Abstract
As a negative regulatory molecule, T-cell immunoglobulin and mucin domain-3 (Tim-3) is closely associated with tumor immunological tolerance. The aim of this study was to investigate Tim-3 expression in invasive ductal breast cancer (IDC), its effect on clinicopathological parameters and its association with cytotoxic lymphocyte infiltration. Tim-3 protein expression was measured in 150 paraffin-embedded IDC specimens and 100 paired normal breast tissue specimens by immunohistochemistry. It was demonstrated that the infiltration of the tumor by CD8+ T cells was significantly higher compared with that of normal tissue, and the Tim-3 expression on CD8+ T cells was higher in IDC tissue compared with that in normal tissue; the differences were statistically significant (both P-values=0.000). The median expression level of Tim-3 on tumor cells was significantly associated with clinicopathological parameters such as age, axillary lymph node metastasis and TNM stage (P=0.015, 0.001 and 0.027, respectively). The expression of Tim-3 on CD8+ T cells was correlated with lymph node metastasis, World Health Organization (WHO) grade and molecular classification (P=0.000, 0.004 and 0.000, respectively). Additionally, the number of tumor-infiltrating CD8+ T cells was associated with primary tumor size, lymph node metastasis, WHO grade, Ki-67 and molecular classification (P=0.017, 0.002, 0.007, 0.003 and 0.000, respectively). Thus, Tim-3 may promote the development and progression of breast cancer and affect the tumor microenvironment; thus, it may be used as an independent prognostic factor for IDC patients.
Keywords: invasive ductal breast cancer, T-cell immunoglobulin and mucin domain-3, tumor-infiltrating cytotoxic lymphocyte, immune regulation, tumor invasion and metastasis, immunohistochemical
Introduction
Breast cancer is a major health concern worldwide and the most common type of cancer among women (1), with a reported 458,000 deaths annually, making it the most common cause of cancer-related mortality among women in developed as well as developing countries (2). Therefore, there is an urgent need for novel biomarkers for the prognosis and effective treatment of breast cancer. The T-cell immunoglobulin and mucin domain (TIM) gene family was positionally cloned in 2001 from within the T-cell and airway phenotype regulator locus as novel allergy and asthma susceptibility genes (3). The TIM gene family consists of eight members (TIM-1-8) on mouse chromosome 11B1.1, and three members (TIM-1, TIM-3 and TIM-4) on human chromosome 5q33.2, a chromosomal region that has been repeatedly associated with asthma, allergy and autoimmunity (4).
Tim-3 was found to be particularly expressed in T helper type 1 (Th1) cells, CD8+ T cells and Th17 cells. At present, Tim-3 expression may be found in innate immune cells, including natural killer (NK) cells, dendritic cells (DCs), monocytes, mast cells and other lymphocyte subpopulations (5–8).
In recent years, Tim-3 has been considered to be a negative regulatory molecule, which plays a crucial role in antitumor immunity. However, the mechanism underlying its antitumor properties remains unknown. The aim of this study was to investigate the expression of Tim-3 in 150 invasive ductal breast cancer (IDC) and 100 normal breast tissue samples by immunohistochemistry and determine the expression of Tim-3 in breast cancer tissue and its association with clinicopathological parameters and cytotoxic lymphocyte (CTL) infiltration.
Patients and methods
Patient selection
A total of 150 breast cancer tissue specimens were collected from female patients at the Department of Breast Surgery of the Southwest Medical University Affiliated Hospital (Sichuan, China) between April, 2013 and May, 2014; all the cases were pathologically diagnosed postoperatively. Following selection of the paraffin blocks, 4-µm sections were prepared, stained with hematoxylin and eosin (HE), and the diagnosis was confirmed by two pathologists. Sections with inflammation, hemorrhage and incisional biopsies with insufficient tissue were excluded from the study. Clinical information, including age, primary tumor size, axillary lymph node metastasis and TNM stage, World Health Organization (WHO) grade, Ki-67, molecular classification and location of the lesion, was extracted from patient files and recorded in tables. The median age of the patients was 49.6 years (range, 33–68 years). Patients without any complications did not receive chemotherapy or other therapies prior to surgery. Furthermore, 100 pathologically confirmed normal breast tissue or benign lesion samples were also obtained, located at a distance 3.0–5.0 cm from the tumor. All the participants provided written informed consent and the study protocol was approved by the Ethics Committee of the Affiliated Hospital of Xinan Medical University. The study was conducted over a period of 6 months.
Reagents and instruments
Rabbit anti-human Tim-3 polyclonal antibody (dilution, 1:500; catalog no., 185703; Abcam, Cambridge, UK); murine monoclonal anti-human CD8 antibody (dilution 1:500, GM710301, Gene Biology Company, Shanghai, China), 10% neutral buffered formalin, xylene, serial concentrations of ethanol, phosphate-buffered solution (PBS), 3% H2O2 and diaminobenzidine (DAB) (all from Jinshan Chemical Reagent Company, Chengdu, China).
