Abstract
An open prospective controlled study was designed to compare the efficacy of short‐term dynamic group psychotherapy with the standard treatment in patients with depressive symptoms attended in the primary care setting. A total of 115 patients with depressive symptoms were assigned to receive psychotherapy (75 min) over 9 months (37 to 39 sessions) (n = 70) or the standard care (n = 45). Outcome measures were the differences between baseline and post‐treatment in the 17‐item Hamilton Depression Rating Scale (HDRS), Hamilton Anxiety Rating Scale (HAM‐A) and the Short‐Form Health Survey (SF‐12) questionnaire in the two study groups. At the end of dynamic group psychotherapy, statistically significant improvements in the mean scores of all questionnaires were observed, whereas in control patients, significant improvements were only observed in the HDRS‐17 scale and in the Mental Component Summary score of the SF‐12. The mean changes after treatment were also higher in the psychotherapy group than in controls in all outcome measures, with statistically significant differences in the mean differences in favour of the psychotherapy group. In summary, implementation of short‐term dynamic group psychotherapy run by experienced psychotherapists for patients with depressive symptoms attended in routine primary care centres is feasible and effective. © 2016 The Authors. Clinical Psychology & Psychotherapy published by John Wiley & Sons Ltd.
Key Practitioner Message
Short‐term dynamic group psychotherapy was delivered as a non‐pharmacological intervention to improve depressive symptoms.
Statistically significant differences as compared with a control group were observed in 17‐item Hamilton Depression Rating Scale (HDRS), Hamilton Anxiety Rating Scale (HAM‐A) and the Short‐Form Health Survey (SF‐12) questionnaire.
Implementation of short‐term dynamic group psychotherapy run by experienced psychotherapists for patients with depressive symptoms attended in routine primary care centres is feasible and effective.
Keywords: Dynamic Group Psychotherapy, Primary Care, Depressive Symptoms, Prospective Controlled Study
Introduction
Depressive disorders and their management is a great concern because of the high prevalence and high burden in terms of disability, treatment costs, effects of families and carers, and loss of workplace productivity (Sobocki, Jönsson, Angst, & Rehnberg, 2006; Mathers & Loncar, 2006; Gustavsson et al., 2011). Depression is a leading cause of disability worldwide and a major contributor to the global burden of disease (Ferrari et al., 2013; Miller, Dell'Osso, & Ketter, 2014; WHO, 2015). Patients with mental disorders receive treatment mostly in the context of primary care (Serrano‐Blanco et al., 2010). More than 80% of patients with depression are managed and treated in primary care, with those seen in secondary care being skewed towards much more severe disease (Timonen & Liukkonen, 2008). Depressed hospitalized patients differ considerably in clinical characteristics from psychiatric outpatient depressives, and clinical features influence the family physician's decision to treat with antidepressants (Lampe, 2012).. Although primary care remains a major access point for the management of depression, significant shortcomings have been recognized in detection, prescription of adequate antidepressant treatment and achievement of remission (Pence, O'Donnell, & Gaynes, 2012; Unützer & Park, 2012; Lesage, 2015). By focusing mainly on somatic complaints and diseases, general practitioners often fail to identify an underlying mental disorder (Minović et al., 2015). Also, clinically significant depressive symptoms are highly prevalent in primary care patients, but the percentage of patients citing depression as a reason for visit is markedly low (Zung, Broadhead, & Roth, 1993). In primary care settings, it has been shown that screening programmes without substantial staff‐assisted depression care supports are unlikely to improve outcomes (O'Connor, Whitlock, Beil, & Gaynes, 2009).
Most primary care physicians initiate and monitor treatment of depression with various pharmacological agents, but owing to time limitation, lack of knowledge or inexperience they are often unable to provide effective non‐pharmacological therapeutic modalities to their patients, although psychotherapeutic interventions are recommended by clinical practice guidelines (American Psychiatric Association, 2000a; National Institute for Health and Care Excellence, 2010). In fact, depression can be effectively monitored in primary care if physicians follow established guidelines and systematically track progress (Manning & Jackson, 2015). Likewise, implementation of a multi‐component programme with clinical, educational and organizational procedures in primary care has proven to be effective (Aragonès et al., 2012).
Dynamically oriented psychotherapies are effective interventions in a variety of mental disorders, including depression. A recent meta‐analysis in which 23 studies of short‐term psychodynamic psychotherapy for depression were evaluated showed a significant decrease in depressive symptoms compared with control conditions (Driessen et al., 2010). In a randomized pilot investigation, moderate‐to‐large effect sizes in favour of a brief dynamic psychotherapy as compared with treatment as usual were reported in patients with moderate‐to‐severe depression in the community mental health system (Gibbons et al., 2012). However, detailed and reliable data characterizing community‐based psychodynamic group therapy in the real‐world setting is limited (Garland et al., 2010; Lorentzen & Ruud, 2014). Moreover, clinical trials assessing the effectiveness of psychodynamic psychotherapy in patients with depressive symptoms selected by the family physician and carried out in the primary care setting are lacking.
Therefore, the objective of the present study was to evaluate through a prospective controlled clinical study, the effectiveness of a short‐term dynamic group psychotherapy performed in the primary care setting and addressed to patients with depressive symptoms referred to dynamic group psychotherapy by family physicians themselves. The final goal was to determine whether results obtained in an investigation close to the patient's social and clinical reality may help to design evidence‐based specific effective interventions to improve the outcome of depression.
