Abstract
Thyroid associated ophthalmopathy is a constellation of symptoms caused by an autoimmune process involving the orbital tissue. It is common in hyperthyroid patients due to Graves’ disease and also reported in euthyroid and hypothyroid Graves’ patients with positive thyroid receptor antibodies. But in Hashimoto’s thyroiditis, thyroid associated ophthalmopathy is a rarely reported and poorly understood entity. Here we report thyroid associated ophthalmopathy in a patient with hypothyroidism and negative thyroid receptor antibodies who showed heterogeneously hypoechoic thyroid gland on ultrasonography, diffuse lymphocytic infiltrate on fine needle aspiration citology and reduced 99m Tc radioisotope uptake, supporting the diagnosis of Hashimoto’s thyroiditis. The patient was treated with levothyroxine and artificial tear drops.
Keywords:Hashimoto’s thyroiditis, thyroid associated ophthalmopathy, Graves’ disease
INTRODUCTION
Thyroid associated ophthalmopathy (TAO) is a constellation of symptoms caused by an autoimmune process involving the orbital tissue. Ocular lesions in autoimmune thyroid diseases occur five times more often in women than in men (16 and 2.9 cases per 100000 annually, respectively) (1). It generally occurs in hyperthyroid patients due to Graves’ disease and sometimes also in euthyroid and hypothyroid patients (2). Most euthyroid and hypothyroid patients with TAO are thyroid receptor antibody (TRAb) positive, and they are diagnosed as having euthyroid Graves’ disease or hypothyroid Graves’ disease. But TAO in Hashimoto’s thyroiditis is a rare entity with very few cases reported until now. Pathogenesis of TAO in Hashimoto’s thyroiditis is poorly understood, as TRAb hypothesis cannot explain it due to the usual negative TRAb status in these patients. Here we report a case of TAO in a patient of Hashimoto thyroiditis.
CASE REPORT
A 63-year-old non-smoker, non-alcoholic male came to our hospital with complaint of fatigue. On general physical examination mild pallor was present. No icterus, cyanosis, clubbing or lymphadenopathy was noted. His blood pressure and pulse rate were 116/78 mm Hg and 68/min, respectively. Ophthalmological examination showed bilateral proptosis, swelling of the eyelids, conjunctival injection (Figure 1) and mild adduction deficiency. The degree of exophthalmos on the Hertel exophtalmometer was 24 mm for the left eye and 20 mm for the right eye. Intraocular pressure was normal in both eyes. Ten point clinical activity score (CAS) was 2 (one point each for swelling of eyelids and conjunctival injection) and NOSPECS class 3 was found. Laboratory data revealed the presence of overt hypothyroidism with a thyrotropin (TSH) level of 35.4 ìIU/mL (normal range 0.35-4.94 by chemiluminescent immunoassay), free 3,5,3’-triiodothyronine (FT3) of 0.23 pg/mL (normal range 1.71-3.71 by chemiluminescent immunoassay) and free thyroxine (FT4) of 0.45 ng/dL (normal range 0.8-1.7 by chemiluminescent immunoassay). TRAb was 1.07 IU/L (normal value <1.75 IU/L; by electrochemiluminescence immunoassay), anti-thyroid peroxidase antibody (Anti TPO) titre was 591.8 IU/mL (normal range 0.08-8.0 IU/mL by chemiluminescent immunoassay). Anti thyroglobulin antibody (ATG) was 871.3 IU/mL (normal value <65 IU/mL by chemiluminescent immunoassay). Ultrasonography (USG) of the thyroid showed heterogeneously hypoechoic thyroid gland without any nodule. The right lobe was 17x15x32 mm and the left lobe 14x16x26 mm in size. The 99mTc scan revealed 0.1% uptake at 20 minutes (normal range 0.3-3 %). Fine needle aspiration cytology (FNAC) showed diffuse lymphocytic infiltrate. Magnetic resonance imaging of orbits revealed mild bilateral proptosis with mild increase in bulk of bilateral inferior recti (maximum thickness 6.5 mm) with sparing of anterior part of tendons (Figure 2).
He was treated with levothyroxine replacement, artificial tear drops and ophthalmopathy responded considerably to the treatment. Glucocorticoid therapy was not given as the clinical activity score was 2.
DISCUSSION
Thyroid associated ophthalmopathy is common in patients with Graves’s disease and hyperthyroidism, and sometimes in those with euthyroid and hypothyroid Graves’ disease and positive TRAb (2). When euthyroid and hypothyroid patients with orbitopathy are TRAb negative, other diseases should be taken into consideration, including cavernous carotid fistula, sphenoid meningioma, orbital lymphoma, idiopathic orbital myositis and IgG4 related disease (3).
