Abstract
Objective
Patient experience is one of the three pillars of quality in healthcare; improving it must be a key aim if we are to make the overall quality of the healthcare we provide better.
Methods
We devised a quality improvement project to improve the patient experience of elective surgery. We conducted surveys of patients and assessed their experience by using semistructured interviews and patient questionnaires. We gathered data about their overall satisfaction, fasting times and their communication with staff. We used this information to inform strategies aimed at improving patient experience.
Results
Our initial results showed that patients who had their operations later in the day were significantly less likely to report a positive experience. We found the main reasons for this were long waiting times, poor communication and prolonged fasting. We implemented changes over ‘Plan, Do, Study, Act’ cycles, including (1) staggering patient arrival times, (2) introducing the concept of the 'Golden Patient', (3) having a single point of contact on the day surgery unit to communicate between theatre staff and patients, (4) using the WHO checklist to finalise list order, and (5) altering patient information letters to include the possibility of a wait on the day of surgery.
Conclusion
This project increased the percentage of patients reporting an ‘Excellent’ or ‘Good’ experience from 65% to 96%. In addition to improving our patients' experience, our project has also delivered shorter waiting times, better dissemination of information and fewer patients reporting hunger or thirst.
Keywords: Surgery, Anaesthesia, Patient Satisfaction, Patient-centred Care, Quality Improvement
Problem
Patient experience is one of the three pillars of quality in healthcare.1 2 If healthcare organisations are to improve the quality of care they provide; then efforts to improve their patients’ experience must be integral to any quality improvement plan.
Improved patient experience is not only linked to increased satisfaction; there is evidence that organisations which emphasise this have better outcomes in terms of patient safety and clinical effectiveness, the other two pillars of quality.3 Good patient experience is associated with a shorter length of stay, lower readmission rates and a lower cost per patient.4 5 ‘Ensuring that people have a positive experience of care’ is one of the five domains in the National Health Service (NHS) Outcomes Framework, which is a set of indicators that measure performance and is the primary mechanism of accountability in the NHS.6 It therefore follows that efforts made to provide a good patient experience are to the benefit of both the patient and the organisation.
Coming to hospital for elective surgery is undoubtedly a stressful time for many people. There is some evidence to show that patients with less anxiety before their surgery feel less pain postoperatively and their wounds may heal more quickly.7 8 When a poor service is provided, it costs more money and is linked to decreased staff satisfaction.9 One could argue that, as healthcare providers, it is our duty to strive to give our patients a good experience as part of our delivery of high quality care. In the paper, ‘High Quality Care for All,’ Lord Darzi states “Quality of care includes quality of caring. This means how personal care is—the compassion, dignity and respect with which patients are treated. It can only be improved by analysing and understanding patient satisfaction with their own experiences.” 10
If we are to improve the overall quality of the healthcare we provide, improving our patients’ experience must be one of our key aims; however, if we are to improve patient experience, we must first measure it. Previously, measurements of patient experience have not been considered as important as some other outcome indicators10 but, in a review of the subject, Manary et al state “the available evidence suggests that measures of patient experience are robust, distinctive indicators of health quality.”11
Background
The Royal Free London NHS Trust is a large, acute trust in North London. It comprises three hospitals: the Royal Free Hospital (RFH), a large teaching hospital which performs approximately 11 500 elective operations per year (personal communication from Mr S. Smith, 2016), and two district generals, Barnet Hospital and Chase Farm Hospital (CFH).
One of the Trust's governing objectives is ‘to provide excellent experience for our patients and staff’ and one of its annual objectives is ‘to be in the top 10% of all providers for patient satisfaction and experience.’12 13
Our project focused on the RFH and the CFH sites because this is where the majority of elective surgery is performed. While there was anecdotal evidence of good patient satisfaction with our service, there had not been any in-depth fact-finding about what our patients really thought about their care.
The process on the day of elective surgery had been tailored primarily for the convenience of the staff. At the RFH, patients were typically asked to arrive at the hospital at 07:30, irrespective of the time of their operation and it was common for them to have fasted longer than necessary,14 as is common in many hospitals.15
We developed a quality improvement (QI) project that would take an in-depth look at the experience of our patients and produce both quantitative and qualitative results. We then used QI methodology to institute changes designed to improve the experience of elective surgery for patients at the Royal Free Hospital.