Method
Participants
A prospective open‐label prospective and controlled study was designed to test the hypothesis that short‐term dynamic group psychotherapy delivered in the primary care setting could improve symptoms and quality of life in patients with depressive symptoms attended by the family physician. Between 2011 and 2013, patients aged 25 years or older with depressive symptoms attended by family physicians working in six primary care centres of Santa Coloma de Gramenet, Barcelona (Spain) were eligible. Santa Coloma de Gramenet is an urban area adjacent to the city of Barcelona, with a total population of 126 000 inhabitants. Patients with history or current use of cannabis, cocaine, heroin and alcohol were excluded from the study, as were patients with borderline personality disorder, psychotic symptoms (delirium, hallucinations), cognitive impairment of organic cause and fibromyalgia. The Mini‐Mental State Examination (MMSE) was administered to all patients older than 65 years of age to exclude age‐related cognitive dementia. The study was approved by the Ethics Committee of Parc de Salut Mar, and written informed consent was obtained from all patients.
Study Procedures
Informative sessions were carried out at each primary care centre. The objective of these sessions was to explain the audience the characteristics of group therapy for patients with depressive symptoms, how it works and how it can help.
Patients with depressive symptoms who met the inclusion criteria were assigned to psychodynamic psychotherapy (intervention) when they were referred by their family physician within the time of recruitment of a group therapy. A total of eight psychotherapy groups across the 3‐year study period, with 75‐min weekly sessions were established. Duration of treatment was 9 months (37–39 weeks). Typically, groups included eight or nine participants and were closed to new participants after the third session. Patients were stratified by ages (decades) for treatment, so that psychotherapies were homogeneous within a given age range. Instructions regarding the range of age that patients should have to be included in psychotherapy groups were given to family physicians by electronic mail. Patients who were not referred within the time of recruitment of a group therapy were included in a control group. The family physician was unaware of the group (intervention or control) to which the patient was finally included. All patients were initially interviewed by a psychiatrist for clinical evaluation, to establish diagnoses according to DSM IV criteria, and to complete the study instruments. After 9 months, patients and controls were interviewed again to assess the clinical outcome.
Treatment
All dynamic psychotherapy sessions were performed in two primary care centres. At the initial interview (assessment visit), participants were explained that group psychotherapy was a space that was sought that everyone could think about and communicate their feelings. The objective of the group was to listen, be heard and to understand what was explained. At the same time, this was an opportunity to have a group experience and to understand what happens in the group. Verbal or written information was not provided.
The conceptual model followed the principles of psychodynamic psychotherapy described by Blagys and Hilsenroth (2000) emphasizing the following areas (with the level of empirical support given in parentheses): (1) a focus on affect and the expression of patient's emotions (strong support), (2) and exploration of patients' attempts to avoid topics or engage in activities that hinder the progress of therapy (strong support), (3) the identification of patterns in patients' actions, thoughts, feelings, experiences and relationships (strong support), (4) an emphasis on past experiences (strong support), (5) a focus on a patients' interpersonal experiences (strong support), (6) an emphasis on the therapeutic relationship (moderate support), and (7) an exploration of patients' wishes, dreams or fantasies (moderate support).
The group psychotherapy technique is based on the concept of the group as a unit of thought, shared most of the time unconsciously, which allows highlighting the individual characteristics of each member of the group (Bion, 1961). The role of the therapist to help the group to carry out the task has been explicitly elaborated in the initial interview. Within the framework described, therapists try to clarify participants' distressing situations, facilitate communication and interpret the unconscious group dynamics, with the aim to enable participants to gain more insight. In this way participants can achieve a better understanding of themselves, improve interpersonal relationships, evolve improving symptoms and reach more adaptive attitudes in everyday life. Treatment is not exclusively directed to specific disorders.
Nondirective psychotherapy was conducted by a psychiatrist–psychotherapist (aged 56 years at the beginning of the study) with more than 20‐year experience in group psychotherapy and with the collaboration of different less experienced co‐therapists in five of the eight psychotherapies. Psychotherapists met regularly after psychotherapy to assess the progress of treatment as well as to discuss Yalom's therapeutic factors, particularly group cohesiveness, hope and interpersonal relationships (Yalom, 2005). All the sessions were recorded on DVD to verify a posteriori adaptation to manuals of group psychotherapy and to perform further studies in the future. Moreover, sessions were supervised regularly by an external expert in group therapy.
Patients assigned to the control group were visited at least once a month by their family physician.
Outcome Measures
Outcome measures included the 17‐item Hamilton Depression Rating Scale (HDRS‐17) and the Hamilton Anxiety Rating Scale (HAM‐A), total and subscale Psychic Anxiety and Somatic Anxiety for the assessment of depression and anxiety, respectively, and the 12‐item Short‐Form Health Survey (SF‐12) questionnaire for the assessment of health‐related quality of life. The SF‐12 measures eight health aspects, namely physical functioning, role limitations because of physical health problems, bodily pain, general health, vitality, social functioning, role limitations because of emotional problems and mental health. Two subscales are derived from the SF‐12: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Higher scores represent better health (scores greater than 50 represent above average health status). Spanish validated versions of the HDRS‐17 (Ramos‐Brieva & Cordero, 1986), HAM‐A (Lobo et al., 2002), and SF‐12 (Schmidt et al., 2012) instruments were used. A score < 7 in the HDRS‐17 represents an absence of depressive symptoms. Other data recorded included demographics (age, gender), diagnosis and antidepressant treatment prescribed by the family physician. Psychiatric diagnoses were established according to DSM‐IV‐TR criteria (American Psychiatric Association, 2000b).
