Abstract
Individuals with Autism Spectrum Disorder (ASD) have a range of health, community, and social support needs across the lifespan that create age‐specific challenges in navigating service sectors. In this study, we set out to identify the priority needs of individuals with ASD across the lifespan, and the factors that predict receiving priority services. Participants included 3,317 individuals with ASD from a Canada‐wide online caregiver survey, stratified into five age groups (preschool, elementary school age, adolescence, emerging adulthood, adulthood). Priority receipt was calculated as a ratio of current services that corresponded to individualized priority need. Age‐stratified Poisson regression analyses were used to identify the sociodemographic, clinical and systemic predictors of priority receipt. Results indicate that the distribution of priority need varied by age, except for social skills programming, which was a high across all groups. The number of high and moderate priority needs diversified with age. Overall, 30% of individuals had none of their priority needs met and priority receipt decreased with age. Systemic factors were most consistently related to priority receipt across the lifespan. Understanding patterns and correlates of priority needs and use that currently exist in different age groups can inform policies to improve service access. Autism Res 2017, 10: 1436–1447. © 2017 International Society for Autism Research, Wiley Periodicals, Inc.
Keywords: autism spectrum disorder, predictors, service need, service receipt, priority needs
Introduction
Individuals with Autism Spectrum Disorder (ASD) may experience considerable impairments in physical and mental condition, activity limitations and participation restrictions that impact their quality of life. As delineated in the International Classification of Functioning, Disability and Health framework [World Health Organization, 2001], overall health and well being is an outcome of interactions between these domains. For individuals with ASD, impairments in physical and mental health [Jones et al., 2015; Moss, Howlin, Savage, Bolton, & Rutter, 2015; Simonoff et al., 2008; Totsika, Hastings, Emerson, Lancaster, & Berridge, 2011] and adaptive and cognitive functioning [Bal, Kim, Cheong, & Lord, 2015; Shattuck, Narendorf et al., 2012] limit activity levels and restrict full participation in society through recreation, school and vocation [Baldwin, Costley, & Warren, 2014; Keen, Webster, & Ridley, 2015; Nicholas, Attridge, Zwaigenbaum, & Clarke, 2015; White, Scahill et al., 2007]. The preponderance of such difficulties, the variability in level of functioning and ASD severity, and the lifelong nature of the condition complicate service planning, and require a prioritization to address expressed needs and individualized care at different life stages [Moes & Frea, 2002; Stahmer, Schreibman, & Cunningham, 2011].
Individuals with ASD have a high level of both normative and perceived service need (see Bradshaw, 1972 for definitions of service need), even compared to people with other developmental disabilities [Gurney, McPheeters, & Davis, 2006; Narendorf et al., 2011; Vohra, Madhavan, Sambamoorthi, & St Peter, 2014]. Some normative service needs are partly predicated by age. For example, young children with ASD (e.g., less than 5 years of age) often require access to early timely assessments [Johnson & Myers, 2007] and early intervention services [Howlin, Magiati, & Charman, 2009], whereas during the school‐age years, service needs may center on behavior management [Siegel & King, 2014] and school supports [Wei, Wagner, Christiano, Shattuck, & Yu, 2014]. Other service needs may span across age and be driven by clinical presentation, including ASD symptom severity, intellectual disability (ID), physical disability, and concurrent medical conditions [Brown, Ouellette‐Kuntz, Hunter, Kelley, & Cobigo, 2011; Chiri & Warfield, 2012; Zablotsky et al., 2015]. These clinical factors may require supports to address behavior problems [Dawson et al., 2010; Weitlauf et al., 2014], social skills [Schohl et al., 2014], and mental health [Johnco et al., 2015; Ung, Selles, Small, & Storch, 2015; van Steensel & Bögels, 2015].
At the same time, not all individuals with ASD receive the services that they or their families report are needed, making it important to identify the variables that impact receipt. Unmet perceived needs in youth with ASD are associated with more severe clinical outcomes [Brown et al., 2012; Hodgetts, Zwaigenbaum, & Nicholas, 2015], and a host of sociodemographic factors. Racial disparities exist in the age of diagnosis and prevalence. Being White is associated with an early diagnosis compared to being non‐White [Mandell, Listerud, Levy, & Pinto‐Martin, 2002] while prevelance rates of ASD are lower in Latino compared to non‐Latinos [Liptak et al., 2008]. Further, being non‐White is associated with receiving less subspecialty care for comorbid medical conditions [Broder‐Fingert, Shui, Pulcini, Kurowski, & Perrin, 2013; Thomas, Ellis, McLaurin, Daniels, & Morrissey, 2007]. Socioeconomic status (SES) is associated with decreased awareness of services and more structural barriers to access [Pickard & Ingersoll, 2015], and specifically, the use of mental health services [Narendorf et al., 2011]. Additional systemic factors, such as a lack of resources in rural areas and education level, have been predictive of reduced receipt of therapeutic support services, including speech/language therapy, respite care and summer camp services [Thomas, Morrissey et al., 2007].
With the myriad of perceived service needs potentially present during each stage of development across the lifespan, and the awareness of limited resources, a user‐defined prioritization of service provision across the life course is critical in a patient‐centered care context. With the rising prevalence of ASD and the resulting demand for support [Ruble, Heflinger, Renfrew, & Saunders, 2005], the supply of services and distribution of resources must first address priority need [Lavelle et al., 2014]. The objective of this study was to identify the perceived priority needs of individuals with ASD across the lifespan, and the sociodemographic and clinical need variables that predict receiving priority services. Our two aims were to: (1) identify and characterize the priority service needs across different age groups and (2) identify the correlates of current priority service receipt. We hypothesized that there would be differences in priority needs and receipt across the lifespan and various sociodemographic, clinical, and systemic factors would predict priority receipt.
Method
Survey
The Canadian Autism Spectrum Disorders Alliance (CASDA) National Autism Needs Assessment Survey was developed to study the needs of Canadians with ASD through an iterative consultative process with a pan‐Canadian team of advocacy organizations and researchers (for more information on the development of the survey, see Weiss, Whelan, McMorris, Carroll, & the Canadian Autism Spectrum Disorders Alliance, 2014). Recruitment occurred from the beginning of April to the end of June 2014, through 60 CASDA member organizations representing people with ASD and their families in every province and territory in Canada. Organizations sent out notifications up to 2 months prior to the survey launch via members' newsletters. When the survey was launched, email notifications and social media (email and Twitter campaigns) were used to further reach out to families across the country. Organizations were provided with marketing materials to assist with their dissemination efforts. After the first month, gaps in survey penetration were identified and direct phone calls by organizations were made to reach communities with lower response rates. Paper copies were made upon request to those unable to complete the survey online. This sampling approach has been previously used by other researchers [Hodgetts et al., 2015; Kogan et al., 2008; Totsika et al., 2011; Shattuck, Narendorf et al., 2012]. The survey was administered in both English and French. Informed consent was obtained at the beginning of the survey. This research was approved by the university's Ethics Review Board.
Sample Inclusion Criteria
Caregivers were instructed to elect one family member with ASD at a time and complete the entire survey separately for each family member with ASD. All participants were required to report having received an official diagnosis of an ASD (Autism, Asperger Syndrome, Pervasive Developmental Disorder–Not Otherwise Specified [PDD‐NOS], PDD, or Autism Spectrum Disorder) by a licensed physician, psychologist, or nurse practitioner, whose scope of practice includes ASD diagnosis to be included. The use of initials, date of birth, province of residence, postal code, and IP address was used to verify that no duplication occurred. Based on these criteria, 100 cases were eliminated; 63 based on a lack of diagnosis, 35 as duplicates, and 2 were incomplete surveys, resulting in 3,185 caregivers reporting on 3,317 individuals.
