐delivered programs are standardized interventions that are delivered via a software program on a computer. These interventions often made use of CD rom disks and preceded internet interventions. This type of delivery method provides the advantage to the individual of being able to access the intervention offline, which might be an important aspect in cases where the internet is not accessible or available. However, this advantage comes with the drawback of not being as interconnected compared with internet interventions, which limits dissemination and collection of data 76. | 11 | 705 |
Nst = number of studies; Np = total number of participants.
Quality assessment
The methodological quality of the studies varied (see Supporting information, Appendix S3). Fifteen of the 17 studies reported an adequate sequence generation. Six studies described adequate allocation concealment. None of the studies blinded the participants and personnel and were hence considered as at high risk of bias. Thirteen of the studies employed toxicology screenings to measure substance use, thus blinding of the outcome assessment was considered as at low risk of bias, while four studies employed self‐reporting scales, thus blinding of the outcome assessment was considered as at high risk of bias for these studies. Incomplete outcome data were handled correctly in 13 studies. All the studies reported all expected outcomes, and finally, none of the included studies had other potential threats to validity. Three studies met six of the seven quality criteria, 10 met five criteria, two met four criteria and the remaining two studies met only three criteria. However, only three of the included RCTs provided their protocol online for evaluation 31, 53, 54. As a result, it is impossible to investigate protocol violations, which have been shown to be a serious threat to the validity of the study results 63.
The overall effect of internet interventions on illicit substance users
Because the number of studies per primary substance was small, we opted to pool the studies together to increase the statistical power and consequently enable the investigation of study characteristics in subgroup analyses. There was a small but significant overall effect of internet interventions on substance use reduction when all experimental conditions (n = 18) were compared with the control conditions at post‐treatment assessment. Heterogeneity was moderate. A visual inspection of the forest plot indicated two possible outliers 57, 58, in which the effect size did not overlap with the 95% CI of the pooled effect size. Therefore, we excluded the possible outliers. This exclusion resulted in a marginal increase of the effect size in favour of internet interventions (see Fig. 2). A post‐hoc power calculation indicated that our set of studies had sufficient statistical power to detect an effect size of 0.16 on the basis of the random‐effects model (with a low level of between‐study variance, τ 2 = 0, a statistical power of 0.80 and a significance level of P < 0.05). Inspection of the funnel plot and Duval & Tweedie's trim‐and‐fill procedure did not indicate publication bias. Moreover, nine studies reported follow‐up outcomes of internet interventions against control conditions, six of which were studies including users of any illicit substances and three included stimulant users. At the follow‐up (6–12 months), internet interventions (n = 9) outperformed control groups on substance use reduction for illicit substance users. The effect size was small but significant (n = 1906, g = 0.22; 95% CI = 0.07–0.37; P = 0.003). A post‐hoc power calculation indicated that our set of studies for follow‐up effects had sufficient statistical power to detect an effect size of 0.22 on the basis of the random‐effects model (with a low level of between‐study variance, τ 2 = 0.001, a statistical power of 0.80 and a significance level of P < 0.05) (Fig. 2 and Table 3).
Figure 2.
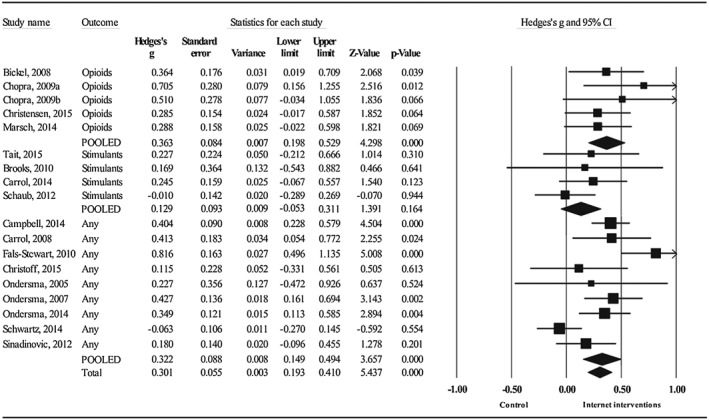
Forest plot of intervention effects at post‐treatment assessments
Table 3.
