Abstract
Objectives
To investigate the role of occupational exposure to endotoxins in lung cancer in a French population-based case–control study (ICARE (Investigation of occupational and environmental causes of respiratory cancers)).
Methods
Detailed information was collected on the occupational history and smoking habits from 2926 patients with histologically confirmed lung cancer and 3555 matched controls. We evaluated each subject’s endotoxin exposure after cross referencing International Standard Classification of Occupations (ISCO) codes (for job tasks) and Nomenclature d'Activités Françaises (NAF) codes (for activity sectors). Endotoxin exposure levels were attributed to each work environment based on literature reports. ORs and 95% CIs were estimated using unconditional logistic regression models and controlled for main confounding factors.
Results
An inverse association between exposure to endotoxins and lung cancer was found (OR=0.80, 95% CI 0.66 to 0.95). Negative trends were shown with duration and cumulative exposure, and the risk was decreased decades after exposure cessation (all statistically significant). Lung cancer risk was particularly reduced among workers highly exposed (eg, in dairy, cattle, poultry, pig farms), but also in those weakly exposed (eg, in waste treatment). Statistically significant interactions were shown with smoking, and never/light smokers were more sensitive to an endotoxin effect than heavy smokers (eg, OR=0.14, 95% CI 0.06 to 0.32 and OR=0.80, 95% CI 0.45 to 1.40, respectively, for the quartiles with the highest cumulative exposure, compared with those never exposed). Pronounced inverse associations were shown with adenocarcinoma histological subtype (OR=0.37, 95% CI 0.25 to 0.55 in the highly exposed).
Conclusions
Our findings suggest that exposure to endotoxins, even at a low level, reduces the risk of lung cancer.
Keywords: case-control studies, endotoxins, lung cancer, occupational exposure
What this paper adds.
Since 1970, epidemiological studies have shown that occupational exposure to high levels of endotoxins may reduce the risk of lung cancer, although with some inaccuracies in measurements of exposure to endotoxins and inadequate adjustment for tobacco smoking.
Our results confirmed the presence of a reduced risk of lung cancer among workers exposed to endotoxins.
We were able to adequately control for cigarette smoking and asbestos exposure and to model dose–effect relationships.
This is the first study to have scanned a wide range of industries and environments exposed to endotoxins. Considerable work was done in order to attribute a definite level of endotoxin exposure to each job held by the subjects.
Introduction
Lung cancer is the most common and most lethal neoplasm worldwide. Tobacco smoke is by far the main aetiological factor in lung carcinogenesis; however, other factors have been recognised as playing a role—most importantly, occupational exposures.1
The first studies conducted on textile worker cohorts, starting in 1973, showed lower rates of lung cancer than expected.2 3 Similar results were found in agricultural workers, and were initially attributed to light smoking habits and/or to a healthy worker effect.4 A potential role of endotoxin exposure was first advanced in 1985.5 Since then, several epidemiological studies have reported that occupational exposure to endotoxins in agriculture, textile or other industries may reduce the risk of lung cancer.6
Endotoxin is a cell wall component of Gram-negative bacteria that is released when bacteria die and lysis occurs. Endotoxins are lipopolysaccharidzes comprising a polysaccharide component responsible for their antigenicity, and a lipid component responsible for their toxicity.7 As bacterial constituents are continuously shed into the surrounding environment, substantial endotoxin exposure occurs—for example, in agricultural work (particularly livestock), waste treatment, textile industries (particularly cotton), and to a lesser degree in cigarette factories, paper mills and dental offices.8 9 Concentrations of airborne endotoxins are usually expressed as ng/m3 or as endotoxin units per volume (EU/m3).
Even at relatively low levels (50–500 EU/m³ over 8 hours), endotoxins have been recognised as important inflammagenic factors in the aetiology of occupational lung diseases, including non-atopic asthma, organic dust toxic syndrome and decreased lung function.10 11 In contrast with these noxious effects, endotoxins might have protective effects on allergy and atopic asthma, possibly through stimulation of the immune system, a mechanism that might also be responsible for reduced lung cancer rates.12
Most epidemiological studies on the association between endotoxin exposure and lung cancer have used occupational history as a proxy of exposure6 and only a few integrated a job–exposure matrix.13 14 Some studies included small numbers and methodological weaknesses due to inadequate adjustment for tobacco smoking and other occupational exposures.6 15 Moreover, interactions with other respiratory diseases have been rarely evaluated, particularly with asthma, where the association with lung cancer risk is still debated.16
The aim of this study was to investigate the association between lung cancer and work in a large range of industries and environments entailing both weak and high exposure to endotoxins in a large population-based case–control study conducted in France. We were able to adequately control for cigarette smoking and asbestos exposure, to model dose–effect relationships and to assess whether the effect of endotoxins was modified by smoking habits or a history of asthma.
Materials and methods
Study population
The ICARE Study (Investigation of occupational and environmental causes of respiratory cancers) is a large multicentre population-based case–control study conducted in France, in 10 administrative departments covered by cancer registries, from 2001 through 2007. All residents newly diagnosed with histologically confirmed lung cancer at ages 18–75 were included. Controls were identified through random digit dialling and were randomly selected through incidence-density sampling methods by a polling institute in the same departments as the cases. They were matched to cases by sex, age (in four categories: <40, 40–54, 55–64, >65) and department of residence. An additional stratification was performed to make the distribution of the controls by socioeconomic status comparable to that of the general population in each department.
Of the 4865 eligible cases identified, 781 (16%) had died, 489 (10%) were unreachable and 238 (5%) were too ill to be interviewed. Among the 3357 remaining subjects, 2926 (87%) agreed to participate. We contacted 4411 controls (94% of the 4673 eligible controls) and 3555 (81%) gave their consent to participate. Additional details of the enrolment and data collection were published previously.17
All respondents gave written informed consent to participate. The study protocol was approved by the institutional review board of the French National Institute of Health and Medical Research (IRB-Inserm, n°01–036).
Data collection
Trained interviewers administered standardised questionnaires during face-to-face interviews. Detailed information was collected from cases and controls for a number of lung cancer risk factors, including sociodemographic characteristics, medical history and smoking habits. Lifetime occupational histories were collected, considering each job held for at least 1 month. Subjects were asked for job title, year the job started and ended, sector and their main and subsidiary tasks. Supplementary questionnaires were used to assist interviewers with detailed technical probing for some occupations. The specific agriculture/livestock questionnaire included, among others, questions about the type of activity, type of livestock on the farm and number of heads.
For each job, the employer’s sector was coded into the French classification of activities (NAF (Nomenclature d'Activités Françaises), 1999) of the National Institute for Statistics and Economics Studies (INSEE),18 and the job was coded according to the International Standard Classification of Occupations (ISCO, 1968) of the International Labour Organisation.19 The coders were blinded to the subject’s disease status.
If the subject was too sick or tired to answer the complete questionnaire, a shortened version was used, including information on smoking and occupational history, but without detailed questions on each job held.
Occupational exposure assessment
The evaluation of exposure to endotoxins was based on a report by the Institut National de Recherche et de Sécurité (INRS),9 whose authors identified published studies on the measurement of air-borne endotoxins, and classified several work environments by providing lower and upper levels of exposure. First, we went to the original articles and computed the mean of geometric means, as they were reported in the papers. Then we attributed this mean level (called intensity and expressed as arbitrary units per volume: UE/m3) to the different work environments, which we classified according to the NAF and ISCO codes. Finally, each job period of the subjects, as defined by the NAF and ISCO code system, was matched to the corresponding work environment with its exposure intensity, providing a quantitative estimate of endotoxin exposure.
Any peculiarity of the study population was also taken into account, when matching job periods to work environments. In France, many agriculture workers have their own farms and carry out activities including both livestock and crops, coded together as ‘Growing of crops combined with farming of animals: mixed farming’ (NAF code 01.3). For this group, we calculated the median number of animals, as declared by the controls in the specific agriculture questionnaire. Subjects who declared a number of animals higher than the median were included in the corresponding livestock’s work environment (dairy farms, cattle, poultry or pigs). Subjects who declared fewer animals than the median were included in greenhouse or outside plant cultivation work environment groups.