Variables
The main dependent variable was the proportion of the top 5 priority services that were received. Respondents indicated (1) current services received in the last 6 months from a list of 23 services and an “other” option that was recoded as needed, and (2) their current top 5 service needs, regardless of what services they had received. The question read, “What are the top FIVE services or supports that you CURRENTLY want for [child's name]?” Participants selected services from the same list in both questions. We calculated a ratio of current receipts that were also identified as top 5 service needs, creating a score that reflects individualized priority service utilization.
Independent variables included clinical, sociodemographic, and systemic indicators. All items were completed by the caregiver in reference to the person with ASD, except when otherwise noted. Overall health status was measured by asking about the individual's current health on a 5‐point Likert scale (1‐poor to 5‐excellent), which was dichotomized as 0–poor or fair health to 1–good, very good, or excellent health; shown to be a valid indicator of morbidity across various populations [Idler & Benyamini, 1997]. A total physical health concerns score was the sum of 30 chronic current physical health conditions that the caregiver identified that was reported by a health care provider [adapted from Gurney et al., 2006]. The question read, “Does [Child's name] currently have these conditions? Select all that [Child's name] currently has.” This question followed immediately after one that asked “Has a doctor or health professional ever told you that [child's name] has any of the following conditions?”, therefore, the question would be understood as querying current conditions as reported by a health professional. Caregivers selected from the following choices: Cerebral Palsy, Tourette Syndrome, Asthma, Diabetes, Epilepsy or seizure disorder, Hearing problems, Vision problems that cannot be corrected with glasses or contact lenses, Bone, joint, or muscle problems, Brain injury or concussion, Chronic gastrointestinal problems (e.g., constipation, acid reflux, diarrhea), Sleep problems/disorder, and an Other field. The Other text was recoded into the following 19 categories that were added to the the original list: Migraine, Sensory disorder, Skin allergy, Severe allergy, Urinary/bladder infection, Systemic immune disorders, Respiratory disorders, Hematology disorders, Cardiovascular diseases, Problems with eating, Thyroid disorders, HPA dysfunction, Growth/gonadal disorders, Renal diseases, Metabolic dysfunction, Other endocrine, Genetic syndromes, Congenital malformations, and Other. A total mental health concerns score was calculated by summing reports about any current psychiatric diagnoses from a provided list (current concerns or diagnosis of anxiety disorder, depression, ADHD/ADD, obsessive‐compulsive disorder, schizophrenia/psychotic disorder or “other,” where “other” was recoded). A behavioral concerns score was the sum of caregiver concerns about any current behavior problems. The question read “Do you have concerns about any of the following for [child's name]? Are there CURRENTLY any problems with: Aggression, Self‐injury, Hurting other, Destruction of property, and Problems with the law.” Caregivers also reported on any current diagnosis of ID, as provided by a healthcare professional.
Sociodemographic measures included the gender of the individual with ASD (recoded as male vs. non‐male), ethnicity (recoded as White/Caucasian vs. non‐White/non‐Caucasian) as well as the highest level of education attained by the caregiver(s). Choices for the size of community were urban, suburban, rural, and remote; the last two choices (rural–19.6%; remote–1.6%) were combined to reflect three groups with more similar numbers. The presence of financial difficulty was determined by asking caregivers “Which of the phrases best describes how you and your family are managing financially these days?” with a 6‐point scale from “we manage very well” to “we are in deep financial trouble” [adapted from Lyon, Tait, & D'Souza, 2005] and dichotomized to reflect any degree of financial trouble. Systemic variables included if respondents could afford services (yes or no), if they currently receive government funding for services (yes or no), the number of caregiver‐directed services received (any of the following: “caregiver training programs, family support/counselling, respite care, or other,” where “other” was recoded as necessary), and number of barriers experienced by the caregiver in accessing services for the individual with ASD, from a list of nine barriers and an “other” category [adapted from Douma, Dekker, De Ruiter, Verhulst, & Koot, 2006]. The question read, “Below are some common reasons why people cannot access services”. Please check off any reasons why [child's name] has not been able to access services he or she needs or would like to have: Cannot afford services, Negative experiences with professionals in the past, Not enough resources—on a waitlist, Lack of trained professionals, Not able to access services because his or her diagnosis does not qualify them for services, Even with a diagnosis, was deemed ineligible for services, [Child's name] is too young to receive the services that he or she needs, [Child's name] is too old to receive the services that he or she needs, Services are too far, Services are not available in the right language, Other barriers (please specify).
Data Analysis
First, the frequency and distribution of the top five service needs and current receipt of those services (priority receipts) were computed. High priority group needs were defined by priority needs that were endorsed by at least 50% of an age group, and moderate priority group needs by priority needs between 25–49%. Age groups were chosen based on transition points in the school system. Second, the correlates of priority receipt were calculated using χ 2 or Spearman's ρ correlation by age group. Variables that were statistically significant (P < .05) at the bivariate level were placed into five separate Poisson regressions to examine age group specific correlates. Poisson regressions were used since dependent variable fitted a count measure distribution. Each model was tested for violations of equidispersion by examining the Chi‐square values relative to the residual degrees of freedom. By age group, the values were .79, 1.04, 1.09, 1.05, and 1.19 for the preschool, elementary, adolescence, emerging adults, and adults respectively, indicating underdispersion in the preschool group and suggesting that our estimates in this group would be more conservative. None of the models were overdispersed, therefore, the five models were maintained for consistency. Caregiver education, community size, presence of ID, health status, mental health concerns, behavioral concerns, ability to afford services, number of caregiver‐directed services, and receipt of government funding were treated as ordinal, and child age, the number of total non‐priority receipts and the number of barriers to service were treated as continuous in final models. Cases with missing data were excluded from the analysis—3 were excluded from the preschool group (n = 225 in group), 78 from the elementary school age group (n = 1479), 39 from the adolescence group (n = 858), 17 from the emerging adult group (n = 550), and 6 from the adult group (n = 205). Regression analyses are presented as adjusted odds ratios (ORs) and 95% confidence intervals (CIs). Post hoc comparisons were corrected using Tukey's LSD method and, for categorical data, adjusted standardize residuals were used. Confidence intervals are reported at α = .05.
Results
Sample Characteristics
The sociodemographic attributes of the sample are displayed in Table 1. The sample of 3,317 individuals was 81.7% (CI: 80.4–83.0%) male, and spanned 2–61 years of age. Based on the low representation of minorities groups, ethnicity was dichotomized to reflect 83.8% (CI: 82.5–85.1) White/Caucasian. The other ethnicities in the sample included “Black or African Canadian” (1.1%), “First Nations/Aboriginal” (0.8%), “multiethnic or multiracial” (2.8%), and “Asian” (6.7%). Most resided in suburban (39.9%, CI: 38.2–41.6%) and urban (38.3%, CI: 36.6–40%) regions, and 42% (CI: 40.3–43.7%) obtained at least an undergraduate university degree. Approximately 24% (CI: 22.6–25.5%) of caregivers reported currently experiencing some or deep financial trouble.
Table 1.