Statistical Analysis
Categorical variables were compared with the chi‐square (χ2) test or the Fisher's exact probability test. Differences in the HDRS‐17, HAM‐A (total score, psychic and somatic subscales), and the Physical and Mental Components Summary scores (PCS/MCS) of the SF‐12 between baseline and post‐treatment (at 9 months) in the intervention and control groups were analysed with the Student's t‐test for independent data. Mean differences of changes were analysed with the Student's t‐test for paired data. The size effect (standardized mean effect) was expressed as Cohen's d. The relationship between initial severity of depression and anxiety and improvement after treatment was assessed with the Pearson's 'product–moment correlation coefficient (r). Analyses were performed in the intention to treat (ITT) data set (patients who attended at least one group psychotherapy session and controls evaluated at baseline) with the last observation carried forward (LOCF) technique for missing data, and in the per‐protocol (PP) data set (patients who completed all dynamic group psychotherapy sessions and patients in the control group evaluated at 9 months). Statistical significance was set at p < 0.05. Data were analysed with the SPSS‐20 statistical programme.
Results
The patient flow is shown in Figure 1. A total of 122 patients referred by the family physician, 7 did not meet the inclusion criteria at the initial interview. Of the remaining 115 patients, 70 started dynamic group psychotherapy and 45 were included in the control group. Twelve patients (17.1%) in the psychotherapy group and 14 (31.1%) in the control group did not complete the 9‐month study period. Therefore, 58 patients completed all psychotherapy group sessions and 31 patients in the control group were evaluated at 9 months. The ITT data set included 115 patients (dynamic group psychotherapy 70, controls 45) and the PP data set included 89 patients (dynamic group psychotherapy 58, controls 31).
Figure 1.
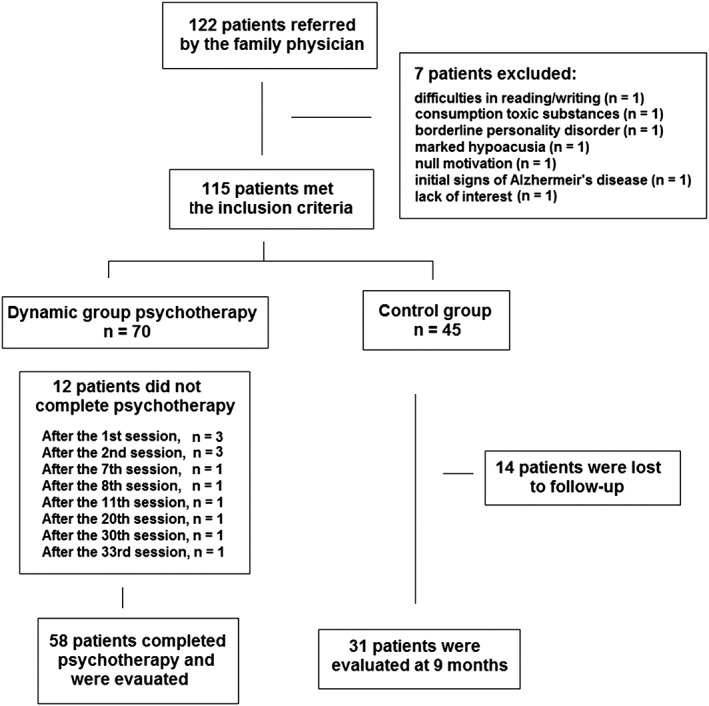
Flow chart of the patients included in the dynamic group psychotherapy and in the control group
As shown in Table 1, the percentages of men and women were higher and lower, respectively, in the psychotherapy group than those in the control group (p = 0.038) but differences in age and psychiatric diagnosis were not observed. Also, no significant differences were found between patients who completed the study and those who did not regarding baseline demographic variables, psychiatric diagnoses and mean scores of anxiety, depression and quality of life.
Table 1.
Demographic features and psychiatric diagnosis in the study groups at the time of recruitment
| Psychotherapy group (n = 70) | Control group (n = 45) | p Value | |
|---|---|---|---|
| Gender | |||
| Males | 25 (35.7) | 8 (17.8) | .038 |
| Females | 45 (64.3) | 37 (82.2) | |
| Age, years, mean (SD) | 49.1 (15.04) | 48.4 (12.3) | .803 |
| Diagnoses | |||
| Dysthymia | 14 (20) | 7 (15.5) | .492 |
| Cyclothymia | 0 | 1 (2.2) | |
| Major depressive disorder | 36 (51.4) | 27 (60) | |
| Adjustment disorder | 20 (28.6) | 10 (22.2) | |
| Completed the study (n = 89) | Did not complete the study (n = 26) | ||
| Gender | |||
| Males | 25 (28.1) | 8 (30.8) | .790 |
| Females | 64 (71.9) | 18 (69.2) | |
| Age, years, mean (SD) | 48.5 (13.6) | 50.0 (15.6) | .624 |
| Diagnoses | |||
| Major depressive disorder* | 49 (55.1) | 15 (57.4) | .543 |
| Dysthymia | 19 (21.3) | 3 (11.5) | |
| Adjustment disorder | 21 (23.6) | 8 (30.8) | |
| HAM‐A, mean (SD) | |||
| Psychic anxiety | 16.12 (4.78) | 15.38 (3.99) | .433 |
| Somatic anxiety | 12.08 (5.90) | 12.38 (5.12) | .797 |
| Total score | 28.15 (9.30) | 27.53 (8.04) | .737 |
| HDRS‐17 total score, mean (SD) | 20.23 (5.26) | 19.38 (6.03) | .581 |
| PCS score, mean (SD) | 41.13 (8.70) | 42.15 (10.27) | .647 |
| MCS score, mean (SD) | 30.34 (8.33) | 31.19 (10.83) | .712 |
Included one case of cyclothymia.