Although it was initially thought that Graves’ disease and Hashimoto’s thyroiditis are separate entities, at present they both are considered to be autoimmune diseases and represent the opposite sides of the same coin. A common factor causing both thyroid disease and ocular abnormalities has been searched for a long time. The TSH-receptor antigen is shared between the thyroid and the orbital tissues in Graves’ disease, thus explaining the extra thyroidal manifestation of the disease (4). Binding sites for both the TSH and the TSH receptor antibodies exist on the orbital cells. Orbital tissues also possess TSH receptor variants (5). Expression of the TSH receptor has been found to be increased in orbital preadipocytes (6). T cells reacting with TSH receptor and various cytokines that stimulate fibroblast proliferation has also been postulated as a possible mechanism of Graves’ ophthalmopathy. In Graves’ disease, TRAb is generally a stimulating type, though the blocking type has been also detected. Whether these blocking type TRAbs are a significant cause of hypothyroidism in hypothyroid Graves’ disease is unclear. In a study it was found that one third of patients with Graves’ disease who developed hypothyroidism after antithyroid medication had a blocking type TRAb (7). On the contrary, Kasagi et al examined five cases of hypothyroid Graves’ disease and detected stimulating, not blocking type TRAb in all patients (8). Hypothyroidism in these cases was not related to the presence of blocking type antibodies. They considered that hypothyroidism in these cases may be associated with high antibody titres against thyroglobin and destructive changes in the thyroid, which were demonstra ted by ultrasound and histological examination, sugges ting concomitant presence of Hashimoto’s thyroiditis.
Thyroid associated ophthalmopathy is rare in patients with Hashimoto’s thyroiditis, and only few cases have been reported (9-12). Pathogenesis of TAO in Hashimoto thyroiditis is poorly understood. Since patients with Hashimoto’s thyroiditis test negative for TRAb, the TRAb hypothesis does not explain the etiology of eye signs in Hashimoto’s thyroiditis. An alternative explanation for the ophthalmopathy in patients with Hashimot thyroiditis is the presence of specific antibodies against eye muscle antigens such as calsequestrin, flavoprotein or G2s (13). We did not test our patient for these antibodies due to financial constraints.
We have reported TAO in a patient with hypothyroidism and negative TRAb who showed heterogeneously hypoechoic thyroid gland on USG, diffuse lymphocytic infiltrate on FNAC and reduced 99m Tc radioisotope uptake, supporting the diagnosis of Hashimoto's thyroiditis. The patient was managed with levothyroxine and artificial tear drops. Glucocorticoids need to be considered if ten point clinical activity score (CAS) . 3. Given that in our patient CAS was 2, glucocorticoids were not used.
FIGURE 1.

FIGURE 1. Physical features of the patient: bilateral proptosis, eyelid swelling, conjunctival injection
FIGURE 2.
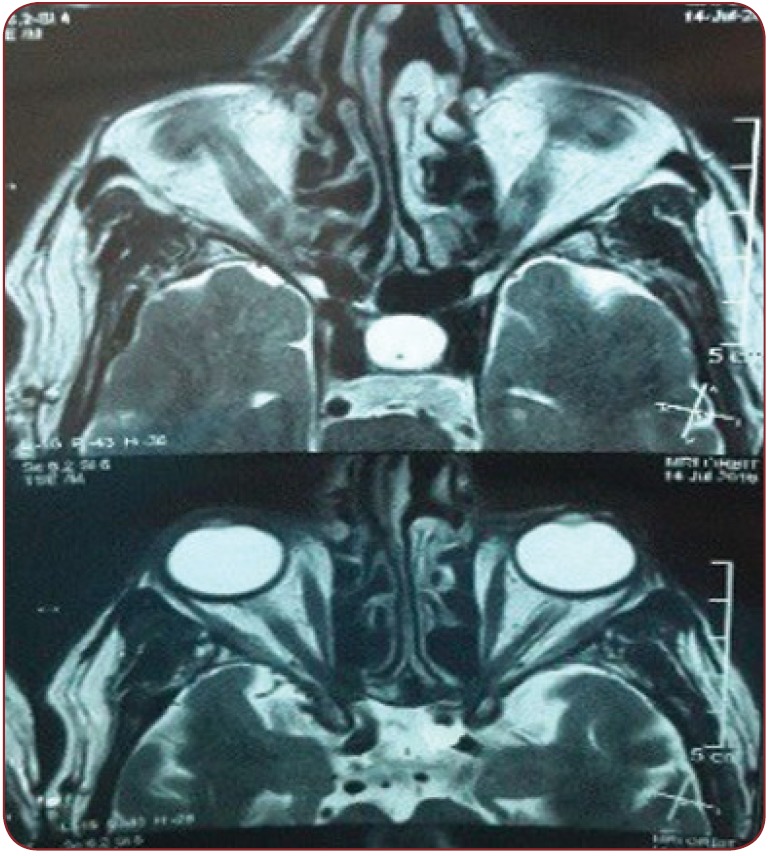
FIGURE 2. Magnetic resonance imaging of orbits: mild bilateral proptosis with mild increase in bulk of bilateral inferior recti with sparing of anterior part of tendons
CONCLUSION
Thyroid associated ophthalmopathy can sometimes occur in Hashimoto’s thyroiditis and awareness of this atypical form is important, because prompt recognition and treatment can prevent corneal involvement and blindness due to optic nerve compression.