Subjects may belong to one or more work environment groups, according to their personal occupational history. For each subject, the maximum intensity of all the work environments in which he/she ever worked was used as his/her exposure level.
In addition, subjects were classified as having high or low endotoxin exposure, with a threshold of 1000 UE/m3. This limit corresponds to the 90th centile of previous endotoxin measurements in France, and was chosen in agreement with the guidelines issued by the INRS, which indicated higher exposures as unacceptable working situations.20 Thus dairy farms (1570 UE/m3), cattle (1570 UE/m3), poultry (84 310 UE/m3), pigs (1510 UE/m3), work with grains (6000 UE/m3), grain transport (2150 UE/m3) and the cotton industry (4540 UE/m3) were classified into the high endotoxin exposure group. The others (eg, cultivation (110 UE/m3), bakeries (49 UE/m3), meat work (23 UE/m3), waste collection and treatment (103 UE/m3), sawmills (190 UE/m3) and wool industry (83 UE/m3)) were categorised as low exposure.
Subjects whose occupational history included both low and high exposure jobs were excluded from the analyses stratified on exposure level (n=22).
A cumulative exposure index was obtained for each subject by summing the product of exposure intensity and duration of each job period, over the entire work history.
Time since cessation was calculated by subtracting age at the last job entailing an exposure to endotoxins from age at diagnosis or interview.
Confounding factors
Lifelong cigarette smoking was classified with the Comprehensive Smoking Index (CSI),21 a single aggregate measure incorporating total duration of cigarette smoking, average number of cigarettes per day and time since smoking cessation.
Subjects were considered asthmatic if they reported having asthma diagnosed by a physician and had no history of chronic obstructive pulmonary disease.
Asbestos exposure was evaluated using a specific job-exposure matrix, as previously described.22
Statistical analyses
Multivariable unconditional logistic regression models were applied to estimate ORs and 95% confidence CIs for all exposure variables. Analyses were systematically adjusted for age at interview, gender, department, number of jobs held, CSI, education level and occupational exposure to asbestos. In our data, the CSI varied linearly with lung cancer risk, thus it has been introduced in the model as a continuous adjusting variable.
All endotoxin exposure variables were transformed into qualitative variables according to quartiles of distribution among the controls. We also performed analyses stratified on smoking status, histological type and history of asthma. The modification effect has been tested with logistic regression by the likelihood ratio method.
Given the small proportion of women exposed to endotoxins (50 cases and 83 controls; 12%), analyses were carried out jointly for men and women. Only work environments with at least 10 exposed subjects and at least five exposed cases were analysed, resulting in exclusion of 8 cases and 14 controls from the analysis.
Dose–response associations were tested with maximum likelihood estimates based on the categorical variables, after testing the linearity of the association. Additionally, we used a restricted cubic spline to model the association between endotoxin exposure duration or time since cessation and lung cancer risk. This approach minimises residual confounding when adjusting for a continuous variables (here, age at interview was included in the model using a restricted cubic spline function).
Statistical analyses were performed using SAS software (SAS Institute Inc; North Carolina USA; version 9.4). All p values were two-sided and a p value ≤0.05 was the threshold for statistical significance.
Results
The main sociodemographic characteristics of the whole study population are summarised in table 1, together with cigarette smoking indices and lung cancer histologies. Twenty per cent of cases and controls were women. Cases were, on average, slightly older than controls, and had a lower education level (both statistically significant). As expected, a considerable increase in the risk of lung cancer was observed in association with cigarette smoking. The mean number of jobs held was higher in controls, while the average duration of employment was longer among cases (both statistically significant); however, the differences between cases and controls were minimal in absolute figures.
Table 1.
Sociodemographic and other selected characteristics of the study population by case–control status
| Characteristics | Cases | Controls | OR* | 95% Cl | ||
| N | % | N | % | |||
| Total | 2926 | 3555 | ||||
| Gender | ||||||
| Male | 2276 | 77.8 | 2780 | 78.2 | ||
| Female | 650 | 22.2 | 775 | 21.8 | p**=0.68 | |
| Department | ||||||
| Calvados | 354 | 12.1 | 462 | 13.0 | – | – |
| Doubs et territoire de Belfort | 149 | 5.1 | 143 | 4.0 | – | – |
| Hérault | 334 | 11.4 | 450 | 12.7 | – | – |
| Isère | 476 | 16.3 | 501 | 14.1 | – | – |
| Loire Atlantique | 350 | 12.0 | 404 | 11.4 | – | – |
| Manche | 320 | 10.9 | 312 | 8.8 | – | – |
| Bas-Rhin | 398 | 13.6 | 469 | 13.2 | – | – |
| Haut-Rhin | 73 | 2.5 | 118 | 3.3 | – | – |
| Somme | 321 | 11.0 | 499 | 14.0 | – | – |
| Vendée | 151 | 5.2 | 197 | 5.5 | – | – |
| Age at interview (years) | ||||||
| <50 | 466 | 15.9 | 827 | 23.3 | 1.00 | Reference |
| 50–60 | 999 | 34.1 | 1012 | 28.5 | 1.75 | (1.51–2.02) |
| 60–70 | 989 | 33.8 | 1186 | 33.4 | 1.47 | (1.27–1.70) |
| ≥70 | 472 | 16.1 | 530 | 14.9 | 1.59 | (1.34–1.88) |
| Mean (SD) | 59.69 (9.34) | 58.52 (10.22) | p**<0.001 | |||
| Highest educational level† | ||||||
| Elementary school or less | 879 | 32.7 | 763 | 21.92 | 1.00 | Reference |
| Middle school | 1077 | 40.1 | 1351 | 38.81 | 0.64 | (0.56–0.73) |
| High school | 257 | 9.6 | 400 | 11.49 | 0.51 | (0.41–0.61) |
| University | 383 | 14.3 | 901 | 25.88 | 0.33 | (0.28–0.40) |
| Unknown | 88 | 3.3 | 23 | 2 | ||
| Cigarette smoking history | ||||||
| Never smoked‡ | 247 | 8.4 | 1326 | 37.3 | 1.00 | Reference |
| Former smokers | 995 | 34.0 | 1485 | 41.77 | 3.45 | (2.93–4.05) |
| Current smokers | 1667 | 57.0 | 742 | 20.87 | 16.35 | (12.92–18.23) |
| Missing | 17 | 0.6 | 2 | 0.06 | ||
| Cumulative cigarette consumption (CSI) | ||||||
| 0‡ | 247 | 8.4 | 1326 | 37.3 | 1.00 | Reference |
| 0–0.5 | 133 | 4.5 | 704 | 19.8 | 1.01 | (0.81–1.27) |
| 0.5–1 | 271 | 9.3 | 565 | 15.9 | 2.67 | (2.20–3.27) |
| 1–1.5 | 505 | 17.3 | 457 | 12.9 | 6.46 | (5.34–7.82) |
| 1.5–2 | 979 | 33.5 | 377 | 10.6 | 14.53 | (12.06–17.52) |
| >2 | 762 | 26.0 | 115 | 3.2 | 36.15 | (28.35–46.11) |
| Missing | 29 | 0.99 | 11 | 0.3 | ||
| Number of jobs held | ||||||
| 0 | 42 | 1.4 | 15 | 0.4 | 2.44 | (1.31–4.54) |
| 1 | 292 | 10.0 | 269 | 7.6 | 1.00 | Reference |
| 2 | 482 | 16.5 | 541 | 15.2 | 0.81 | (0.66–1.01) |
| 3 | 552 | 18.9 | 691 | 19.4 | 0.7 | (0.57–0.86) |
| 4 | 512 | 17.5 | 614 | 17.3 | 0.71 | (0.58–0.88) |
| ≥5 | 1046 | 35.7 | 1425 | 40.1 | 0.61 | (0.51–0.75) |
| Number of jobs held, mean (SD) | 4.14 (2.65) | 4.38 (2.54) | p**=0.0002 | |||
| Total duration of employment, mean (SD)† | 34.40 (10.82) | 34.02 (10.24) | P**=0.02 | |||
| Histological types | ||||||
| Squamous cell carcinoma | 906 | 31.0 | – | – | ||
| Small cell carcinoma | 429 | 14.7 | – | – | ||
| Adenocarcinoma | 1145 | 39.1 | – | – | ||
| Large cell carcinoma | 246 | 8.4 | – | – | ||
| Other types | 200 | 6.8 | – | – | ||
*OR adjusted for age at interview and department.