Data as numbers and percentages in parenthesis unless otherwise stated.
Except for two patients treated with benzodiazepines, the remaining patients were treated with selective serotonin re‐uptake inhibitors (SSRIs) or serotonin and norepinephrine re‐uptake inhibitors (SNRIs in five patients) at least for 3 months before the assessment interview. Only 21% of the patients had been visited in specialized centres on one or more occasions.
Table 2 shows the mean (SD) values of the HDRS‐17, HAM‐A (total score, psychic and somatic subscales), and the PCS and MCS scores of the SF‐12 at baseline and at the end of treatment in the intervention and the control groups both in the analyses of the ITT and PP data sets. At baseline the study sample was homogeneous with high scores in the depression and anxiety scales and low quality of life. At the end of dynamic group psychotherapy, statistically significant improvements in the mean scores of all questionnaires were observed, both in the ITT and PP populations. In control patients, significant improvements were only observed in the HDRS‐17 scale and in the MCS score of the SF‐12.
Table 2.
Mean (SD) scores at baseline and at the end of the study in patients undergoing dynamic group psychotherapy and in controls
| Dynamic group psychotherapy | Control group | |||||||
|---|---|---|---|---|---|---|---|---|
| No. patients | Baseline | Post‐treatment | p Value | No. patients | Baseline | At 9 months | p Value | |
| HAM‐A | ||||||||
| Psychic anxiety | ||||||||
| ITT data set | 70 | 15.43 (4.14) | 10.13 (4.69) | <.001 | 45 | 15.73 (4.25) | 15.02 (5.23) | .182 |
| PP data set | 58 | 15.62 (4.19) | 9.22 (4.33) | <.001 | 31 | 14.94 (3.59) | 13.9 (4.95) | .184 |
| Somatic anxiety | ||||||||
| ITT data set | 70 | 12.53 (5.34) | 6.87 (4.55) | <.001 | 45 | 11.71 (4.61) | 12.06 (5.91) | .697 |
| PP data set | 58 | 12.74 (5.38) | 5.91 (3.79) | <.001 | 31 | 11.98 (5.24) | 12.22 (6.05) | .699 |
| Total score | ||||||||
| ITT data set | 70 | 27.80 (8.39) | 17.0 (8.25) | <.001 | 45 | 27.47 (8.25) | 27.24 (10.18) | .830 |
| PP data set | 58 | 28.19 (8.64) | 15.16 (7.25) | <.001 | 31 | 26.29 (6.73) | 25.97 (9.83) | .831 |
| HDRS‐17 total score | ||||||||
| ITT data set | 70 | 19.26 (6.03) | 9.73 (6.38) | <.001 | 45 | 20.07 (5.59) | 18.18 (6.36) | .029 |
| PP data set | 58 | 19.31 (6.21) | 7.81 (4.67) | <.001 | 31 | 19.52 (5.79) | 16.77 (6.45) | .028 |
| PCS score | ||||||||
| ITT data set | 70 | 41.37 (10.1) | 44.19 (10.21) | .010 | 45 | 42.79 (9.73) | 43.29 (11.52) | .428 |
| PP data set | 58 | 41.89 (10.36) | 45.29 (10.27) | .010 | 31 | 42.64 (10.3) | 40.99 (10.8) | .431 |
| MCS | ||||||||
| ITT data set | 70 | 31.78 (11.3) | 42.43 (10.89) | <.001 | 45 | 29.78 (8.47) | 33.18 (11.13) | .020 |
| PP data set | 58 | 31.71 (12) | 45.17 (10.13) | <.001 | 31 | 30.21 (8.39) | 35.16 (11.6) | .019 |
HAM‐A = Hamilton Anxiety Rating Scale. ITT = intention to treat. PP = per protocol. HDRS‐17 = 17‐item Hamilton Depression Rating Scale. PCS = Physical Component Summary. MCS = Mental Component Summary.
In both the ITT and PP data sets, the mean (SD) changes after treatment were also higher in the psychotherapy group than in controls in all outcome measures, with statistically significant differences in the mean differences in favour of the psychotherapy group: HAM‐A total anxiety, 10.57 (95% confidence interval [CI] 7.50–13.64, p < 0.001); HDRS‐17, 7.63 (95% CI 5.25–10.02, p < 0.001); PCS, 3.95 (95% CI 0.49–7.41, p = 0.026) and MCS, 7.73 (95% CI 3.38–12.09, p = 0.001) (Table 3). Large effect sizes were found for improvements in total anxiety (d = 1.25) and depression (d = 1.23) and medium effect sizes for improvements in PCS (d = 0.45) and MCS (d = 0.64).
Table 3.