Immunohistochemistry
To quantify Tim-3 cells in large numbers of patients, paraffin-embedded IDC samples were processed for immunohistochemistry. The specimens were fixed in 10% neutral buffered formalin, embedded in paraffin and cut into 4-µm serial sections. Paraffin-embedded tissues were dewaxed in xylene, rehydrated by serial concentrations of ethanol and rinsed in PBS, followed by treatment with 3% H2O2 to block endogenous peroxidase. Following heating in a microwave at 750 W for 15 min to retrieve the tissue antigen, the sections were incubated with 10% normal goat serum at room temperature for 10 min to block non-specific reactions. This was followed by washing with PBS and incubation with polyclonal rabbit anti-human Tim-3 antibody (dilution, 1:500, clone 185703, IgG2a; Abcam), murine monoclonal anti-human CD8 antibody, for 12 h at 4°C, and with horseradish peroxidase-conjugated goat anti-rat IgG (dilution, 1:500; GM710301; Gene Biology Company, Shanghai, China). Following washing with PBS, the sections were developed in DAB substrate. The sections were then counterstained with hematoxylin for 2 min and dehydrated in ethanol and xylene prior to mounting on slides. The sections were subjected to EnVision immunohistochemical staining. PBS instead of primary antibodies was used as negative control. Visualization was achieved with ABC-Elite Reagent (Sigma, St. Louis, MO, USA). The sections were counterstained with Mayer's hematoxylin (Sigma). The nuclei were stained with 1% ammonium hydroxide. The number of Tim-3 cells was counted in five fields at a magnification of ×400.
Statistical analysis
All the data were analyzed with the SPSS software package, version 17.0 (SPSS Inc., Chicago, IL, USA). Due to the non-normal distribution, the Mann-Whitney U-test was used for comparison between groups. Independent samples t-test was used for the comparison of two means; the Chi-squared test was used for rate comparison. P-values <0.05 were considered to indicate statistically significant differences.
Results
Expression of Tim-3 in the tissue of invasive breast carcinoma and normal breast tissue
Tim-3 was found to be expressed on the surface of the tumor cells (Fig. 1) and CD8+ T cells (Fig. 2). Tim-3 expression on IDC cells (98%) was significantly higher compared with that in normal breast tissue (13%; χ2=0.195, P=0.000). Similarly, the expression of Tim-3 on CD8+ T cells in IDC tissue (90%) was also significantly increased compared with that in normal breast tissue (23%; χ2=11.11, P=0.000; Table I).
Figure 1.
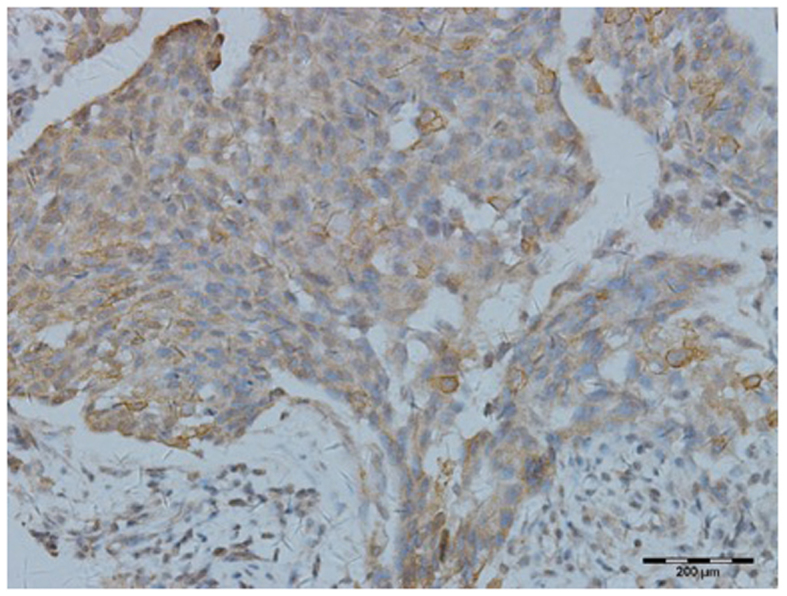
Photomicrograph showing high expression of Tim-3 on invasive ductal breast carcinoma cells (immunohistochemical staining; original magnification, ×400). Tim-3, T-cell immunoglobulin and mucin domain-3.
Figure 2.
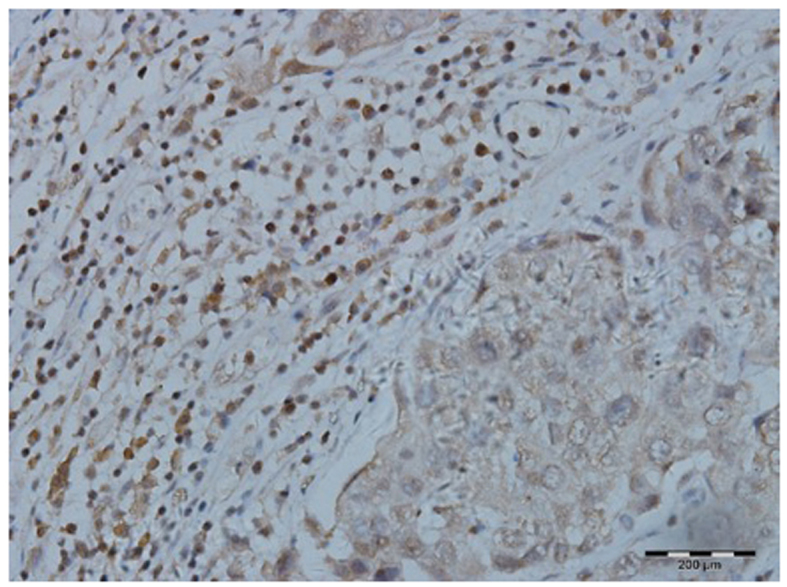
Photomicrograph of a section showing high expression of Tim-3 on the cytotoxic lymphocytes infiltrating invasive ductal breast carcinoma (immunohistochemical staining; original magnification, ×400). Tim-3, T-cell immunoglobulin and mucin domain-3.