Subgroup analyses of associations between effect sizes and study characteristics (Hedges's g).a
| Ncomp | g | 95% CI | I 2 | 95% CI | P b | ||
|---|---|---|---|---|---|---|---|
| All studies | 18 | 0.30 | 0.19 to 0.41*** | 50 | 13–71 | ||
| 2 possible outliers removedc | 16 | 0.31 | 0.23 to 0.39*** | 0 | 0–52 | ||
| Primary substance | Anyd | 9 | 0.32 | 0.15 to 0.49*** | 69 | 38–85 | 0.146 |
| Opioids | 5 | 0.36 | 0.20 to 0.53*** | 0 | 0–85 | ||
| Stimulants | 4 | 0.13 | –0.05 to 0.31 | 0 | 0–85 | ||
| Subgroup analyses (n = 18) | |||||||
| Control groupe | Active | 13 | 0.31 | 0.16 to 0.46*** | 62 | 31–79 | 0.978 |
| Non‐active | 5 | 0.31 | 0.17 to 0.45*** | 0 | 0–79 | ||
| Type | CRA + CM | 6 | 0.39 | 0.26 to 0.52*** | 0 | 0–75 | 0.382 |
| MI | 5 | 0.30 | 0.16 to 0.44*** | 0 | 0–79 | ||
| CBT | 4 | 0.19 | 0.02 to 0.35 | 17 | 0–87 | ||
| Other | 3 | 0.34 | –0.18 to 0.85 | 90 | 74–96 | ||
| Format | Add‐on | 10 | 0.41 | 0.30 to 0.52*** | 12 | 0–54 | 0.011 |
| Standalone | 8 | 0.17 | 0.03 to 32* | 43 | 0–75 | ||
| Type of assessment | Tox. screening | 12 | 0.42 | 0.32 to 0.52*** | 0 | 0–58 | 0.016 |
| Self‐report | 11 | 0.26 | 0.05 to 0.42* | 71 | 46–84 | ||
| Screening | DSM‐IV | 9 | 0.42 | 0.27 to 0.56*** | 22 | 0–63 | 0.048 |
| Cut‐off scores | 9 | 0.21 | 0.07 to 0.36** | 55 | 4–79 | ||
| Medication | Yes | 6 | 0.34 | 0.19 to 0.48*** | 0 | 0–75 | 0.774 |
| No | 3 | 0.22 | –0.06 to 0.50 | 67 | 0–91 | ||
| NR | 9 | 0.30 | 0.11 to 0.50** | 67 | 34–84 | ||
| Analyses | ITT analyses | 13 | 0.31 | 0.20 to 0.42*** | 36 | 0–67 | 0.883 |
| Comp. analyses | 5 | 0.33 | 0.04 to 0.63* | 69 | 20–88 | ||
| Recruitment | Clinical | 10 | 0.34 | 0.18 to 0.49*** | 63 | 28–82 | 0.341 |
| Community | 8 | 0.23 | 0.01–0.37** | 11 | 0–71 | ||
| Setting | Computer, out‐patient clinic | 9 | 0.36 | 0.26 to .47*** | 0 | 0–65 | 0.002 |
| Computer, hospital | 4 | 0.23 | –0.44 to 0.50 | 71 | 19–90 | ||
| Internet, home | 3 | 0.11 | –0.07 to 0.29 | 0 | 0–90 | ||
| Computer, university | 1 | 0.12 | –0.33 to 0.56 | 0 | NA | ||
| Computer, residential centre | 1 | 0.82 | 0–50 to 1.14*** | 0 | NA | ||
| Female‐only studies | Yes | 3 | 0.37 | 0.20 to 0.55*** | 0 | 0–90 | 0.448 |
| No | 15 | 0.29 | 0.16 to 0.42*** | 57 | 23–76 |
BI = brief intervention; CET = cognitive enhancement therapy; Comp. = completers; EDUC = psychoeducation; ITT = intention‐to‐treat; MI = motivational interviewing; NA = not applicable; Ncomp = number of comparisons; NR = not reported; PA = positive affect; TAU = treatment as usual; Tox. = toxicology; WLC = waiting‐list control.