Baseline measurement
In July 2015, we conducted a one-day survey of patients on the Day Surgery Unit (DSU) at the RFH.16 The patients surveyed were those scheduled to have general anaesthesia on an all-day theatre list which had at least two patients on it. We assessed the experience of those patients by using semistructured interviews and a patient questionnaire. Patients were asked questions about their overall satisfaction, fasting times and their communications with staff.
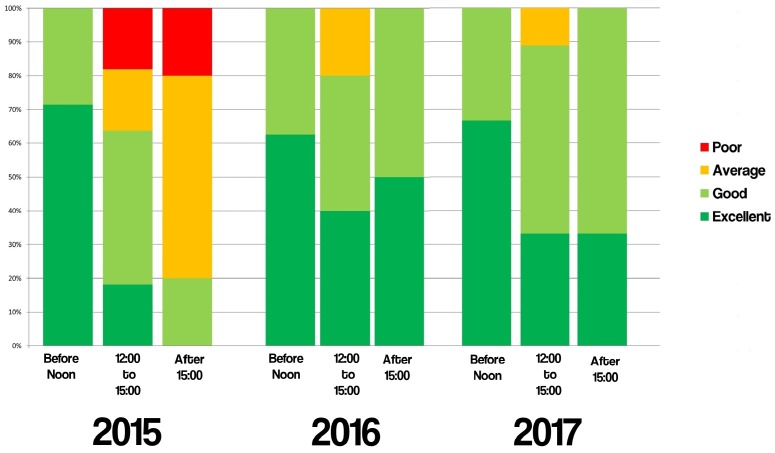
This baseline measurement found that 65% of our patients rated their experience as ‘Excellent’ or ‘Good.’ When results were analysed by time of day, we found that 71% of patients who had their surgery before 12:00 rated their experience as ‘Excellent.’ However, of those who had their surgery after 1500, 80% rated their experience as ‘Average’ or ‘Poor.’ People having their operations after 15:00 were significantly more likely to report an ‘Average’ or ‘Poor’ experience (p=0.01) (see figure 1).
Figure 1.
Satisfaction scores in 2015 by time of day.
Design
The baseline data collection showed that the processes on DSU worked well for some patients, but poorly for others. Those who had their surgery very soon after arriving in the hospital had a more positive experience.
We went to the DSUs at the RFH and CFH and spoke to the patients about their experiences. As with the baseline surveys, we spoke to those who were scheduled to have general anaesthesia on an all-day theatre list which had at least two patients on it. We asked them to complete a questionnaire that would elicit quantitative and qualitative information about their experience of the elective surgical process.
We also conducted audio or video interviews with those patients who consented to this.
This information gave us insight into the reasons behind our patients’ experiences and we used this to devise and develop potential ways to improve the service. We fed back the information about our patients’ experience, including the video interviews, to relevant stakeholders such as the Theatres Strategy Group, the Anaesthetic Department and the DSU nurses. We collaborated with these stakeholders to make changes.
We used a series of PDSA (Plan, Do, Study, Act) cycles to improve patient experience in a strategy that included all team members in a multidisciplinary approach. PDSA cycles were implemented over a matter of weeks or months.
Strategy
PDSA cycle 1: engaging the multidisciplinary team
We spoke to all the nurses on the DSU at the RFH site. We used a combination of written surveys and unstructured interviews, then analysed their comments and suggestions about how to improve the patients’ experience on their day of surgery. We then presented the findings of both the patient and staff surveys to the Theatre Strategy Group, the Head of Nursing and the Anaesthetic Department.
Working together, we agreed on the following actions.
Staggering patient arrival times
Several patients told us that the long wait before their operation was the biggest issue that negatively affected their experience. Patients were asked to arrive at 07:30 and some of them had to wait for more than eight hours on the DSU before their operation. We worked with the admissions staff to stagger arrival times so that patients who were to have their operations in the afternoon could arrive later in the day. List staggering was rolled out specialty-by-specialty over a period of months with the agreement of the surgical teams. By February 2017, the vast majority of surgical lists were staggered. The decision on how to stagger was left to the individual surgical teams. Some choose to have a simple morning/afternoon split (eg, morning patients arrive at 07:30 and afternoon patients arrive at 11:30), whereas others ask patients to arrive 3-hour time slots throughout the day.
The Golden Patient
We have introduced the concept of the ‘Golden Patient.’ This means that the first patient of the day is identified before the day of surgery by the theatre bookings team and then ratified by the consultant surgeon. This patient is asked to come to the hospital 15 min earlier than the others so that they can then be changed, prepared and sent for in a timely fashion, thereby minimising knock-on delays for the rest of the day.