Mean (SD) changes after treatment and mean differences in the two study groups
| Mean (SD) changes after treatment | Mean differences (95% confidence interval) | p Value | ||||
|---|---|---|---|---|---|---|
| No. patients | Psychotherapy group | No. patients | Control group | |||
| HAM‐A | ||||||
| Psychic anxiety | ||||||
| ITT data set | 70 | −5.30 (5.36) | 45 | −0.71 (3.52) | 4.58 (2.94 to 6.23) | <.001 |
| PP data set | 58 | −6.39 (5.26) | 31 | −1.03 (4.22) | 5.36 (2.94 to 6.23) | <. 001 |
| Somatic anxiety | ||||||
| ITT data set | 70 | −5.65 (5.56) | 45 | 0.24 (4.18) | 5.90 (4.09 to 7.70) | <.001 |
| PP data set | 58 | −6.82 (5.42) | 31 | 0.35 (5.06) | 7.18 (4.83 to 9.52) | <. 001 |
| Total score | ||||||
| ITT data set | 70 | −10.08 (9.69) | 45 | −0.22 (6.89) | 10.57 (7.50 to 13.64) | <.001 |
| PP data set | 58 | −23.03 (9.16) | 31 | −0.32 (8.35) | 12.71 (8.77 to 16.64) | <. 001 |
| HDRS‐17 total score | ||||||
| ITT data set | 70 | −9.52 (6.71) | 45 | −1.88 (5.59) | 7.63 (5.25 to 10.02) | <.001 |
| PP data set | 58 | −11.50 (5.61) | 31 | −2.74 (6.59) | 8.75 (6.11 to 11.39) | <. 001 |
| PCS score | ||||||
| ITT data set | 70 | 2.82 (8.90) | 45 | −1.34 (9.50) | 3.95 (0.49 to 7.41) | .026 |
| PP data set | 58 | 3.40 (9.69) | 31 | −1.64 (11.48) | 5.05 (0.47 to 9.62) | .031 |
| MCS | ||||||
| ITT data set | 70 | 11.14 (14.1) | 45 | 3.40 (9.47) | 7.73 (3.38 to 12.09) | .001 |
| PP data set | 58 | 13.45 (14.7) | 31 | 4.94 (11.13) | 8.5 (2.57 to 14.3) | .005 |
HAM‐A = Hamilton Anxiety Rating Scale. ITT = intention to treat. PP = per protocol. HDRS‐17 = 17‐item Hamilton Depression Rating Scale. PCS = Physical Component Summary. MCS = Mental Component Summary.
As shown in Figures 2 and 3, there was a statistically significant relationship between severity of anxiety and depression at baseline and improvements after treatment in the PP population (r = −0.670, p < 0.001 for total anxiety; r = −0.692, p < 0.001 for depression). In the ITT population, the relationship between severity of anxiety and depression at baseline and improvements after treatment was also statistically significant (r = − 0.591, p < 0.001 for total anxiety; r = −0.504, p < 0.001 for depression).
Figure 2.
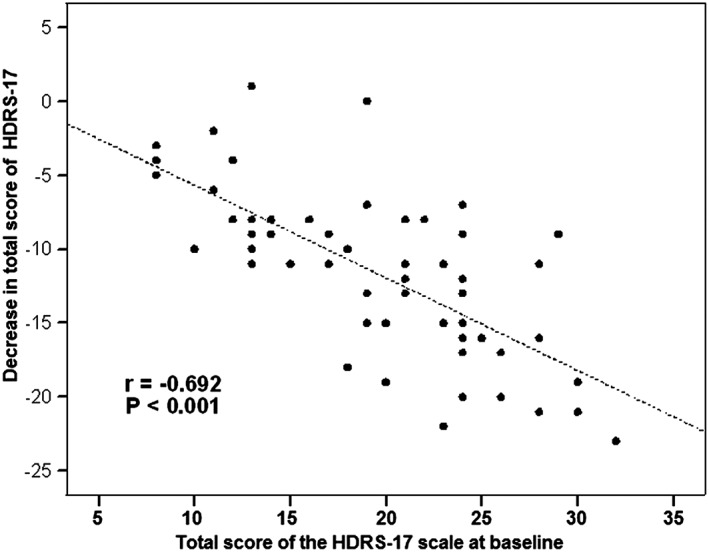
Correlation between severity of depressive symptoms at baseline and improvement after treatment (PP population)
Figure 3.
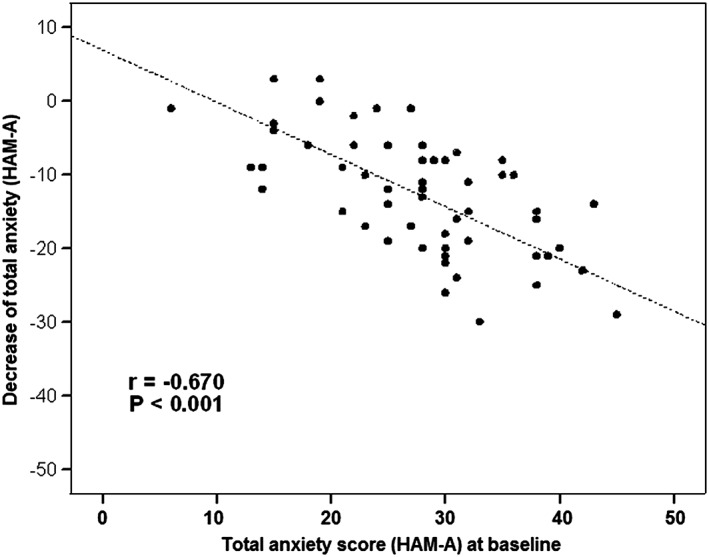
Correlation between severity of anxiety at baseline and improvement after treatment (PP population)
At the end of the study, the percentage of patients with absence of depressive symptoms (score < 7 in the HDRS‐17) was 44.8% (26/58) in the dynamic group psychotherapy and 12.9% (4/31) in the control group (p < 0.001).