According to the random‐effects model;
the P‐values in this column indicate if the difference between the effect sizes in the subgroups is significant; CI = confidence interval (*P ≤ 0.05; **P < 0.01; ***P ≤ 0.001);
By the term ‘any illicit substances’ we describe individuals who use at least one illicit substance and are included in transdiagnostic interventions targeting various substances at once.
Active controls include: TAU, MI, BI, EDUC; inactive controls include: WLC, add‐on.
Substance‐specific results of internet interventions
The effects of internet interventions on substance use reduction were similar for opioid users (n = 606, g = 0.36; 95% CI = 0.20–0.53, P < 0.001) and users of any illicit substances, indicating a small but significant effect. A visual inspection of the forest plot indicated two possible outliers 57, 58, in which the effect size did not overlap with the 95% CI of the pooled effect size. Therefore, we excluded the possible outliers. This exclusion resulted in a marginal increase of the effect size for users of any illicit substances in favour of internet interventions (n = 1749, g = 0.35; 95% CI = 0.24–0.45, P < 0.001; I2 = 0; 95% CL = 0–71, P = .750). Conversely, the effect of internet intervention on stimulant use reduction was small and non‐significant when compared to the control conditions (n = 481, P = 0.164) (Fig. 2 and Table 3).
Subgroup analyses
We conducted a series of subgroup analyses (see Table 3, Supporting information, Appendix S2). These analyses indicated that add‐on interventions were more effective compared to unguided standalone interventions and the type of assessment; specifically, toxicology screenings were associated with higher effect sizes compared to self‐report. Interventions delivered in an out‐patient clinic via computer were significantly more effective compared to interventions delivered via computer at a university and via the internet at home. Finally, the type of eligibility screening also affected the outcomes; specifically, DSM‐IV diagnoses were associated with higher effect sizes compared to cut‐off scores on self‐reported substance use (Table 3).
Meta‐regression analyses
The meta‐regression analyses did not reveal significant associations between the effect size of internet interventions on substance use reduction and (a) duration (slope: 0.002; 95% CI = −0.007 to 0.012, P = 0.652), (b) number of sessions (slope: 0.003; 95% CI = −0.003 to 0.008, P = 0.338) and (c) risk of bias (slope: −0.063; 95% CI = −0.187 to 0.062, P = 0.326).
Discussion
The present systematic review was the first, to our knowledge, to examine the effectiveness of internet interventions regarding substance use reduction of opioids, stimulants and any illicit substances at both post‐treatment and at the follow‐up. We found a small but significant overall effect size of internet interventions for the reduction of illicit substance use at post‐treatment (g = 0.30) and at the follow‐up assessment (g = 0.22). Specifically, internet interventions decreased opioid use (g = 0.36) and any illicit substance use significantly (g = 0.32), but did not reduce stimulant use significantly. These findings are in line with the broader literature of internet interventions on nicotine, alcohol and cannabis use reduction that indicate small but significant effects 22, 23, 26.
Our subgroup analyses displayed varying effects, depending on certain characteristics of the trials; namely, format of the intervention, type of the assessment, screening and setting. Specifically, (a) add‐on interventions displayed higher effects compared to unguided standalone interventions, (b) studies which applied toxicology screenings as outcome measure were associated with higher effect sizes compared to studies that applied self‐report measures, (c) DSM‐IV diagnoses were associated with higher effect sizes compared to cut‐off scores on self‐reported substance use, and finally (d) studies that conducted the intervention in clinical out‐patient clinics showed higher effect sizes compared to other settings.