Demographics for Study Sample Based on Caregiver Reports of Individuals With ASD by Age Group
| n (%) or Mean (SD) | χ 2 | ||||||
|---|---|---|---|---|---|---|---|
| Total | 0–4 y.o. | 5–11 y.o. | 12–17 y.o. | 18–24 y.o. | 25+ y.o. | ||
| N = 3317 | n = 225 | n = 1479 | n = 858 | n = 550 | n = 205 | ||
| Sociodemographic factors | |||||||
| Gender (Male) | 2709 (81.7) | 171 (76) | 1212 (82) | 717 (83.6) | 446 (81.1) | 163 (79.5) | 7.8 |
| Ethnicity (Caucasian) | 2779 (83.8) | 168 (74.7) a | 1194 (80.7) a,b | 747 (87.1) b | 483 (87.8) b,c | 187 (91.2) c | 30.1* |
| Time in Canada (>20 years) | 3026 (91.4) | 189 (84) a | 1300 (88.1) a | 804 (93.8) b | 532 (96.9) b | 201 (98) b | 75.2*** |
| Highest level of education (household) | 3.53** | ||||||
| ≤High school‐level certificate | 246 (7.4) | 22 (9.7) a | 104 (7) a | 62 (7.2) a | 43 (7.8) a | 15 (7.3) a | |
| College‐level diploma | 1571 (47.3) | 107 (47.6) a,b | 699 (47.2) a,b | 438 (51) b | 244 (44.4) a,b | 83 (40.5) a | |
| Undergraduate degree | 899 (27.1) | 68 (30.2) a | 422 (28.5) a | 213 (24.8) a | 135 (24.5) a | 61 (29.8) a | |
| Graduate/Professional degree | 517 (15.6) | 25 (11.1) a | 221 (14.9) a,b,c | 119 (13.9) a,c | 107 (19.5) b | 45 (22) b,c | |
| Undisclosed | 84 (2.6) | 3 (1.3) | 33 (2.2) | 26 (3) | 21 (3.8) | 1 (0.5) | |
| Financial difficulty | 798 (24.1) | 60 (26.7) a | 417 (28.2) a | 206 (24) a | 88 (16) b | 27 (13.2) b | 47.5*** |
| Community size | 20.2** | ||||||
| Remote/Rural | 698 (21) | 41 (18.2) a | 300 (20.3) a | 201 (23.4) a | 121 (22) a | 36 (18.5) a | |
| Suburban | 1325 (39.9) | 77 (34.2) a | 613 (41.4) a | 345 (40.2) a | 218 (39.6) a | 72 (35.1) a | |
| Urban | 1269 (38.3) | 106 (47.1) a | 554 (37.4) a,b | 305 (35.5) b | 207 (37.6) a,b | 97 (47.3) a | |
Note. For each variable, if the omnibus test statistic was statistically significant, post hoc comparisons were conducted. Values within the same row that differ are denoted by different superscripts.
*P < .05; **P < .01; ***P < .001.
Clinical and systemic variables by age group are found in Table 2. Intellectual disability was reported in 45.8% (CI: 44.1–47.5%) of cases, occurring more in the emerging adult group than in the other groups (F[4, 3316] = 12.1, P < .001). Few caregivers rated the individual's health status as poor or fair (7.8%, CI: 6.9–8.7%); the adult group was more likely to have poor or fair health compared to the other groups (F[4, 3316] = 13.9, P < .001). On average, individuals experienced 1.3 (SD = 1.5) current physical health conditions, which increased across the age groups (F[4, 3316] = 17.7, P < .001) and had 1.2 (SD = 1.4) behavioral concerns, with fewer concerns in the adult group compared to the elementary school age, adolescent and emerging adult groups (F[4, 3316] = 4.2, P =.002). The number of mental health problems ranged considerably, with the adolescent and both adult groups having more concerns than younger age groups (F[4, 3316] = 81.3, P < .001). Individuals with ASD were currently receiving a mean of 3.2 (SD = 2.4) services overall. Overall receipt was lower in the preschool and elementary school age groups (F[4, 3316] = 22.8, P < .001). Caregivers received on average 1.1 (SD = 0.9) services that were directed to themselves. Overall, 31.7% (CI: 30.1–33.3%) stated they could not afford the services they would like, even though 59.5% (CI: 57.8–61.2%) were receiving some government funding for services. An average of 3.4 (SD = 1.9) types of barriers to accessing services were endorsed.
Table 2.
Profile of Clinical Need and Systemic Factors of Sample as Reported by Caregivers of Individuals With ASD by Age Group
| n (%) or Mean (SD) | F‐value or χ 2 | ||||||
|---|---|---|---|---|---|---|---|
| Total | 0–4 y.o. | 5–11 y.o. | 12–17 y.o. | 18–24 y.o. | 25+ y.o. | ||
| N = 3317 | n = 225 | n = 1479 | n = 858 | n = 550 | n = 205 | ||
| Clinical need variables | |||||||
| Intellectual disability | 1520 (45.8) | 101 (44.9) a | 604 (40.8) a | 394 (45.9) a | 317 (57.6) b | 104 (45.8) a,b | 47.8*** |
| Health status (poor or fair vs. other) | 260 (7.8) | 14 (6.2) a | 88 (5.9) a | 66 (7.7) a | 50 (9.1) a | 42 (20.5) b | 54.7*** |
| No. of physical health conditions | 1.24 (1.43) | 0.85 (1.24) a | 1.09 (1.34) a,b | 1.34 (1.47) b,c | 1.48 (1.48) c,d | 1.24 (1.43) d | 17.7*** |
| No. of behavioral concerns | 1.19 (1.40) | 1.03 (1.37) a | 1.23 (1.39) b | 1.24 (1.42) b | 1.19 (1.46) b | 1.19 (1.40) a | 4.21** |
| No. of mental health concerns | 1.17 (0.90) | 0.47 (0.63) a | 1.02 (0.83) b | 1.41 (0.91) c | 1.39 (0.91) c | 1.17 (0.90) c | 81.3*** |
| Systemic factors | |||||||
| Services (cannot afford) | 1053 (31.7) | 74 (32.9) | 474 (32) | 280 (32.6) | 160 (29.1) | 1054 (31.7) | 2.3 |
| Gov't funding (have received) | 1973 (59.5) | 99 (44.2) a | 841 (57.4) b | 559 (65.6) c | 357 (65.5) c | 1380 (60) a,b,c | 46.1*** |
| No. of caregiver‐directed services | 1.09 (0.94) | 0.87 (0.85) a | 1.08 (0.89) b | 1.19 (1.00) b | 1.14 (0.98) b | 0.87 (0.95) a | 8.86*** |
| No. of barriers to services | 3.39 (1.88) | 2.77 (1.60) a | 3.24 (1.74) a | 3.61 (1.99) b | 3.63 (2.03) b,c | 3.49 (2.03) c | 14.1*** |
| No. of services received | 3.20 (2.44) | 3.89 (1.97) a | 3.50 (2.35) a | 3.00 (2.47) b | 2.66 (2.48) b,c | 2.52 (2.70) b,c | 22.8*** |
Note. For each variable, if the omnibus test statistic was statistically significant, post hoc comparisons were conducted. Values within the same row that differ are denoted by different superscripts.
The range of physical health conditions was from 0 to 11.
The range of behavioural concerns was from 0 to 5.
The range of mental health concerns was from 0 to 4.
The range of caregiver‐directed services was from 0 to 4.
The range of barriers to services was from 0 to 11.
The range of services received was from 0 to 15.
*P < .05; **P < .01; ***P < .001.
Patterns of Priority Needs
Caregivers picked the top five services currently needed for their child. Overall, social skills programs were a high priority need across all five age groups at 61.4% (CI: 59.7–63.1%). Activity‐based programs (43.2%, CI: 41.5–44.9%), recreational programs (41.8%, CI: 40.1–43.5%), life skills training (36.9%, CI: 35.3–38.5%), employment training and adult day programs (28.0%, CI: 26.5–29.5%), specialized summer camps (26.5%, CI: 25–28%), and early interventions that were not characterized as intensive behavioral intervention (IBI) (26.0%, CI: 24.5–27.5%) all emerged as moderate priority needs across the entire sample.
The priority needs by age groups are shown in Table 3, with high and moderate needs shaded in gray. Priority needs varied by cohort, except for social skills programming, which was high for all ages. In addition to social skills, early intervention, activity‐based and daycare programs emerged as high priority needs for the preschool group. At the elementary school ages, activity and recreation‐based programs and specialized summer camps were high priority needs. For adolescents, life skills training was the only high priority need. For adults, there was a high priority need for employment training and adult day programs, and for emerging adults, life skills training. There were also a considerable number of moderate needs including respite in preschool, behavior management in elementary school, activity and recreation‐based programs and mental health treatments for adolescents and adults, and housing for adults.
Table 3.