To assess whether psychotherapy was consistent with characteristics of dynamic psychotherapy reported by Blagys and Hilsenroth (2000), a random sample of two sessions recorded on DVD was evaluated by four independent experts in psychotherapy. Of the 138 interventions carried out by therapists in the two sessions, the four experts agreed that 89% of the content corresponded to the characteristics established by Blagys and Hilsenroth (2000).
Discussion
The present study evaluates the effect of adding dynamic group psychotherapy to pharmacological treatment for patients with depressive symptoms attended in the primary care setting. Short‐term dynamic psychotherapy (weekly sessions over a 9‐month period) conducted by experienced psychotherapists and delivered at the primary care centres was effective in reducing symptoms of anxiety and depression, as well as improving health‐related quality of life. The effect size was very large for anxiety and depression and moderate for quality of life. The moderate effect size for the PCS and MCS of the SF‐12 may be explained by the presence of two psychotherapy groups with patients older than 65 years of age, in which the presence of other chronic conditions is common. Also, the observation of a significant correlation between severity of anxiety and depression at baseline and improvement after treatment indicates that dynamic group psychotherapy is a valuable complementary strategy for patients with severe disease. The fact that similar results were obtained in the PP and ITT analyses (in ITT analysis the estimation of the treatment effect is more conservative) adds strength to the present findings.
In our country, it has been reported that about 70% of patients with mental health disorders are exclusively treated by family physicians (Serrano‐Blanco et al., 2010). Although depressive disorders are the most common mental health problems in the community setting, screening instruments are not diagnostic tools and their use may overestimate the prevalence of depression (Bros Cugat & Jara Martin, 2015). Despite strong efforts, the diagnosis and management of depression bring many challenges in the primary care setting. There is no evidence from randomized controlled trials (RCTs) of better health outcomes as a result of screening for depression. In fact, there are numerous factors suggesting that depression screening, even with collaborative depression care, may not be beneficial for patients. These include the high rate of patients already treated, uncertainty about the ability of depression screening tools to accurately identify previously unrecognized patients and relatively small treatment effects among patients with less severe depression who would be most likely to be identified through screening. According to recommendations of the Canadian Task Force on Preventive Health Care (CTFPHC), routine screening would expose some patients to avoidable risks and would pose a significant cost burden (Thombs & Ziegelstein, 2013). Also, the United States Preventive Services Task Force (USPSTF) recommendation to screen adults for depression in primary care settings when staff‐assisted depression management programmes are available is not supported by evidence from any RCTs that are directly relevant to the recommendation (Thombs et al., 2014). In our study, no routine screening method was used. Patients with depressive symptoms were evaluated by the family physician and diagnosis of depression confirmed by criteria of the DSM‐IV‐R. Then, patients who gave consent were referred to dynamic group psychotherapy.
In terms of potential limitations, the non‐blinded evaluation of patients and the unknown number of patients who were approached by the family physician and refused treatment should be considered. However, in order to cause a minimum interference in referrals, patients were assigned to psychodynamic psychotherapy when they were referred by the family physician within the time of recruitment of a group therapy, otherwise they were included as controls. Also, data were obtained from validated symptom‐oriented measures and in real‐world clinical practice. The high percentage of women and the distribution of diagnosis of severity of disease are consistent with data reported in other studies (Ruiz, Silva, & Miranda, 2001; Blackmore et al., 2009). The fact that age limit was not an inclusion criteria may explain the high mean age of our patients (49.1 years), and it has been shown that dynamic group psychotherapy is beneficial for elderly people (Canete, Stormont, & Esquerro, 2000). Patients discontinued group therapy mostly during the first sessions, as previously reported (Blackmore, Tantam, Parry, & Chambers, 2012), although a more comprehensive assessment of the indication of psychotherapy or in‐depth evaluation of the patients' motivation may reduce the number of patients lost to continue with treatment. The number of patients lost to follow‐up was greater among controls. One of the reasons may be the lack of contact with the research team over a long period of 9 months.
Different studies, including an excellent systematic review (Blackmore et al., 2009), have provided evidence of the efficacy of dynamic psychotherapy across a variety of settings, conditions and measures (Crits‐Christoph, 1992; Piper et al., 2001; Shedler, 2010; Lorentzen, Ruud, Fjeldstad, & Høglend, 2013), but to our knowledge data on the usefulness of dynamic group psychotherapy in patients with depressive symptoms carried out by specialized psychotherapists in primary care centres have not been previously reported. A short‐term dynamic group psychotherapy, with a total of 37 to 39 sessions (75 min weekly) was adequate to the needs of our public health care services and seems to be sufficient to improve symptoms notably. In a recent study, short‐ and long‐term therapy seemed equally effective for typical outpatients seeking group psychotherapy (Lorentzen et al., 2013).
The present study shows that implementation of short‐term dynamic group psychotherapy run by experienced psychotherapists for patients with depressive symptoms attended in routine primary care centres is feasible and effective, with marked improvement in symptoms of depression and anxiety, as well as in quality of life. These findings, however, still need corroborating through other research with a larger number of patients in the Spanish population as well as in other patients attended in the primary health care systems of other countries. Assessment of the variability among therapists to distinguish results related to the therapists and results related to the method is also a suggestive research line. Based on the recordings, a qualitative study is currently being conducted, the preliminary results of which indicate improvements in the patients' capacity to symbolize and use of metaphors. Also the items of Blagys and Hilsenroth (2000) that appeared more frequently in our analysis are items (5) a focus on a patients' interpersonal experiences and (7) an exploration of patients' wishes, dreams or fantasies.