**p Values are derived from the Pearson’s χ2 test for categorical variables or Student's test for continuous variables.
†Only available for the complete questionnaire.
‡Non-smokers were subjects who had smoked fewer than 100 cigarettes in their lifetime.
§Former smokers were subjects who had stopped smoking at least 2 years before diagnosis (cases)/interview (controls).
CSI, Comprehensive Smoking Index.
In the ICARE population, 465 cases (15.9%) and 660 controls (18.6%) were classified as ever exposed to endotoxins. Overall, a statistically significant inverse association between exposure to endotoxins and lung cancer was found (OR=0.80, 95% CI 0.66 to 0.95), as is shown in table 2. Analysis by work environment group showed a decrease in lung cancer risk among workers highly exposed to endotoxins in dairy, cattle, poultry, pig farms and in waste collection and treatment, with strong statistically significant ORs between 0.25 (dairy farmers) and 0.51. No other association reached statistical significance, but there was a suggestion of a reduced risk for greenhouse plant cultivation, work with grains and grain transport, while risks seemed to be increased for workers in meat processing, sawmills, wool industry and dental offices. ORs around unity were found for some other work environments (outside plant cultivation, bakeries, slaughterhouses, cotton industry and paper factories), while for others no meaningful comparison was possible, owing to low numbers.
Table 2.
Distribution of cases and controls and risk of lung cancer by work environmenf
| INRS Work Environment Group | Sector/activity (NAF code*) | Occupation/process (ISCO code†) | Cases | Controls | OR§ | 95% Cl |
| Mean UE/m3(±SD)‡ | N | N | ||||
| Never worked in environment exposed to endotoxins¶ | 2461 | 2895 | 1.00 | Reference | ||
| Ever worked in environment exposed to endotoxins** | 465 | 660 | 0.8 | (0.66–0.95) | ||
| Agriculture | ||||||
| Greenhouse plant cultivation | 23 | 39 | 0.66 | (0.33–1.33) | ||
| 110 (±4.3) | Growing of vegetables; truck farming (01.1C) | Farm managers and supervisors (6–00†) | ||||
| Growing of horticultural specialities and nursery products(01.1D) | General farmers (6–11) | |||||
| Growing of fruit (except grapes) (01.1F) | Horticultural Farmer (6–12.70) | |||||
| Agricultural service activities (01.4A) | General Farm Workers (6–21.05/10) | |||||
| Growing of crops combined with farming of animals (mixed farming)(01.3Z) | Nursery Workers and Gardeners (627†) | |||||
| Outside plant cultivation | 99 | 131 | 0.94 | (0.66–1.35) | ||
| 110 (±2.5) | Growing of crops; market gardening; horticulture (01.1*) | Farm managers and supervisors (6–00†) | ||||
| Agricultural service activities (01.4A) | General farmers (6–11) | |||||
| Growing of crops combined with farming of animals (mixed farming)(01.3Z) | Specialised farmers (6–12.20/30/70) | |||||
| General farm workers (6–21†) | ||||||
| Field crop and vegetable farm workers (6–22†) | ||||||
| Orchard, vineyard and related tree and shrub crop workers (6–23†) | ||||||
| Nursery workers and gardeners(6–27†) | ||||||
| Dairy farms†† | 31 | 87 | 0.25 | (0.14–0.45) | ||
| 1570 (±2.5) | Farming of cattle (01.2A) | Farm managers and supervisors (6–00†) | ||||
| Farming of sheep, goats, horses, asses, mules and hinnies (01.2C) | General farmers (6–11) | |||||
| Animal husbandry service activities, except veterinary activities (01.4D) | Specialised farmers (6–12.40/50) | |||||
| Growing of crops combined with farming of animals (mixed farming)(01.3Z) | General farm workers (6–21†) | |||||
| Dairy farm workers (6–25†) | ||||||
| Cattle†† | 97 | 256 | 0.43 | (0.31–0.6) | ||
| 1570 (±2.5) | Farming of cattle (01.2A) | Farm managers and supervisors (6–00†) | ||||
| Farming of sheep, goats, horses, asses, mules and hinnies (01.2C) | General farmers (6–11) | |||||
| Growing of crops combined with farming of animals (mixed farming)(01.3Z) | Specialised farmers (6–12.40/50) | |||||
| General farm workers (6–21†) | ||||||
| Livestock workers (6–24†) | ||||||
| Dairy farm workers (6–25†) | ||||||
| Poultry†† | 34 | 109 | 0.44 | (0.26–0.71) | ||
| 84 310 (±13) | Farming of poultry (01.2G) | Farm managers and supervisors (6–00†) | ||||
| Growing of crops combined with farming of animals (mixed farming)(01.3Z) | General farmers (6–11) | |||||
| Poultry farmer (6–12.60) | ||||||
| Farm worker (general)(6–21.05) | ||||||
| Poultry farm workers (6–26†) | ||||||
| Pigs†† | Farming of swine (01.2E) | Farm managers and supervisors (6–00†) | 39 | 115 | 0.48 | (0.3–0.76) |
| 1510 (±2.1) | Growing of crops combined with farming of animals (mixed farming)(01.3Z) | General farmers (6–11) | ||||
| Livestock farmer (6–12.40) | ||||||
| General farm workers (6–21†) | ||||||
| Livestock worker (general) (6–24.10) | ||||||
| Pig farm workers (6–24.40) | ||||||
| Work with grains | 25 | 45 | 0.72 | (0.36–1.4) | ||
| 6000 (±8.6) | Growing of cereals and other crops n.e.c. (01.1A) | Farm managers and supervisors (6–00†) | ||||
| Growing of fruit (except grapes) (01.1F) | General farmers (6–11) | |||||
| Agricultural service activities (01.4A) | Specialised farmers (6–12.20/30/70) | |||||
| Manufacture of grain mill products. starches and starch products (15.6*) | General farm workers (6–21†) | |||||
| Field crop and vegetable farm workers (6–22†)excluding 6–22.40 and 6–22.60 | ||||||
| Grain millers and related workers (7–71†) | ||||||
| Agri-transformation/agri-food | ||||||
| Flour manufacturing | 2 | 2 | - | - | ||
| 280 (±7.7) | Flour milling (15.6A) | Grain millers and related workers (7–71†) | ||||
| Coffee-roasting plant and tea trading | 4 | 4 | - | - | ||
| 140 (±3.4) | Processing of tea and coffee (15.8P) | Tea, coffee and cocoa preparers (7–77†) | ||||
| Sugar production | 1 | 2 | - | - | ||
| 130 (±4.0) | Manufacture of sugar (15.8 hour) | Sugar processers and refiners (7–72†) | ||||
| Bakeries | 48 | 44 | 1.07 | (0.64–1.81) | ||
| 49 (±7.4) | Bakery and bakery confectionery (15.8C) | Bakers, pastry cooks and confectionery makers (7–76†) | ||||
| Grain transport | 8 | 14 | 0.4 | (0.13–1.23) | ||
| 2150 (±9.0) | Growing of cereals and other crops n.e.c. (01.1A) | Farm machinery operators (628†) | ||||
| Growing of fruit (except grapes) (01.1F) | Motor vehicle drivers (9–85.50/60) | |||||
| Agricultural service activities (01.4A) | ||||||
| Manufacture of grain mill products. starches and starch products (1.56*) | ||||||
| Slaughterhouses | 30 | 25 | 1.07 | (0.55–2.09) | ||
| 51 (±6.8) | Production and preserving of meat (15.1A) | Butchers and meat preparers (7–73†) | ||||
| Production and preserving of poultry meat (15.1C) | ||||||
| Meat processing | 22 | 19 | 1.41 | (0.63–3.13) | ||
| 23 (±3.6) | Industrial production of meat products (15.1E) | Butchers and meat preparers (7–73†) | ||||
| Cooked meats production and trade (15.1F) | ||||||
| Waste collection and treatment | 26 | 43 | 0.51 | (0.27–0.95) | ||
