Abstract
The article describes the medical approach of a frequent pathology, chronic venous insufficiency.
Chronic venous insufficiency requires early diagnosis as well as an evaluation of the associated risk factors; also, patients need to understand the disease and its treatment, and to become compliant with all their physician’s recommendations. Importantly, the physician should correctly evaluate the disease and decide the best option for the patient.
These days, it is crucial that the patient benefits from optimal treatment choice in order to prevent complications.
CVI is a potentially severe pathology that has been underdiagnosed and undertreated for a long time and requires patience from the patient as well as care from the physician.
BACKGROUND
Chronic venous insufficiency (CVI) is a common but underdiagnosed cause of leg pain and swelling, and it is frequently associated with varicose veins. It is a consequence of the dysfunction of the valve of the veins, associated with an impaired circulation of blood in the leg veins (1). Valve failure may occur due to a weakening of the valves as a result of varicose veins, or damage to the deep veins secondary to venous thrombosis, trauma or venous obstruction. The failure of the valves allows the blood to flow back down (reflux) into the section of vein below. This prevents the reduction in venous pressure that normally occurs during exercise, resulting in venous hypertension. In addition, poor function or failure of the calf muscle pump due to inactivity, immobility or abnormal gait may contribute to venous hypertension. Chronic venous hypertension causes abnormalities in the capillaries within the leg tissues that make them more permeable. This allows fluid, proteins and blood cells leak into the tissues. Venous hypertension may also be associated with an increased inflammatory response, changes in the structure of the microvasculature and reduced skin and tissue oxygenation (2). It has been postulated that valvular dysfunction causing reflux was the initial pathological change in CVD. The existing evidence seems to favour pre-existing weakness in the wall, which produces dilation and causes secondary valvular incompetence (3). Overall, these effects cause changes in the skin and subcutaneous tissues such as oedema, hyperpigmentation, lipodermatosclerosis, atrophe blanche and varicose eczema, and contribute to a greater skin fragility, increasing the risk of leg ulceration and delayed healing (2).
Risk factors for CVI
Family history
Increasing age over 30
One or more blood clots in superficial or deep veins
Female gender; varicose veins occur nearly as commonly in men
Prolonged standing
Heavy lifting
Multiple pregnancies
Limited physical activity
High blood pressure
Obesity
Diagnosis of CVI
Clinical examination is the first step for diagnosing CVI. The accuracy of the diagnosis can be increased by using a hand-held instrument called Doppler that allows the examiner to listen to the blood flow. The most accurate exam is a venous duplex ultrasound scan, that provides an accurate image of the vein, so that any blockage caused by blood clots or improper vein valve function can be detected. To exclude other causes of leg swelling, an MRI or CAT scan can be used (1).
Treatment of CVI
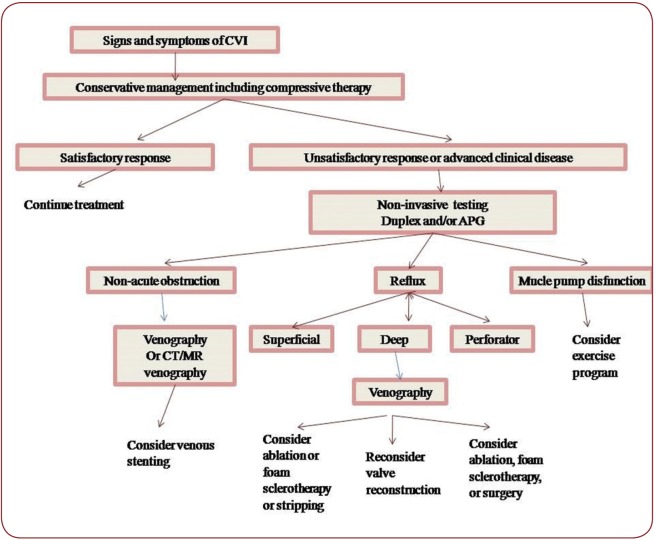
The treatment of CVI consists of both medical and surgical approaches and involves additional conservative therapeutic methods, as illustrated in Figure 1:
diet and lifestyle
avoidance of prolonged standing or sitting
structured exercise such as walking or strengthen calf muscles may improve calf muscle function
elevation of the feet above the tights when sitting and above the heart when lying down, three to four times a day, to reduce swelling (1)
compression stocking use – a very important part of the conservative treatment in CVI; stockings are non-invasive, safe and can be sufficient in treating uncomplicated venous disease
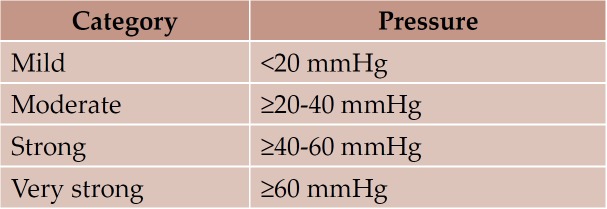
Compression therapy systems applied externally to the lower leg increase pressure of the skin and underlying structures to counteract the force of gravity. This can help to relieve the symptoms in the lower limb by acting to the venous and lymphatic systems to improve removal of fluid (blood and lymph) from the limb (2).
