Abstract
Background
Madagascar conducted the first two phases of a national free mass distribution campaign of long-lasting insecticidal nets (LLINs) during a political crisis in 2009 aiming to achieve coverage of two LLINs per household as part of the National Malaria Control Strategy. The campaign targeted households in 19 out of 91 total health districts.
Methods
A community-based cross-sectional household survey using a three-stage cluster sample design was conducted four months post campaign to assess LLIN ownership, access and use. Multivariable logistic regression analysis was used to identify factors associated with household LLIN access and individual LLIN use.
Results
A total of 2211 households were surveyed representing 8867 people. At least one LLIN was present in 93.5% (95% confidence interval [CI], 91.6–95.5%) of households and 74.8% (95% CI, 71.0–78.6%) owned at least two LLINs. Access measured as the proportion of the population that could potentially be covered by household-owned LLINs was 77.2% (77.2% (95% CI, 72.9–81.3%) and LLIN use by all individuals was 84.2% (95% CI, 81.2–87.2%). LLIN use was associated with knowledge of insecticide treated net use to prevent malaria (OR = 3.58, 95% CI, 1.85–6.94), household ownership of more LLINs (OR 2.82, 95% CI 1.85–4.3), presence of children under five (OR = 2.05, 95% CI, 1.67–2.51), having traveled to the distribution point and receiving information about hanging a bednet (OR = 1.56, 95% CI, 1.41–1.74), and having received a post-campaign visit by a community mobilizer (OR = 1.75, 95% CI, 1.26–2.43). Lower LLIN use was associated with increasing household size (OR = 0.81 95% CI 0.77–0.85) and number of sleeping spaces (OR = 0.55, 95% CI, 0.44–0.68).
Conclusions
A large scale free mass LLIN distribution campaign was feasible and effective at achieving high LLIN access and use in Madagascar. Campaign process indicators highlighted potential areas for strengthening implementation to optimize access and equity.
Introduction
The Global Malaria Action Plan calls for the rapid scale up of key malaria prevention interventions including widespread use of long-lasting insecticidal nets (LLINs) by people at risk for malaria since research has demonstrated their effectiveness in reducing all-cause malaria mortality and morbidity in young children [1, 2]. Monitoring and evaluation of LLIN distribution efforts is important to help determine the impact of LLINs and to inform optimal program implementation strategies within the national malaria control program (NMCP).
In Madagascar, malaria remains a leading cause of morbidity and mortality in children under five years of age. Achieving 80% LLIN coverage in children under five and pregnant women is one of the main targets of the NMCP [3]. Madagascar revised its malaria strategy to rapidly scale up malaria control activities as outlined in the 2008–2012 National Strategic Plan for Malaria Control in view of pre-elimination [3]. Revisions included prioritizing universal coverage with the objective of two LLINs per household to achieve maximum coverage and no longer targeting only pregnant women and children under five. Prior to the strategy revision, LLINs had been distributed when available: 1) free through sub-national integrated immunization campaigns targeting children under five and pregnant women, 2) through sale of highly subsidized LLINs (at approximately $1.50 per LLIN), and 3) through routine distribution during antenatal clinic visits and immunization visits for children under one year old. The combination of these methods contributed to an important increase in ownership of at least one LLIN per household (from 20.5% in 2004 to 79.8% in 2008) as well as an increase in reported LLIN usage among children the previous night (from 13.3% in 2004 to 69.1% in 2008) [4, 5]. However, the gap that remained to cover all households with two LLINs was sizeable; in 2008 the frequency of households owning at least two LLINs was only 27.2% in LLIN-targeted endemic zones [6].
Subsequently the local Madagascar Roll Back Malaria (RBM) partnership with the NMCP/Service de Lutte Contre le Paludisme, (NMCP/SLP) worked with donors to identify and secure resources to scale up to the nationally-defined coverage goal of two LLINs per household, and maintain target coverage levels through 2012. As a result of the staggered availability of funds and lead-time needed for procurement and delivery of LLINs, Madagascar planned a phased or “rolling” campaign. The overall LLIN campaign and associated goal of two LLINs per household was targeted to 91 of 111 health districts where malaria is endemic per Madagascar’s National Strategic Plan for Malaria Control 2008–2012. The remaining 20 health districts are highland districts with lower malaria transmission and different control strategies including indoor residual spraying (IRS) and epidemic surveillance [3].
Madagascar conducted the first two phases of a stand-alone mass free LLIN distribution campaign in 19 health districts on the East Coast, a geographic zone with an estimated population of 3.8 million, during November 16–22 (12 districts) and December 14–20, 2009 (7 districts). Community volunteers known as community “mobilizers” were recruited to visit each household prior to the campaign, and provided two LLIN vouchers per household, LLIN education, and information about the planned distribution dates and sites. LLINs were transported and distributed to the population free-of-cost at community-level distribution points in order to reach even the most remote areas. Household representatives were asked to bring their vouchers to the distribution point to exchange for two LLINs on a pre-planned distribution day. Over 1,730,000 LLINs were distributed. After the campaign, the community mobilizers were asked to visit households to deliver educational messages and encourage and assist hang-up of newly distributed LLINs. The campaign was led by the Madagascar Ministry of Health and Family Planning as a collaborative effort among the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM); Population Services International; UNICEF; the U.S. President’s Malaria Initiative; the International Federation of Red Cross and Red Crescent Societies; the Malagasy Red Cross; USAID; U.S. Centers for Disease Control and Prevention (CDC); World Health Organization; and others.
The distribution of LLINs through a community-level free mass distribution was expected to increase the national levels of LLIN ownership and usage in Madagascar by 2010. A household survey provided an opportunity to quickly assess coverage results and LLIN use after the early roll-out phases. The main objectives of the survey were to measure household LLIN coverage, access, and use in the 19 districts which were part of the first two phases of the universal coverage LLIN campaign.
Materials and methods
Location and timing of survey
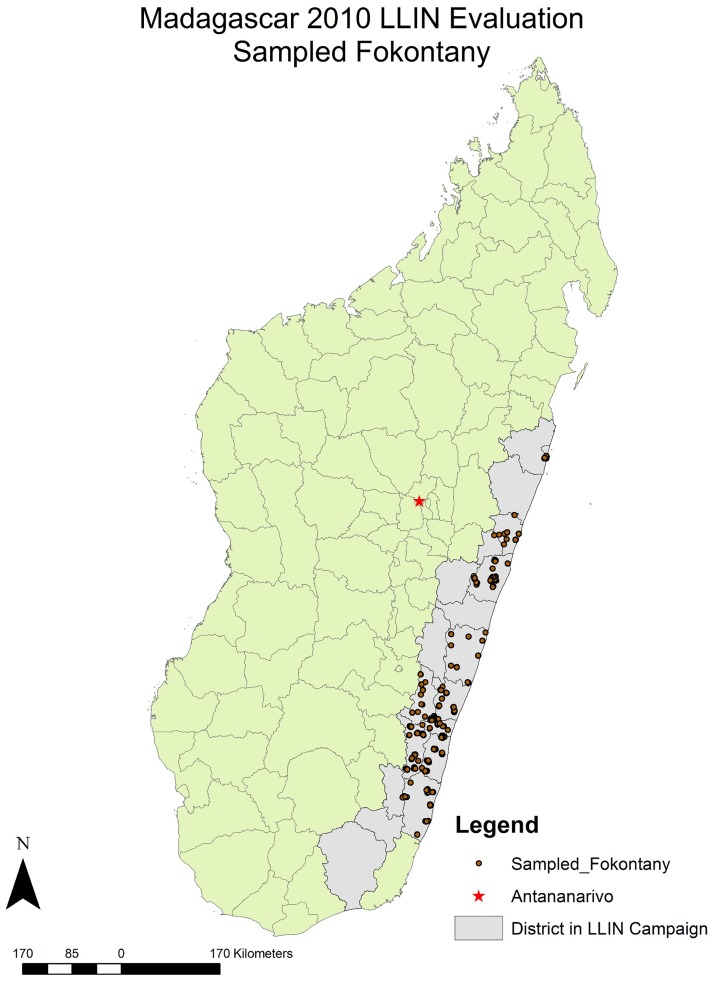
The community-based cross-sectional household survey took place between April and May 2010, during the end of the rainy season on the east coast of Madagascar. The survey was sub-national, focusing in 4 regions and 19 districts which were targeted in the first two phases of the mass free LLIN distribution campaign (Fig 1).
Fig 1. Map of Madagascar districts involved in the 2009 LLIN distribution campaign and sampled fokontany (villages) included in the evaluation.
Sampling and data collection
Three-stage cluster sampling was conducted. Ten districts were selected using probability proportional to population size (PPS) sampling. Population estimates were based on official district estimates extrapolated from the most recent national census in 1993 which estimated the population of Madagascar to be 19.7 million in 2008. Within each of the districts, 9 fokontany (villages) or enumeration areas were selected by PPS. All households within the selected enumeration areas were then mapped using personal digital assistant (PDA)-based GPS technology (custom software, CDC, Atlanta GA) and twenty-five households were selected for interviews by random sampling using the household listing created by the GPS mapping exercise [7].
Survey teams administered a detailed questionnaire to each household following a standard format similar to those used LLIN coverage surveys elsewhere [8–10]. Household members, bednets, and sleeping spaces were inventoried. Household-level questions focused on bednet ownership; type, quantity and quality of nets; net use and net hang up; campaign-specific process indicators such as: how many nets they received and retained as part of the mass campaign distribution; information, education and communication (IEC); household visits by community mobilizers; and whether they received a voucher. Demographic characteristics of household members and reported bednet use were collected. A household was defined as “all persons eating from the same food pot”, in line with the definition used in previous surveys in Madagascar.