Distribution of Current Priority Service Needs Endorsed by Caregivers of Individuals With ASD by Age Group
| % of Individuals (95% CI) | |||||
|---|---|---|---|---|---|
|
0–4 y.o. (n = 225) |
5–11 y.o. (n = 1479) |
12–17 y.o. (n = 858) |
18–24 y.o. (n = 550) |
25+ y.o. (n=205) |
|
| Early detection | 8 (4.5–11.5) | 2.6 (1.8–3.4) | 1.9 (1–2.8) | 1.1 (0.2–2) | 2.4 (0.3–4.6) |
| Early intensive behavioural intervention (IBI) | 72 (66.1–77.9) | 17 (15.1–18.9) | 2.4 (1.4–3.5) | ‐ | ‐ |
| Non‐IBI early intervention | 72.4 (66.6–78.3) | 24.1 (21.9–26.2) | 4.3 (3–5.7) | ‐ | ‐ |
| Applied behaviour analysis (not early or intensive) | ‐ | 0.9 (0.5–1.4) | ‐ | ‐ | ‐ |
| OT/PT (not part of early intervention) | ‐ | 1.5 (0.9–2.1) | 1 (0.4–1.7) | ‐ | ‐ |
| Speech language (not part of early intervention) | ‐ | 0.9 (0.4–1.4) | 1 (0.4–1.7) | ‐ | ‐ |
| Daycare programs | 53.3 (46.8–59.9) | 8.2 (6.8–9.6) | 1.5 (0.7–2.3) | ‐ | ‐ |
| After school programs | 4.9 (2.1–7.7) | 27.7 (25.4–29.9) | 19.6 (16.9–22.2) | 4.5 (2.8–6.3) | ‐ |
| Recreational programs | 41.8 (35.3–48.2) | 50.5 (48–53.1) | 44.8 (41.4–48.1) | 36 (32–40) | 36.1 (29.5–42.7) |
| Social skills programs | 61.3 (55–67.7) | 74.4 (72.2–76.7) | 70.5 (67.5–73.6) | 50 (45.8–54.2) | 50.7 (43.9–57.6) |
| Activity‐based programs | 53.8 (47.3–60.3) | 57.6 (55.1–60.1) | 43.7 (40.4–47) | 29.5 (25.6–33.3) | 31.2 (24.9–37.6) |
| Specialized summer camps | 19.6 (14.4–24.7) | 47.1 (44.6–49.7) | 39.7 (36.5–43) | 16.4 (13.3–19.5) | 9.8 (5.7–13.8) |
| Housing | ‐ | 2 (1.3–2.7) | 8.3 (6.4–10.1) | 38.2 (34.1–42.2) | 42.4 (35.7–49.2) |
| Diagnostic assessments | 9.8 (5.9–13.7) | 12.2 (10.5–13.8) | 13.9 (11.6–16.2) | 9.5 (7–11.9) | 15.6 (10.6–20.6) |
| Respite | 28.9 (23–34.8) | 30.4 (28.1–32.8) | 23.9 (21–26.7) | 22.4 (18.9–25.8) | 12.7 (8.1–17.2) |
| Specialized transportation | ‐ | 3.6 (2.6–4.5) | 3.7 (2.5–5) | 7.5 (5.3–9.6) | 8.8 (4.9–12.7) |
| Mental health treatment | ‐ | 15.1 (13.3‐17) | 25.2 (22.3–28.1) | 26.5 (22.9–30.2) | 30.2 (24–36.5) |
| Crisis intervention | ‐ | 3.5 (2.6–4.5) | 4.9 (3.5–6.3) | 6.2 (4.2–8.2) | 7.8 (4.1–11.5) |
| Behaviour management for behaviour problems | 19.6 (14.4–24.7) | 36.6 (34.1–39) | 28.4 (25.4–31.5) | 18.7 (15.5–22) | 17.6 (12.4–22.8) |
| Community safety training | 7.1 (3.8–10.5) | 17.2 (15.3–19.2) | 23.2 (20.4–26) | 18.7 (15.5–22) | 19.5 (14.1–24.9) |
| Life skills training | 7.6 (4.1–11) | 24.7 (22.5–26.9) | 56.8 (53.4–60.1) | 54.9 (50.8–59.1) | 40.5 (33.8–47.2) |
| Post ‐secondary education | ‐ | 3.2 (2.3–4.1) | 24.2 (21.4–27.1) | 42.4 (38.2–46.5) | 25.4 (19.4–31.3) |
| Employment training and adult program | ‐ | 1.4 (0.8–1.9) | 16.8 (14.3–19.3) | 63.1 (59.1–67.1) | 58.5 (51.8–65.3) |
Note. Cells with “‐” have a low response rate (n < 5), so % not provided.
High (>50%) and moderate (25–49.9%) needs shaded in dark and light gray, respectively.
Priority Receipts
Priority receipt was calculated by asking if participants were currently receiving services that corresponded to their current priority needs (from 0—no current priority needs had received services, to 5—all priority needs had services). Overall, 30.6% (CI: 29.1–32.2%) received no priority services, 28.1% (CI: 26.6–29.7%) received 1 priority service, 20.4% (CI: 19.1–21.8%) received 2, 12.8% (CI: 11.6–13.9%) received 3, and only 8% (CI: 7.1–8.9%) had at least four. The preschool group received more priority services (M = 1.85, CI: 1.68–2.01) than the elementary school group (M = 1.56, CI: 1.49–1.63), who had more priority receipt than the older groups (adolescent: M = 1.26, CI: 1.18–1.35; emerging adults: M = 1.15, CI: 1.05–1.25; adults: M = 1.3, CI: 0.98–1.36; F[4, 3272] = 21.49, P < .001; see Fig. 1).
Figure 1.
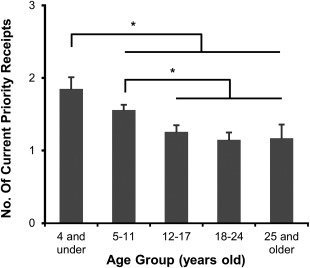
Differences in the number of current priority service receipts (from 0 to 5) across the lifespan for individuals with ASD, as reported by caregivers (mean ± 95% CI); * statistically significant difference, P < .05.
Correlates and Predictors of Priority Receipt
The bivariate correlates among independent variables and the number of priority receipts for each age group are shown in Table 4. Variables that were statistically significant at a bivariate level were placed in Poisson regressions by age group (see Table 5). In the preschool group, priority receipt was related to the ability to afford services (OR = 1.32, CI: 1.06–1.64) and having 3 or more caregiver‐directed services (OR = 1.64, CI: 1.11–2.45). In the elementary school age group, each increase in the level of household education and of community size increased the likelihood of priority receipt, while having two or more mental health concerns decreased receipt (OR = 0.83, CI: 0.73–0.93). All the systemic factors predicted priority receipt in this age group. In the adolescent group, though caregiver education, the presence of ID, and of behavioral concerns was related at the bivariate level, only systemic factors were predictive of priority receipt. Specifically, receiving government funding (OR = 1.18, CI: 1.02–1.37), having more caregiver‐direct services (up to an OR = 1.83, CI: 1.45–2.31, for 3+ services), and receiving each additional non‐priority service (OR = 1.15, CI: 1.11–1.19) influenced the number of priority receipts. For emerging adults, having 1–2 caregiver‐direct services and more non‐priority services received increased the likelihood of obtaining priority receipt (OR = 1.17, CI: 1.13–1.22), whereas for the 25+ group, having a diagnosis of ID increased the chances of obtaining priority receipt (OR = 1.35, CI: 1–1.83), in addition to more non‐priority services (OR = 1.19, CI: 1.11–1.28).
Table 4.