Limitations
We were not able to extract data from all eligible studies, because one study did not report outcome data 27. This study found no significant effects in substance use when adding an add‐on internet intervention to the TAU setting. Moreover, it should be taken into account that certain characteristics of the trials (add‐on intervention, toxicology screening, out‐patient clinic) are associated predominantly with intensive treatments that were compared with TAU, while other characteristics (e.g. unguided standalone interventions, self‐report assessments, home setting) were associated predominantly with less intensive interventions and compared primarily (except for three [40,58,63] studies) with inactive interventions, such as assessment‐only and waiting‐list. For this reason, we suggest that the unexpected finding of toxicology screenings and DSM diagnoses being associated with higher effect sizes might be the fact that they are applied in studies with intensive treatments that target severe users and have higher chances of yielding high effect sizes compared to studies with less intensive treatments that target less severe users. Another explanation might be that a study requiring toxicology screenings might lead to selection bias by recruiting more adherent patients. Therefore, these findings should be considered with caution. Moreover, five of the included studies applied completers' only analyses 31, 39, 50, 56, 58, which might have induced heterogeneity in our findings, especially considering the high attrition of certain studies. Also, we experienced some difficulty in assessing the influence medication might have had on the effect sizes, as only a minority of studies specifically excluded patients who were on medication and the majority of the studies did not report the proportion of patients being on medication. Finally, the small number of available studies for certain substances restricted our ability to reach solid conclusions about these populations. Additionally, psychiatric comorbidity was not examined by the included trials. Such comorbidities might influence the adherence and the efficacy of the internet interventions. Previous research has shown that transdiagnostic interventions for substance users with comorbid mental disorders are more effective 63 and have higher adherence rates 64 compared to separate treatment plans for individual disorders.
Summarizing the empirical literature on the effectiveness of internet interventions for substance users presented several challenges. The utilized outcomes to determine superiority of a condition varied substantially, and although this variation of outcomes has been noted by previous studies 11, 12, 64 little effort has been taken place to overcome this challenge. Therefore, we suggest that future studies should approach this issue to further improve the comparability of outcome findings. Furthermore, the relatively high rate of attrition might be a serious restriction. This is especially true for unguided standalone interventions and is often considered a serious threat to the integrity of the study results 65. Therefore, further research should investigate possible predictors to prevent attrition.
Conclusion
Although more research is necessary to assess the effectiveness of internet interventions in illicit substance users, this method of treatment delivery seems to be a promising solution for achieving substance use reduction in these target populations.
Declaration of interests
None.
Supporting information
Appendix S1 Pubmed search string.
Appendix S2 Definition of subgroup analyses.
Appendix S3 Risk of bias assessment.
Boumparis, N. , Karyotaki, E. , Schaub, M. P. , Cuijpers, P. , and Riper, H. (2017) Internet interventions for adult illicit substance users: a meta‐analysis. Addiction, 112: 1521–1532. doi: 10.1111/add.13819.
References