Single point of contact on DSU
Another significant problem we identified was the difficulty in communicating between theatres and the DSU. The staff in theatres would call one of several phones on DSU and find it difficult to speak to the correct nurse. We introduced the idea of a single point of contact. The DSU charge nurse would carry a portable telephone and would take all calls from theatres and then disseminate information such as the order of the list and which patients could be given a drink.
Increasing the utility of the WHO checklist
Before the start of every operating list, the theatre team performs a ‘team brief’ as part of the WHO Safer Surgery Checklist.17 18 The team brief was used as an opportunity to finalise and ‘lock in’ the order of the patients on the list. This information, along with estimated start times, would be passed on to the DSU charge nurse. This meant that appropriate patients could drink something or leave DSU and return closer to their theatre time.
Our staff survey found that if there were was no phone call from theatres, some DSU nurses were unwilling to call and ask about theatre times. Following this, the senior DSU nurses provided some education to the DSU nurses to highlight the importance of knowing the list order and empower the DSU nurses to call theatres and request the list order and approximate theatre times. This enabled them to pass this information onto the patients and to give drinks as appropriate.
These actions represent major changes to the way patients are admitted and involved several people along the admissions chain. These changes took several months to implement.
PDSA cycle 2: managing expectations
In April 2016, we repeated the patient and staff interviews, using the same methodology and questionnaire as before (see online supplementary file 1). Our aim was to see if there was any improvement in our patients’ experience and to observe whether any of the previously identified problems had been resolved.
bmjoq-2017-000079supp001.docx (32.3KB, docx)
We analysed the effects of list staggering and the ‘Golden Patient’ and found that both these interventions made a positive contribution to our patients' experience. Waiting times were reduced: the percentage of patients waiting for more than 4.5 hours fell from 47% to 19%, and the percentage waiting for more than 6.5 hours fell from 27% to 0%. However, while some lists had staggered arrival times, others did not. We continued to work with the bookings teams and individual surgeons to increase the number of surgical lists that have a ‘Golden Patient’ and are staggered.
One problem was that if the ‘Golden Patient’ did not arrive in a good time for their admission, it had serious adverse effects on the running of the whole theatre list. To ameliorate this, the nurses on DSU began calling the ‘Golden Patient’ the day before their operation to ensure that they were able to get to the hospital at the correct time.
We discovered that the information given to patients before they came to the hospital was not clear enough and did not mention the possibility of any sort of wait on the day of surgery. Our survey showed that half of the patients expected to have their operation within 2 hours of arrival at the hospital. To better manage our patients’ expectations, we have altered the patient information letters to state that there may be a waiting time before their operation. We identified pre-assessment clinic as an opportunity to set expectations before the day of the operation. We worked with the nurses in pre-assessment and now they raise the likelihood of waiting with patients before the day of their operation. Also, our colleagues have produced a video that explains the patient journey and mentions that there may be a wait. This video is on the Trust's website so that patients can view it before they come to the hospital.19
The data from the project were presented at the theatre staff's clinical governance day with the aim of reinforcing the changes we have made. The Theatre Strategy team then performed a rolling series of ‘deep dive’ exercises in which they take a detailed look at the processes of each surgical specialty in turn. Staggering patients’ arrival on the day of surgery and identifying the ‘Golden Patient’ are now part of this process as they both improve patient satisfaction and increase theatre efficiency (see online supplementary file 1).
Results
When quoted, p values are calculated using a web-based two-tailed Fisher's exact test (https://www.graphpad.com/quickcalcs/contingency1/).
Our baseline data from the RFH in July 2015 showed that patients who had their operations later in the day were less likely to report a positive experience. We identified three main reasons for low satisfaction scores.
Long waiting times. Nearly half (47%) of patients waited for more than 4.5 hours before surgery and 27% waited more than 6.5 hours.
Poor communication. There was a clear disparity between our patients’ expectations and what the staff knew the reality was likely to be. Forty-seven per cent of patients thought their operation would start within 2 hours of arrival. Furthermore, only 36% were informed of the likely start time of their operation.
Prolonged fasting. All of the patients had not eaten for more than 10 hours and 62% had not had clear fluids for more than 6 hours before their operation. Both hunger and thirst scores were lower for those patients who had their operation before 12:00 compared with those who had their operation later in the day.