Selected Factors Associated With Priority Service Receipts in Individuals With ASD by Age Group
| 0–4 y.o. | 5–11 y.o. | 12–17 y.o. | 18–24 y.o. | 25+ y.o. | ||
|---|---|---|---|---|---|---|
| n = 223 | n = 1458 | n = 850 | n = 541 | n = 199 | Statistic | |
| Sociodemographic factors | ||||||
| Age | 0.04 | −0.13*** | −0.13*** | 0.07 | 0.03 | Spearman's ρ |
| Household education | 15.36 | 36.92** | 23.99 | 17.11 | 16.77 | χ 2 |
| Community size | 20.39* | 25.43** | 10.61 | 16.46 | 7.75 | χ 2 |
| Clinical need variables | ||||||
| Health status | 1.6 | 6.79 | 1.46 | 3.52 | 3.21 | χ 2 |
| Intellectual disability | 3.97 | 4.48 | 13.13* | 19.29** | 18.57** | χ 2 |
| No. of behavioural concerns (0 to 3+) | −0.01 | −0.05 | 0.07* | 0.08 | 0.12 | Spearman's ρ |
| No. of mental health concerns (0 to 2+) | 0.04 | −0.10*** | 0.01 | −0.04 | −0.01 | Spearman's ρ |
| Systemic factors | ||||||
| Services (affordability) | 15.82** | 36.97*** | 4.4 | 9.44 | 3 | χ 2 |
| Government funding (ever received) | 6.67 | 29.38*** | 33.53*** | 20.18** | 3.22 | χ 2 |
| No. of caregiver‐directed services (0 to 3+) | 0.18** | 0.20*** | 0.31*** | 0.18*** | 0.19** | Spearman's ρ |
| No. of barriers to services | 0.07 | −0.08** | 0.01 | −0.08 | 0.02 | Spearman's ρ |
| No. of non‐priority services received | 0.01 | 0.22** | 0.40*** | 0.36*** | 0.43*** | Spearman's ρ |
Table 5.
Adjusted ORs (and 95% CIs) for Selected Factors Associated With Current Priority Receipt in Individuals With ASD by Age Groups
| OR (95% CI) (*P < .05, **P < .01, ***P < .001) | |||||
|---|---|---|---|---|---|
| 0–4 y.o. | 5–11 y.o. | 12–17 y.o. | 18–24 y.o. | 25+ y.o. | |
| Sociodemographic factors | |||||
| Highest level of education (in household) | |||||
| ≤High school‐level certificate | 1 | 1 | |||
| College‐level diploma | 1.26 (1.04–1.53)* | 0.93 (0.73–1.19) | |||
| Undergraduate degree | 1.43 (1.17–1.75)*** | 1.04 (0.8–1.35) | |||
| Graduate/Professional degree | 1.44 (1.16–1.78)** | 1.15 (0.87–1.52) | |||
| Community size | |||||
| Remote/Rural | 1 | 1 | |||
| Suburban | 1.24 (0.93–1.66) | 1.14 (1.01–1.29)* | |||
| Urban | 1.12 (0.85–1.48) | 1.13 (1–1.28)* | |||
| Clinical need factors | |||||
| Intellectual disability | |||||
| Absent | 1 | 1 | 1 | ||
| Present | 1.03 (0.91–1.18) | 1.09 (0.91–1.31) | 1.35 (1–1.83)* | ||
| Behavioral concerns | |||||
| None | 1 | ||||
| 1 | 1.1 (0.93–1.29) | ||||
| 2 | 1.01 (0.83–1.22) | ||||
| 3+ | 0.93 (0.79–1.1) | ||||
| Mental health concerns | |||||
| None | 1 | ||||
| 1 | 1 (0.9–1.1) | ||||
| 2+ | 0.83 (0.73–0.93)** | ||||
| Systemic factors | |||||
| Services | |||||
| Cannot afford | 1 | 1 | |||
| Can afford | 1.32 (1.06–1.64)* | 1.21 (1.09–1.33)*** | |||
| Gov't funding | |||||
| Never received | 1 | 1 | 1 | ||
| Have received | 1.17 (1.07–1.28)*** | 1.18 (1.02–1.37)* | 1.12 (0.92–1.36) | ||
| Caregiver‐directed services | |||||
| None | 1 | 1 | 1 | 1 | 1 |
| 1 | 1.22 (0.98–1.52) | 1.18 (1.06–1.32)** | 1.44 (1.2–1.73)*** | 1.4 (1.13–1.74)** | 1.24 (0.9–1.69) |
| 2 | 1.29 (0.95–1.75) | 1.33 (1.18–1.51)*** | 1.75 (1.44–2.13)*** | 1.36 (1.06–1.73)* | 1.07 (0.71–1.62) |
| 3+ | 1.64 (1.11–2.45)* | 1.66 (1.41–1.97)*** | 1.83 (1.45–2.31)*** | 1.31 (0.97–1.77) | 1.37 (0.85–2.19) |
| Barriers to services | 0.96 (0.93–0.98)** | ||||
| Non‐priority services received | 1.07 (1.04–1.1)*** | 1.15 (1.11–1.19)*** | 1.17 (1.13–1.22)*** | 1.19 (1.11–1.28)*** | |
Discussion
This is the first study to examine patterns of recent service use, in light of current priority needs, in a large sample of individuals with ASD, stratified into preschool, elementary school, adolescence, emerging adult and adult age groups. In a sample of individuals with ASD across Canada, we found that only a small proportion of individuals received services that corresponded to their endorsed priority needs and that priority service receipt decreased with age. Last, we found that predictors of priority receipt also varied by age.
There is an increasing challenge in aligning access to services with the pressing needs of individuals with ASD across the lifespan. While the emphasis in the literature has been on needs in general, no other study had identified perceived priority needs and related receipts across different age groups. Understanding patterns and correlates of priority service use across the lifespan can help to inform policies to improve service access. In addition, our study is unique in terms of the sample size and statistical power. Previous work had combined age ranges across key developmental periods (e.g., preschool and elementary school age) [Hodgetts et al., 2015; Montes, Halterman, & Magyar, 2009], which may mask distinct effects in particular cohorts.
Individuals with ASD often have a high level of service need, relative to other groups with developmental disabilities [Vohra et al., 2014]. Across the lifespan, early intervention services [Howlin et al., 2009], followed by behavior management [Siegel & King, 2014)] and school supports [Wei et al., 2014] are relevant for children whereas services related to community programs, school success, and life skills training are typically needed as adolescents transition to adulthood [Orsmond, Krauss, & Seltzer, 2004; Shattuck, Wagner, Narendorf, Sterzing, & Hensley, 2011], followed by residential needs and supports for advanced education or vocational success in adulthood [Lounds Taylor et al., 2012; Shattuck, Roux et al. 2012]. We observed a pattern of priority needs reflecting this age‐specific pattern. Notably, our data shows a broadening of need across a greater number of areas after the preschool age. The preschool age group was consistent in its priority needs, with five identified as high (agreed on by at least 50% of the sample), and two as moderate (endorsed by 25–49%), whereas in the elementary school age group, four were high and three were moderate. This trending spread of priority needs continues in adolescence (two high and five moderate), through emerging adulthood (three high and four moderate) into adulthood (two high and five moderate), and points to an age‐related diversification of need. These data suggest that an approach emphasizing individualized service planning that involve multiple sectors is needed to address the priority needs in adolescences and adults with ASD [Lubetsky, Handen, Lubetsky, & McGonigle, 2014].
This study is the first to examine if an individual receives what they currently deem a priority need. It may strike some that if an individual receives services for a need (a met need), then that need is perceived to be non‐priority and subsequent attention and prioritization would be shifted to another area of need. However, that is not necessarily the case as our data shows that approximately 40% of the sample received services for at least two of their priority needs, indicating some alignment between priority need and receipt and suggesting that an area of met need may still be deemed a priority. At the same time, only a small proportion received services that address all of their priority needs, even as they may currently be receiving other services, indicating a potential misalignment of service availability with their current situation or that the overall level of perceived need is not currently being adequately addressed by existing services. And even within this context of overall low priority receipt, our data affirms that the service system as a whole is relatively more aligned with the priority needs of young children with ASD [Gerhardt & Lainer, 2011]. This age related pattern will likely change with the increasing recognition of ASD needs across the life course [Pellicano, Dinsmore, & Charman, 2014; Shepherd & Waddell, 2015].