Financial statement: none declared.
Authorship statement: All authors agreed the final version of the submitted manuscript.
Conflict of interests: none declared.
Patient consent obtained prior to the case report study.
Contributor Information
Deepak JAIN, Associate Professor, Department of Medicine, Pt.B.D.Sharma PGIMS, Rohtak, India.
Sudhir MOR, Resident, Department of Medicine, Pt.B.D.Sharma PGIMS, Rohtak, India.
Hari Krishan AGGARWAL, Senior Professor $ Head Department of Medicine IV, Pt.B.D.Sharma PGIMS, Rohtak, India.
Pulkit CHHABRA, Resident, Department of Medicine, Pt.B.D.Sharma PGIMS, Rohtak, India.
Promil JAIN, Assistant Professor, Department of Pathology, Pt.B.D.Sharma PGIMS, Rohtak, India.
REFERENCES
- Krassas GE, Wiersinga WM. - Thyroid eye disease: current concepts and the EUGOGO perspective. Thyroid International. 2005;4:3–4. [Google Scholar]
- Ponto KA, Binder H, Diana T, et al. - Prevalence, Phenotype, and Psychosocial Well-Being in Euthyroid/Hypothyroid Thyroid-Associated Orbitopathy. Thyroid. 2015;25:942–948. doi: 10.1089/thy.2015.0031. [DOI] [PubMed] [Google Scholar]
- Cheuk W, Chan JK. - IgG4-related Sclerosing Disease: A Critical Appraisal of an Evolving Clinicopathologic Entity. Adv Anat Pathol. 2010;17:303–332. doi: 10.1097/PAP.0b013e3181ee63ce. [DOI] [PubMed] [Google Scholar]
- Bartalena L, Wiersinga WM, Pinchera A. - Graves’ ophthalmopathy: state of the art and perspectives. J Endocrinol Invest. 2004;27:295–301. doi: 10.1007/BF03345280. [DOI] [PubMed] [Google Scholar]
- Paschke R, Metcalfe A, Alcalde L, et al. - Presence of nonfunctional thyrotropin receptor variant transcripts in retroocular and other tissues. J Clin Endocrinol Metab. 1994;79:1234–1238. doi: 10.1210/jcem.79.5.7962314. [DOI] [PubMed] [Google Scholar]
- Valyasevi RW, Erickson DZ, Harteneck DA, et al. - Differentiation of human orbital preadipocyte fibroblasts induces expression of functional thyrotropin receptor. J Clin Endocrinol Metab. 1999;84:2557–2562. doi: 10.1210/jcem.84.7.5838. [DOI] [PubMed] [Google Scholar]
- Tamai H, Kasagi K, Takaichi Y, et al. - Development of spontaneous hypothyroidism in patients with Graves’ disease treated with antithyroidal drugs: clinical, immunological, and histological fi ndings in 26 patients. J Clin Endocrinol Metab. 1989;69:49–53. doi: 10.1210/jcem-69-1-49. [DOI] [PubMed] [Google Scholar]
- Kasagi K, Hidaka A, Nakamura H, et al. - Thyrotropin receptor antibodies in hypothyroid Graves’ disease. J Clin Endocrinol Metab. 1993;76:504–508. doi: 10.1210/jcem.76.2.8094394. [DOI] [PubMed] [Google Scholar]
- Grzesiuk W, Szydlarska D, Pragacz A, Bar-Andziak E. - Thyroid-associated orbitopathy in patients with Hashimoto’s thyroiditis: a case report. Pol Arch Med Wewn. 2008;118:318–321. [PubMed] [Google Scholar]
- Tomer Y. - Unilateral ophthalmopathy in a patient with Hashimoto’s thyroiditis. Thyroid. 2000;10:99–100. doi: 10.1089/thy.2000.10.99. [DOI] [PubMed] [Google Scholar]
- Leo M, Menconi F, Rocchi R, et al. - Role of the underlying thyroid disease on the phenotype of Graves’ orbitopathy in a tertiary referral center. Thyroid. 2015;25:347–351. doi: 10.1089/thy.2014.0475. [DOI] [PubMed] [Google Scholar]
- Iyengar VS, Gosain V, Jagannatha K, Ramegowda RB. - Thyroid ophthalmopathy in asymptomatic Hashimoto’s thyroiditis with hypothyroidism–An unusual presentation. J Assoc Physicians India. 2016;64:101. [Google Scholar]
- Miller A, Arthurs B, Boucher A, et al. - Significance of antibodies reactive with a 64 kDa eye muscle mem-brane antigen in patients with thyroid autoimmunity. Thyroid. 1992;2:197–202. doi: 10.1089/thy.1992.2.197. [DOI] [PubMed] [Google Scholar]