Table I.
Expression of Tim-3 on breast tissue cells and on CTLs in IDC and normal breast or benign lesions.
| Expression of Tim-3 on breast tissue cells | Expression of Tim-3 on CTLs | ||||
|---|---|---|---|---|---|
| Variables | Patient no. | High (n) | Rate (%) | High (n) | Rate (%) |
| IDC | 150 | 147 | 98 | 135 | 90 |
| Normal breast/benign lesions | 100 | 13 | 13 | 23 | 23 |
| χ2 | 0.195 | 11.11 | |||
| P-value | 0.000 | 0.000 | |||
Tim-3, T-cell immunoglobulin and mucin domain-3; CTL, cytotoxic lymphocyte; IDC, invasive ductal carcinoma.
Association between Tim-3 expression and clinicopathological characteristics in IDC patients
The expression of Tim-3 on tumor cells was significantly associated with clinicopathological characteristics, such as gender, age, lymph node metastasis and TNM stage (P=0.015, 0.001 and 0.027, respectively). Our study indicated that the median expression level of Tim-3 on CD8+ T cells was significantly associated with clinicopathological parameters such as lymph node metastasis, TNM stage, WHO grade and molecular classification (P=0.000, 0.004, 0.009 and 0.000, respectively), whereas it was not correlated with other clinicopathological parameters (all P-values >0.05; Table II).
Table II.
Association between the expression of Tim-3 and the clinicopathological characteristics of patients with breastinfiltrating ductal carcinoma.
| Tim-3 expression | |||||||
|---|---|---|---|---|---|---|---|
| On tumor cells | On CTLs | ||||||
| Variables | Patient no. (n=150) | Low (%) | High (%) | P-value | Low (%) | High (%) | P-value |
| Age, years | 0.015 | 0.991 | |||||
| <45 | 48 | 27 (56.25) | 21 (43.75) | 24 (50.00) | 24 (50.00) | ||
| ≥45 | 102 | 36 (35.29) | 66 (64.71) | 52 (50.98) | 50 (49.02) | ||
| Tumor size | 0.422 | 0.114 | |||||
| T1 | 51 | 24 (47.06) | 27 (52.94) | 31 (60.78) | 20 (39.21) | ||
| T2 | 36 | 15 (41.67) | 21 (58.33) | 18 (50.00) | 18 (50.00) | ||
| T3 | 60 | 24 (40.00) | 36 (60.00) | 27 (45.00) | 33 (55.00) | ||
| T4 | 3 | 0 (0.00) | 3 (100.00) | 0 (0.00) | 3 (100.00) | ||
| Lymph node status | 0.001 | 0.000 | |||||
| N0 | 42 | 21 (50.00) | 21 (50.00) | 36 (85.71) | 6 (14.29) | ||
| N1 | 69 | 36 (52.17) | 33 (47.82) | 28 (40.58) | 41 (59.42) | ||
| N2 | 24 | 3 (12.50) | 21 (87.50) | 6 (25.00) | 18 (75.00) | ||
| N3 | 15 | 3 (20.00) | 12 (80.00) | 6 (40.00) | 9 (60.00) | ||
| TNM stage | 0.027 | 0.004 | |||||
| I | 18 | 12 (66.67) | 6 (33.33) | 10 (55.56) | 8 (44.44) | ||
| II | 42 | 21 (50.00) | 21 (50.00) | 30 (71.43) | 12 (28.57) | ||
| III | 60 | 18 (30.00) | 42 (70.00) | 27 (45.00) | 33 (55.00) | ||
| IV | 30 | 12 (40.00) | 18 (60.00) | 9 (30.00) | 21 (70.00) | ||
| WHO grade | 0.536 | 0.009 | |||||
| I | 15 | 6 (40.00) | 9 (50.00) | 3 (20.00) | 12 (80.00) | ||
| II | 99 | 39 (39.39) | 60 (60.61) | 49 (49.49) | 50 (50.51) | ||
| III | 36 | 18 (50.00) | 18 (50.00) | 24 (66.67) | 12 (33.33) | ||
| Ki-67, % | 0.630 | 0.512 | |||||
| <14 | 39 | 15 (38.46) | 24 (61.24) | 18 (46.15) | 21 (53.85) | ||
| ≥14 | 111 | 48 (43.24) | 63 (56.76) | 58 (52.25) | 53 (47.75) | ||
| Molecular classification | 0.314 | 0.000 | |||||
| Luminal A | 24 | 9 (37.50) | 15 (62.50) | 15 (62.50) | 9 (37.50) | ||
| Luminal B | 60 | 30 (50.00) | 30 (50.00) | 18 (30.00) | 42 (60.00) | ||
| HER2-overexpressing | 36 | 15 (41.67) | 21 (58.33) | 19 (52.78) | 17 (47.22) | ||
| Basal-like | 30 | 9 (30.00) | 21 (70.00) | 24 (80.00) | 6 (20.00) | ||
Tim-3, T-cell immunoglobulin and mucin domain-3; CTL, cytotoxic lymphocyte; TNM, tumor-node-metastasis; WHO, World Health Organization; HER2, human epidermal growth factor receptor 2.