- 1. Whiteford H. A., Ferrari A. J., Degenhardt L., Feigin V., Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the global burden of disease study 2010. PLOS ONE 2015; 10: e0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. United Nations Office on Drugs and Crime . World Drug Report [internet]. Vienna, Austria; 2015. Available at: https://www.unodc.org/documents/wdr2015/World_Drug_Report_2015.pdf (accessed 26 June 2016) (Archived at http://www.webcitation.org/6iYfzHX4U). [Google Scholar]
- 3. Degenhardt L., Whiteford H. A., Ferrari A. J., Baxter A. J., Charlson F. J., Hall W. D. et al. Global burden of disease attributable to illicit drug use and dependence: findings from the global burden of disease study 2010. Lancet 2013; 382: 1564–1574. [DOI] [PubMed] [Google Scholar]
- 4. Murray C. J. L., Vos T., Lozano R., Naghavi M., Flaxman A. D., Michaud C. et al. Disability‐adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990‐2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 380: 2197–2223. [DOI] [PubMed] [Google Scholar]
- 5. National Drug Intelligence Center . The Economic Impact of Illicit Drug Use on American Society. Washington, DC: National Drug Intelligence Center; 2011. [Google Scholar]
- 6. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) . Cost and financing of drug treatment services in Europe: An exploratory study [internet]. Lisbon: EMCDDA; 2011. Available at: http://www.emcdda.europa.eu/attachements.cfm/att_143682_EN_TDSI11001ENC.pdf (accessed 26 June 2016) (Archived at http://www.webcitation.org/6iYgEALD9). [Google Scholar]
- 7. Wood E., Kerr T., Spittal P. M., Tyndall M. W., O'Shaughnessy M. V., Schechter M. T. The health care and fiscal costs of the illicit drug use epidemic: the impact of conventional drug control strategies. B C Med J 2003; 45: 128–134. [Google Scholar]
- 8. Douaihy A. B., Kelly T. M., Sullivan C. Medications for substance use disorders. Soc Work Public Health 2013; 28: 264–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Veilleux J. C., Colvin P. J., Anderson J., York C., Heinz A. J. A review of opioid dependence treatment: pharmacological and psychosocial interventions to treat opioid addiction. Clin Psychol Rev 2010; 30: 155–166. [DOI] [PubMed] [Google Scholar]
- 10. Lussier J. P., Heil S. H., Mongeon J. A., Badger G. J., Higgins S. T. A meta‐analysis of voucher‐based reinforcement therapy for substance use disorders. Addiction 2006; 101: 192–203. [DOI] [PubMed] [Google Scholar]
- 11. Magill M., Ray L. A. Cognitive–behavioral treatment with adult alcohol and illicit drug users: a meta‐analysis of randomized controlled trials. J Stud Alcohol Drugs 2009; 70: 516–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dutra L., Stathopoulou G., Basden S. L., Leyro T. M., Powers M. B., Otto M. W. A meta‐analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry 2008; 165: 179–187. [DOI] [PubMed] [Google Scholar]
- 13. Roozen H. G., Boulogne J. J., Van Tulder M. W., Van Den Brink W., De Jong C. A. J., Kerkhof A. J. F. M. A systematic review of the effectiveness of the community reinforcement approach in alcohol, cocaine and opioid addiction. Drug Alcohol Depend 2004; 74: 1–13. [DOI] [PubMed] [Google Scholar]
- 14. Smedslund G., Berg R. C., Hammerstrøm K. T., Steiro A., Leiknes K. A., Dahl H. M. et al. Motivational interviewing for substance abuse Cochrane Database Syst Rev 2011; Issue 5 Art. No.: CD008063. https://doi.org/10.1002/14651858.CD008063.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Powers M. B., Vedel E., Emmelkamp P. M. G. Behavioral couples therapy (BCT) for alcohol and drug use disorders: a meta‐analysis. Clin Psychol Rev 2008; 28: 952–962. [DOI] [PubMed] [Google Scholar]
- 16. Saloner B., Karthikeyan S. Changes in substance abuse treatment use among individuals with opioid use disorders in the United States, 2004–2013. JAMA 2015; 314: 1515. [DOI] [PubMed] [Google Scholar]
- 17. Center for Behavioral Health Statistics and Quality (CBSHQ) . National Survey on Drug Use and Health: Detailed Tables [Internet]. Rockville, MD: CBSHQ; 2014. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf (accessed 26 June 2016) (Archived at http://www.webcitation.org/6iYgL98oV). [Google Scholar]