Data analysis
Data from the Microsoft® Access database were transferred to Stata® version 10 (Stata Corporation, College Station, Texas, USA) and SAS version 9.3 (SAS Institute, Cary, NC) for verification, data management, and analysis. Specialized analysis survey procedures using Stata® (SVY procedure) or SAS (Proc Survey) were used to produce valid estimates and calculate standard errors to account for clustering at the primary sampling unit (district) level and sampling weights. Descriptive statistical analysis and Rao-Scott chi-square statistics were used for tests of association. Two multivariable logistic regression models were constructed to assess relationships between independent explanatory variables and key outcomes: 1) household LLIN ownership of at least one LLIN per two people, and 2) LLIN use the night preceding the survey by individuals (residing in households owning at least one LLIN), while controlling for confounding factors. For the household ownership model, in order to get the odds of each individual in a household having access to a LLIN, the outcome “access” was modeled using the single-trial specification syntax in SAS with one record corresponding to each person in the household and using binary coding for whether they had access to a LLIN based on the RBM goal of 1 net: 2 person ratio and the number of LLINs owned by the household. Pre-existing LLIN estimates were calculated by taking total LLINs per household at the time of the survey and subtracting the number of campaign LLINs received and present [10]. A map of Madagascar indicating districts included in the 2009 distribution campaign and the fokontany sampled in the evaluation was generated using ESRI (ArcGIS) software.
A section of the questionnaire addressed the overall economic status of housing and living quarters. These questions were adapted from the 2000 Multiple Indicator Cluster Survey and 2003–4 and 2008 Demographic and Health Surveys (DHS) and were used to develop a wealth index using principal components analysis [11]. Questions included type of materials used in construction of the housing dwelling, ownership of certain assets, and water sources. A wealth index score was calculated for each household and based on this score, households were assigned to one of five wealth quintiles from least wealthy (1) to most wealthy (5) using quintile cut-off points established for the 2008 DHS. Economic equity ratio was calculated as the ratio of proportion in the richest to the poorest wealth quintile.
For the purposes of this paper, net ownership and use results are presented for LLINs instead of the standard insecticide treated net (ITN) indicators because the difference between ITNs and LLINs in this setting was negligible (< 1%). The most recent RBM Monitoring and Evaluation Reference Group indicators were used to assess universal access to and utilization of LLINs: 1) the proportion of households with a sufficient number of LLINs to protect all individuals sleeping in the household assuming each LLIN is shared by two people, 2) the proportion of the population with access to a LLIN in the household (i.e., universal coverage defined as one LLIN per two people), and 3) the proportion of the population that slept under a LLIN the previous night.[12]
Ethical considerations
The evaluation protocol and questionnaire were reviewed by the Madagascar Ministry of Health Ethics Review Board and the CDC Ethical Review Committee. The evaluation was approved by both entities. There were no known risks involved with this evaluation and participation was voluntary with informed consent. Verbal consent was approved by Ethics boards and obtained prior to collecting survey data after explaining the objective of the study and types of questions the participants would be asked, the advantages of participating, confidentiality of responses and emphasizing the voluntary nature of participating. Verbal consent was documented using the PDA.
Results
Household characteristics
Among the 90 fokontany sampled, there were a total of 2239 households selected. Among these, 2211 (98.8%) were surveyed, including 54.3% from districts covered in the November campaign and 45.7% from districts covered in the December campaign. There were 1005 households with at least one child under the age of five and 240 households with at least one pregnant woman among household members (see Table 1). The average household size was 4.1 people (95% CI, 3.9–4.3 persons) and 41.6% of households were among the two poorest wealth quintiles. Selected household assets are listed in Table 1.
Table 1. Household, individual and bed net characteristics.
| Household Characteristics | Number | Weighted%* (95% CI†) |
|---|---|---|
| Households surveyed | 2211 | - |
| Households in districts participating in November 2009 campaign | 1536 | 54.3 (26.7–81.9) |
| Households in districts participating in December 2009 campaign | 675 | 45.7 (18.1–73.3) |
| Individuals living in surveyed household | 8867 | - |
| Average number of members per household | 4.1 | (3.9–4.3) |
| Range of household sizes | 1–18 | - |
| Households with children under 5 years old | 1005 | 44.0 (38.5–49.5) |
| Households with pregnant women (15–49 years old) | 240 | 9.6 (7.6–11.5) |
| Sleeping spaces inventoried | 3719 | - |
| Households by Wealth Quintile | ||
| 1 (poorest) | 433 | 17.5 (9.7–25.4) |
| 2 | 654 | 24.1 (14.9–33.2) |
| 3 | 546 | 20.4 (12.1–28.6) |
| 4 | 309 | 14.5 (12.4–16.6) |
| 5 (richest) | 269 | 23.5 (1.0–46.0) |
| Selected Household Assets | ||
| Type of roof | ||
| Thatch, palm or leaf | 1447 | 61.2 (42.3–80.2) |
| Rustic mat, palm/bamboo | 192 | 6.1 (3.5–8.8) |
| Sheet metal | 446 | 26.6 (9.1–44.2) |
| Type of wall | ||
| Bamboo/cane/palm | 1617 | 68.7 (55.0–82.5) |
| Wood planks | 251 | 15.3 (4.4–26.2) |
| Owns a | ||
| Radio | 924 | 48.0 (35.4–60.6) |
| TV | 239 | 20.6 (1.8–39.3) |
| Cell phone | 339 | 25.9 (4.1–47.7) |
| Bicycle | 306 | 21.5 (7.9–35.0) |
| Motorcycle | 64 | 5.1 (0.3–10.4) |
| Car | 20 | 1.8 (0.01–3.6) |
| Livestock or other animals | 1400 | 57.3 (46.0–70.0) |
| Malaria prevention activities cited by household | ||
| Sleeps under bed net | 1942 | 89.3 (85.4–93.2) |
| Keeps the environment clean | 325 | 20.7 (8.1–33.3) |
| Removes stagnant water around the house | 190 | 11.1 (3.9–18.4) |
| Closes the windows | 198 | 9.0 (7.2–10.9) |
| Burns herbs or dung | 218 | 8.2 (4.5–11.9) |
| Uses insecticide coils | 116 | 6.2 (3.0–9.4) |
| Covers with blankets or sheets at night | 200 | 7.8 (3.8–11.8) |
| Takes medication (nivaquine, etc.) | 13 | 0.4 (0.2–0.6) |
| Knowledge of advantages of using a LLIN‡ as cited by household | ||
| Protection against mosquitos | 1445 | 65.4 (60.5–70.1) |
| Peaceful sleep | 1101 | 49.7 (44.2–55.3) |
| Prevent malaria | 1384 | 62.6 (58.5–66.7) |
| Privacy | 39 | 1.8 (1.2–2.3) |
| Don’t know | 53 | 2.4 (1.5–3.3) |
| Individual Characteristics | ||
| Total individuals | 8867 | - |
| Male gender | 4228 | 47.2 (46.3–48.1) |
| Children < 5 years old | 1372 | 14.8 (12.9–16.6) |
| Women (15–49 years old, not pregnant) | 2012 | 23.6 (21.8–25.4) |
| Pregnant women (15–49 years old) | 243 | 2.4 (1.9–2.9) |
| Slept in the house the night before | 8716 | 98.4 (97.6–99.1) |
| Education Level | ||
| No formal education | 3240 | 33.5 (24.5–42.6) |
| Primary school | 4113 | 43.4 (38.0–48.8) |
| Middle school | 903 | 13.3 (7.2–19.4) |
| Secondary school | 339 | 5.9 (0.2–38.7) |
| Higher than secondary school | 110 | 2.0 (0.2–3.9) |
| Don’t know/not sure | 162 | 1.8 (1.2–2.4) |
| Slept in household the night prior to the survey | 8716 | 98.4 (97.6–99.1) |
| Average number of people per sleeping space | 3.4 | (3.3–3.5) |
| Range of number of people per sleeping space | 1–15 | - |
| Bed net Characteristics | ||
| Total bed nets inventoried (any bed net) | 4551 | - |
| LLINs | 4278 | 94.0 (92.2–95.7) |
| Proportion of existing LLINs used the previous night | 3078 | 73.8 (69.6–78.0) |
| Bed net hanging the night before the survey | 3183 | 72.0 (67.3–76.8) |
| Old bed nets, not hanging and no longer used for sleeping | 228 | 4.4 (2.8–6.0) |
| Old LLINs, not hanging and no longer used for sleeping | 140 | 3.0 (2.0–4.1) |
| Bed nets in usable condition | 4323 | 95.6 (94.0–97.2) |
| Ever-treated bed net (ITN§) | 4140 | 95.3 (93.8–96.9) |
| LLIN | 4138 | 95.3 (93.7–96.9) |
| Campaign net | 3540 | 77.7 (68.1–87.4) |
| Campaign LLIN | 3488 | 76.3 (67.3–85.3) |
| Source from campaign—free | 3363 | 74.9 (65.6–84.2) |
| Source from campaign–paid something | 177 | 2.8 (0.8–4.9) |
| Other source—free | 184 | 5.3 (3.4–7.1) |
| Other source–paid something | 599 | 17.0 (9.1–24.9) |
| New in good condition (no holes) | 3419 | 73.8 (69.5–78.0) |
| New still in original packaging | 353 | 8.1 (5.8–10.5) |
| Average number of bed nets per household | 2.1 | (2.0–2.2) |
| Range of bed nets per household | 1–8 | |
| Average number of sleepers per LLIN used | 2.6 | (2.4–2.7) |
| Range of sleepers per LLIN used | 1–10 | - |
*Adjusted for clustering and sampling weights
†Confidence Intervals (CI)
‡Long lasting insecticidal net (LLIN)
§Insecticide treated net (ITN)
When households were asked what their members do for protection against malaria, 89.3% cited sleeping under a bednet, 20.7% cited keeping the environment around their home clean, and 11.1% cited draining stagnant water. The most frequently reported advantages of using a LLIN were: protection against mosquitos (65.4%), protection against malaria (62.6%), and peaceful sleep (49.7%).