| Waste collection and treatment | Sewage and refuse disposal. sanitation and similar activities (90.0*) | Charworkers, cleaners and related workers (5–52†) | ||||
| 103 (±3.1) | Stationary engine and related equipment operators not elsewhere classified (9–69.50/60/90) | |||||
| Material handling equipment operators not elsewhere classified (9–79.30/90) | ||||||
| Motor vehicle drivers (9–85.50/60/90) | ||||||
| Labourers (9–99.10) | ||||||
| Wood industry | ||||||
| Sawmills | 80 | 69 | 1.36 | (0.9–2.07) | ||
| 190 (±5.7) | Manufacture of wood and of products of wood and cork, except furniture; | Sawyers, plywood makers and related wood-processing workers (7–32†) | ||||
| manufacture of articles of straw and plaiting materials (20*) | Cabinet makers and related woodworkers (8–1†) | |||||
| Carpenters, joiners and parquetry workers (9–54†) | ||||||
| Textile industry | ||||||
| Cotton | 19 | 17 | 1.03 | (0.28–3.74) | ||
| 4540 (±15) | Preparation and spinning of textile fibres (17.1A/M) | Fibre preparers (7–51‡ excluding 7–51.20) | ||||
| Cotton-type weaving (17.2A) | Spinners and winders (7–52†) | |||||
| Manufacture of made-up textile articles, except apparel (17.4*) | Weavers and related workers (7–54†) | |||||
| Manufacture of other textiles (17.5A/C/E/G) | Spinners, weavers, knitters, dyers and related workers not elsewhere classified (7–59.20/25) | |||||
| Wool | 12 | 8 | 2.25 | (0.75–6.75) | ||
| 83 (±24) | Preparation and spinning of textile fibres (17.1C/E/F) | Fibre preparers (7–51†) | ||||
| Textile weaving (17.2C/E) | Spinners and winders (7–52†) | |||||
| Manufacture of carpets and rugs (17.5A) | Knitters (7–55†) | |||||
| Manufacture of knitted and crocheted fabrics (17.6Z) | Spinners, weavers, knitters, dyers and related workers not elsewhere classified (7–59†) | |||||
| Manufacture of knitted and crocheted hosiery (17.7A) | ||||||
| Manufacture of knitted and crocheted pullovers, cardigans and similar articles (17.7C) | ||||||
| Medical/veterinary/research sectors | ||||||
| Veterinary clinics | 1 | 3 | - | - | ||
| 2.9 (±2.1) | Veterinary activities (85.2Z) | Veterinarians (0–65†) | ||||
| Veterinary assistants (0–66†) | ||||||
| Practical aid (veterinary) (5–99.60) | ||||||
| Dental offices | 6 | 5 | 2.73 | (0.65–11.04) | ||
| 4.1 (±3.3) | Dental practice activities (85.1E) | Dentists (0–63†) | ||||
| Dental assistants (0–64†) | ||||||
| Nursing aids (5–99.40) | ||||||
| Other industries | ||||||
| Cigarette/cigar manufacture | 4 | - | - | - | ||
| 29 (±3.5) | Manufacture of tobacco products (16.0*) | Tobacco preparers and tobacco product makers (7–8†) | ||||
| Paper factory | 18 | 17 | 1.13 | (0.46–2.78) | ||
| 69 (±7) | Manufacture of pulp, paper and paper products (21*) | Paper pulp preparers(7–33†) | ||||
| Paper makers (7–34†) | ||||||
| Paper and paperboard products makers (9–1†) | ||||||
*All four-digit codes within that code were considered.
†all five-digit codes within that code were considered.
‡Concentrations of airborne endotoxins expressed as endotoxins units (EU)/m3.
§OR adjusted for age at interview, department, sex, Comprehensive Smoking Index (CSI), number of job periods, education and occupational exposure to asbestos. The never exposed to endotoxins are always the reference group.
¶Never means having no job in work environment group potentially exposed to endotoxins.
**Ever means having held at least one job in work environment group potentially exposed to endotoxins.
††Subjects, having declared a number of heads higher than the median for the specific questionnaire, were also included.
ISCO: International Standard Classification of Occupations; NAF: Nomenclature d'Activités Françaises.
Table 3 illustrates the analysis of lung cancer risk according to several characteristics of each subject’s endotoxin exposure. The finding of an overall inverse association between endotoxin exposure and lung cancer was corroborated by the statistically significant trends with duration and cumulative exposure. In detail, exposure periods longer than 14 years decreased lung cancer risk by >40%, while the quartile of subjects with the highest cumulative exposure had an almost 60% decrease. The risk was also significantly decreased in the workers who were exposed to endotoxins until 21 years before interview.
Table 3.
Lung cancer risk associated with exposure to endotoxins
| Work environment group* | |||||||||||||||
| Total exposed to endotoxins | Weakly exposed† | Highly exposed ‡ | |||||||||||||
| Cases | Controls | OR§ | 95% Cl | ptrend | Cases | Controls | OR§ | 95% Cl | ptrend | Cases | Controls | OR§ | 95% Cl | ptrend | |
| N | N | N | N | N | N | ||||||||||
| Exposure to endotoxins | |||||||||||||||
| Never¶ | 2461 | 2895 | 1.00 | Reference | 2461 | 2895 | 1.00 | Reference | 2461 | 2895 | 1.00 | Reference | |||
| Ever** | 465 | 660 | 0.8 | (0.66 to 0.95) | 306 | 310 | 1.09 | (0.87 to 1.36) | 151 | 336 | 0.51 | (0.4 to 0.67) | |||
| Duration of exposure (years) | |||||||||||||||
| ≤6 | 179 | 185 | 1.03 | (0.78 to 1.36) | 129 | 120 | 1.24 | (0.9 to 1.73) | 50 | 64 | 0.66 | (0.41 to 1.08) | |||
| >6–14 | 111 | 150 | 0.97 | (0.7 to 1.34) | 72 | 67 | 1.35 | (0.87 to 2.09) | 33 | 80 | 0.6 | (0.36 to 0.99) | |||
| >14–34 | 86 | 160 | 0.58 | (0.41 to 0.81) | 58 | 79 | 0.67 | (0.43 to 1.04) | 27 | 77 | 0.45 | (0.25 to 0.81) | |||
| >34 | 85 | 165 | 0.57 | (0.4 to 0.82) | 0.0002 | 44 | 44 | 1.01 | (0.57 to 1.80) | 40 | 115 | 0.41 | (0.25 to 0.68) | <0.0001 | |
| Missing | 4 | 3 | 1 | ||||||||||||
| Cumulative exposure (UE*years)†† | |||||||||||||||
| Quartile 1 | 169 | 165 | 1.23 | (0.92 to 1.63) | 81 | 84 | 1.11 | (0.75 to 1.66) | 51 | 87 | 0.55 | (0.35 to 0.88) | |||
| Quartile 2 | 148 | 168 | 0.85 | (0.63 to 1.14) | 75 | 71 | 1.17 | (0.77 to 1.76) | 43 | 79 | 0.82 | (0.51 to 1.34) | |||
| Quartile 3 | 87 | 162 | 0.63 | (0.44 to 0.90) | 81 | 78 | 1.19 | (0.78 to 1.81) | 29 | 85 | 0.42 | (0.24 to 0.72) | |||
| Quartile 4 | 57 | 164 | 0.42 | (0.28 to 0.63) | 0.01 | 66 | 77 | 0.81 | (0.51 to 1.27) | 0.87 | 27 | 84 | 0.37 | (0.21 to 0.65) | <0.0001 |
| Missing | 4 | 1 | 3 | 1 | 1 | ||||||||||
| Time since cessation of exposure (years) | |||||||||||||||
| ≤5 | 72 | 172 | 0.6 | (0.41 to 0.86) | 46 | 71 | 0.81 | (0.51 to 1.31) | 25 | 98 | 0.38 | (0.21 to 0.69) | |||
| >5–21 | 100 | 162 | 0.7 | (0.51 to 0.99) | 66 | 78 | 0.98 | (0.63 to 1.52) | 33 | 77 | 0.47 | (0.27 to 0.82) | |||
| >21–39 | 148 | 167 | 0.91 | (0.67 to 1.22) | 106 | 99 | 1.1 | (0.76 to 1.58) | 39 | 66 | 0.62 | (0.37 to 1.04) | |||
| >39 | 142 | 159 | 0.95 | (0.69 to 1.3) | 0.18 | 86 | 62 | 1.4 | (0.91 to 2.15) | 0.2 | 53 | 95 | 0.61 | (0.38 to 0.94) | |
| Missing | 3 | 2 | 1 | 0.0002 | |||||||||||
*Work environment groups were classified into those weakly and highly exposed to endotoxins with a threshold of 1000 UE/m3; 22 subjects had both low and high endotoxin exposure jobs and were excluded from the stratified analysis.