Systemic factors were consistent at predicting priority receipt across age groups, even though the types of priority needs varied. Studies have highlighted that individuals with developmental disorders, including ASD, face multiple barriers to accessing services [Einfeld et al., 2006; Krauss, Gulley, Sciegaj, & Wells, 2003]. Even in situations of high support need, barriers related to a lack of information about care, the ability of the service to meet client needs, waitlists, and eligibility requirements [Weiss & Lunsky, 2010]. Interestingly, one of the most consistent factors across age groups was the number of caregiver‐directed services, reflecting the importance of embedding family support into the service system oriented to the individual with ASD [Benevides, Carretta, & Mandell, 2016; Golnik, Ireland, & Borowsky, 2009]. Also, the ability to afford service increased the odds of priority receipt in the youngest two age groups, and the presence of government funding increased the odds in the elementary school age and adolescent groups. Priority needs in these age groups often are costly and may not be adequately covered under the current publicly available system, making affordability or funding significant contributors to receipt. For instance, evidence‐based intensive early intervention often costs between $40,000 and 75,000 per year [Motiwala, Gupta, Lilly, Ungar, & Coyte, 2006], and ineligible or wait‐listed families may pay out of pocket for timely access [Järbrink, Fombonne, & Knapp, 2003]. The increased odds of priority receipt due to both affordability and funding at the younger ages may also reflect that the financial resources of younger families play an important role, and that government funding is needed to augment timely priority receipt.
Specific service receipt is often driven by clinical presentation, including ASD symptom severity, ID, physical disability, and concurrent medical conditions [Chiri & Warfield, 2012; Zablotsky et al., 2015]. In our bivariate analyses, some clinical factors were also related to priority service receipt. However, few clinical needs emerged as statistically significant when considering all the variables together, suggesting that while we may tend to focus on these factors in determining priority service provision, they do not drive access to the broader array of health, education, and social service needs that people with ASD require. For example, while the presence of mental health concerns may indeed trigger priority service around mental health care, it may be provided in an isolated way and not related to broader case coordinator of service delivery [Carbone, Behl, Azor, & Murphy, 2009]. One exception was that having 2 or more mental health concerns decreased the likelihood of priority receipt in the elementary school age group. Given that the majority of individuals with ASD have at least one mental health concern [Simonoff et al., 2008], having two or more could represent a level that the pediatric service system is not equipped to address during an age period when these problems often first emerge. The other clinical predictor was the presence of ID status in adults. Others have shown that this variable enables access to adult services [Taylor & Henninger, 2015], possibly because eligibility for adult services is often determined based on ID status, whereas child and youth service receipt is predicated by an ASD diagnosis.
This study has a number of limitations. First, the survey was based on caregiver report of ASD, without clinical validation and data are limited by parents' knowledge and recollection, which could impact the validity of the results as reflecting the true priority needs of those with ASD. While not the gold standard in ascertainment, several large scale family caregiver surveys have used caregiver report of official diagnosis and other variables [Kogan et al., 2009, 2008; Lin, Yu, & Harwood, 2012; Totsika et al., 2011; Shattuck, Narendorf et al., 2012] and a verification study showed reliability of diagnosis by caregivers [Daniels et al., 2012]. Second, our data was collected by convenience sampling using primarily online methods, which may have created barriers to participation for some families. Survey penetration into rural and ethnic minority communities was low compared to the demographics of the general population. At the same time, our sample demographics were similar in many respects to other Canadian studies that also use convenience sampling [Hodgetts et al., 2015] and to non‐Canadian caregiver report studies [Kogan et al., 2008; Shattuck, Narendorf et al., 2012; Totsika et al., 2011], and our rates of clinical need are in line with rates reported in other jurisdictions [Van Naarden Braun et al., 2015]. Third, this study was a cross sectional design and cohort effects such as the needs or predictor variables of people at different ages may change over time. Fourth, we were not able to reach a larger proportion of older adults in our survey and therefore, this study is limited in our ability to understanding the changing needs and receipts of individual with ASD throughout their adult life. Fifth, the survey did not measure ASD severity and as a result, this study was not able to examine how ASD symptomology affected service need and receipt.
In conclusion, this study identifies age group specific priority needs and predictors of priority receipt in the ASD service system. It highlights the complexity of navigating multiple service sectors to address these changing needs, which can ultimately result in a high burden for individuals with ASD and their caregivers, and speaks to the importance of intersectoral planning and treatment provision. This study suggests that coordinated system reforms that allow for individualized care plans could provide supports in priority areas for individuals with ASD and their families. Future research examining the cost‐effectiveness of targeting priority need through specific services [e.g., Penner et al., 2015] and comparing those with various levels of priority receipt will determine the utility of focusing on priority need. Changes in policies that determine parent support, service funding, and align needs with service availability, will be key to ensuring priority receipt across the life course and sectors.
Author Contributions
Both authors have made substantial contributions to the conception and design and/or analysis and interpretation of the data; authors have been involved in drafting and revising the article and have given final approval of the version submitted for publication and agree to be accountable for all aspects of this work. Dr. Lai carried out the data analysis and co‐wrote the manuscript equally. Dr. Weiss conceptualized and designed the study, carried out the data collection, and co‐wrote the manuscript equally.
Acknowledgments
We wish to acknowledge the Canadian Autism Spectrum Disorders Alliance (CASDA) with special thanks to Margaret Whelan and Cynthia Carroll for their input on the survey and in recruitment, and Carly McMorris for research assistant support on earlier work related to the dataset. A particular thanks to all the individuals with ASD and their families who participated in this survey, and to Yona Lunsky for her reviews of the survey design. The National ASD Needs Assessment Survey was administered by CASDA with financial support from The Public Health Agency of Canada (PHAC). All phases of this study were also funded by the Chair in Autism Spectrum Disorders Treatment and Care Research to Dr. Weiss (#RN284208; Canadian Institutes of Health Research in partnership with Autism Speaks Canada, the Canadian Autism Spectrum Disorders Alliance, Health Canada, NeuroDevNet and the Sinneave Family Foundation. Additional funds from York University). The authors declare no conflict of interest in this study.