We implemented several changes during this project, and the overall percentage of patients reporting their experience as ‘Excellent’ or ‘Good’ increased from 65% in 2015 to 93% in 2016 and to 96% in 2017.
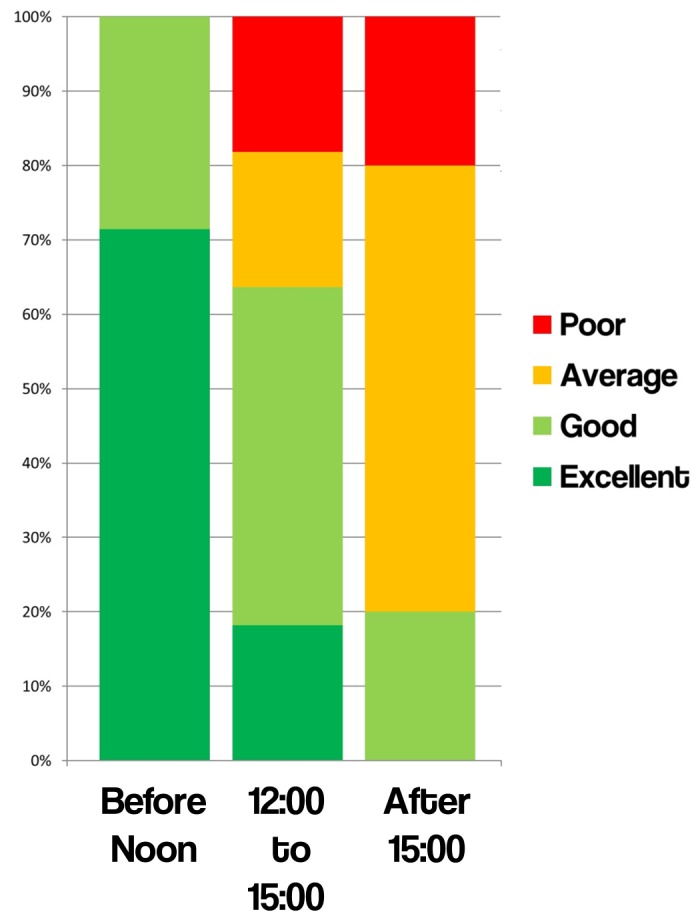
When analysed by time of day, the results are as follows:
For patients who had their surgery before 12:00, 100% of patients rated their experience as ‘Excellent’ or ‘Good’ in 2015, and this stayed the same in both 2016 and 2017.
For patients who had their surgery between 12:00 and 15:00, 64% of patients rated their experience as ‘Excellent’ or ‘Good’ in 2015. The results from 2016 and 2017 showed improvement at 80% and 89%, respectively.
For patients who had their surgery after 15:00, only 20% of patients rated their experience as ‘Excellent’ or ‘Good’ in 2015. This improved by 100% in both 2016 and 2017.
In the 2015 cohort, when comparing patients who had their operation before 12:00 with those who had their operation after 15:00, those having their operation later in the day were statistically significantly more likely to report their experience as ‘Average’ or ‘Poor’ compared with ‘Excellent’ or ‘Good’ (p=0.01) (figure 1). In both the 2016 and 2017 cohorts, there was no statistically significant difference in the experience for patients having their operations before 12:00 and those who had it after 15:00 (p=1.00) (figure 2).
Figure 2.
Satisfaction scores by time of day.
A long waiting time before surgery was repeatedly mentioned by patients in their interviews as a factor that contributed to a poor experience. This project has delivered a significantly shorter waiting time for our patients. The percentage of patients waiting more than 4.5 hours fell from 47% in 2015 to 19% in 2016, and again to 7% in 2017. The percentage with a very long wait of more than 6.5 hours fell from 19% in 2015 to 0% in both 2016 and 2017.
In addition, we looked at whether patients were made more aware of the time of their operation. In 2015, 36% of patients knew of the time of their operation. This improved to 47% in 2016, and 48% in 2017. This means that there is still work to be done to improve our communication with patients.
With respect to thirst, 36% of patients reported ‘moderate’ or ‘severe’ thirst in 2015. This reduced to 29% in 2016, and 21% in 2017. Regarding hunger, 41% of patients reported ‘moderate’ or ‘severe’ hunger in 2015. This fell to 21% in 2016, and 18% in 2017. Notably, no patients reported ‘severe’ hunger in 2016 or 2017.