†Weakly exposed group included cultivation, agri-transformation/agri-food excluding grain transport, waste collection and treatment, sawmills, wool industry, medical/veterinary/research sectors, cigarette/cigar manufacture and paper factory.
‡Highly exposed group included dairy farms, cattle, poultry, pigs, work with grains and transport and cotton industry. §OR adjusted for age at interview, department, sex, Comprehensive Smoking Index (CSI), number of job periods, education and occupational exposure to asbestos. The never exposed to endotoxins are always the reference group.
¶Never means having no job in work environment group potentially exposed to endotoxin.,
**Ever means having held at least one job in work environment group potentially exposed to endotoxins.
††Cumulative exposure was transformed into qualitative variables according to quartiles of distribution among controls in each group: quartile 1 ([0–1012]; [0–380]; [4602–12560]); quartile 2 ([1012–7670]; [380–940]; [12560–40820]); quartile 3 ([7670–58090]; [940–2874]; [40820–87920)); quartile4 (>58090; >2874; >87 920) UE* years, respectively, for total, weakly and highly exposed to endotoxins.
Subjects were then divided into those weakly (n=306/310 cases/controls) and highly (n=151/336 cases/controls) exposed to endotoxins. The two subgroups differed also in their mean exposure duration, which for cases and controls was 15 years (SD 14.33) and 23 years (SD 18.17), respectively. No statistically significant association could be demonstrated among those weakly exposed, where most ORs were around unity, but the risk appeared to be reduced by 20% among those workers exposed until recently and in those with the strongest cumulative exposure. On the other hand, all the associations reported above for the whole population were reinforced in the subjects who had high occupational exposure to endotoxins. The risk for subjects ever-exposed was halved compared with those never exposed, the trends for duration and cumulative exposure index were reinforced, and the risk was significantly reduced even after a few years of exposure, in the lowest quartile of cumulative exposure and after the longest interval from cessation.
Figure 1 shows the spline charts obtained for duration of exposure and for time since last exposure, where the ORs are plotted against time, with the reference value fixed at 0 years. In Figure 1a, the curve of the weakly exposed subjects shows a steep increase during the first few years, followed by a linear decrease, so that ORs become lower than 1.0 between 20 and 30 years of exposure and continue to decline thereafter. The curve of the strongly exposed workers exhibits instead a continuous descending risk of lung cancer, steeply decreasing to half risk around 10 years and then decreasing more smoothly. Figure 1b shows that cessation of exposure led to a progressive and linear reduction of the endotoxin effect, irrespective of the level of exposure. The two curves are almost parallel, although that of the highly exposed workers starts well below unity and crosses the line corresponding to OR=1.0 only 50 years from the last exposure, while that of the weakly exposed subjects always remains in the area of positive association.
Figure 1.
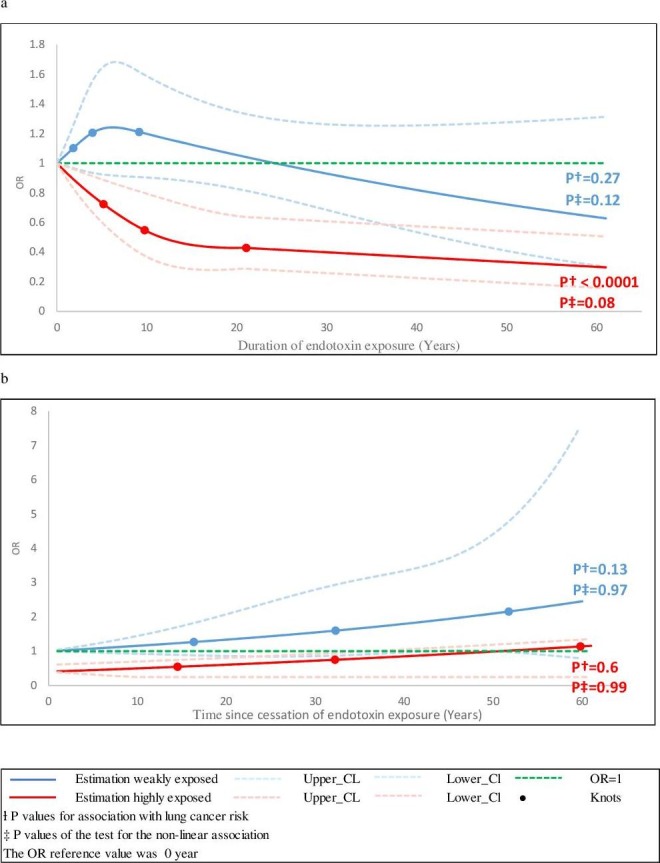
(A) Spline graphs showing the association between lung cancer risk and duration of exposure to endotoxins; (B) Spline graphs showing the association between lung cancer risk and time since cessation of exposure to endotoxins.
The analyses were then stratified by smoking status (table 4). Subjects ever exposed to endotoxins who were light or never smokers had their risk of lung cancer reduced by one-third, which was statistically significant in comparison with non-exposed workers. On the other hand, the subgroup of heavy smokers appeared to be less sensitive to the effect of endotoxin exposure, with OR only slightly reduced. The interaction between endotoxin exposure and cigarette smoking was statistically significant. In detail, for never/light smokers ORs were lower than unity (statistically significant) for the pairs of quartiles with the longest duration, strongest cumulative exposure or more recent exposure, and definitely low for the extreme quartiles (OR=0.26, 0.14 and 0.28, respectively). All interactions were strongly statistically significant.
Table 4.