Association between Tim-3 expression and the degree of CD+8 T-cell infiltration
The degree of CD8+ T-cell infiltration in IDC (Fig. 3) was higher compared with that in normal breast tissue (Fig. 4). Further analysis revealed that the degree of CD8+ T-cell infiltration was significantly correlated with primary tumor size, lymph node metastasis, WHO grade, Ki-67 and molecular classification (P=0.017, 0.002, 0.007, 0.003 and 0.000, respectively), whereas it was not correlated with other clinicopathological parameters (all P-values >0.05; Table III).
Figure 3.
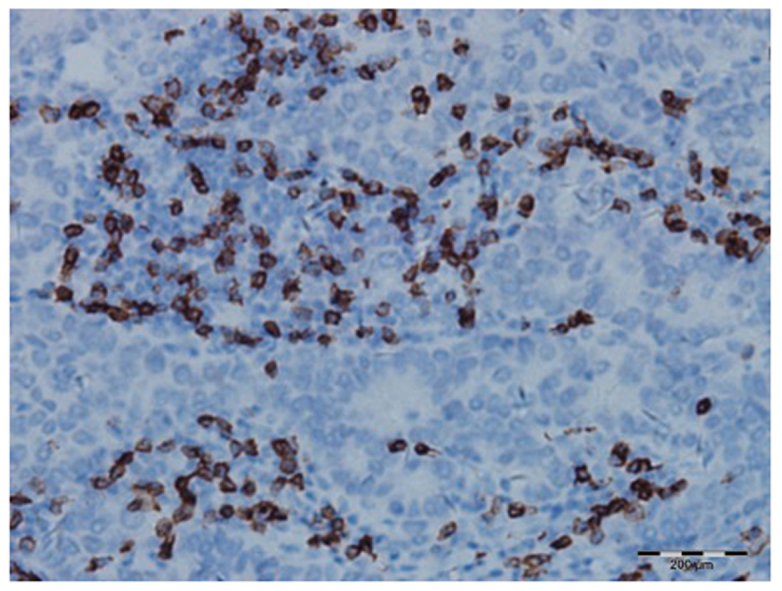
Photomicrograph of a section showing the extensive infiltration by CD8+ T-cells in invasive ductal breast carcinoma tissue (immunohistochemical staining; original magnification, ×200).
Figure 4.
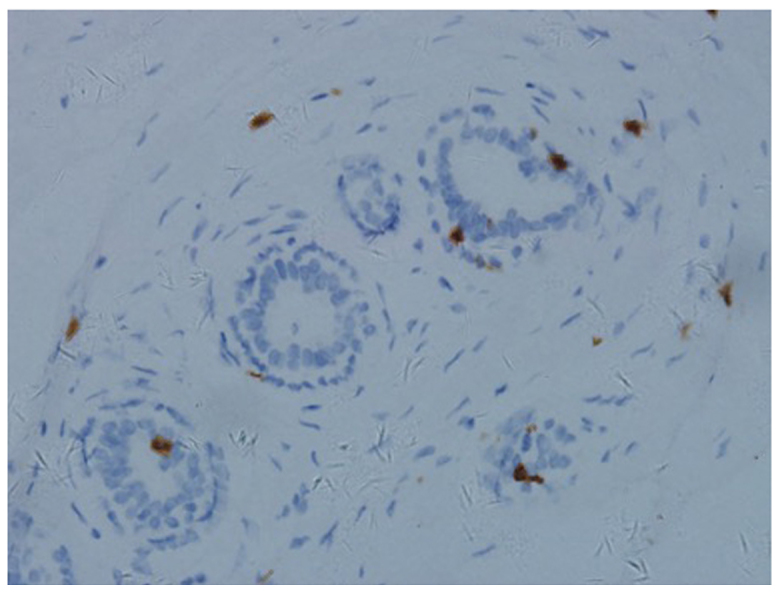
Photomicrograph of a section showing limited infiltration by CD8+ T-cells in normal breast tissue (immunohistochemical staining; original magnification, ×200).
Table III.