Some of the qualitative comments from patients are as follows:
“I'm a bit hungry, I suppose. And perhaps a bit more anxious than I would have been earlier in the morning, simply because I've been waiting all day—and second because you're thinking ‘I've got the same surgeons who have been doing operations for 6 hours doing a job on me in a while.’” Patient A, 2015
“I think (the wait) is just bloody awful, really. They asked me to come up here at half past seven and I'm still waiting. They haven't told me why… I just have to wait.’ Patient B, 2015
“(My overall experience) has been very good. Everyone seems really friendly and I'm quite pleased with it. If you ask questions, you get answers and that's really good.’ Patient C, 2016
‘It's been perfect, I've had no problems with the staff at all. The service has been excellent.’ Patient D, 2016
‘Very professional and pleasant experience. Thank you.’ Patient E, 2017
Lessons and limitations
Engagement of multidisciplinary teams was paramount to this project. For example, to stagger the patients’ arrival times, coordination begins with the schedulers in the admission department and involves surgeons, anaesthetists, preassessment nurses, managers and DSU nurses.
Our Trust is a large organisation and the large number of people involved posed several challenges. Some steps, such as changing patients’ admissions letters, took a long time to implement. Each step required a great deal of effort and goodwill. Sometimes, there was resistance to change; however, we found that once the benefits of change were demonstrated, people were more willing to engage with the project. This highlights the critical importance of giving feedback to the people involved with initiatives. Some work on this project remains ongoing, for instance, identifying the ‘Golden Patient’ remains a challenge on some lists and is the focus of further work.
One potential limitation was that the numbers of patients eligible for participation in our study varied. Our nurses report that they have more time to spend with each patient when there is a higher staff-to-patient ratio. However, the busiest day was in February 2017, which had the best satisfaction scores. This shows that our project's changes are robust and lead to increased patient satisfaction despite the ward being under more pressure.
Each PDSA cycle involved multiple interventions and large numbers of people. This is because the reasons that lead to a poor patient experience are multifactorial. The factors identified, such as long waiting times and poor communication have multiple causes. Also, the processes involved in making changes such as the ‘Golden Patient’ are long and complex. As such, rather than making a series of small changes and trying to measure their individual effectiveness, we simultaneously made several changes with the aim of influencing the system as a whole. We found this approach to be effective; however, it does mean that it is not possible to quantify the contribution that individual interventions made to the overall improvement in patient experience.
Some of the interventions, such as list staggering, were introduced specialty-by-specialty basis. Our project measured the experience of all patients, not just those of a particular specialty, and this meant that some of the interventions did not fit neatly into a PDSA cycle.
Conclusion
Quality improvement is at the centre of what our Trust is trying to achieve. One of the Trust's annual objectives is to implement our organisation-wide approach to quality improvement in order to provide better services and better value for patients. The Royal Free London NHS Foundation Trust aims to be in the top 10% of all healthcare providers for patient satisfaction and experience.12
Coulter et al wrote that “Careful observation, measurement, recording, interpretation, and analysis of patients’ subjective experiences are essential to appreciating what is working well in healthcare, what needs to change, and how to go about making improvements.”20
Our project has achieved its primary aim of improving overall patient experience. The percentage of patients reporting an ‘Excellent’ or ‘Good’ experience increased from 65% to 96%. By speaking to our patients and our staff, we were able to discover the reasons behind low satisfaction scores and use this information to focus our efforts on changes that were likely to be most productive. In this way, our project has delivered shorter waiting times, there are fewer patients reporting feeling thirsty or hungry and overall satisfaction has increased. The interdisciplinary workgroup was crucial in getting the input and engagement of the different teams involved in this process.
With our work so far, we have demonstrated how to make the experience of elective surgery better, but there are plenty of opportunities for continued improvement. Further review and data collection continue and it is hoped that by targeting the behaviours of the multidisciplinary team and patients, we will continue to improve the experience of elective surgery for our patients.
Acknowledgments
The authors would like to thank all those involved in this project, especially the DSU nurses and our patients who agreed to take part.
Footnotes
Twitter: @RFAnaesthesia
Contributors: TF and VVR designed the study. All authors collected data for the study. All authors analysed the data collected. TF, SW, VVR and HE conducted patient interviews and analysed their results. TF and SW wrote the first draft of the article. TF completed the final revision of the article.
Competing interests: None declared.