Conflicts of Interest
None.
Funding
None.
Acknowledgement
The authors thank Sergi Mojal for statistical analysis and Marta Pulido, MD, for editing the manuscript and editorial assistance.
Bros, I. , Notó, P. , and Bulbena, A. (2017) Effectiveness of Short‐Term Dynamic Group Psychotherapy in Primary Care for Patients with Depressive Symptoms. Clin. Psychol. Psychother., 24: 826–834. doi: 10.1002/cpp.2029.
References
- American Psychiatric Association (2000a). Practice guideline for the treatment of patients with major depressive disorder. American Journal of Psychiatry, 157(4 Suppl), 1–45. [PubMed] [Google Scholar]
- American Psychiatric Association (2000b). Diagnostic and statistical manual of mental disorders (4th edition Text Revision ed.) D.C.: Washington. [Google Scholar]
- Aragonès, E. , Piñol, J. L. , Caballero, A. , López‐Cortacans, G. , Casaus, P. , Hernández, J. M. , Badia, W. , & Folch, S. (2012). Effectiveness of a multi‐component programme for managing depression in primary care: A cluster randomized trial. The INDI project. Journal of Affective Disorders, 142, 297–305. DOI:10.1016/j.jad.2012.05.020. [DOI] [PubMed] [Google Scholar]
- Bion, W. R. (1961). Experiences in groups. London: Tavistock Institute Ed. [Google Scholar]
- Blackmore, C. , Beecroft, C. , Parry, G. , Booth, A. , Tantam, D. , Chambers, E. , Simpson, E. , Roberts, E. , & Saxon, D. (2009). A systematic review of the efficacy and clinical effectiveness of group analysis and analytic/dynamic group psychotherapy. Centre for Psychological Services Research, School of Health and Related Research, University of Sheffield, UK.
- Blackmore, C. , Tantam, D. , Parry, G. , & Chambers, E. (2012). Report on a systematic review of the efficacy and clinical effectiveness of group analysis and analytic/dynamic group psychotherapy. Group Analysis. The International Journal of Group‐Analytic Psychotherapy, 45, 49–69. DOI:10.1177/0533316411424356. [Google Scholar]
- Blagys, M. D. , & Hilsenroth, M. J. (2000). Distinctive features of short‐term psychodynamic‐interpersonal psychotherapy: A review of the comparative psychotherapy process literature. Clinical Psychology: Science and Practice, 7, 167–188. [Google Scholar]
- Bros Cugat, I. , & Jara Martin, M. (2015). Screening tests of depression. Some reflections. Atencion Primaria, pii: S0212‐6567(15)00003‐7. DOI:10.1016/j.aprim.2014.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canete, M. , Stormont, F. , & Esquerro, A. (2000). Group analytic psychotherapy with the elderly. British Journal of Psychotherapy, 17, 94–105. DOI:10.1111/j.1752-0118.2000.tb00563.x. [Google Scholar]
- Crits‐Christoph, P. (1992). The efficacy of brief dynamic psychotherapy: A meta‐analysis. American Journal of Psychiatry, 149, 151–158. [DOI] [PubMed] [Google Scholar]
- Driessen, E. , Cuijpers, P. , de Maat, S. C. , Abbass, A. A. , de Jonghe, F. , & Dekker, J. J. (2010). The efficacy of short‐term psychodynamic psychotherapy for depression: A meta‐analysis. Clinical Psychology Review, 30, 25–26. DOI:10.1016/j.cpr.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Ferrari, A. J. , Charlson, F. J. , Norman, R. E. , Patten, S. B. , Freedman, G. , Murray, C. J. , Vos, T. , & Whiteford, H. A. (2013). Burden of depressive disorders by country, sex, age, and year: Findings from the global burden disease study 2010. PLoS Medicine, 10, e1001547 DOI:10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland, A. F. , Huriburt, M. S. , Brookman‐Frazze, L. , Taylor, R. M. , & Accurso, E. C. (2010). Methodological challenges of characterizing usual care psychotherapeutic practice. Administration and Policy in Mental Health, 37, 208–220. DOI:10.1007/s10488-009-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons, M. B. , Thompson, S. M. , Scott, K. , Schauble, L. A. , Mooney, T. , Thompson, D. , … (2012). Supportive–expressive dynamic psychotherapy in the community mental health system: A pilot effectiveness trial for the treatment of depression. Psychotherapy (Chicago, Ill.), 49, 303–316. DOI:10.1037/a0027694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustavsson, A. , Svensson, M. , Jacobi, F. , Allgulander, C. , Alonso, J. , Beghi, E. , et al. (2011). Cost of disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21, 718–779. [DOI] [PubMed] [Google Scholar]
- Lampe, L. (2012). Diagnostic processes in mental health: GPs and psychiatrists reading from the same book but on a different page. Australasian Psychiatry, 20, 3674–378. [DOI] [PubMed] [Google Scholar]
- Lesage, A. (2015). Better treatment for depression. Canadian Medical Association Journal, 187, 438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobo, A. , Chamorro, L. , Luque, A. , Dal‐Ré, R. , Badia, X. , & Baró, E. (2002). Validation of the Spanish versions of the Montgomery–Asberg Depression and Hamilton Anxiety rating scales. Medicina Clínica, 118, 493–499. [DOI] [PubMed] [Google Scholar]