Association between expression of Tim-3 on CTLs and the clinicopathological parameters of breast infiltrating ductal carcinoma.
| Expression of Tim-3 on CTLs | |||||
|---|---|---|---|---|---|
| Variables | Patient no. (n=150) | Low (%) | High (%) | χ2 | P-value |
| Age, years | 3.160 | 0.075 | |||
| <45 | 48 | 18 (37.50) | 30 (62.50) | ||
| ≥45 | 102 | 24 (23.53) | 78 (76.47) | ||
| Tumor size | 10.177 | 0.017 | |||
| T1 | 51 | 15 (29.41) | 36 (70.59) | ||
| T2 | 36 | 6 (16.67) | 30 (83.33) | ||
| T3 | 60 | 18 (30.00) | 42 (70.00) | ||
| T4 | 3 | 3 (100.00) | 0 (0.00) | ||
| Lymph node status | 14.482 | 0.002 | |||
| N0 | 42 | 3 (7.14) | 39 (92.87) | ||
| N1 | 69 | 27 (39.13) | 42 (60.87) | ||
| N2 | 24 | 6 (25.00) | 18 (75.00) | ||
| N3 | 15 | 6 (40.00) | 9 (60.00) | ||
| TNM stage | 3.564 | 0.313 | |||
| I | 18 | 3 (16.67) | 15 (83.33) | ||
| II | 42 | 12 (28.57) | 30 (71.43) | ||
| III | 60 | 15 (25.00) | 45 (75.00) | ||
| IV | 30 | 12 (40.00) | 18 (60.00) | ||
| WHO grade | 9.939 | 0.007 | |||
| I | 15 | 9 (60.00) | 6 (40.00) | ||
| II | 99 | 27 (27.27) | 72 (72.72) | ||
| III | 36 | 6 (16.67) | 30 (83.33) | ||
| Ki-67 | 8.615 | 0.003 | |||
| <14% | 39 | 18 (46.15) | 21 (53.85) | ||
| ≥14% | 111 | 24 (21.62) | 87 (78.38) | ||
| Molecular classification | 23.636 | 0.000 | |||
| Luminal A | 24 | 9 (37.50) | 15 (62.50) | ||
| Luminal B | 60 | 27 (45.00) | 33 (55.00) | ||
| HER2-overexpressing | 36 | 6 (16.67) | 30 (83.33) | ||
| Basal-like | 30 | 0 (0.00) | 30 100.00) | ||
| Tim-3 expression on tumor | 0.946 | 0.331 | |||
| Low | 63 | 15 (23.80) | 48 (76.20) | ||
| High | 87 | 27 (31.03) | 60 (68.97) | ||
CTL, cytotoxic lymphocyte; TNM, tumor-node-metastasis; WHO, World Health Organization; HER2, human epidermal growth factor receptor 2; Tim-3, T-cell immunoglobulin and mucin domain-3.
Furthermore, by evaluating the abovementioned parameters that were statistically significant by logistic multifactor regression analysis, axillary lymph node metastasis, WHO grade, Ki-67 and molecular classification were found to significantly affect the extent of the tumor infiltration by CTLs (all P-values <0.05; Table IV).
Table IV.
Analysis of multiple factors affecting the infiltration degree by CTLs.
| Exp(B) CI 95% | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | B | SE | Wald | df | Sig | Exp(B) | Upper limit | Lower limit |
| Tumor size | −13.962 | 0.685 | 425.901 | 1 | 0.229 | 1.767 | 0.488 | 8.566 |
| Lymph node status | −4.649 | 1.387 | 11.236 | 1 | 0.001 | 0.010 | 0.046 | 1.345 |
| WHO grade | 0.576 | 1.137 | .257 | 1 | 0.002 | 1.779 | 0.023 | 0.665 |
| Ki-67 | 1.240 | 0.860 | 39.34 | 1 | 0.038 | 3.456 | 1.020 | 29.720 |
| Molecular classification | 16.910 | 985.39 | 0.000 | 1 | 0.000 | 2.200E9 | 7.140E8 | 4.791E10 |
| Tim-3 expression on tumor | −0.983 | 0.640 | 2.359 | 1 | 0.125 | 0.374 | 1.07 | 1.312 |
CTLs, cytotoxic lymphocytes; WHO, World Health Organization; SE, standard error; df, degree of freedom; CI, confidence interval.
Discussion
Co-opted immune checkpoint pathways are likely involved in the mechanism underlying tumor immune suppression. Tim-3 is a newly confirmed molecule with an important immunological function in several physiological and pathological processes.
Tim-3 was initially found to be selectively expressed on terminally differentiated interferon γ-producing CD4+ Th1 cells and CD8+ cytotoxic T cells (9,10), as well as on Th17 cells, DCs, monocytes, regulatory T cells (Tregs), mast cells, NK cells and tumor-infiltrating lymphocytes. It is also expressed on tumor cells, such as melanoma, squamous cell carcinoma, gastric cancer and non-small-cell lung cancer cells, but not on CD4+ Th2 cells (10–18).
Previous studies suggested that Tim-3 may modulate the immune response of Th1 cells and regulate cell immune tolerance (19,20). Tim-3 has also drawn significant attention in autoimmune diseases, anaphylactic diseases, immune tolerance and antitumor immunity (21,22). The Tim-3/galectin-9 pathway plays an important role in the suppressive tumor microenvironment (TME). In a variety of cancers, the overexpression of Tim-3 is associated with poor prognosis (9).
Tim-3 marks the most suppressed or dysfunctional population of CD8+ T cells in preclinical models of solid as well as hematological malignancies; thus, Tim-3 may be a key immune checkpoint in tumor-induced immune suppression (18,23).
The Tim-3/galectin-9 pathway contributes to the TME in the human body and Tim-3 is also characterized as a key regulator of the dysfunctional CD8+ T-cell phenotype (18,24) early in the TME, where neoplastic growth is promoted via induction of CD8+ T-cell dysfunctionality (25).