Individual characteristics
Among the 8867 persons living in the surveyed households, 4228 (47.2%) were male, 1372 (14.8%) were children under five years old, and 243 (2.4%) were pregnant women. Almost all individuals, 8716 (98.4%) reported sleeping in the house the night prior to the survey. The majority of individuals, 64.6%, had a primary school education or higher.
Bednet characteristics
There were a total of 4551 bednets inventoried and 3719 sleeping spaces counted among the households surveyed. There was an average of 2.1 bednets per household (95% CI, 2.0–2.2), ranging between 1–8 bednets per household. The average number of individuals sharing a sleeping space was 3.4 (95% CI, 3.3–3.5) ranging from 1 to 15 people.
Among the 4551 bednets, 4280 met the criteria of an ITN and the remaining 271 were identified as untreated nets. All of the ITNs were LLINs except two (4278, >99.9%). The overall number and proportion of LLINs that were reported to be used the previous night was 3078 or 73.8%. Among LLINs used, there was an average of 2.6 (95% CI, 2.4–2.7) people sleeping under the LLIN the previous night (Table 1). Households reported that 228 (4.4%) of the nets inventoried were no longer used for sleeping because they were perceived by users as too old, including 140 LLINs. Further details of net characteristics can be found in Table 1.
LLIN campaign
Progress towards bednet campaign coverage target of two LLINs per household
Campaign process indicators are summarized in Table 2. Only 70.1% (95% CI, 59.0–81.2%) of households reported receiving the campaign goal of at least two LLINs, and 11.1% of households reported that they did not receive any LLINs at all during the campaign. Results were fairly equitable across wealth quintiles. The top five reasons for not receiving a campaign net were: household members were absent during the distribution (28.1%), household members were not listed on the distribution census list (12.2%), no bednets were available (14.0%), household members did not have a voucher (14.2%), and household members did not possess an official identity card (4.6%).
Table 2. Campaign process indicators.
| Campaign Indicator | All Households, N = 2211 | |
|---|---|---|
| Number | Weighted %* (95% CI†) | |
| Number of nets that each HH‡ received from the campaign | ||
| Two or more nets | 1634 | 70.1 (59.0–81.2) |
| One net | 346 | 18.8 (9.6–28.0) |
| Zero nets | 231 | 11.0 (7.2–15.0) |
| HH received information about the campaign | 2019 | 91.8 (89.6–94.0) |
| HH received a pre-distribution visit by a mobilizer | 1494 | 66.1 (60.9–71.3) |
| HH received a voucher | 1823 | 84.2 (81.0–87.5) |
| Mobilizer explained how to use voucher | 1665 | 91.0 (86.9–95.1) |
| Number of vouchers received: | ||
| 1 voucher | 716 | 32.5 (28.3–36.8) |
| ≥2 vouchers | 1107 | 51.7 (45.7–57.7) |
| Did not receive a voucher | 361 | 14.9 (11.7–18.1) |
| Don’t know | 27 | 0.8 (0.6–11.6) |
| HH traveled to distribution point | 1918 | 86.9 (84.2–89.6) |
| Time to travel to distribution point: | ||
| Less than 30 minutes | 1197 | 68.2 (58.1–78.2) |
| Between 30 minutes and one hour | 333 | 16.2 (10.6–21.8) |
| One to two hours | 194 | 7.5 (4.3–10.7) |
| More than 2 hours | 130 | 5.4 (2.6–8.3) |
| Half a day | 40 | 1.6 (0.6–2.7) |
| One day | 16 | 0.8 (0.0–1.6) |
| More than one day | 1 | 0.02 (0.0–0.1) |
| Don’t know | 7 | 0.2 (0.0–0.5) |
| Type of information messages received at distribution point | ||
| How to hang the net | 870 | 40.9 (26.3–55.5) |
| How to wash/take care of the net | 896 | 42.3 (28.5–56.2) |
| Why it is important to use the net | 721 | 35.1 (29.2–40.8) |
| Other | 114 | 6.0 (4.3–7.7) |
| HH received a post-distribution visit by mobilizer | 577 | 26.9 (21.3–32.4) |
| Received a hang-up demonstration | 277 | 40.6 (24.0–57.2) |
| Told importance of sleeping under bed net every night | 471 | 81.7 (77.2–86.2) |
| Told how to care for the bed net | 261 | 40.2 (25.7–54.8) |
| Received other malaria information | 43 | 6.9 (1.6–12.2) |
| Did not receive any IEC messages during visit | 75 | 14.3 (5.7–22.9) |
*Adjusted for clustering and sampling weights
†Confidence Intervals
‡HH: Household
At the time of the survey, households were asked if they still possessed the campaign LLINs that they initially received. Among the 1980 households that received one or more campaign LLINs, 1848 (93.7%) reported they had retained all the campaign nets and 1965 (99.3%) retained at least one campaign net. There were a total of 132 campaign nets that were no longer in possession by the households. For the majority of nets (84% of the 132 not retained) the reason cited was because they were given away to others.
Campaign mobilization, information, education and communication
Among the 2211 households responding to the survey, 2019 (91.8%) had received information about the bednet campaign. The primary source of information most commonly cited was: 1) the fokontany chief (60.2%), 2) a community mobilizer (21.8%), and 3) a health worker (11.1%). Campaign Information Education Communication (IEC) materials and messaging were less commonly cited: only 1.1% reported the radio as a source, 0.4% reported banner/posters, 0.1% reported Tam Tam (village criers), and 0.3% reported television as their main source of information.
Two thirds of households (66.1%) reported they received a pre-distribution visit by a campaign community mobilizer. Only 1823 households (84.2%) said they received vouchers prior to the campaign: 32.5% of households received only one voucher and 51.7% received two or more vouchers (Table 2). The large majority (91.0%) of households that received vouchers reported the community mobilizer explained how to use the voucher. Among the 361 households that did not receive a voucher, 17.4% said there were not enough vouchers left, 14.9% said they were not visited by a mobilizer, and only 6 (1.3%) reported they did not get a voucher because they did not have enough money to pay for it although vouchers were supposed to be distributed for free. Almost half (42.1%) did not know why they were not given a voucher.
Among the 1918 households (86.9%) that traveled to the distribution point, 98.9% traveled on foot and 83.5% felt the distance was reasonable. Over two-thirds of households (68.2%), reported it took less than 30 minutes of travel time to reach the distribution point from their home, 16.2% said it took between 30 minutes and 1 hour, and 16.3% said it took over 1 hour of travel time (Table 2). Only 17 households (1%) said it took one full day or more of travel time to reach the distribution point. When households were asked what type of information they received at the distribution point, 40.9% cited how to hang a net, 42.3% said they received messages on washing and caring for nets, and 35.1% were told why it was important to use the net.
Only 577 (26.9%) of households received a visit by a mobilizer after the campaign (Table 2). Among these, 277 (40.6%) households received a hang-up demonstration and the reported delivery of key post-campaign messaging was variable: 81.7% reported they were told the importance of sleeping under the net every night and only 40.2% were told how to care for their net. Furthermore, 14.3% of households said they did not receive any education or malaria prevention messages during the post-campaign visit.
LLIN ownership and LLIN access
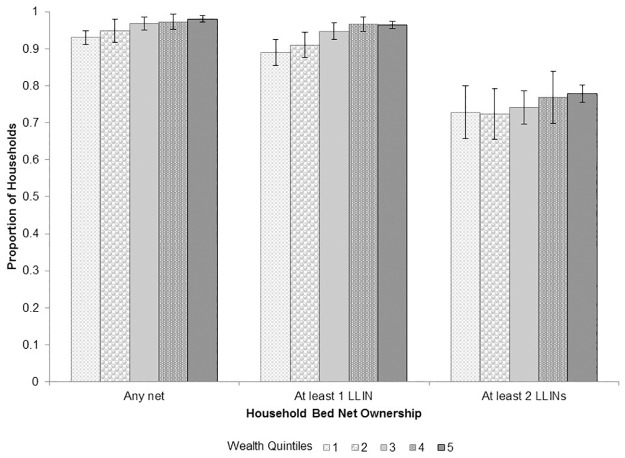
Among the 2211 households responding to the survey, post-campaign net ownership was high: 93.5% (95% CI, 91.6–95.5%) owned at least one LLIN, and 74.8% (95% CI, 71.0–78.5%) owned at least two LLINs. Fig 2 shows household LLIN ownership by wealth quintile: 89.1% (95% CI, 85.6–92.6%) of households in the poorest wealth quintile owned at least one LLIN compared to >96% in the two richest wealth quintiles; however, for ownership of at least two LLINs, differences between wealth quintiles were not significant. The average number of LLINs per household was 2.0 (95% CI, 1.9–2.1).
Fig 2. Proportion of households owning 1) any net 2) at least one LLIN and 3) at least two LLINs, by wealth quintile (1 = poorest, 5 = wealthiest quintile).