- 18. Xu J., Rapp R. C., Wang J., Carlson R. G. The multidimensional structure of external barriers to substance abuse treatment and its invariance across gender, ethnicity, and age. Subst Abuse 2008; 29: 43–54. [DOI] [PubMed] [Google Scholar]
- 19. Substance Abuse and Mental Health Services Administration (SAMHSA) . Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings [internet]. Rockville, MD: SAMHSA; 2014. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf (accessed 26 June 2016) (Archived at: http://www.webcitation.org/6iYgVTSgK). [Google Scholar]
- 20. Taylor C. B., Luce K. H. Computer‐ and internet‐based psychotherapy interventions. Curr Dir Psychol Sci 2003; 12: 18–22. [Google Scholar]
- 21. Murphy S. M., Campbell A. N. C., Ghitza U. E., Kyle T. L., Bailey G. L., Nunes E. V. et al. Cost‐effectiveness of an internet‐delivered treatment for substance abuse: data from a multisite randomized controlled trial. Drug Alcohol Depend 2016; 161: 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Riper H., Blankers M., Hadiwijaya H., Cunningham J., Clarke S., Wiers R. et al. Effectiveness of guided and unguided low‐intensity internet interventions for adult alcohol misuse: a meta‐analysis. PLOS ONE 2014; 9: e99912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tait R. J., Spijkerman R., Riper H. Internet and computer based interventions for cannabis use: a meta‐analysis. Drug Alcohol Depend 2013; 133: 295–304. [DOI] [PubMed] [Google Scholar]
- 24. Cunningham J. A., Khadjesari Z., Bewick B. M., Riper H. Internet‐based interventions for problem drinkers: from efficacy trials to implementation. Drug Alcohol Rev 2010; 29: 617–622. [DOI] [PubMed] [Google Scholar]
- 25. Boon B., Risselada A., Huiberts A., Riper H., Smit F. Curbing alcohol use in male adults through computer generated personalized advice: randomized controlled trial. J Med Internet Res 2011; 13: e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Graham A. L., Carpenter K. M., Cha S., Cole S., Jacobs M. A., Raskob M. et al. Systematic review and meta‐analysis of internet interventions for smoking cessation among adults. Subst Abuse Rehabil 2016; 7: 55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Riper H., Andersson G., Christensen H., Cuijpers P., Lange A., Eysenbach G. Theme issue on e‐mental health: a growing field in internet research. J Med Internet Res 2010; 12: e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Horsley T., Dingwall O., Sampson M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst Rev 2011; Issue 8 Art. No.: MR000026. https://doi.org/10.1002/14651858.MR000026.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higgins J. P. T., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D. et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Acosta M. C., Marsch L. A., Xie H., Guarino H., Aponte‐Melendez Y. A web‐based behavior therapy program influences the association between cognitive functioning and retention and abstinence in clients receiving methadone maintenance treatment. J Dual Diagn 2012; 8: 283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Campbell A. N. C., Nunes E. V., Matthews A. G., Stitzer M., Miele G. M., Polsky D. et al. Internet‐delivered treatment for substance abuse: a multisite randomized controlled trial. Am J Psychiatry 2014; 171: 683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Marsch L. A., Guarino H., Acosta M., Aponte‐melendez Y., Cleland C., Grabinski M. et al. Web‐based behavioral treatment for substance use disorders as a partial replacement of standard methadone maintenance treatment. J Subst Abuse Treat 2014; 46: 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hedges L. V., Olkin I. Statistical Methods for Meta‐Analysis, 1st edn. Cambridge, MA: Academic Press; 1985, p. 369. [Google Scholar]
- 34. Dupont R. L. Creating a New Standard for Addiction Treatment Outcomes. [internet]. Rockville, MD: Institute for Behavior and Health, Inc.; 2014. Available at: http://www.williamwhitepapers.com/pr/IBH%20Creating%20a%20New%20Standard%20for%20Addiction%20Treatment%20Outcomes%202014.pdf (accessed 26 June 2016) (Archived at http://www.webcitation.org/6pCV0iOJL).