Several recent studies demonstrated that Tim-3 is highly expressed in a large number of tumor tissues types, including cervical cancer (15), gastric cancer (16), acute myeloid leukemia (23) lung cancer (25), ovarian cancer (26) and glioma (27). In this study, the Tim-3 expression on tumor cells and CD8+ T cells of IDC and normal breast tissues was investigated by immunohistochemistry. The expression of Tim-3 in IDC tissue was distinctly higher compared with that in normal breast tissue (P=0.000), which suggested that Tim-3 was involved in the pathogenesis of breast cancer via its regulatory effect on various immune cells and tumor cells, indicating that Tim-3 may play an important role in tumorigenesis. The expression of Tim-3 on tumor cells may affect the malignant biological behavior of the tumor.
In the present study, we observed that the expression of Tim-3 in IDC was significantly associated with age (P<0.05), reflecting the decrease in the overall immune ability of the body with advancing age. The expression of the negative regulatory immune molecule Tim-3 on breast cancer cells was clearly increased.
Our test results also demonstrated that the strength of the Tim-3 expression on tumor cells exhibited an increasing trend with the increasing number of metastatic axillary lymph nodes and advanced pathological stage. Furthermore, the expression of Tim-3 on IDC cells was significantly correlated with local axillary lymph node metastasis and pathological stage (P<0.05), but the results of our study demonstrated that primary tumor size, WHO grade, Ki-67 and molecular classification of breast IDC were not significantly associated with the expression of Tim-3 on tumor cells. The possible underlying mechanisms may be as follows: i) A large amount of Tim-3 on the tumor cell surface forms a ‘shield’ to protect Tim-3-positive tumor cells from the toxicity of immunological effector cells; however, the expression of negative immune regulatory factor Tim-3 does not affect the proliferation and differentiation of tumor cells. ii) In some cases, the size of the primary tumor is large at clinical diagnosis; thus, immune adjustment factors are no longer able to interfere with the growth of tumor cells, or there is a disproportional rate of tumor cell proliferation and immune clearance. iii) The experimental data may be insufficient; thus, larger samples are required to confirm the findings.
In nearly all previous studies, immune cells were identified by specific cluster of differentiation (CD) markers, following immunohistochemical staining of the slides. It is important to distinguish between different types of T lymphocytes, as they all have different functions in the TME.
CD8+ T cells play an important role in the TME. CTL is the main antitumor immune cell type, which may identify tumor antigens and eliminate tumor cells with one of two main mechanisms: i) The perforin pathway, or ii) the Fas/FasL-mediated apoptosis pathway. Fourcade et al (28) discovered that Tim-3 was expressed on NY-ESO-1-specific CD8+ T cells in patients with advanced melanoma. They found that the blockade of both the Tim-3 and programmed cell death protein-1 (PD-1) pathways may reverse tumor-induced T-cell exhaustion in patients with advanced melanoma. Our results suggested that the Tim-3 expression on CD8+ T cells was correlated with tumor invasion and TNM stage, which may be due to Tim-3-induced T-cell exhaustion, leading to tumor occurrence.
Our test data demonstrated that the expression of Tim-3 on tumor-infiltrating CTLs increased as axillary lymph node metastasis progressed. Lymph node metastasis and TNM stage, primary tumor size, WHO grade and molecular classification are significantly associated with the expression of Tim-3 on CTL cells (P<0.05).
This indicates that the expression of Tim-3 on CTLs may inhibit the tumor cell-killing function of CTLs. Even in the TME, CD8+ CTLs may transform into CD8+ Tregs, decreasing the tumor-infiltrating CTL immune surveillance, decreasing the local immune function and promoting the growth of tumor cells and metastasis.
The present study analyzed the association of tumor-infiltrating CTLs and the pathological characteristics of breast-infiltrating ductal carcinoma by single factor analysis of variance and demonstrated that primary tumor size, axillary lymph node metastasis, WHO grade, Ki-67 and molecular classification may statistically significantly affect the degree of tumor CTL infiltration (P<0.05).
Furthermore, the abovementioned statistically significant parameters were assessed by multiple logistic regression analysis and the results also demonstrated that axillary lymph node metastasis, WHO grade, Ki-67 and molecular classification significantly affect the extent of CTL infiltration of the tumor. The possible underlying mechanism may be as follows: i) High expression of the negative immunomodulatory molecule Tim-3 on tumor-infiltrating CTLs may result in immune malfunction; as the tumor grows, CD8+ CTLs may transform into CD8+ Tregs. ii) Low degree of CTL infiltration may lead to poor local immunity, which may contribute to tumor growth. iii) The lower the degree of tumor differentiation, the higher its antigenicity, which may cause a stronger local immune response.
In conclusion, Tim-3 is expressed in the majority of solid tumors and tumor-infiltrating CTLs. This finding suggests that Tim-3 participates in the immune escape through the following mechanisms: i) When it binds to its receptor, Tim-3 may induce T-cell apoptosis or immune incompetence; ii) a large amount of Tim-3 on the tumor cell surface may form a ‘shield’, which may protect Tim-3-positive tumor cells from toxic injury or elimination by CTLs; iii) Tim-3 positive cells may also affect T-cell secretion of negative cytokines or Treg coordination.