There were 1005 households with at least one child under five years old. Net ownership in this subgroup was equally high: 93.8% (95% CI, 90.8–96.8%) of households with at least one child under five owned at least one LLIN and 77.5% (95% CI, 73.8–81.2%) owned at least two. Among the 240 households with at least one pregnant woman, the percentage owning one LLIN and two LLINs were similar at 93.9 (95% CI, 90.2–97.7%) and 72.8 (95% CI, 65.0–80.6%), respectively
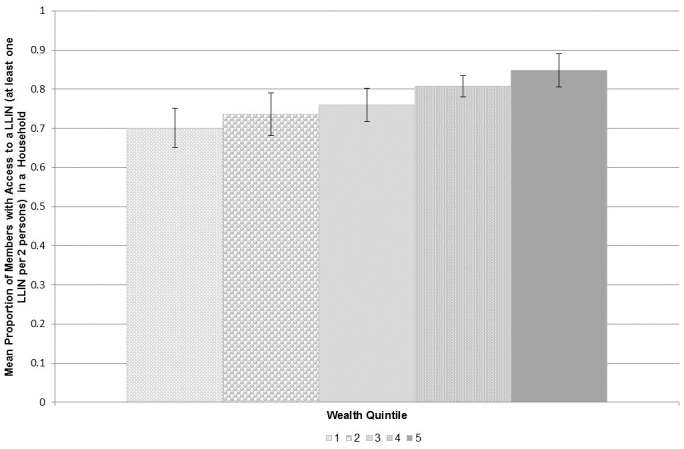
Among all households, 58.6% (95% CI, 53.3–63.9%) owned enough nets to meet the RBM goal ratio of at least one LLIN for every two people. Access measured as the proportion of the population that could potentially be covered by household-owned LLINs was 77.2% (77.2% (95% CI, 72.9–81.3%). Fig 3 illustrates this indicator stratified by wealth quintile showing that the proportion of the population with access to a LLIN increased with increasing wealth status. The equity ratio of the wealthiest to the poorest households was 1.2 (wealthiest quintile = 84.9% (95% CI, 83.3–86.4%), poorest quintile = 70.1% (95% CI, 65.1–75.1%)). Reasons reported for not receiving a bednet during the campaign included the following: households not registered, no bednets available at the distribution point, and individuals did not have an identification card to present.
Fig 3. Average proportion of household members with access to a LLIN (at least one LLIN per 2 persons) by wealth quintile (1 = poorest, 5 = wealthiest quintile).
In contrast, pre-existing LLIN coverage was low at 31.1% (95% CI, 19.1–43.2%), 9.2% (95% CI, 3.2–15.2%), and 10.2% (95% CI, 6.0–14.4%) for the proportion of households owning of at least one pre-existing LLIN, at least two pre-existing LLINs, and at least one pre-existing LLIN per two people, respectively.
A multivariable model to assess factors associated with LLIN access defined as a minimum of one LLIN per two people (RBM goal) was created and odds ratios associated with LLIN access are shown in Table 3. The final model consisted of 24 variables. Decreased odds of an individual having access to a LLIN in a household was significantly associated with having a child under five years old in the household (OR 0.58, 95% CI 0.50–0.67), poor wealth status (OR 0.36, 95%CI 0.24–0.54 for the poorest quintile compared to the richest), not owning a radio (OR 0.75, 95% CI 0.63–0.90), more sleeping spaces in the household (OR 0.77, 95% CI 0.69–0.86), not receiving a pre-campaign voucher (OR 0.4, 95% CI 0.33–0.49), and living in a district covered by the December campaign vs. districts covered in the November campaign (OR 0.75, 95% CI 0.63–0.90). Campaign factors significantly associated with increased LLIN access included having received a pre-campaign household visit (OR 1.2, 95% CI 1.01–1.42). Households with a member that knew malaria could be prevented by sleeping under a LLIN were associated with increased odds of access (OR 2.33, 95% CI 1.88–2.90). LLIN access was not associated with presence of a pregnant woman in the household, highest level of education in the household, knowledge that LLINs protect against mosquito bites or having received any information about the campaign. Nor was it associated with travel time or relative distance from the distribution point to the household.
Table 3. Factors associated with household access to LLINs (ratio of LLINs to people).
| Household Access to LLINs* | Unadjusted OR† | p | Adjusted OR† | 95% CI‡ | p |
|---|---|---|---|---|---|
| Household with at least one pregnant woman | 0.93 | 0.62 | 1.10 | 0.86–1.42 | 0.44 |
| At least one child under five years old in household | 0.68 | <0.0001 | 0.58 | 0.50–0.67 | <0.0001 |
| Number of people sleeping in household | 0.78 | <0.0001 | - | - | - |
| Highest level of education in household | |||||
| No formal education | Ref | Ref | Ref | Ref | 0.32 |
| Primary school | 1.19 | 0.002 | 1.12 | 0.88–1.44 | |
| Middle school | 1.54 | 0.94 | 1.27 | 0.92–1.75 | |
| Secondary school | 2.39 | 0.003 | 1.54 | 1.03–2.29 | |
| Higher than secondary school | 2.06 | 0.23 | 1.31 | 0.70–2.44 | |
| Wealth quintile | |||||
| 1 (poorest) | 0.42 | <0.0001 | 0.36 | 0.24–0.54 | <0.0001 |
| 2 | 0.50 | 0.006 | 0.43 | 0.29–0.64 | |
| 3 | 0.58 | 0.32 | 0.44 | 0.30–0.64 | |
| 4 | 0.78 | 0.032 | 0.60 | 0.41–0.87 | |
| 5 (richest) | Ref | Ref | Ref | Ref | |
| Campaign wave | |||||
| November 2009 | Ref | Ref | Ref | <0.01 | |
| December 2009 | 0.82 | 0.027 | 0.75 | 0.63–0.90 | |
| Cited malaria could be prevented by sleeping under an insecticide treated mosquito net | 2.68 | <0.0001 | 2.33 | 1.88–2.90 | <0.0001 |
| Cited most important advantage of LLIN was to protect against mosquito bites | 1.28 | 0.009 | 1.11 | 0.95–1.30 | 0.18 |
| Received information about the campaign | 2.03 | <0.0001 | 1.13 | 0.86–1.49 | 0.38 |
| Received a pre-campaign household visit | 1.56 | <0.0001 | 1.20 | 1.01–1.42 | 0.04 |
| Received a campaign voucher | |||||
| Yes | Ref | Ref | Ref | Ref | <0.0001 |
| No | 0.33 | <0.0001 | 0.40 | 0.33–0.49 | |
| Don’t know | 1.09 | 0.021 | 1.51 | 0.80–2.85 | |
| Possession of a radio | 1.14 | 0.14 | 0.75 | 0.63–0.90 | <0.01 |
| Number of sleeping spaces in household | 0.96 | 0.51 | 0.77 | 0.69–0.86 | <0.0001 |
| Number of people sharing a sleeping space in household | 0.68 | <0.0001 | - | - | - |
| Traveled to distribution point and travel time | |||||
| ≤ 1 hour | Ref | Ref | Ref | Ref | 0.55 |
| > 1 hour | 0.69 | 0.37 | 1.07 | 0.86–1.32 | |
| Don’t Know | 0.38 | <0.0001 | 0.63 | 0.23–1.75 | |
| Distribution point location relative to household | |||||
| In same village | Ref | - | Ref | Ref | 0.22 |
| In another village in same fokontany | 0.76 | 0.039 | 0.85 | 0.69–1.04 | |
| In another village outside fokontany | 0.64 | 0.97 | 0.81 | 0.65–1.00 | |
| Other | 0.35 | <0.0001 | 0.94 | 0.35–2.53 |
*Long lasting Instecticidal Nets (LLINs).
†Odds Ratio (OR).
‡Confidence Interval (CI).
LLIN use
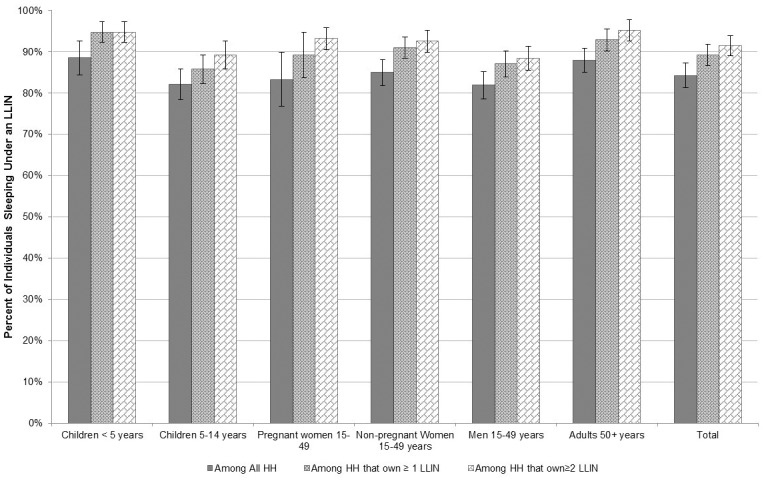
The majority, 84.2% (95% CI, 81.2–87.2%) of individuals that slept in the household the night before the survey reported using a LLIN. Among vulnerable groups providing information about LLIN use, including 1372 children under five and 243 pregnant women, reported LLIN use was 88.5% (95% CI, 84.4–92.6%) and 83.3% (95% CI, 76.8–89.8%), respectively. Reported LLIN use was high (>80%) among all age and gender groups including children 5–14 years old, non-pregnant women 15–49 years old, men 15–49 years old and adults over 50 years old illustrated in Fig 4. The proportion of the population reporting having slept under a LLIN increased for each of these groups in the subset of households that owned at least one LLIN and increased further among households that owned at least two LLINs. Among the 1634 (70.1%) households that owned at least two LLINs, the proportion of all individuals, children under 5 and pregnant women that reported sleeping under a LLIN was very high at over 90% as shown in Fig 4.
Fig 4. LLIN use by specific age group and gender among 1) all households 2) households that own at least one LLIN and 3) households that own at least two LLINs.
Universal LLIN use, defined as all household members sleeping under a LLIN, was estimated by calculating the proportion of households in which every member reported sleeping under a LLIN the night before the survey. Among the 2198 households with at least one person that slept in the household the night before the survey, 76.8% (95% CI, 73.2–80.4%) reported that all household members slept under a LLIN, with equity across wealth quintiles. When these households were further stratified by those that owned at least one LLIN and those that owned at least two LLINs, universal LLIN use was even higher at 82.1% (95% CI, 78.6–85.6%) and 85.2% (95% CI, 81.8–88.6%), respectively.