- 35. Cohen J. Statistical power analysis for the behavioral sciences, 2nd edn. Statistical Power Analysis for the Behavioral Sciences (rev. edn), Vol. 2 Cambridge, MA: Academic Press; 1988. [Google Scholar]
- 36. Lipsey M. W., Wilson D. B. Practical Meta‐Analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 37. Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Stat Med 2000; 19: 3127–3131. [DOI] [PubMed] [Google Scholar]
- 38. Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014; 14: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chopra M. P., Landes R. D., Gatchalian K. M., Jackson L. C., Buchhalter A. R., Stitzer M. L. et al. Buprenorphine medication versus voucher contingencies in promoting abstinence from opioids and cocaine. Exp Clin Psychopharmacol 2009; 17: 226–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. de Oliveira C. A., Boerngen‐Lacerda R. Reducing substance involvement in college students: a three‐arm parallel‐group randomized controlled trial of a computer‐based intervention. Addict Behav 2015; 45: 164–171. [DOI] [PubMed] [Google Scholar]
- 41. Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. Introduction to Meta‐Analysis. 1. Chichester: John Wiley & Sons; 2009, p. 452. [Google Scholar]
- 42. Ioannidis J. P. A., Patsopoulos N. A., Evangelou E. Uncertainty in heterogeneity estimates in meta‐analyses. BMJ 2007; 335: 914–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Orsini N., Bottai M., Higgins J., Buchan I. HETEROGI: Stata module to quantify heterogeneity in a meta‐analysis. Boston Department of Economics, Boston, MA: Statistical Software Components; 2006. [Google Scholar]
- 44. Egger M., Davey Smith G., Schneider M., Minder C., Mulrow C., Egger M., et al. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Duval S., Tweedie R. Trim and fill: a simple funnel‐plot‐based method of testing and adjusting for publication bias in meta‐analysis. Biometrics 2000; 56: 455–463. [DOI] [PubMed] [Google Scholar]
- 46. Levinthal C. F. Drugs, Behavior, and Modern Society, 8th edn. New Zealand: Pearson Education; 2013. [Google Scholar]
- 47. Higgins J. P. T., Green S. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1. 0 (updated March 2011). The Cochrane Collaboration; 2011. Available at: http://handbook.cochrane.org (accessed 26 June 2016) (Archived at http://www.webcitation.org/6pfIXRTz9). [Google Scholar]
- 48. World Health Organization (WHO) Group . The Alcohol, Smoking and Substance Involvement Screening Test (Assist): Development, Reliability and Feasibility. Geneva: WHO; 2002. [DOI] [PubMed]
- 49. Hildebrand M. The psychometric properties of the drug use disorders identification test (DUDIT): a review of recent research. J Subst Abuse Treat 2015; 53: 52–59. [DOI] [PubMed] [Google Scholar]
- 50. Bickel W. K., Marsch L. A., Buchhalter A. R., Badger G. J. Computerized behavior therapy for opioid‐dependent outpatients: a randomised control trial. Exp Clin Psychopharmacol 2008; 16: 132–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carroll K. M., Kiluk B. D., Nich C., Gordon M. A., Portnoy G. A., Marino D. R. et al. Computer‐assisted delivery of cognitive‐behavioral therapy: efficacy and durability of CBT4CBT among cocaine‐dependent individuals maintained on methadone. Am J Psychiatry 2014; 171: 436–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Christensen D. R., Landes R. D., Jackson L., Marsch L. A., Mancino M. J., Chopra M. P. et al. Adding an internet‐delivered treatment to an efficacious treatment package for opioid dependence. J Consult Clin Psychol 2014; 82: 964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Schaub M. P., Sullivan R., Haug S., Stark L. Web‐based cognitive behavioral self‐help intervention to reduce cocaine consumption in problematic cocaine users: randomized controlled trial. J Med Internet Res 2012; 14: e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tait R. J., McKetin R., Kay‐Lambkin F., Carron‐Arthur B., Bennett A., Bennett K. et al. A web‐based intervention for users of amphetamine‐type stimulants: 3‐month outcomes of a randomized controlled trial. JMIR Ment Health 2014; 1: e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Brooks A. C., Ryder D., Carise D., Kirby K. C. Feasibility and effectiveness of computer‐based therapy in community treatment. J Subst Abuse Treat 2010; 39: 227–235. [DOI] [PubMed] [Google Scholar]
- 56. Carroll K. M., Ball S. A., Martino S., Nich C., Babuscio T. A., Nuro K. F. et al. Computer‐assisted delivery of cognitive‐behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry 2008; 165: 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Fals‐Stewart W., Lam W. K. K. Computer‐assisted cognitive rehabilitation for the treatment of patients with substance use disorders: a randomized clinical trial. Exp Clin Psychopharmacol 2010; 18: 87–98. [DOI] [PubMed] [Google Scholar]