References
- Bal, V.H. , Kim, S.‐H.H. , Cheong, D. , & Lord, C. (2015). Daily living skills in individuals with autism spectrum disorder from 2 to 21 years of age. Autism: The International Journal of Research and Practice, 19, 774–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin, S. , Costley, D. , & Warren, A. (2014). Employment activities and experiences of adults with high‐functioning autism and Asperger's Disorder. Journal of Autism and Developmental Disorders, 44, 2440–2449. [DOI] [PubMed] [Google Scholar]
- Benevides, T.W. , Carretta, H.J. , & Mandell, D.S. (2016). Differences in perceived need for medical, therapeutic, and family support services among children with ASD. Pediatrics, 137, 2–85. [DOI] [PubMed] [Google Scholar]
- Bradshaw, J. (1972). A taxonomy of social need In McLachlan G. (Ed.), Problems and progress in medical care. Oxford University Press: Oxford. [Google Scholar]
- Broder‐Fingert, S. , Shui, A. , Pulcini, S.D. , Kurowski, D. , & Perrin, J.M. (2013). Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics, 132, 94–100. [DOI] [PubMed] [Google Scholar]
- Brown, H.K. , Ouellette‐Kuntz, H. , Hunter, D. , Kelley, E. , & Cobigo, V. (2012). Unmet needs of families of school‐aged children with an autism spectrum disorder. Journal of Applied Research in Intellectual Disabilities: JARID, 25, 497–508. [DOI] [PubMed] [Google Scholar]
- Brown, H.K. , Ouellette‐Kuntz, H. , Hunter, D. , Kelley, E. , & Cobigo, V. , & Lam, M. (2011). Beyond an autism diagnosis: Children's functional independence and parents' unmet needs. Journal of Autism and Developmental Disorders, 41, 1291–1302. [DOI] [PubMed] [Google Scholar]
- Carbone, P.S. , Behl, D.D. , Azor, V. , & Murphy, N.A. (2009). The medical home for children with autism spectrum disorders: Parent and pediatrician perspectives. Journal of Autism and Developmental Disorders, 40, 317–324. [DOI] [PubMed] [Google Scholar]
- Chiri, G. , & Warfield, M.E. (2012). Unmet need and problems accessing core health care services for children with autism spectrum disorder. Maternal and Child Health Journal, 16, 1081–1091. [DOI] [PubMed] [Google Scholar]
- Daniels, A.M. , Rosenberg, R.E. , Anderson, C. , Law, J.K. , Marvin, A.R. , & Law, PA. (2012). Verification of parent‐report of child autism spectrum disorder diagnosis to a web‐based autism registry. Journal of Autism and Developmental Disorders, 42, 257–265. [DOI] [PubMed] [Google Scholar]
- Dawson, G. , Rogers, S. , Munson, J ., Smith, M ., Winter, J ., Greenson, J ., … Varley, J . (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125, e17–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douma, J.C.H. , Dekker, M.C. , De Ruiter, K.P. , Verhulst, F.C. , & Koot, H.M. (2006). Help‐seeking process of parents for psychopathology in youth with moderate to borderline intellectual disabilities. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 1232–1242. [DOI] [PubMed] [Google Scholar]
- Einfeld, S.L. , Piccinin, A.M. , Mackinnon, A ., Hofer, S. M., Taffe , J., Gray , M K.., … Tonge, B.J . (2006). Psychopathology in young people with intellectual disability. JAMA, 296, 1981–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt, P.F. , & Lainer, I. (2011). Addressing the needs of adolescents and adults with autism: A crisis on the horizon. Journal of Contemporary Psychotherapy, 41, 37–45. [Google Scholar]
- Golnik, A. , Ireland, M. , & Borowsky, I.W. (2009). Medical homes for children with autism: A physician survey. Pediatrics, 123, 966–971. [DOI] [PubMed] [Google Scholar]
- Gurney, J.G. , McPheeters, M.L. , & Davis, M.M. (2006). Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Archives of Pediatrics & Adolescent Medicine, 160, 825–830. [DOI] [PubMed] [Google Scholar]
- Hodgetts, S. , Zwaigenbaum, L. , & Nicholas, D. (2015). Profile and predictors of service needs for families of children with autism spectrum disorders. Autism: The International Journal of Research and Practice, 19, 673–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin, P. , Magiati, I. , & Charman, T. (2009). Systematic review of early intensive behavioral interventions for children with autism. American Journal on Intellectual and Developmental Disabilities, 114, 23–41. [DOI] [PubMed] [Google Scholar]
- Idler, E.L. , & Benyamini, Y. (1997). Self‐rated health and mortality: A review of twenty‐seven community studies. Journal of Health and Social Behavior, 38, 21–27. [PubMed] [Google Scholar]
- Järbrink, K. , Fombonne, E. , & Knapp, M. (2003). Measuring the parental, service and cost impacts of children with autistic spectrum disorder: A pilot study. Journal of Autism and Developmental Disorders, 33, 395–402. [DOI] [PubMed] [Google Scholar]
- Johnco, C.J. , Nadai, A.S.D. , Lewin, A.B. , Ehrenreich‐May, J. , Wood, J.J ., & Storch, E.A . (2015). defining treatment response and symptom remission for anxiety disorders in pediatric autism spectrum disorders using the Pediatric Anxiety Rating Scale. Journal of Autism and Developmental Disorders, 45, 3232–3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, C.P. , & Myers, S.M. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120, 1183–1215. [DOI] [PubMed] [Google Scholar]
- Jones, K.B. , Cottle, K. , Bakian, A ., Farley, M ., Bilder, D ., Coon, H ., & McMahon, W.M . (2015). A description of medical conditions in adults with autism spectrum disorder: A follow‐up of the 1980s Utah/UCLA Autism Epidemiologic Study. Autism: The International Journal of Research and Practice, 20, 551–561. [DOI] [PubMed] [Google Scholar]
- Keen, D. , Webster, A. , & Ridley, G. (2015). How well are children with autism spectrum disorder doing academically at school? An overview of the literature. Autism: The International Journal of Research and Practice, 20, 276–294. [DOI] [PubMed] [Google Scholar]
- Kogan, M.D. , Blumberg, S.J. , Schieve, L.A. , Boyle, C.A. , Perrin, J.M. , Ghandour, R.M. , … van Dyck, P.C. (2009). Prevalence of parent‐reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics, 124, 1395–1403. [DOI] [PubMed] [Google Scholar]
- Kogan, M.D. , Strickland, B.B. , Blumberg, S.J. , Singh, G.K. , Perrin, J.M. , & van Dyck, P.C. (2008). A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005‐2006. Pediatrics, 122, 58. [DOI] [PubMed] [Google Scholar]
- Krauss, M.W. , Gulley, S. , Sciegaj, M. , & Wells, N. (2003). Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Mental Retardation, 41, 329–339. [DOI] [PubMed] [Google Scholar]
- Lavelle, T.A. , Weinstein, M.C. , Newhouse, J.P. , Munir, K. , Kuhlthau, K.A. , & Prosser, L.A. (2014). Economic burden of childhood autism spectrum disorders. Pediatrics, 133, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, S.C. , Yu, S.M. , & Harwood, R.L. (2012). Autism spectrum disorders and developmental disabilities in children from immigrant families in the United States. Pediatrics, 130, 7. [DOI] [PubMed] [Google Scholar]
- Liptak, G.S. , Benzoni, L.B. , Mruzek, D.W. , Nolan, K.W. , Thingvoll, M.A. , Wade, C.M. , & Fryer, G.E. (2008). Disparities in diagnosis and access to health services for children with autism: Data from the National Survey of Children's Health. Journal of Developmental and Behavioral Pediatrics, 29, 152–160. [DOI] [PubMed] [Google Scholar]
- Lounds Taylor, J. , Dove, D. , Veenstra‐VanderWeele, J. , Sathe, N.A. , McPheeters, M.L. , Jerome, R.N. , & Warren, Z. (2012). Interventions for adolescents and young adults with autism spectrum disorders. Comparative Effectiveness Review No. 65. AHRQ Publication No. 12‐EHC063‐EF. Rockville, MD: Agency for Healthcare Research and Quality. [PubMed]
- Lubetsky, M.J. , Handen, B.L. , Lubetsky, M. , & McGonigle, J.J. (2014). Systems of care for individuals with autism spectrum disorder and serious behavioral disturbance through the lifespan. Child and Adolescent Psychiatric Clinics of North America, 23, 97–110. [DOI] [PubMed] [Google Scholar]
- Lyon, N. , C., Tait ., & D'Souza, J. (2005). Families and Children Study (FACS) 2003, Wave 5 technical report, London: National Centre for Social Research.