Sakuishi et al (18) reported that, in lymphocytes infiltrating solid tumors in mice, co-expression of Tim-3 and PD-1 may be detected. The multi-targeted therapy of Tim-3 and PD-1 has been highly effective in controlling tumor growth. Our study demonstrated that the expression of Tim-3 in breast cancer tissue was negatively correlated with certain clinicopathological parameters; however, the underlying mechanisms remain unclear. Therefore, further research on the multi-targeted therapy of Tim-3 and PD-1 for the treatment of breast cancer.
In conclusion, Tim-3 is highly expressed in breast IDC cells and tumo-infiltrating CTLs. The expression of Tim-3 exhibits a positive correlation with the malignant behavior of the tumor. The expression of Tim-3 on CTLs is negatively correlated with degree of CTL infiltration, and Tim-3 expression in breast cancer exerts a negative effect on immune regulation. The largest diameter of the primary tumor, the number of metastatic axillary lymph nodes, degree of tumor cell differentiation and molecular classification of breast cancer significantly afect the extent of the CTL infiltration of the tumor tissue.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Eccles SA, Aboagye EO, Ali S, Anderson AS, Armes J, Berditchevski F, Blaydes JP, Brennan K, Brown NJ, Bryant HE, et al. Critical research gaps and translational priorities for the successful prevention and treatment of breast cancer. Breast Cancer Res. 2013;15:R92. doi: 10.1186/bcr3493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McIntire JJ, Umetsu SE, Akbari O, Potter M, Kuchroo VK, Barsh GS, Freeman GJ, Umetsu DT, DeKruyff RH. Identification of Tapr (an airway hyperreactivity regulatory locus) and the linked Tim gene family. Nat Immunol. 2001;2:1109–1116. doi: 10.1038/ni739. [DOI] [PubMed] [Google Scholar]
- 4.McIntire JJ, Umetsu DT, DeKruyff RH. TIM-1, a novel allergy and asthma susceptibility gene. Springer Semin Immunopathol. 2004;25:335–348. doi: 10.1007/s00281-003-0141-3. [DOI] [PubMed] [Google Scholar]
- 5.Hastings WD, Anderson DE, Kassam N, Koguchi K, Greenfield EA, Kent SC, Zheng XX, Strom TB, Hafler DA, Kuchroo VK. TIM-3 is expressed on activated human CD4+ T cells and regulates Th1 and Th17 cytokines. Eur J Immunol. 2009;39:2492–2501. doi: 10.1002/eji.200939274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson AC, Anderson DE, Bregoli L, Hastings WD, Kassam N, Lei C, Chandwaskar R, Karman J, Su EW, Hirashima M, et al. Promotion of tissue inflammation by the immune receptor Tim-3 expressed on innate immune cells. Science. 2007;318:1141–1143. doi: 10.1126/science.1148536. [DOI] [PubMed] [Google Scholar]
- 7.Khademi M, Illés Z, Gielen AW, Marta M, Takazawa N, Baecher-Allan C, Brundin L, Hannerz J, Martin C, Harris RA, et al. T Cell Ig- and mucin-domain-containing molecule-3 (TIM-3) and TIM-1 molecules are differentially expressed on human Th1 and Th2 cells and in cerebrospinal fluid-derived mononuclear cells in multiple sclerosis. J Immunol. 2004;172:7169–7176. doi: 10.4049/jimmunol.172.11.7169. [DOI] [PubMed] [Google Scholar]
- 8.Nakae S, Iikura M, Suto H, Akiba H, Umetsu DT, Dekruyff RH, Saito H, Galli SJ. TIM-1 and TIM-3 enhancement of Th2 cytokine production by mast cells. Blood. 2007;110:2565–2568. doi: 10.1182/blood-2006-11-058800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson AC. Tim-3, a negative regulator of anti-tumor immunity. Curr Opin Immunol. 2012;24:213–216. doi: 10.1016/j.coi.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Anderson AC, Anderson DE, Bregoli L, Hastings WD, Kassam N, Lei C, Chandwaskar R, Karman J, Su EW, Hirashima M, et al. Promotion of tissue inflammation by the immune receptor Tim-3 expressed on innate immune cells. Science. 2007;318:1141–1143. doi: 10.1126/science.1148536. [DOI] [PubMed] [Google Scholar]
- 11.Ngiow SF, Teng MW, Smyth MJ. Prospects for TIM3-targeted antitumor immunotherapy. Cancer Res. 2011;71:6567–6571. doi: 10.1158/0008-5472.CAN-11-1487. [DOI] [PubMed] [Google Scholar]
- 12.Wiener Z, Kohalmi B, Pocza P, Jeager J, Tolgyesi G, Toth S, Gorbe E, Papp Z, Falus A. TIM-3 is expressed in melanoma cells and is upregulated in TGF-beta stimulated mast cells. J Invest Dermatol. 2007;127:906–914. doi: 10.1038/sj.jid.5700616. [DOI] [PubMed] [Google Scholar]