Compression therapy has two mechanisms of action: a static effect or resting pressure and a dynamic effect due to the changing circumference of the leg during walking. Applying external pressure will increase pressure in the limb; this will be distributed evenly, according to Pascal’s law. The greater the pressure increase in the lower limb, he greater the force that pushes the fluid out of the limb (2).
Bandages with a high SSI – static stiffness index – (inelastic) are able to remain rigid due to their lack of extensibility. This allows them to generate intermittent high working pressures and low resting pressures, improving both comfort and effectiveness of calf muscle pump (2).
Bandages with a low SSI provide constant pressure, maintaining a therapeutic level of compression a rest, but with less marked changes in pressure during exercise (2).
Compressive stockings are a required treatment component during travel in patients who require surgical interventions and in those with advanced CVI (>C4 disease). In patients with resolution of symptoms under compliant compressive stocking use, surveillance at every 6 months is recommended. If the patient develops breakthrough symptoms or if physical examination findings deteriorate, the patient must be counselled for intervention (4).
Pharmaceutical treatment
Sulodexide is an agent with polypharmacological actions which targets several sites involved in the pathogenesis of CVD. The chemical composition of sulodexide consists of 80% fast-moving heparine and 20% dermatan sulphate (5). The pharmacological effects of sulodexide differ substantially from other glycosaminoglycans and are mainly characterized by a prolonged halflife, profibrinolytic properties and reduced effects on both the coagulation cascade and bleeding parameters. The dual thrombin inhibitory action via both antithrombin and heparin cofactor II gives sulodexide its potent antithrombotic effect with a low hemorrhagic profile (5).
Sulodexide has endothelial protective effects by inducing the over expression of growth factors that are important in the protection and repair of several organs. It is capable of maintaining and restoring the endothelial glycocalix structures. Several studies have also demonstrated the anti-inflammatory properties of sulodexide (5). Studies on drug interactions with sulodexide have shown that its oral administration in cardiovascular disease, metabolic disorders and in prevention and treatment of thrombosis does not interfere with the pharmacological interactions of other routinely used agents (5).
The efficacy of sulodexide has been shown in several clinical trials in patients with peripheral vascular disease, peripheral arterial occlusive disease, coronary disease, cerebral vascular ischemia, myocardial infarction, post-thrombotic syndrome, intermittent claudication and vascular complications of diabetics (5).
Surgical treatment
It is reserved for patients whose symptoms remain uncontrolled or worsen despite initial conservative treatment, and may consist of ligation with stripping, simple ligation and division, sclerotherapy, stab evulsion, radiofrequency ablation, endovenous laser therapy.
FIGURE 1.
FIGURE 1. Algorhythm for diagnosing and treating CVI (6)
TABLE 1.
TABLE 1. Categorisation of compression bandage systems (2)
CONCLUSION
These days, it is very important that the patient benefits from optimal choice of treatment in order to prevent complications. CVI is a potentially severe pathology that has been underdiagnosed and treated for a long time and that requires patience from the patient and care from the physician.
Conflict of interests: none declared.
Financial support: none declared.
Contributor Information
Marilena SPIRIDON, Department of Cardiology, “St. Spiridon” Clinical Emergency Hospital, Iasi, Romania.
Dana CORDUNEANU, Department of Internal Medicine, “St. Spiridon” Clinical Emergency Hospital, Iasi, Romania.
REFERENCES
- - What is Chronic Venous Insuffi ciency (CVI)? Vascular Disease Foundation. h! p://vasculardisease.org/fl yers/ chronic-venous-insuffi ciency-fl yer.pdf. . ; [Google Scholar]
- - Principles of compression in venous disease: a practitioner’s guide to treatment and prevention of venous leg ulcers. Wounds International. . 2013; [Google Scholar]
- Perrin M, Ramelet AA. - Pharmacological Treatment of Primary Chronic Venous Disease: Rationale, Results and Unanswered Question. Eur J Vasc Surg. 2011;41:117–125. doi: 10.1016/j.ejvs.2010.09.025. [DOI] [PubMed] [Google Scholar]
- Jennifer Heller. - Treatment of Chronic Venous Insufficiency. Supplement of Endovascular Today. 2011; :12–15. [Google Scholar]
- Hoppenstead DA, Fareed J. - Pharmacological profi le of sulodexide. International Angiology. 2014;33:229–235. [PubMed] [Google Scholar]
- - http://circ.ahajournals.org/content/130/4/333. . ; [Google Scholar]