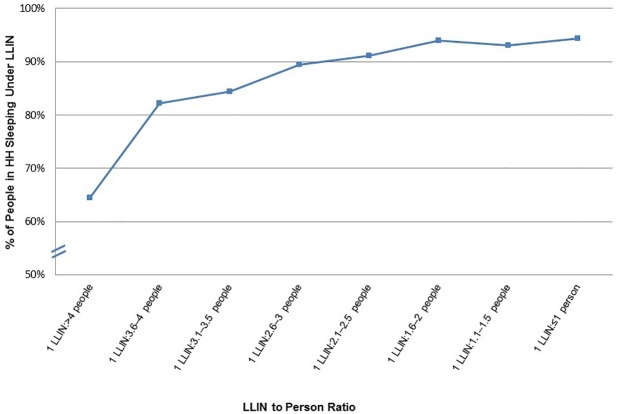
LLIN use was stratified by the LLIN-to-person ratio, shown in Fig 5. LLIN use was over 90% when the LLIN-to-person ratio was 1:3 (0.33) or more. Among households that achieved the RBM goal of at least one LLIN per two persons (ratio 1:2 or more, ≥0.5), 93–94% of members were using a LLIN. In contrast, in households where there were more than four people per LLIN, use fell to ≤ 65%.
Fig 5. Proportion of people sleeping under a LLIN within households by LLIN to person ratio.
Only 3183 (72%) of bednets were reported to be hanging the night before the survey. Of the 1140 usable nets that were not hanging, the main reasons cited were: all household members were already sleeping under other bednets (37.1%), the net was too old and worn (1.9%), the net was used for travelers or guests (17.5%), the net was being saved for future use (9.9%), and there was not enough room to hang the net (9.7%). There were rare reports of bednets not hung because they were being used for other purposes (0.6%) or not hung because they were perceived to not work or because household members did not like to use them (0.5%).
Results of a multivariable analysis to identify factors associated with the odds of individuals using a LLIN, among households owning LLINs, are shown in Table 4. Increased odds of individuals using a LLIN was associated with older age (OR 1.02, 95% CI 1.01–1.02) and inversely associated with the head of the household having a primary education or higher (OR 0.74, 95% CI 0.66–0.83). Increased odds of use was also associated with the following household characteristics: lower economic status or wealth quintile (OR 1.84, 95% CI 0.88–3.85 for the poorest compared to the richest), number of children under five in the household (OR 2.05, 95% CI 1.67–2.51), knowledge by a member of the household that malaria is prevented by sleeping under a LLIN (OR 3.58, 95%CI 1.69–6.94), living in a household that traveled to and received information on how to hang a bednet at the distribution site (OR 1.56, 95% CI 1.41–1.74), and living in a household that received a post campaign visit by a community mobilizer who told them to sleep under the net nightly (OR 1.75, 95% CI 1.26–2.43). Higher odds of LLIN use was inversely associated with household size (OR 0.81, 95% CI 0.77–0.85). Increased odds of LLIN use was also independently associated with living in a household with higher quality wall material such as earth, bamboo reinforced with mud, wood planks compared to a simple palm/cane/bamboo wall. LLIN use was not associated with gender, household ownership of a radio or type of household roof.
Table 4. Factors associated with LLIN use.
| LLIN* Use | Unadjusted OR† | p | Adjusted OR† | 95% CI‡ | p |
|---|---|---|---|---|---|
| Female gender | 1.14 | 0.01 | 1.10 | 0.99–1.23 | 0.08 |
| Age | 1.01 | <0.0001 | 1.02 | 1.01–1.02 | <0.0001 |
| Primary education or higher | 0.69 | 0.01 | 0.74 | 0.66–0.83 | <0.0001 |
| Wealth Quintile | |||||
| 1 (poorest) | 1.57 | 0.05 | 1.84 | 0.88–3.85 | <0.0001 |
| 2 | 1.46 | 0.09 | 1.45 | 0.70–3.00 | |
| 3 | 1.22 | 0.68 | 1.28 | 0.70–2.32 | |
| 4 | 0.76 | 0.01 | 0.78 | 0.67–0.91 | |
| 5 (richest) | Ref | - | Ref | ||
| Household size (number of people sleeping in household) | 0.89 | 0.0006 | 0.81 | 0.77–0.85 | <0.0001 |
| Number of children under five years old in household | 1.58 | 0.006 | 2.05 | 1.67–2.51 | <0.0001 |
| Number of LLINs owned by household | 1.68 | 0.003 | 2.82 | 1.85–4.3 | <0.0001 |
| Number of free nets in household | 1.29 | 0.008 | - | - | - |
| Number of nets from the campaign in household | 1.61 | <0.0001 | - | - | - |
| Number of hanging LLINs in household | 7.34 | <0.0001 | - | - | - |
| Number of sleeping spaces in individual’s household | 0.69 | 0.0007 | 0.55 | 0.44–0.68 | <0.0001 |
| Number of people sharing an individual’s sleeping space | 1.06 | 0.53 | - | - | - |
| Knowledge in household that malaria is prevented by sleeping under an insecticide treated net | 2.97 | 0.001 | 3.58 | 1.85–6.94 | 0.0002 |
| Live in HH that traveled to distribution site | 1.08 | 0.61 | |||
| Lives in HH that traveled to distribution site and received information on how to hang a bed net | 1.82 | <0.0001 | 1.56 | 1.41–1.74 | <0.0001 |
| Lives in HH that traveled to distribution site and received information on importance of bed net usage | 1.12 | 0.35 | |||
| Lives in HH that received a post-campaign visit | 1.17 | 0.17 | - | - | - |
| Lives in HH that received a post-campaign visit and | |||||
| Volunteer said to sleep under the net nightly | 1.42 | 0.0006 | 1.75 | 1.26–2.43 | <0.0001 |
| Volunteer did not mention sleeping under net | 0.60 | <0.0001 | 1.34 | 0.98–1.82 | |
| Lives in HH that did not receive a post-campaign visit | Ref | Ref | Ref | Ref | |
| Live in HH that received a post-campaign visit and was shown how to hang net | 1.51 | 0.01 | - | - | - |
| Live in HH that received a post-campaign visit and was told importance of sleeping under bed net | 2.37 | 0.0001 | - | - | - |
| Household roof material | |||||
| Thatch | Ref | Ref | Ref | Ref | 0.43 |
| Sod | 1.33 | 0.01 | 1.39 | 0.66–2.93 | |
| Mat | 0.81 | 0.84 | 0.74 | 0.36–1.53 | |
| Sheet Metal | 0.78 | 0.51 | 0.94 | 0.50–1.76 | |
| Other | 0.62 | 0.18 | 1.00 | 0.38–2.63 | |
| Household wall material | |||||
| Palm/cane/bamboo | Ref | Ref | Ref | Ref | <0.0001 |
| Dirt/earth | 0.61 | 0.001 | 1.14 | 0.63–2.04 | |
| Bamboo with mud | 1.93 | 0.003 | 1.70 | 0.82–3.53 | |
| Wood planks | 0.85 | 0.19 | 1.29 | 1.05–1.59 | |
| Other | 0.92 | 0.66 | 1.67 | 1.03–2.71 | |
| Possession of a radio | 0.83 | 0.32 | 1.41 | 0.92–2.16 | 0.11 |
*Long lasting Instecticidal Nets (LLINs).
†Odds Ratio (OR).
‡Confidence Interval (CI).
Discussion
The 2009 LLIN campaign was the first free mass distribution campaign targeting all individuals (i.e., not limited to pregnant women and children under 5) and attained historic high rates of both LLIN access and use in Madagascar. The campaign reduced disparities in ownership and use across economic groups, improving equity, which was consistent with results of free mass distribution campaigns in other countries [13–16]. The large majority of nets used by household members were in good physical condition and thus, if used correctly, would provide both individual protection against malaria as well as community-level reductions in mosquito density and survival to reduce malaria transmission exposure [17].
Performance against the targets
Insecticide-treated mosquito nets were first distributed in Madagascar in 2002 through social marketing and starting in 2005, through free routine distribution in health clinics targeting pregnant women and children [18]. An integrated campaign which distributed both free LLINs on a large scale for the first time during a national campaign to provide measles vaccination, mebendazole, and vitamin A to children under five resulted in household ownership of at least one LLIN of 76.8% and LLIN use by pregnant women, children under 5, and all household members in the targeted districts at 68.5%, 80.8% and 59.9%, respectively [19]. Compared to these previous efforts, the stand-alone 2009 free universal mass distribution campaign increased LLIN ownership by >30% and LLIN use by >25% (see S1 Table). Furthermore, using the pre-existing LLIN coverage estimate as a baseline, the campaign increased household ownership of at least two LLINs by 68% and increased household ownership of at least one LLIN per two people from 10.2%, immediately pre-campaign, to 58.6% post-campaign, representing more than a fivefold increase, moving towards the RBM goal.
The average number of LLINs owned per household was two overall, meeting the national strategy target; however, only 70.1% of households reported receiving two or more campaign LLINs during the 2009 distribution and it remains concerning that 13% of households were not reached at all, highlighting distribution weaknesses. Campaign supervisors reported distribution sites that ran out of nets or had to further ration nets during the campaign indicating that several sites did not have enough to provide two LLINs for every household in their communities. After the campaign, compiled data from the household registration process revealed that the registered population of the 19 districts was 116% of that projected from the adjusted census estimates that were used to plan and quantify nets needed for the campaign, which corroborates the theory that there were insufficient nets and could further explain why the campaign goal of two LLINs per household was not met.