Association between lung cancer and exposure to endotoxins by smoking status
| Never/light smokers* | Heavy smokers† | ||||||||
| Cases | Controls | OR‡ | 95% Cl | Cases | Controls | OR‡ | 95% Cl | p-Value Interaction§ | |
| N | N | N | N | ||||||
| Exposure to endotoxins | |||||||||
| Never¶ | 559 | 2090 | 1.00 | Reference | 1873 | 797 | 1.00 | Reference | |
| Ever** | 92 | 505 | 0.64 | (0.49 to 0.85) | 373 | 152 | 0.87 | (0.7 to 1.1) | 0.01 |
| Duration of exposure (years) | |||||||||
| ≤6 | 37 | 129 | 1.13 | (0.75 to 1.7) | 142 | 56 | 0.96 | (0.67 to 1.36) | |
| 6–14) | 24 | 119 | 0.72 | (0.44 to 1.20) | 87 | 30 | 1.15 | (0.73 to 1.80) | |
| >14–34 | 17 | 116 | 0.53 | (0.30 to 0.96) | 69 | 42 | 0.62 | (0.40 to 0.95) | |
| >34 | 13 | 141 | 0.26 | (0.14 to 0.51) | 72 | 24 | 0.81 | (0.48 to 1.33) | |
| Missing | 1 | 3 | 0.01 | ||||||
| Cumulative exposure (UE*years)¶ | |||||||||
| Quartile 1 | 43 | 109 | 1.66 | (1.1 to 2.5) | 126 | 56 | 0.97 | (0.68 to 1.38) | |
| Quartile 2 | 19 | 125 | 0.6 | (0.34 to 1.01) | 129 | 42 | 1.03 | (0.7 to 1.52) | |
| Quartile 3 | 21 | 128 | 0.57 | (0.34 to 0.95) | 66 | 33 | 0.61 | (0.38 to 0.98) | |
| Quartile 4 | 8 | 143 | 0.14 | (0.06 to 0.32) | 49 | 20 | 0.8 | (0.45 to 1.4) | |
| Missing | 1 | 3 | 1 | 0.0003 | |||||
| Time since cessation of exposure (years) | |||||||||
| ≤5 | 10 | 143 | 0.28 | (0.14 to 0.57) | 62 | 29 | 0.88 | (0.54 to 1.43) | |
| >5–21 | 18 | 127 | 0.42 | (0.23 to 0.75) | 82 | 32 | 0.92 | (0.59 to 1.44) | |
| >21–39 | 27 | 112 | 1.02 | (0.64 to 1.62) | 121 | 55 | 0.9 | (0.62 to 1.29) | |
| >39 | 36 | 123 | 0.93 | (0.6 to 1.43) | 106 | 36 | 0.81 | (0.53 to 1.24) | |
| Missing | 1 | 2 | 0.007 | ||||||
| p value§=0.007 | |||||||||
*Never/light smokers were subjects with Cumulative Smoking Index (CSI)≤1.
†Heavy smokers were subjects with CSI>1
‡OR adjusted for age at interview, department, sex, number of job periods, education and occupational exposure to asbestos. The never exposed to endotoxins are always the reference group.
§p Value for interaction between endotoxins and smoking status (using the likelihood ratio test).
¶Never means having no job in work environment group potentially exposed to endotoxins.
**Ever means having held at least one job in work environment group potentially exposed to endotoxins.
Analyses by histological subtype of lung cancer showed that the strongest inverse association with endotoxin exposure was with adenocarcinoma (one-third less; see online supplementary table 1). In the highly exposed the risk was decreased by almost two-thirds for adenocarcinoma, and by about 40% in the case of squamous cell and small cell lung cancer (fully or borderline statistically significant).
oemed-2016-104117supp001.pdf (302.9KB, pdf)
The inverse association between occupational exposure to endotoxins and lung cancer risk seemed to be more pronounced among subjects with a history of asthma (see online supplementary table 2). A slight decreased risk was suggested in the weakly exposed and was more definite among those who underwent high exposure, who showed borderline statistical significance in the small subgroup that had a history of asthma (OR=0.22). No interaction was demonstrated.
Discussion
This large population-based case–control study investigated in detail the association between lung cancer risk and occupational exposure to endotoxins. It attributed a definite level of endotoxin exposure to each job held by the subjects. Our results confirmed the presence of a decreased risk of lung cancer among workers exposed to endotoxins. A slight decreased risk in weak exposures was suggested for the first time, in addition to the strong association that was seen, as expected, among those highly exposed (particularly in livestock farms). Dose–response trends were shown with duration and cumulative exposure to endotoxins, while the inverse association diminished over time after cessation of exposure.
Our results are consistent with previous publications, particularly for workers in the livestock sector. Three meta-analyses on occupational exposures in agriculture found relative risks of lung cancer significantly reduced by one-third or more among farmers.23 24 However, the SYNERGY pooled analysis found slightly increased risks in association with occupational exposure to organic dust, endotoxins, or contact with animals or animal products, although high heterogeneity existed between studies.25
We classified the exposures to endotoxins as high or low according to the INRS guidelines.20 Among the highly exposed, we found a stronger inverse association with lung cancer risk for dairy farmers than for cattle, poultry and pig farmers, while non-significantly lowered ORs were seen in the small groups of workers in the grain sector. Similarly, lower lung cancer risks have been shown among dairy farmers in comparison with sheep or pig farmers and grain producers.15 26 The risk tended to decrease as the farm size and the number of livestock augmented, and was increased in farmers who switched from dairy to crop.
On the other hand, no association with lung cancer risk was found in our small group of cotton textile workers. This result was rather unexpected, as the majority of epidemiological studies on the textile industry suggest a reduced risk of lung cancer in this work environment,6 with few exceptions.27 However, most published studies have been conducted on unspecified ‘textile workers’, and the meta-analysis by Lenters et al found a statistically decreased risk specifically among cotton textile workers (with substantial heterogeneity between studies).6
A slight but suggestive association was found between low endotoxin exposure and lung cancer risk. In detail, we found that the risk was halved in association with waste collection and treatment (statistically significant). Similarly, a reduced rate of deaths from lung cancer has been reported in municipal waste workers.28
In the group of subjects with low exposure to endotoxins, the most common work environments were plant cultivation, meat production, sawmills and bakeries. The sector of plant cultivation was generally included in crop farming in the above-mentioned articles. Most epidemiological studies of lung cancer in meat workers provide evidence of a positive association between exposure to meat aerosols and lung cancer, as suggested by our data.29 Association between the wood industry and lung cancer is still a source of debate, and a recent meta-analysis was inconclusive.30 The possibility of residual confounding by wood dust exposure cannot be ruled out in our analyses; however, additional adjustments for this factor and for industries and occupations known (list A) or suspected (list B) to be associated with lung cancer risk did not substantially change our results (not shown). Studies on bakers and baking-related occupations did not suggest any significant association with lung cancer risk.31
Different strains of Gram-negative bacteria are found in different environments, and this might affect the observed associations. For example, Enterobacter agglomerans is predominant in the poultry industry, whereas Escherichia coli, Proteus and Acinetobacter spp are common in the agriculture sector.7 32
No study on the association with lung cancer has been conducted to date which directly measures endotoxin exposure obtained by personal or environmental sampling. On the other hand, few studies have attempted qualitative or quantitative estimates of duration or intensity of the exposure, and most of them argue in favour of the existence of a dose–effect relationship.
Our results suggest that lung cancer risk is reduced with increasing duration of exposure to endotoxins. Most studies carrying out similar investigations found similar results,2 14 33 with a few exceptions.3 34
Results based on proxies of intensity of exposure also seem to converge towards a dose-dependent effect. In a cohort study on agriculture workers, it was observed that lung cancer risk was reduced with increasing number of livestock and with raising poultry,35 similar to the results already mentioned for dairy farmers.15
A few studies have tried to set up job exposure matrices but their conclusions are contradictory. A protective role of endotoxins has been demonstrated in a cohort of cotton industry workers, with an effect dependent on the cumulative dose.36 However, other research, including the pooled analysis of case–control studies conducted in the framework of the SYNERGY project, found a procarcinogenic association with cumulative exposure to endotoxins.25 27
High exposure to endotoxins seems to be decreasingly but significantly associated with lung cancer over time, even decades after cessation, but the slight decrease of risk stopped earlier in the low exposure group. Two studies suggested that the effect of endotoxin could be attenuated after cessation of exposure, and hypothesised that there is involvement of some form of immunological memory, as endotoxins do not bioaccumulate.33 37 Another study found that the protective role of endotoxins was persistent after 10 years of cessation of exposure.36
The large number of subjects in our study allowed us to investigate the association between endotoxin exposure and lung cancer by subgroups. Thus, it was possible to stratify by smoking status, which has never been explored in detail previously. A strong inverse association of endotoxin exposure and lung cancer was found among light or never smokers, while it was almost completely masked by heavy smoking habits. Endotoxins seemed to modify the impact of carcinogenic substances (daily use of diesel tractors) similarly, in a recent cohort study.38
We have no clear explanation for our result, but an involvement of gene–environment interactions might be hypothesised, at the risk of some speculation, based on findings in the literature. For example, CD14 is a co-receptor of endotoxins that plays an important role in the regulation of inflammatory response to these molecules. A single nucleotide polymorphism of CD14 has been shown to be associated differently with respiratory function in light and heavy smokers.39
We also carried out for the first time a detailed analysis by lung cancer histology. Pronounced inverse associations were shown, mainly in the subgroup with high exposure to endotoxins, particularly with adenocarcinoma, similar to the above-mentioned study on diesel use.38
In our data, the inverse association between occupational exposure to endotoxins and lung cancer was stronger among subjects with a history of asthma, for workers both weakly and highly exposed. Reduced lung cancer risk in subjects with asthma might be the result of lifestyle changes related to the presence of the disease, particularly as regards tobacco smoke.40 Indeed, we verified that in our analysis 70% of subjects who had a history of asthma were never or light smokers. However, only a few subjects had a history of asthma and our results should be interpreted with caution.