Ethics approval: This project evaluated the service we are providing to our patients with aim of improving the quality of that service. It did not involve new research on our patients and, as such, approval from the Researchand Ethics Committee was not required. This statement was agreed by the Royal Free London's Research and Development department.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Darzi A. High Quality care for all. NHS Next Stage Review Final Report. Department of Health, 2008. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/228836/7432.pdf (accessed 31 July 2017). [Google Scholar]
- 2. NHS England. Improving patient experience. https://www.england.nhs.uk/ourwork/pe/ (accessed 7 Sep 2016).
- 3. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570 doi:10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boulding W, Glickman SW, Manary MP, et al. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care 2011;17:41–8. [PubMed] [Google Scholar]
- 5. Stone S. A retrospective evaluation of the impact of the Planetree patient-centered model of care on inpatient quality outcomes. HERD 2008;1:55–69. doi:10.1177/193758670800100406 [DOI] [PubMed] [Google Scholar]
- 6. NHS Group. The NHS Outcomes Framework 2015/16. Department of Health, 2014. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/385749/NHS_Outcomes_Framework.pdf (accessed 15 Sep 2016). [Google Scholar]
- 7. Kain ZN, Mayes LC, Caldwell-Andrews AA, et al. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics 2006;118:651–8. doi:10.1542/peds.2005-2920 [DOI] [PubMed] [Google Scholar]
- 8. Broadbent E, Petrie KJ, Alley PG, et al. Psychological stress impairs early wound repair following surgery. Psychosom Med 2003;65:865–9. doi:10.1097/01.PSY.0000088589.92699.30 [DOI] [PubMed] [Google Scholar]
- 9. Boorman S. Health NHS. NHS Health and Wellbeing. Department of Health, 2009. http://webarchive.nationalarchives.gov.uk/20130124052412/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_108907.pdf (accessed 31 July 2017). [Google Scholar]
- 10. Browne K, Roseman D, Shaller D, et al. Measuring patient experience as A strategy for improving primary care. Health Aff 2010;29:921–5. [DOI] [PubMed] [Google Scholar]
- 11. Manary MP, Boulding W, Staelin R, et al. N Engl J Med 2013;368:201–3. [DOI] [PubMed] [Google Scholar]
- 12. Clarke C. Operation Plan Document for 2016/17 Royal Free London NHS Foundation Trust. Royal Free London NHS Foundation Trust. 2016. http://s3-eu-west-1.amazonaws.com/files.royalfree.nhs.uk/AboutUs/Publishable_summary_of_operational_plan_2016-17_v1_0_18apr16.pdf (accessed 15 Sep 2016).
- 13. Royal Free London NHS Foundation Trust. Our vision, mission and values. 2016. https://www.royalfree.nhs.uk/about-us/world-class-expertise-local-care/our-vision-mission-and-values/ (accessed 15 Sep 2016).
- 14. Kaur R, Hoogenboom E, Mangwiro R, et al. , 2016. Poster presented at: health Education England, North Central East London Quality Improvement Conference. Anaesthesia Outcome Measures in Royal Free Hospital, London, London, UK. [Google Scholar]
- 15. Falconer R, Skouras C, Carter T, et al. Preoperative fasting: current practice and areas for improvement. Updates Surg 2014;66:31–9. doi:10.1007/s13304-013-0242-z [DOI] [PubMed] [Google Scholar]
- 16. Raman V V, Fregene T. Elective surgery in the NHS: are patients satisfied with their experience on the day of their operation? Anaesthesia 2016;71(Suppl. 2):83. [Google Scholar]
- 17. The Royal College of Surgeons. The high performing surgical team - A guide to best practice. The Royal college of surgeons of England., 2014. https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/the-high-performing-surgical-team/ (accessed 31 July 2017). [Google Scholar]
- 18. The Word Health Organisation. WHO surgical safety checklist and implementation manual. http://www.who.int/patientsafety/safesurgery/ss_checklist/en/ (accessed 13 Sep 2016).
- 19. Kidel C. What to expect on the day of your operation. 2016. http://www.royalfree.nhs.uk/services/services-a-z/anaesthetics/on-the-day-of-your-operation/ (accessed 15 Sep 2016).
- 20. Coulter A, Locock L, Ziebland S, et al. Collecting data on patient experience is not enough: they must be used to improve care. BMJ 2014;348:g2225 doi:10.1136/bmj.g2225 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2017-000079supp001.docx (32.3KB, docx)