Analysis using 2013 MERG indicators measuring access to LLINs based on the recommended ratio of one LLIN for every two persons reveals the fixed “two nets per household” distribution approach during the campaign fell short of the RBM goal of one LLIN for every two persons. The fixed distribution methodology of two LLINs per household, regardless of size, is likely to have led to inequitable distribution of nets given the variation in household size. The mean household size in the survey was 4.1 with a wide range and 36% of households had more than four members sleeping in the household indicating that two LLINs would provide suboptimal coverage in this group. LLIN use was over 90% among households with a LLIN to person ratio of 1:≤3 (0.33), moreover, the average number of people reported sleeping under each LLIN was 2.6. Thus, in order to ensure all household members are adequately protected in Madagascar one LLIN for every two persons is needed.
Lessons learned from campaign planning and implementation
Campaign implementation process indicators identified key weaknesses in the household registration and voucher distribution process, including charging “hidden fees” for vouchers or nets when they were meant to be free. Vouchers were expensive, logistically difficult to distribute, and sub-optimally used. This resulted in some households not receiving any vouchers and a substantial portion only receiving one voucher, causing an inequitable and insufficient distribution of nets. Campaign monitors anecdotally reported instances where vouchers were falsely reproduced in the field threatening the integrity of the campaign. Vouchers posed a similar barrier during an integrated vaccination/bednet campaign in Niger and vouchers schemes used to distribute nets to pregnant women attending antenatal clinic services have common operational challenges [15, 20, 21]. Vouchers can work well in some settings [10]–however given the implementation challenges in Madagascar and the significant added expense to produce and distribute them, it is difficult to justify future use.
Among households that did not receive a campaign net, the majority did not receive a pre-campaign visit by a mobilizer underscoring the need for a more fair and transparent pre-campaign registration process. Households that received a pre-campaign visit were independently associated with higher LLIN access. Few households had post-campaign visits by community mobilizers and for those that did, visits were of poor quality (e.g., IEC messages not delivered adequately, less than 50% received hang-up demonstrations).
The main source of communication about the campaign cited by households was the fokontany chief, in addition to the mobilizers and health center staff. This important community leader role should be integrated effectively in future campaign planning to optimize information dissemination. Sites appeared to be well placed as most households reported that the distance they were required to travel was reasonable. Over 80% of households said travel to the distribution point took less than one hour and travel times were not found to be associated with lower LLIN access or use thus the campaign organization of one distribution site per three fokontany was adequate. This is an important consideration for future campaigns given the increased cost associated with each additional distribution point. One caveat is that the population density is high on the East coast and the organization of one distribution point per three fokontany may not work equally as well in other parts of the country where distances between fokontany are much larger and fokontany may be more remote and physically isolated.
Factors associated with LLIN access and use
There are limited reports of factors associated with high intra-household access to a LLIN (at least one LLIN per two people). When considering household ownership of at least one LLIN, determinants of coverage included factors similar to those reported in this survey. Higher ownership associated with increased malaria knowledge was reported in a sub-district in Madagascar in 2008 prior to large scale campaign distribution, and has been reported in other countries [22, 23]. Households citing malaria could be prevented by sleeping under an ITN were positively associated with both better access and higher use in our setting.
The proportion of the population using a LLIN (84.2%) was higher than population LLIN access, supporting the hypothesis that there is a strong culture of LLIN acceptance in Madagascar and there are minimal barriers to use when nets are available in contrast to other settings where LLIN distribution led to increased ownership but did not result in a concomitant increase in use as expected [24–32].
The strongest predictor of individual LLIN use was having more LLINs available in the household. Using survey data from 15 countries, Eisele et al. showed that ITN use by children under five years old increased as intra-household ITN access increased [30]. Recent surveys from Nigeria and Sierra Leone also documented improved household access was associated with higher LLIN use by all individuals, similar to our findings in Madagascar [31, 33]. To improve coverage in future campaigns, quantification estimates and allocation of LLINs to households should be based on household size as recommended by Kilian et al. [34].
Lack of ownership was the predominant reason that members of these poorer households were not protected. Reasons reported for not receiving a bednet during the campaign point to modifiable deficiencies in the campaign implementation process. Recommendations were subsequently made to include non-registered households and persons without identification if they were verified by local authorities. Among wealthier households the largest proportion of non-users lived in households owning and hanging at least one LLIN suggesting other factors are likely to explain this gap–such as inadequate quantity of nets to cover all household members, deficiency in knowledge of the importance of using a bednet, or other reasons inhibiting users from sleeping under a bednet. Pulford et al. conducted a review of the literature among published household surveys and qualitative studies of reasons for not using a mosquito net when available and found the most widely reported reasons were discomfort from heat and perceived low mosquito density [35]. However, these were the least frequently cited reasons for not using nets (<4%) in this Madagascar survey.
Households that received a post campaign visit were also significantly associated with use indicating that targeted post-campaign interpersonal communication activities could effectively promote use, although the evaluation was not designed to test this hypothesis. Evidence of the association between behavior change communication strategies (BCC) and behaviors like net use has been mixed. A recent cluster randomized trial in Togo demonstrated an association between post-campaign BCC and net use [36]. In Ethiopia, repeated malaria IEC interventions with heads of households at the community level have resulted in behavior change and increased LLIN use [37]. Keating et. al. reported an association between high ITN use and exposure to malaria-related messages in communities in Zambia with near universal coverage, although a specific intervention to provide IEC at the household level using community health workers in itself did not significantly influence ITN use [38, 39]. The effectiveness of community level IEC/BCC efforts may be country or community specific given a similar cluster-randomized trial of post-campaign household visits and targeted IEC among intervention communities in Uganda also did not show an increase in LLIN use compared to control communities [40].
In our setting, 8.2% of LLINs were found new and untouched in their original packaging and almost 1/3 of nets not hung were being reserved for guests or future use. Effective mobilization should aim to educate household members on the importance of using the new (more effective) LLINs with an emphasis on replacing older nets that are still hanging. Retention and use of older nets in poor condition, even after acquiring new LLINs, has been reported in other settings [39]. Overall, very few LLINs were repurposed or misused, a finding similar to that recently reported in Zambia and Sierra Leone, and one that is contrary to popular belief [33, 39, 41].
Multiple studies report households having a member with a higher education and literacy level have been associated with increased LLIN use, similar to our findings, and this may facilitate understanding of malaria prevention health promotion messages and behavior [22, 27, 42–46]. In Madagascar, malaria prevention messages had been disseminated through mass media during off-campaign years, as well as through campaign-specific mass media, primarily radio. This could explain why owning a radio was associated with higher LLIN access. Radio possession was also identified to be an important factor associated with higher LLIN use in Ethiopia [47] and listening to a radio once a week was reported as a determinant of use among pregnant women in a recent review [22]. Although it is not possible to discern which specific activities may have been the most effective in promoting malaria prevention behaviors from this survey, developing effective BCC activities, especially targeting less educated households, should be a priority even in the setting of a well-established net culture such as in the East Coast of Madagascar.
Multivariable logistic regression analysis of factors associated with LLIN access confirmed the association between increasing wealth and better access. A similar finding was reported by Thwing et al. in Senegal where poorer households had high ownership of at least one net, but intra-household access was higher among wealthier households [10]. Although LLIN access inequity between rich and poor has vastly improved, some disparities remain between socio-economic groups and continue to be a program challenge [19, 39, 43, 48, 49]. In contrast, increased LLIN use was independently associated with poorer households compared to wealthier households, a finding similar to that reported for children under five years old after an integrated free distribution campaign in Madagascar in 2007 [50, 51]. While there have been several reports of higher ITN use among wealthier populations compared to poorer ones [43, 52, 53], analysis of a few large household surveys have reported higher ITN use among those living in households in the poorest wealth quintile similar to our findings, especially when analyzing the use of bednets distributed free of cost [22, 40, 43, 51].
Surprisingly, households with at least one child under five were associated with lower LLIN access despite a long-standing history of LLIN distribution BCC and strategies that targeted vulnerable groups. Given the low coverage of pre-existing LLINs it is possible that previous LLINs distributed to target the under five year old children were already more than three years old and had become either unusable with regular wear and tear, were discarded or given away. Despite this result for access, individuals living in households with more children under five were associated with higher LLIN use; this finding has been reported previously in a small study from a sub-district of Madagascar, as well as other settings, and could be a result of higher perceived vulnerability to malaria by small children leading to higher overall LLIN use in these households [43, 54]. It is likely program IEC/BCC efforts from previous antenatal clinic LLIN distribution efforts and social marketing in Madagascar also reinforced the use of LLINs in households with children under 5 years old, especially on the East Coast where it was these were the main methods of distributing LLINs from 2006–2009. The number of sleeping spaces in the household were inversely associated with LLIN use and warrants further analysis of intra-household sleeping and net use patterns to potentially inform both distribution strategies and BCC activities to promote optimal use [55].
These survey results reflect the success of the first two phases of a three-phase national campaign and lessons learned were used to inform subsequent LLIN campaign planning. The 2009 campaign and the subsequent 2010 LLIN distribution campaign covering additional geographic areas increased LLIN ownership to 94% among at risk malaria zones nationwide, access to 77% and use among the general population to 82% by May 2011, resulting in almost half of the estimated 34,000 lives saved among children under five between 2000 and 2011 [18]. Large scale-up of net ownership through free mass distribution campaigns is feasible and effective at achieving high ownership and retention six months after distribution and high use in Madagascar by all individuals as well as vulnerable groups. Improvements in campaign planning and implementation could further ensure equitable LLIN access.
The 2011 MIS results represented relative immediate post-campaign coverage and use resulting from both the 2009 LLIN campaign (East Coast) and the subsequent 2010 LLIN campaign (remaining malaria at risk areas in the North, West and South). However, later studies showed high coverage and use rates were not sustainable over time. Kesteman et al. conducted a cross sectional survey in 2012, over two years after the 2009/2010 campaign and found LLIN ownership to be as low as 40–65% depending on the geographic area, access was only 43% and use 64% [56]. The 2013 MIS reported areas of the county that did not benefit from additional campaign distributions in the interim had declines in ownership of at least one LLIN to 68%, access to 39% and use to 51% compared to those that did (ownership of at least one LLIN 96% and use 87%) [57]. These repeated cross-sectional measures over time underscore the challenges and limitations on the ground of maintaining adequate malaria prevention using existing LLIN technology under program conditions in Madagascar.