- Lorentzen, S. , & Ruud, T. (2014). Group therapy in public mental health services: Approaches, patients and group therapists. Journal of Psychiatric and Mental Health Nursing, 21, 219–225. [DOI] [PubMed] [Google Scholar]
- Lorentzen, S. , Ruud, T. , Fjeldstad, A. , & Høglend, P. (2013). Comparison of short‐ and long‐term dynamic group psychotherapy: Randomised clinical trial. British Journal of Psychiatry, 203, 280–287. DOI:10.1192/bjp.bp.112.113688. [DOI] [PubMed] [Google Scholar]
- Manning, J. S. , & Jackson, W. C. (2015). Providing guideline‐concordant assessment and monitoring for major depression in primary care. Journal of Clinical Psychiatry, 76, e3 DOI:10.4088/JCP.13013tx7c. [DOI] [PubMed] [Google Scholar]
- Mathers, C. D. , & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine, 3, e442 DOI:10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, S. , Dell'Osso, B. , & Ketter, T. A. (2014). The prevalence and burden of bipolar depression. Journal of Affective Disorders, 169(Suppl 1), S3–S11. DOI:10.1016/S0165-0327(14)70003-5. [DOI] [PubMed] [Google Scholar]
- Minović, S. M. , Erjavec, K. , Polijičanin, T. , Vrabec, B. , & Brečić, P. (2015). Prevalence of depressive symptoms associated sociodemographic factors in primary health care patients. Psychiatria Danubina, 27, 31–37. [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) , (2010). Depression: The treatment and management of depression in adults. Retrieved April 13, 2015, From http://www.nice.org.uk/guidance/cg90/chapter/1‐recommendations
- O'Connor, E. A. , Whitlock, E. P. , Beil, T. L. , & Gaynes, B. N. (2009). Screening for depression in adult patients in primary care settings: A systematic evidence review. Annals of Internal Medicine, 151, 793–803. DOI:10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
- Pence, B. W. , O'Donnell, J. K. , & Gaynes, B. N. (2012). The depression treatment cascade in primary care: A public health perspective. Current Psychiatry Reports, 14, 328–335. DOI:10.1007/s11920-012-0274-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper, W. E. , McCallum, M. , Joyce, A. S. , Rosie, J. S. , & Ogrodniczuk, J. S. (2001). Patient personality and time‐limited group psychotherapy for complicated grief. International Journal of Group Psychotherapy, 51, 525–552. [DOI] [PubMed] [Google Scholar]
- Ramos‐Brieva, J. C. , & Cordero, A. (1986). Validación de la versión castellana de la escala de Hamilton para la depresión. Actas Luso‐Españolas de Neurología y Psiquiatría, 118, 324–334. [PubMed] [Google Scholar]
- Ruiz, A. , Silva, H. , & Miranda, E. (2001). Clinical and psychometric diagnosis of depression in patients in general medicine. Revista Médica de Chile, 129, 627–633. [PubMed] [Google Scholar]
- Serrano‐Blanco, A. , Palao, D. J. , Luciano, J. V. , Pinto‐Meza, A. , Luján, L. , Fernández, A. , … (2010). Prevalence of mental disorders in primary care: results from the diagnosis and treatment of mental disorders in primary care study (DASMAP). Social Psychiatry and Psychiatric Epidemiology, 45, 201–210. DOI:10.1007/s00127-009-0056-y. [DOI] [PubMed] [Google Scholar]
- Schmidt, S. , Vilagut, G. , Garin, O. , Cunillera, O. , Tresserras, R. , Brugulat, P. , … (2012). Reference guidelines for the 12‐Item Short‐Form Health Survey version 2 based on the Catalan general population. Medicina Clínica, 139, 613–625. DOI:10.1016/j.medcli.2011.10.024. [DOI] [PubMed] [Google Scholar]
- Shedler, J. (2010). The efficacy of psychodynamic psychotherapy. American Psychologist, 65, 98–109. [DOI] [PubMed] [Google Scholar]
- Sobocki, P. , Jönsson, B. , Angst, J. , & Rehnberg, C. (2006). Cost of depression in Europe. Journal of Mental Health and Policy Economics, 8, 87–98. [PubMed] [Google Scholar]
- Thombs, B. D. , & Ziegelstein, R. C. (2013). Depression screening in primary care: Why the Canadian task force on preventive health care did the right thing. Canadian Journal of Psychiatry, 58, 692–696. [DOI] [PubMed] [Google Scholar]
- Thombs, B. D. , Ziegelstein, R. C. , Roseman, M. , Kloda, L. A. , & Ioannidis, J. P. (2014). There are no randomized controlled trials that support the United States Preventive Services Task Force Guideline on screening for depression in primary care: A systematic review. BMC Medicine, 12, 13 DOI:10.1186/1741-7015-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timonen, M. , & Liukkonen, T. (2008). Management of depression in adults. British Medical Journal, 336, 435–439. DOI:10.1136/bmj.39478.609097.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unützer, J. , & Park, M. (2012). Strategies to improve the management of depression in primary care. Primary Care, 39, 415–431. DOI:10.1016/j.pop.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Depression . Retrieved, April 13, 2015, From http://www.who.int/mediacentre/factsheets/fs369/en/
- Yalom, I. D. (2005). The theory and practice of group psychotherapy (5th ed.) New York: Basic Books. [Google Scholar]
- Zung, W. W. , Broadhead, W. E. , & Roth, M. E. (1993). Prevalence of depressive symptoms in primary care. Journal of Family Practice, 37, 337–344. [PubMed] [Google Scholar]