- 13.Zhuang X, Zhang X, Xia X, Zhang C, Liang X, Gao L, Zhang X, Ma C. Ectopic expression of TIM-3 in lung cancers: A potential independent prognostic factor for patients with NSCLC. Am J Clin Pathol. 2012;137:978–985. doi: 10.1309/AJCP9Q6OVLVSHTMY. [DOI] [PubMed] [Google Scholar]
- 14.Yan J, Zhang Y, Zhang JP, Liang J, Li L, Zheng L. Tim-3 expression defines regulatory T cells in human tumors. PLoS One. 2013;8:e58006. doi: 10.1371/journal.pone.0058006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao Y, Zhou X, Huang X, Li Q, Gao L, Jiang L, Huang M, Zhou J. Tim-3 expression in cervical cancer promotes tumor metastasis. PLoS One. 2013;8:e53834. doi: 10.1371/journal.pone.0053834. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Jiang J, Jin MS, Kong F, Cao D, Ma HX, Jia Z, Wang YP, Suo J, Cao X. Decreased galectin-9 and increased Tim-3 expression are related to poor prognosis in gastric cancer. PLoS One. 2013;8:e81799. doi: 10.1371/journal.pone.0081799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang ZZ, Grote DM, Ziesmer SC, Niki T, Hirashima M, Novak AJ, Witzig TE, Ansell SM. IL-12 upregulates TIM-3 expression and induces T cell exhaustion in patients with follicular B cell non-Hodgkin lymphoma. J Clin Invest. 2012;122:1271–1282. doi: 10.1172/JCI59806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med. 2010;207:2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sánchez-Fueyo A, Tian J, Picarella D, Domenig C, Zheng XX, Sabatos CA, Manlongat N, Bender O, Kamradt T, Kuchroo VK, et al. Tim-3 inhibits T helper type 1-mediated auto- and alloimmune responses and promotes immunological tolerance. Nat Immunol. 2003;4:1093–1101. doi: 10.1038/ni987. [DOI] [PubMed] [Google Scholar]
- 20.Sabatos CA, Chakravarti S, Cha E, Schubart A, Sánchez-Fueyo A, Zheng XX, Coyle AJ, Strom TB, Freeman GJ, Kuchroo VK. Interaction of Tim-3 and Tim-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat Immunol. 2003;4:1102–1110. doi: 10.1038/ni988. [DOI] [PubMed] [Google Scholar]
- 21.Simmons WJ, Koneru M, Mohindru M, Thomas R, Cutro S, Singh P, Dekruyff RH, Inghirami G, Coyle AJ, Kim BS, Ponzio NM. Tim-3+ T-bet+ tumor-specific Th1 cells colocalize with and inhibit development and growth of murine neoplasms. J Immunol. 2005;174:1405–1415. doi: 10.4049/jimmunol.174.3.1405. [DOI] [PubMed] [Google Scholar]
- 22.Hu WK, Lu XX, Yang S, Xu GP, Lan F, Chen SX, Ni W, Xiong WN, Xiong SD. Expression of the Th1-specific cell-surface protein Tim-3 increases in a murine model of atopic asthma. J Asthma. 2009;46:872–877. doi: 10.3109/02770900903199953. [DOI] [PubMed] [Google Scholar]
- 23.Zhou Q, Munger ME, Veenstra RG, Weigel BJ, Hirashima M, Munn DH, Murphy WJ, Azuma M, Anderson AC, Kuchroo VK, Blazar BR. Coexpression of Tim-3 and PD-1 identifies a CD8+ T-cell exhaustion phenotype in mice with disseminated acute myelogenous leukemia. Blood. 2011;117:4501–4510. doi: 10.1182/blood-2010-10-310425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takamura S, Tsuji-Kawahara S, Yagita H, Akiba H, Sakamoto M, Chikaishi T, Kato M, Miyazawa M. Premature terminal exhaustion of Friend virus-specific effector CD8+ T cells by rapid induction of multiple inhibitory receptors. J Immunol. 2010;184:4696–4707. doi: 10.4049/jimmunol.0903478. [DOI] [PubMed] [Google Scholar]
- 25.Gao X, Zhu Y, Li G, Huang H, Zhang G, Wang F, Sun J, Yang Q, Zhang X, Lu B. TIM-3 expression characterizes regulatory T cells in tumor tissues and is associated with lung cancer progression. PLoS One. 2012;7:e30676. doi: 10.1371/journal.pone.0030676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu J, Liu C, Qian S, Hou H. The expression of Tim-3 in peripheral blood of ovarian cancer. DNA Cell Biol. 2013;32:648–653. doi: 10.1089/dna.2013.2116. [DOI] [PubMed] [Google Scholar]
- 27.Han S, Feng S, Xu L, Shi W, Wang X, Wang H, Yu C, Dong T, Xu M, Liang G. Tim-3 on peripheral CD4+ and CD8+ T cells is involved in the development of glioma. DNA Cell Biol. 2014;33:245–250. doi: 10.1089/dna.2013.2306. [DOI] [PubMed] [Google Scholar]
- 28.Fourcade J, Sun Z, Benallaoua M, Guillaume P, Luescher IF, Sander C, Kirkwood JM, Kuchroo V, Zarour HM. Upregulation of Tim-3 and PD-1 expression is associated with tumor antigen-specific CD8+T cell dysfunction in melanoma patients. J Exp Med. 2010;207:2175–2186. doi: 10.1084/jem.20100637. [DOI] [PMC free article] [PubMed] [Google Scholar]