Limitations
Self-reported household ownership and use, specifically sleeping under a net the night before the survey, was not verified by observation, and is a limitation of the standard household survey methodology. The survey teams were only able to visually confirm the presence of 82% of reported LLINs in the households. However, we believe people would be more likely to under-report ownership in the hopes of being given another net thus LLIN ownership could be slightly underreported. Also there were 52 bednets that were identified as campaign nets but could not be verified to be LLINs per standard survey methods described above. It is possible these nets were also LLINs which would slightly increase LLIN ownership and use estimates.
Survey data were collected six months after the campaign and self-reported information on voucher receipt and exchange, household visits by community mobilizers and other campaign-type indicators could be subject to recall or reporting bias; however, we would expect this to be minimal. Furthermore, some key indicators like in-home post-campaign hang-up demonstrations are relatively unusual and distinct events in the community that are unlikely to be subject to recall bias.
In addition this cross-sectional survey was not able to directly assess LLIN use over time which has been reported to deteriorate in other settings.[43] Longitudinal studies are needed to address this important programmatic question.
Supporting information
(TIF)
Acknowledgments
We acknowledge the community members in the surveyed districts of Madagascar, especially those households who participated in the study. We thank the district health teams that helped us to coordinate and conduct the survey. We are indebted to the NMCP and RBM partners, including UNICEF, World Health Organization, who made this survey possible and helped to formulate recommendations with the results. We thank Mr. Fidelys Solomampionona Andrianorosoa Ratelolahy for his leadership in conducting the mass free bednet distribution. We acknowledge Population Services International and the non-governmental organization, TANDEM, for their assistance in hiring data collectors and providing logistical support. We thank the USAID for their support of the survey, especially Mr. Donald Dickerson the USAID President’s Malaria Initiative USAID resident advisor and Dr. Noë Rakotondrajaona, the USAID senior malaria advisor at the time of the survey.
Data Availability
The IRB/Ethics Committee approved protocol specifies the data for this evaluation were required to be turned over to the Ministry of Health/National Malaria Control Program in Madagascar and did not allow for public sharing of patient-level data. The previous Ministry of Health Malaria Program Director co-author has since left the programme and is not authorized to grant permission. None of the other co-authors are authorized to release the data at this time. The restrictions prohibiting the authors from making the minimal data set publicly available: the approved protocol procedures. Institutional/non-author contact information at which data can be requested: Access to the data can be made upon request from Dr. Mauricette Andriamananjara, Vector Control Team, National Malaria Control Program (Programme National de Lutte Contre le Paludisme) Madagascar by email: nambinisoa@yahoo.fr.
Funding Statement
This work was supported by the US President's Malaria Initiative. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Roll Back Malaria Partnership. The Global Malaria Action Plan For a Malaria-Free World. Roll Back Malaria Partnership, 2008. [Google Scholar]
- 2.Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;(2):CD000363 Epub 2004/04/24. doi: 10.1002/14651858.CD000363.pub2 . [DOI] [PubMed] [Google Scholar]
- 3.NMCP M. National Strategic Plan in the Fight Against Malaria in Madagascar 2008–2012: from control towards elimination of malaria. 2009.
- 4.PSI. Tracking Results Continuously (TRaC) Survey among 15–49 Year Old Women with Children Under Five: Malaria Prevention. Antananarivo, Madagascar: PSI, 2004 September 2008. Report No.
- 5.PSI. Tracking Results Continuously (TRaC) Survey among 15–49 Year Old Women with Children Under Five: Malaria Prevention. Antananarivo, Madagascar: PSI, 2008 September 2008. Report No.
- 6.Kulkarni MA, Desrochers RE, Goodson JL, Mandy J, Cotte AH, J C, et al. Evaluation de l’appropriation et l’utilisation des moustiquaires imprégnées d’insecticide à longue durée (MIDs) au Madagascar six mois après la campagne intégrée rougeole/paludisme d’octobre 2007. Antananarivo: Health Bridge, U.S. Centers for Disease Control and Prevention, 2008 June 2008. Report.
- 7.Steinhardt LC, Chinkhumba J, Wolkon A, Luka M, Luhanga M, Sande J, et al. Quality of malaria case management in Malawi: results from a nationally representative health facility survey. PLoS One. 2014;9(2):e89050 doi: 10.1371/journal.pone.0089050 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolkon A, Vanden Eng JL, Morgah K, Eliades MJ, Thwing J, Terlouw DJ, et al. Rapid scale-up of long-lasting insecticide-treated bed nets through integration into the national immunization program during child health week in Togo, 2004. Am J Trop Med Hyg. 2010;83(5):1014–9. doi: 10.4269/ajtmh.2010.09-0599 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thwing J, Hochberg N, Vanden Eng J, Issifi S, Eliades MJ, Minkoulou E, et al. Insecticide-treated net ownership and usage in Niger after a nationwide integrated campaign. Trop Med Int Health. 2008;13(6):827–34. doi: 10.1111/j.1365-3156.2008.02070.x . [DOI] [PubMed] [Google Scholar]
- 10.Thwing JI, Perry RT, Townes DA, Diouf MB, Ndiaye S, Thior M. Success of Senegal's first nationwide distribution of long-lasting insecticide-treated nets to children under five—contribution toward universal coverage. Malar J. 2011;10:86 doi: 10.1186/1475-2875-10-86 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rutstein S. O. JK. DHS Comparative Reports No. 6: The DHS Wealth Index. Calverton, MD: ORC Macro, 2004 2004. Report No.
- 12.RBM. Household Survey Indicators for Malaria Control Roll Back Malaria, 2013 June 2013. Report No.
- 13.Grabowsky M, Nobiya T, Ahun M, Donna R, Lengor M, Zimmerman D, et al. Distributing insecticide-treated bednets during measles vaccination: a low-cost means of achieving high and equitable coverage. Bull World Health Organ. 2005;83(3):195–201. Epub 2005/03/31. . [PMC free article] [PubMed] [Google Scholar]
- 14.Noor AM, Amin AA, Akhwale WS, Snow RW. Increasing coverage and decreasing inequity in insecticide-treated bed net use among rural Kenyan children. PLoS Med. 2007;4(8):e255 Epub 2007/08/24. doi: 10.1371/journal.pmed.0040255 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC. Distribution of Insecticide-Treated Bednets During a Polio Immunization Campaign—Niger, 2005. MMWR. 2006;55(33):913–6. [PubMed] [Google Scholar]
- 16.Saurabh S, Kumar SG, Sahu SK, Thapaliya S, Sudharsanan S, Vasanthan T. Use of insecticide-treated bednets in an urban coastal area of Puducherry, India: A cross-sectional study. Indian J Public Health. 2013;57(4):276–9. Epub 2013/12/20. doi: 10.4103/0019-557X.123269 . [DOI] [PubMed] [Google Scholar]
- 17.Killeen GF, Smith TA, Ferguson HM, Mshinda H, Abdulla S, Lengeler C, et al. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. 2007;4(7):e229 Epub 2007/07/05. doi: 10.1371/journal.pmed.0040229 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Focus on Madagascar: Roll Back Malaria Partnership Progress & Impact Series, Country Reports Number 7. 2013.