- 58. Schwartz R. P., Gryczynski J., Mitchell S. G., Gonzales A., Moseley A., Peterson T. R. et al. Computerized versus in‐person brief intervention for drug misuse: a randomized clinical trial. Addiction 2014; 109: 1091–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ondersma S. J., Chase S. K., Svikis D. S., Schuster C. R. Computer‐based brief motivational intervention for perinatal drug use. J Subst Abuse Treat 2005; 28: 305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ondersma S. J., Svikis D. S., Schuster C. R. Computer‐based brief intervention a randomized trial with postpartum women. Am J Prev Med 2007; 32: 231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sinadinovic K., Wennberg P., Berman A. H. Targeting problematic users of illicit drugs with internet‐based screening and brief intervention: a randomized controlled trial. Drug Alcohol Depend 2012; 126: 42–50. [DOI] [PubMed] [Google Scholar]
- 62. Ondersma S. J., Svikis D. S., Thacker L. R., Beatty J. R., Lockhart N. Computer‐delivered screening and brief intervention (e‐SBI) for postpartum drug use: a randomized trial. J Subst Abuse Treat 2014; 46: 52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sweetman E. A., Doig G. S. Failure to report protocol violations in clinical trials: a threat to internal validity? Trials 2011; 12: 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Allen J. P., Columbus M. Alcohol consumption measures In: Sobell L. C., Sobell M. B., editors. Assessing Alcohol Problems: a Guide for Clinicians and Researchers Treatment Handbook Series 4. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995, pp. 55–73. [Google Scholar]
- 65. Cunningham J. A., Kypri K., Mccambridge J. The use of emerging technologies in alcohol treatment. Alcohol Res Health 2011; 33: 320–326. [PMC free article] [PubMed] [Google Scholar]
- 66. Santa Ana E. J., Martino S., Ball S. A., Nich C., Frankforter T. L., Carroll K. M. What is usual about ‘treatment‐as‐usual’? Data from two multisite effectiveness trials. J Subst Abuse Treat 2008; 35: 369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Ball J. C., Ross A. The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and Outcomes. New York, NY: Springer‐Verlag; 1991. [Google Scholar]
- 68. Meyers R. J., Villanueva M., Smith J. E. The community reinforcement approach: history and new directions. J Cogn Psychother 2005; 19: 247–260. [Google Scholar]
- 69. Prendergast M., Podus D., Finney J., Greenwell L., Roll J. Contingency management for treatment of substance use disorders: a meta‐analysis. Addiction 2006; 101: 1546–1560. [DOI] [PubMed] [Google Scholar]
- 70. Becker J., Haug S., Sullivan R., Schaub M. P. Effectiveness of different web‐based interventions to prepare co‐smokers of cigarettes and cannabis for double cessation: a three‐arm randomized controlled trial. J Med Internet Res 2014; 16: e273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rollnick S., Miller W. R. What is motivational interviewing? Behav Cogn Psychother 1995; 23: 325. [DOI] [PubMed] [Google Scholar]
- 72. Carroll K. M. A Cognitive–Behavioral Approach: Treating Cocaine Addiction [internet]. Rockville, MD; 1998. Available at: https://archives.drugabuse.gov/pdf/CBT.pdf (accessed 30 July 2016) (Archived at http://www.webcitation.org/6jO06230Y). [Google Scholar]
- 73. Center for Substance Abuse Treatment . Brief Interventions and Brief Therapies for Substance Abuse [internet]. Rockville (MD); 1999. Available at: http://adaiclearinghouse.org/downloads/tip-34-brief-interventions-and-brief-therapies-for-substance-abuse-60.pdf (accessed 26 June 2016) (Archived at http://www.webcitation.org/6iYj18P7a). [Google Scholar]
- 74. Sofuoglu M., DeVito E. E., Waters A. J., Carroll K. M. Cognitive enhancement as a treatment for drug addictions. Neuropharmacology 2013; 64: 452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Darvell M. J., Kavanagh D. J., Connolly J. M. A qualitative exploration of internet‐based treatment for comorbid depression and alcohol misuse. Internet Interv 2015; 2: 174–182. [Google Scholar]
- 76. Bickel W. K., Christensen D. R., Marsch L. A. A review of computer‐based interventions used in the assessment, treatment, and research of drug addiction. Subst Use Misuse 2011; 46: 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Pubmed search string.
Appendix S2 Definition of subgroup analyses.
Appendix S3 Risk of bias assessment.