- Mandell, D.S. , Listerud, J. , Levy, S.E. , & Pinto‐Martin, J.A. (2002). Race differences in the age at diagnosis among medicaid‐eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1447–1453. [DOI] [PubMed] [Google Scholar]
- Moes, D.R. , & Frea, W.D. (2002). Contextualized behavioral support in early intervention for children with autism and their families. Journal of Autism and Developmental Disorders, 32, 519–533. [DOI] [PubMed] [Google Scholar]
- Montes, G. , Halterman, J.S. , Magyar, C.I. (2009). Access to and satisfaction with school and community health services for US children with ASD. Pediatrics, 124, 13. [DOI] [PubMed] [Google Scholar]
- Moss, P. , Howlin, P. , Savage, S. , Bolton, P. , & Rutter, M. (2015). Self and informant reports of mental health difficulties among adults with autism findings from a long‐term follow‐up study. Autism: The International Journal of Research and Practice, 19, 832–841. [DOI] [PubMed] [Google Scholar]
- Motiwala, S.S. , Gupta, S. , Lilly, M.B. , Ungar, W.J. , & Coyte, P.C. (2006). The cost‐effectiveness of expanding intensive behavioural intervention to all autistic children in Ontario: In the past year, several court cases have been brought against provincial governments to increase funding for Intensive Behavioural Intervention (IBI). This economic evaluation examines the costs and consequences of expanding an IBI program. Healthcare Policy = Politiques De Santé, 1, 135–151. [PMC free article] [PubMed] [Google Scholar]
- Narendorf, S.C. , Shattuck, P.T. , & Sterzing, P.R. (2011). Mental health service use among adolescents with an autism spectrum disorder. Psychiatric Services, 62, 975–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narendorf, S.C. , Fedoravicius, N. , McMillen, J.C. , McNelly, D. , & Robinson, D.R. (2012). Stepping down and stepping in: Youth's perspectives on making the transition from residential treatment to treatment foster care. Children and Youth Services Review, 34, 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas, D.B. , Attridge, M. , Zwaigenbaum, L. , & Clarke, M. (2015). Vocational support approaches in autism spectrum disorder: A synthesis review of the literature. Autism: The International Journal of Research and Practice, 19, 235–245. [DOI] [PubMed] [Google Scholar]
- Orsmond, G.I. , Krauss, M.W. , & Seltzer, M.M. (2004). Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders, 34, 245–256. [DOI] [PubMed] [Google Scholar]
- Pellicano, E. , Dinsmore, A. , & Charman, T. (2014). What should autism research focus upon? Community views and priorities from the United Kingdom. Autism: The International Journal of Research and Practice, 18, 756–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner, M. , Rayar, M. , Bashir, N. , Roberts, S.W. , Hancock‐Howard, R.L. , & Coyte, P.C. (2015). Cost‐Effectiveness analysis comparing pre‐diagnosis autism spectrum disorder (ASD)‐targeted intervention with Ontario's Autism Intervention Program. Journal of Autism and Developmental Disorders, 45, 2833. [DOI] [PubMed] [Google Scholar]
- Pickard, K.E. , & Ingersoll, B.R. (2015). Quality versus quantity: The role of socioeconomic status on parent‐reported service knowledge, service use, unmet service needs, and barriers to service use. Autism: The International Journal of Research and Practice, 20, 106–115. [DOI] [PubMed] [Google Scholar]
- Ruble, L.A. , Heflinger, C.A. , Renfrew, J.W. , & Saunders, R.C. (2005). Access and service use by children with autism spectrum disorders in Medicaid Managed Care. Journal of Autism and Developmental Disorders, 35, 3–13. [DOI] [PubMed] [Google Scholar]
- Schohl, K.A. , Van Hecke, A.V. , Carson, A.M. , Dolan, B. , Kars, J. , & Stevens, S. (2014). A replication and extension of the PEERS intervention: Examining effects on social skills and social anxiety in adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 532–545. [DOI] [PubMed] [Google Scholar]
- Shattuck, P.T. , Narendorf, S.C. , Cooper, B. , Sterzing, P.R. , Wagner, M. , & Taylor, J.L. (2012). Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics, 129, 1042–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck, P.T. , Roux, A.M. , Hudson, L.E. , Taylor, J.L. , Maenner, M.J. , & Trani, J.F. (2012). Services for adults with an autism spectrum disorder. Canadian Journal of Psychiatry. Revue Canadienne De Psychiatrie, 57, 284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck, P.T. , Wagner, M. , Narendorf, S. , Sterzing, P. , & Hensley, M. (2011). Post‐high school service use among young adults with an autism spectrum disorder. Archives of Pediatrics & Adolescent Medicine, 165, 141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd, C.A. , & Waddell, C. (2015). A qualitative study of autism policy in Canada: Seeking consensus on Children's services. Journal of Autism and Developmental Disorders, 45, 3550–3664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel, M. , & King, B.H. (2014). Autism and developmental disorders: Management of serious behavioral disturbance. Child and Adolescent Psychiatric Clinics of North America, 23, xii–xv. [DOI] [PubMed] [Google Scholar]
- Simonoff, E. , Pickles, A. , Charman, T. , Chandler, S. , Loucas, T. , & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population‐derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 921–929. [DOI] [PubMed] [Google Scholar]
- Stahmer, A.C. , Schreibman, L. , & Cunningham, A.B. (2011). Toward a technology of treatment individualization for young children with autism spectrum disorders. Brain Research, 1380, 229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, J.L. , & Henninger, N.A. (2015). Frequency and correlates of service access among youth with autism transitioning to adulthood. Journal of Autism and Developmental Disorders, 45, 179–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, K.C. , Ellis, A.R. , McLaurin, C. , Daniels, J. , & Morrissey, J.P. (2007). Access to care for autism‐related services. Journal of Autism and Developmental Disorders, 37, 1902–1912. [DOI] [PubMed] [Google Scholar]
- Totsika, V. , Hastings, R.P. , Emerson, E. , Lancaster, G.A. , & Berridge, D.M. (2011). A population‐based investigation of behavioural and emotional problems and maternal mental health: Associations with autism spectrum disorder and intellectual disability. Journal of Child Psychology and Psychiatry, and allied disciplines, 52, 91–99. [DOI] [PubMed] [Google Scholar]
- Ung, D. , Selles, R. , Small, B.J. , & Storch, E.A. (2015). A systematic review and meta‐analysis of cognitive‐behavioral therapy for anxiety in youth with high‐functioning autism spectrum disorders. Child Psychiatry and Human Development, 46, 533–547. [DOI] [PubMed] [Google Scholar]
- Van Naarden Braun, K. , Christensen, D. , Doernberg, N. , Schieve, L. , Rice, C. , Wiggins, L. , …, Yeargin‐Allsopp, M. (2015). Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan atlanta, 1991‐2010. PLoS One, 10, e0124120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Steensel, F.J. , & Bögels, S.M. (2015). CBT for anxiety disorders in children with and without autism spectrum disorders. Journal of Consulting and Clinical Psychology, 83, 512–523. [DOI] [PubMed] [Google Scholar]
- Vohra, R. , Madhavan, S. , Sambamoorthi, U., & St Peter, C. (2014). Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism: The International Journal of Research and Practice, 18, 815–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei, X. , Wagner, M. , Christiano, E.R. , Shattuck, P. , & Yu, J.W. (2014). Special education services received by students with autism spectrum disorders from preschool through high school. The Journal of Special Education, 48, 167–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, J. , & Lunsky, Y. (2010). Service utilization patterns in parents of youth and adults with intellectual disability who experienced behavioral crisis. Journal of Mental Health Research in Intellectual Disabilities, 3, 145–163. [Google Scholar]
- Weiss, J.A. , Whelan, M. , McMorris, C. , Carroll, C. , & The Canadian Autism Spectrum Disorders Alliance. (2014). Autism in Canada: National needs assessment survey for families, individuals with autism spectrum disorder and professionals. Available from: http://www.casda.ca/#ourwork
- Weitlauf, A.S. , McPheeters, M.L. , Peters, B. , Sathe, N. , Travis, R. , Aiello, R. , & Warren, Z. (2014). Therapies for children with autism spectrum disorder: Behavioral interventions update. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014 Aug. (Comparative Effectiveness Review, No. 137.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK241444/ [PubMed]
- White, S.W. , Scahill, L. , Klin, A. Koeng, K. , & Volkmar, F.R. (2007) Educational placements and service use patterns of individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37, 1403–1412. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2001) International classification of functioning, disability and health (ICF). Geneva: World Health Organization. [Google Scholar]
- Zablotsky, B. , Pringle, B.A. , Colpe, L.J. , Kogan, M.D. , Rice, C. , & Blumberg, S.J. (2015). Service and treatment use among children diagnosed with autism spectrum disorders. Journal of Developmental and Behavioral Pediatrics: JDBP, 36, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]