- 19.Kulkarni MA, Vanden Eng J, Desrochers RE, Cotte AH, Goodson JL, Johnston A, et al. Contribution of integrated campaign distribution of long-lasting insecticidal nets to coverage of target groups and total populations in malaria-endemic areas in Madagascar. Am J Trop Med Hyg. 2010;82(3):420–5. Epub 2010/03/09. doi: 10.4269/ajtmh.2010.09-0597 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh N, Mehra RK, Srivastava N. Malaria during pregnancy and infancy, in an area of intense malaria transmission in central India. Annals of tropical medicine and parasitology. 2001;95(1):19–29. . [DOI] [PubMed] [Google Scholar]
- 21.CDC. Distribution of Insecticide-Treated Bednets During an Integrated Nationwide Immunization Campaign—Togo, West Africa December 2004. MMWR. 2005;54(39):994–6. [PubMed] [Google Scholar]
- 22.Singh M, Brown G, Rogerson SJ. Ownership and use of insecticide-treated nets during pregnancy in sub-Saharan Africa: a review. Malar J. 2013;12:268 doi: 10.1186/1475-2875-12-268 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krezanoski PJ, Tsai AC, Hamer DH, Comfort AB, Bangsberg DR. Household malaria knowledge and its association with bednet ownership in settings without large-scale distribution programs: Evidence from rural Madagascar. Journal of global health. 2014;4(1):010401 doi: 10.7189/jogh.04.010401 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shargie EB, Ngondi J, Graves PM, Getachew A, Hwang J, Gebre T, et al. Rapid increase in ownership and use of long-lasting insecticidal nets and decrease in prevalence of malaria in three regional States of ethiopia (2006–2007). Journal of tropical medicine. 2010;2010 Epub 2010/10/12. doi: 10.1155/2010/750978 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ye Y, Patton E, Kilian A, Dovey S, Eckert E. Can universal insecticide-treated net campaigns achieve equity in coverage and use? the case of northern Nigeria. Malar J. 2012;11:32 Epub 2012/02/03. doi: 10.1186/1475-2875-11-32 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loha E, Tefera K, Lindtjorn B. Freely distributed bed-net use among Chano Mille residents, south Ethiopia: a longitudinal study. Malar J. 2013;12:23 Epub 2013/01/22. doi: 10.1186/1475-2875-12-23 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gobena T, Berhane Y, Worku A. Low long-lasting insecticide nets (LLINs) use among household members for protection against mosquito bite in Kersa, Eastern Ethiopia. BMC Public Health. 2012;12:914 Epub 2012/10/31. doi: 10.1186/1471-2458-12-914 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alaii JA, Hawley WA, Kolczak MS, ter Kuile FO, Gimnig JE, Vulule JM, et al. Factors affecting use of permethrin-treated bed nets during a randomized controlled trial in western Kenya. Am J Trop Med Hyg. 2003;68(4 Suppl):137–41. Epub 2003/05/17. . [PubMed] [Google Scholar]
- 29.Korenromp EL, Miller J, Cibulskis RE, Kabir Cham M, Alnwick D, Dye C. Monitoring mosquito net coverage for malaria control in Africa: possession vs. use by children under 5 years. Trop Med Int Health. 2003;8(8):693–703. Epub 2003/07/19. . [DOI] [PubMed] [Google Scholar]
- 30.Eisele TP, Keating J, Littrell M, Larsen D, Macintyre K. Assessment of insecticide-treated bednet use among children and pregnant women across 15 countries using standardized national surveys. Am J Trop Med Hyg. 2009;80(2):209–14. Epub 2009/02/05. . [PubMed] [Google Scholar]
- 31.Garley AE, Ivanovich E, Eckert E, Negroustoueva S, Ye Y. Gender differences in the use of insecticide-treated nets after a universal free distribution campaign in Kano State, Nigeria: post-campaign survey results. Malar J. 2013;12:119 Epub 2013/04/12. doi: 10.1186/1475-2875-12-119 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aderibigbe SA, Olatona FA, Sogunro O, Alawode G, Babatunde OA, Onipe AI, et al. Ownership and utilisation of long lasting insecticide treated nets following free distribution campaign in South West Nigeria. The Pan African medical journal. 2014;17:263 doi: 10.11604/pamj.2014.17.263.3927 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett A, Smith SJ, Yambasu S, Jambai A, Alemu W, Kabano A, et al. Household possession and use of insecticide-treated mosquito nets in Sierra Leone 6 months after a national mass-distribution campaign. PLoS One. 2012;7(5):e37927 doi: 10.1371/journal.pone.0037927 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilian A, Boulay M, Koenker H, Lynch M. How many mosquito nets are needed to achieve universal coverage? Recommendations for the quantification and allocation of long-lasting insecticidal nets for mass campaigns. Malar J. 2010;9:330 Epub 2010/11/23. doi: 10.1186/1475-2875-9-330 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pulford J, Hetzel MW, Bryant M, Siba PM, Mueller I. Reported reasons for not using a mosquito net when one is available: a review of the published literature. Malar J. 2011;10:83 doi: 10.1186/1475-2875-10-83 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Desrochers RE, Siekmans K, Berti PR, Bramhill K, Buchan SA, Battah GK, et al. Effectiveness of post-campaign, door-to-door, hang-up, and communication interventions to increase long-lasting, insecticidal bed net utilization in Togo (2011–2012): a cluster randomized, control trial. Malar J. 2014;13:260 doi: 10.1186/1475-2875-13-260 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deribew A, Birhanu Z, Sena L, Dejene T, Reda AA, Sudhakar M, et al. The effect of household heads training on long-lasting insecticide-treated bed nets utilization: a cluster randomized controlled trial in Ethiopia. Malar J. 2012;11:99 doi: 10.1186/1475-2875-11-99 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keating J, Hutchinson P, Miller JM, Bennett A, Larsen DA, Hamainza B, et al. A quasi-experimental evaluation of an interpersonal communication intervention to increase insecticide-treated net use among children in Zambia. Malar J. 2012;11:313 Epub 2012/09/11. doi: 10.1186/1475-2875-11-313 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macintyre K, Littrell M, Keating J, Hamainza B, Miller J, Eisele TP. Determinants of hanging and use of ITNs in the context of near universal coverage in Zambia. Health Policy Plan. 2012;27(4):316–25. Epub 2011/06/10. doi: 10.1093/heapol/czr042 . [DOI] [PubMed] [Google Scholar]
- 40.Kilian A, Balayo C, Feldman M, Koenker H, Lokko K, Ashton RA, et al. The effect of single or repeated home visits on the hanging and use of insecticide-treated mosquito nets following a mass distribution campaign—a cluster randomized, controlled trial. PLoS One. 2015;10(3):e0119078 doi: 10.1371/journal.pone.0119078 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steketee RW, Eisele TP. Is the scale up of malaria intervention coverage also achieving equity? PLoS One. 2009;4(12):e8409 Epub 2009/12/23. doi: 10.1371/journal.pone.0008409 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baume CA, Koh AC. Predictors of mosquito net use in Ghana. Malar J. 2011;10:265 doi: 10.1186/1475-2875-10-265 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Njau JD, Stephenson R, Menon M, Kachur SP, McFarland DA. Exploring the impact of targeted distribution of free bed nets on households bed net ownership, socio-economic disparities and childhood malaria infection rates: analysis of national malaria survey data from three sub-Saharan Africa countries. Malar J. 2013;12:245 Epub 2013/07/17. doi: 10.1186/1475-2875-12-245 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ugwu EO, Ezechukwu PC, Obi SN, Ugwu AO, Okeke TC. Utilization of insecticide treated nets among pregnant women in Enugu, South Eastern Nigeria. Nigerian journal of clinical practice. 2013;16(3):292–6. doi: 10.4103/1119-3077.113449 . [DOI] [PubMed] [Google Scholar]
- 45.Tchinda VH, Socpa A, Keundo AA, Zeukeng F, Seumen CT, Leke RG, et al. Factors associated to bed net use in Cameroon: a retrospective study in Mfou health district in the Centre Region. Pan Afr Med J. 2012;12:112 . [PMC free article] [PubMed] [Google Scholar]
- 46.Tinoaga Ouedraogo L, Ouedraogo I, Yameogo A, Ouedraogo V. Determinants of long-lasting insecticidal net use in Burkina Faso after a mass distribution in the Diebougou health district. Revue d'epidemiologie et de sante publique. 2013;61(2):121–7. doi: 10.1016/j.respe.2012.09.004 . [DOI] [PubMed] [Google Scholar]
- 47.Negash K, Haileselassie B, Tasew A, Ahmed Y, Getachew M. Ownership and utilization of long-lasting insecticide-treated bed nets in Afar, northeast Ethiopia: a cross-sectional study. Pan Afr Med J. 2012;13 Suppl 1:9 . [PMC free article] [PubMed] [Google Scholar]
- 48.O'Meara WP, Smith N, Ekal E, Cole D, Ndege S. Spatial distribution of bednet coverage under routine distribution through the public health sector in a rural district in Kenya. PLoS One. 2011;6(10):e25949 Epub 2011/10/25. doi: 10.1371/journal.pone.0025949 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Welch K, Fuster M. Barriers in access to insecticide-treated bednets for malaria prevention: an analysis of Cambodian DHS data. J Vector Borne Dis. 2012;49(1):1–7. Epub 2012/05/16. . [PubMed] [Google Scholar]
- 50.Thawani N, Kulkarni MA, Sohani S. Factors associated with coverage and usage of long-lasting insecticidal nets in madagascar. Journal of tropical medicine. 2009;2009:451719 doi: 10.1155/2009/451719 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Auta A. Demographic Factors Associated with Insecticide Treated Net use Among Nigerian Women and Children. North American journal of medical sciences. 2012;4(1):40–4. doi: 10.4103/1947-2714.92903 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ahmed SM, Zerihun A. Possession and usage of insecticidal bed nets among the people of Uganda: is BRAC Uganda Health Programme pursuing a pro-poor path? PLoS One. 2010;5(9). doi: 10.1371/journal.pone.0012660 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sundararajan R, Kalkonde Y, Gokhale C, Greenough PG, Bang A. Barriers to malaria control among marginalized tribal communities: a qualitative study. PLoS One. 2013;8(12):e81966 doi: 10.1371/journal.pone.0081966 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krezanoski PJ, Comfort AB, Tsai AC, Bangsberg DR. Households with young children and use of freely distributed bednets in rural Madagascar. International health. 2014;6(1):29–34. doi: 10.1093/inthealth/iht033 . [DOI] [PubMed] [Google Scholar]
- 55.Baume CA, Marin MC. Intra-household mosquito net use in Ethiopia, Ghana, Mali, Nigeria, Senegal, and Zambia: are nets being used? Who in the household uses them? Am J Trop Med Hyg. 2007;77(5):963–71. . [PubMed] [Google Scholar]
- 56.Kesteman T, Randrianarivelojosia M, Mattern C, Raboanary E, Pourette D, Girond F, et al. Nationwide evaluation of malaria infections, morbidity, mortality, and coverage of malaria control interventions in Madagascar. Malar J. 2014;13:465 doi: 10.1186/1475-2875-13-465 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.INSTAT. Enquête sur les Indicateurs du Paludisme (EIPM) 2013. Calverton, MD, USA: Institut National de la Statistique (INSTAT), Programme National de lutte contre le Paludisme (PNLP), Institut Pasteur de Madagascar (IPM) et ICF International.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
Data Availability Statement
The IRB/Ethics Committee approved protocol specifies the data for this evaluation were required to be turned over to the Ministry of Health/National Malaria Control Program in Madagascar and did not allow for public sharing of patient-level data. The previous Ministry of Health Malaria Program Director co-author has since left the programme and is not authorized to grant permission. None of the other co-authors are authorized to release the data at this time. The restrictions prohibiting the authors from making the minimal data set publicly available: the approved protocol procedures. Institutional/non-author contact information at which data can be requested: Access to the data can be made upon request from Dr. Mauricette Andriamananjara, Vector Control Team, National Malaria Control Program (Programme National de Lutte Contre le Paludisme) Madagascar by email: nambinisoa@yahoo.fr.