Strengths and limitations
ICARE is one of the largest multicentre population-based case–control studies on occupational risk factors for lung cancer ever conducted. Incident cases were identified in collaboration with the French network of cancer registries, which allowed us to recruit virtually all lung cancer cases in the departments covered. Furthermore, the 11 departments included in the study comprised a considerable fraction of the French population (13%), providing a broad view on a variety of situations with endotoxin exposure.
To our knowledge, this is the first report that scans a wide range of industries and environments exposed to endotoxins. Work environments were first identified by cross referencing two coding systems: one for the tasks and duties undertaken in each job (ISCO codes) and one for the activity sectors (NAF codes). An exposure level was attributed thereafter to each work environment, based on a thorough review of the measurements reported in the literature. These stringent criteria helped us to minimise misclassification bias, although they might have reduced the number of exposed subjects in some cases.
Reduced risk has been attributed to residual confounding by smoking in some studies on endotoxin exposure.41 In our study, the three most important components of smoking history were incorporated in the CSI, a comprehensive and well-validated index.21 In addition, the large number of subjects allowed us to stratify in order to carefully evaluate the interactions with smoking.
We could stratify also according to a history of asthma. As this was a case–control study, where data were collected retrospectively, it is possible that cases declared their history of respiratory diseases more accurately than controls. However, subjects were interviewed using a standardised questionnaire not focusing only on their respiratory history, thus minimising any difference among cases and controls in the probability of reporting errors. In addition, although the term ‘asthma’ is not ambiguous, we preferred to exclude from our analysis those subjects who reported a double respiratory history of asthma and chronic bronchitis, as they might represent special situations that could affect our results.
Our study had some potential limitations. Misclassification may occur when retrospectively assessing occupational exposures. The coders were blind to the case–control status of the subjects, so reducing the possibility of differential misclassification that could result in an average bias towards the null. Our study did not have specific endotoxin measurements for each subject and for each sector. Furthermore, we considered that endotoxin exposure doses were stable, although variability according to season and among study subjects even within the same industry and in the same task has often been reported. The relatively recent development of endotoxin measurement techniques should encourage their inclusion in the protocol of future epidemiological studies.9
In conclusion, we provide evidence that occupational exposure to endotoxins reduces the incidence of lung cancer, particularly, but not exclusively, in subjects with high exposure levels and in never/light smokers. A dose–response trend has been demonstrated, and the effect diminished over time after exposure removal. Nevertheless, further investigations are necessary to replicate these results in a larger population. More research into the mechanisms of activity of endotoxin could also provide useful information for lung cancer prevention and treatment strategies.
Acknowledgments
The ICARE Study was supported by Agence Nationale de Sécurité Sanitaire, de l’alimentation, de l’environnement et du travail (ANSES); Fondation de France; Agence Nationale de la Recherche (ANR); Institut National du Cancer (INCA); Fondation pour la Recherche Médicale (FRM); Institut national de Veille Sanitaire (InVS); Direction Générale de la Santé (DGS); Fondation ARC pour la Recherche sur le Cancer; Direction Générale du Travail rattachée au Ministère du travail, de l’emploi, de la formation professionnelle et du dialogue social (DGT).
Footnotes
Contributors: IS and DL are the co-principal investigators of the ICARE (Investigation of occupational and environmental CAuses of REspiratory cancers) Study. They designed the study, directed its implementation and oversaw all aspects of the study, including recruitment of patients and controls, funding and quality control of data. SBK carried out the statistical analyses, interpreted the results and wrote the manuscript. MN participated in writing the manuscript.
FG contributed to the statistical analysis and interpretation of the results. SC and MS managed the data, and prepared datasets for statistical analyses. MM and GM conceived the variables included in the analysis and the strategy of the analysis. FM is responsible for a cancer registry and coded the histology of the lung cancer cases.
Funding: The ICARE Study was supported by Agence Nationale de Sécurité Sanitaire, de l’alimentation, del’environnement et du travail (ANSES); Fondation de France; Agence Nationale de la Recherche (ANR); Institut National du Cancer (INCA ; Fondation pour la Recherche Médicale (FRM); Institut National de Veille Sanitaire (InVS); Direction Générale de la Santé (DGS); Fondation ARC pour la Recherche sur le Cancer; Direction Générale du Travail rattachée au Ministère du travail, de l’emploi, de la formation professionnelle et du dialogue social (DGT). MN was partially supported by the University of Genoa, Genoa, Italy. This work was funded by la Fondation de France.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The international review board of the French National Institute of Health and Medical Research (IRB-INSERM, n 01-036) and by the French Data Protection Authority (CNIL n90120)
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: Members of ICARE Study Group : Registre des cancers du Calvados, France (Anne-Valérie Guizard); Registre des cancers du Doubs et du Territoire de Belfort, France (Arlette Danzon, Anne-Sophie Woronoff); Registre des cancers du Bas-Rhin, France (Velten Michel); Registre des cancers du Haut-Rhin, France (Antoine Buemi, Émilie Marrer); Registre des cancers de l’Hérault, France (Brigitte Tretarre); Registre des cancers de l’Isère, France (Marc Colonna, Patricia Delafosse); Registre des cancers de Loire-Atlantique-Vendée, France (Paolo Bercelli, Florence Molinie); Registre des cancers de la Manche, France (Simona Bara); Registre des cancers de la Somme, France (Benedicte Lapotre-Ledoux, Nicole Raverdy); Inserm, Centre for research in Epidemiology and Population Health (CESP), U1018, Environmental Epidemiology of Cancer Team, F-94807, Villejuif, France (Oumar Gaye, Farida Lamkarkach).
References
- 1. Malhotra J, Malvezzi M, Negri E, et al. . Risk factors for lung cancer worldwide. Eur Respir J 2016;48:889–902. 10.1183/13993003.00359-2016 [DOI] [PubMed] [Google Scholar]
- 2. Henderson V, Enterline PE. An unusual mortality experience in cotton textile workers. J Occup Med 1973;15:717–9. [PubMed] [Google Scholar]
- 3. Levin LI, Gao YT, Blot WJ, et al. . Decreased risk of lung cancer in the cotton textile industry of Shanghai. Cancer Res 1987;47:5777–81. [PubMed] [Google Scholar]
- 4. Lange JH. Reduced cancer rates in agricultural workers: a benefit of environmental and occupational endotoxin exposure. Med Hypotheses 2000;55:383–5. 10.1054/mehy.2000.1072 [DOI] [PubMed] [Google Scholar]
- 5. Enterline PE, Sykora JL, Keleti G, et al. . Cotton dust and cancer. Lancet 1985;2:934–5. [DOI] [PubMed] [Google Scholar]
- 6. Lenters V, Basinas I, Beane-Freeman L, et al. . Endotoxin exposure and lung cancer risk: a systematic review and meta-analysis of the published literature on agriculture and cotton textile workers. Cancer Causes Control 2010;21:523–55. 10.1007/s10552-009-9483-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chaby R. TEC DOC, Des endotoxines aux lipoplysaccharides Structures, activités et effets physiologiques: Lavoisier, 2010. [Google Scholar]
- 8. Liebers V, Brüning T, Raulf-Heimsoth M. Occupational endotoxin-exposure and possible health effects on humans. Am J Ind Med 2006;49:474–91. 10.1002/ajim.20310 [DOI] [PubMed] [Google Scholar]
- 9. Duquenne P, Marchand G, Duchaine C. Measurement of endotoxins in bioaerosols at workplace: a critical review of literature and a standardization issue. Ann Occup Hyg 2013;57:137–72. 10.1093/annhyg/mes051 [DOI] [PubMed] [Google Scholar]
- 10. Williams LK, Ownby DR, Maliarik MJ, et al. . The role of endotoxin and its receptors in allergic disease. Ann Allergy Asthma Immunol 2005;94:323–32. 10.1016/S1081-1206(10)60983-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Smit LA, Wouters IM, Hobo MM, et al. . Agricultural seed dust as a potential cause of organic dust toxic syndrome. Occup Environ Med 2006;63:59–67. 10.1136/oem.2005.021527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riedler J, Braun-Fahrländer C, Eder W, et al. . Exposure to farming in early life and development of asthma and allergy: a cross-sectional survey. Lancet 2001;358:1129–33. 10.1016/S0140-6736(01)06252-3 [DOI] [PubMed] [Google Scholar]
- 13. Astrakianakis G, Seixas NS, Ray R, et al. . Lung cancer risk among female textile workers exposed to endotoxin. J Natl Cancer Inst 2007;99:357–64. 10.1093/jnci/djk063 [DOI] [PubMed] [Google Scholar]
- 14. Kuzmickiene I, Stukonis M. Lung cancer risk among textile workers in Lithuania. J Occup Med Toxicol 2007;2:14. 10.1186/1745-6673-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mastrangelo G, Marzia V, Marcer G. Reduced lung cancer mortality in dairy farmers: is endotoxin exposure the key factor? Am J Ind Med 1996;30:601–9. [DOI] [PubMed] [Google Scholar]
- 16. Rosenberger A, Bickeböller H, McCormack V, et al. . Asthma and lung cancer risk: a systematic investigation by the International Lung Cancer Consortium. Carcinogenesis 2012;33:587–97. 10.1093/carcin/bgr307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Luce D, Stücker I; ICARE Study Group. Investigation of occupational and environmental causes of respiratory cancers (ICARE): a multicenter, population-based case-control study in France. BMC Public Health 2011;11:928 10.1186/1471-2458-11-928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. INSEE. National institute for statistics and economic studies. Nomenclature d'activités Françaises. Paris, France: , 2000. [Google Scholar]
- 19. The International Labour Office. International standard classification of occupations. Geneva, Switzerland 1968. [Google Scholar]
- 20. Isabelle Balty NB, David C, Burzoni S, et al. . Valeurs guides endotoxines. Interprétation des résultats de métrologie des bioaérosols. Hygiène et Sécurité du Travail 2015. [Google Scholar]
- 21. Leffondré K, Abrahamowicz M, Xiao Y, et al. . Modelling smoking history using a comprehensive smoking index: application to lung cancer. Stat Med 2006;25:4132–46. 10.1002/sim.2680 [DOI] [PubMed] [Google Scholar]
- 22. Guida F, Paget-Bailly S, Lamkarkach F, et al. . Risk of lung cancer associated with occupational exposure to mineral wools: updating knowledge from a French population-based case-control study, the ICARE study. J Occup Environ Med 2013;55:786–95. 10.1097/JOM.0b013e318289ee8b [DOI] [PubMed] [Google Scholar]
- 23. Davis DL, Blair A, Hoel DG. Agricultural exposures and cancer trends in developed countries. Environ Health Perspect 1993;100 39–44. 10.1289/ehp.9310039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Acquavella J, Olsen G, Cole P, et al. . Cancer among farmers: a meta-analysis. Ann Epidemiol 1998;8:64–74. 10.1016/S1047-2797(97)00120-8 [DOI] [PubMed] [Google Scholar]
- 25. Peters S, Kromhout H, Olsson AC, et al. . Occupational exposure to organic dust increases lung cancer risk in the general population. Thorax 2012;67:111–6. 10.1136/thoraxjnl-2011-200716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Laakkonen A, Pukkala E. Cancer incidence among Finnish farmers, 1995-2005. Scand J Work Environ Health 2008;34:73–9. 10.5271/sjweh.1167 [DOI] [PubMed] [Google Scholar]
- 27. Checkoway H, Lundin JI, Costello S, et al. . Possible pro-carcinogenic association of endotoxin on lung cancer among Shanghai women textile workers. Br J Cancer 2014;111:603–7. 10.1038/bjc.2014.308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rapiti E, Sperati A, Fano V, et al. . Mortality among workers at municipal waste incinerators in Rome: a retrospective cohort study. Am J Ind Med 1997;31:659–61. [DOI] [PubMed] [Google Scholar]
- 29. Johnson ES, Choi KM. Lung cancer risk in workers in the meat and poultry industries--a review. Zoonoses Public Health 2012;59:303–13. 10.1111/j.1863-2378.2012.01459.x [DOI] [PubMed] [Google Scholar]
- 30. Hancock DG, Langley ME, Chia KL, et al. . Wood dust exposure and lung cancer risk: a meta-analysis. Occup Environ Med 2015;72:889–98. 10.1136/oemed-2014-102722 [DOI] [PubMed] [Google Scholar]
- 31. Behrens T, Kendzia B, Treppmann T, et al. . Lung cancer risk among bakers, pastry cooks and confectionary makers: the SYNERGY study. Occup Environ Med 2013;70:810–4. 10.1136/oemed-2013-101469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Guillam MT, Claude C, Dewitte JD, et al. . Aérocontaminants et morbidité chez les éleveurs de volailles. Archives des Maladies Professionnelles et de l'Environnement 2007;68:161–8. 10.1016/S1775-8785(07)88913-2 [DOI] [Google Scholar]
- 33. Mastrangelo G, Grange JM, Fadda E, et al. . Lung cancer risk: effect of dairy farming and the consequence of removing that occupational exposure. Am J Epidemiol 2005;161:1037–46. 10.1093/aje/kwi138 [DOI] [PubMed] [Google Scholar]
- 34. Pezzotto SM, Poletto L. Occupation and histopathology of lung cancer: a case-control study in Rosario, Argentina. Am J Ind Med 1999;36:437–43. [DOI] [PubMed] [Google Scholar]
- 35. Beane Freeman LE, Deroos AJ, Koutros S, et al. . Poultry and livestock exposure and cancer risk among farmers in the agricultural health study. Cancer Causes Control 2012;23:663–70. 10.1007/s10552-012-9921-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McElvenny DM, Hurley MA, Lenters V, et al. . Lung cancer mortality in a cohort of UK cotton workers: an extended follow-up. Br J Cancer 2011;105:1054–60. 10.1038/bjc.2011.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Applebaum KM, Ray RM, Astrakianakis G, et al. . Evidence of a paradoxical relationship between endotoxin and lung cancer after accounting for left truncation in a study of Chinese female textile workers. Occup Environ Med 2013;70:709–15. 10.1136/oemed-2012-101240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tual S, Silverman DT, Koutros S, et al. . Use of dieselized farm equipment and incident lung cancer: findings from the Agricultural Health Study Cohort. Environ Health Perspect 2016;124:611–8. 10.1289/ehp.1409238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhou H, Alexis NE, Almond M, et al. . Influence of C-159T SNP of the CD14 gene promoter on lung function in smokers. Respir Med 2009;103:1358–65. 10.1016/j.rmed.2009.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Koshiol J, Rotunno M, Consonni D, et al. . Chronic obstructive pulmonary disease and altered risk of lung cancer in a population-based case-control study. PLoS One 2009;4:e7380 10.1371/journal.pone.0007380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Blair A, Freeman LB. Epidemiologic studies in agricultural populations: observations and future directions. J Agromedicine 2009;14:125–31. 10.1080/10599240902779436 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
oemed-2016-104117supp001.pdf (302.9KB, pdf)


