Placing infants supine for sleep is crucial to decreasing deaths. In this article, we report choices mothers make when deciding how to position infants for sleep.
Abstract
BACKGROUND AND OBJECTIVES:
The American Academy of Pediatrics recommends infants be placed supine for sleep. Our objectives in this study were to, in a nationally representative sample, examine (1) prevalence of maternal intention regarding infant sleeping position and of actual practice and (2) factors associated with their choices.
METHODS:
We recruited mothers from 32 US hospitals, oversampling African American and Hispanic mothers, in a nationally representative sample of mothers of infants aged 2 to 6 months. Survey questions assessed choice of usual infant sleeping position, all sleeping positions, intention for sleep position, as well as actual practice. Multivariable logistic regression analyses controlled for demographic, receipt of doctor advice, and theory of planned behavior variables (attitudes, subjective norms, and perceived control).
RESULTS:
Of the 3297 mothers, 77.3% reported they usually placed their infants in the supine position for sleep, but fewer than half reported that they exclusively did so. Only 43.7% of mothers reported that they both intended to and then actually placed their infants exclusively supine. African American mothers and those who did not complete high school were more likely to intend to use the prone position. Theory of planned behavior factors (attitudes, subjective norms, and perceived control) and doctor advice were associated with maternal choice.
CONCLUSIONS:
Not all mothers place their infants exclusively supine for sleep. Many mothers intend to place their infants supine yet often do not do so in actual practice. Factors potentially amenable to intervention including attitudes, subjective norms, and doctor advice are associated with intention and practice.
What’s Known on This Subject:
Each year infants die of unsafe sleep practices. Placing infants in the supine position for sleep reduces the risk of dying, yet infants continue to be placed in other than the supine position for sleep.
What This Study Adds:
Using a national sample, we present recent data about the prevalence of mothers’ intentions and also of actual practice regarding infant sleep position and uncover factors associated with this choice that are potentially amenable to change through educational interventions.
Sudden unexpected infant death, which includes sudden infant death syndrome (SIDS), remains the leading cause of postneonatal infant death in the United States.1 Between 2011 and 2014, there were 6683 infant deaths reported from SIDS (0.42/1000 live births) and an additional 3029 infant deaths from accidental suffocation and strangulation in bed (0.19/1000 live births).2 During this same period, the number of SIDS deaths varied by race and ethnicity, with the death rate for non-Hispanic African American infants of 0.76 per 1000 live births compared with Hispanic infants of 0.25 per 1000 live births.2 To decrease sudden unexpected infant death, the American Academy of Pediatrics (AAP) has recommended since 2005 that infants be placed exclusively in the supine position for sleep.3 Despite this recommendation, not all infants are placed supine for sleep. In our previous report in which we used data from the National Infant Sleep Position (NISP) study, a telephone survey, we found that in 2007, almost 72% of caregivers reported that they usually placed their infants in the supine position for sleep.4 The percentage placed in the supine position for sleep varied by race, with African American mothers least likely to usually place their infants supine for sleep. Like others, we found that the choice to place infants supine was also associated with the caregiver’s beliefs about comfort and choking.4,5 In addition, compared with mothers with less than a college education, those with a college education were more likely to place their infants in the supine position as were those who reported being told by a doctor to place their infants to sleep exclusively in the supine position.4 The NISP study, sponsored by the National Institutes of Health as a vehicle for following national trends related to safe infant sleep, included caregivers from across the country; however, as a telephone survey, it underrepresented important groups of infant caregivers (including African American and Hispanic mothers) and was therefore not felt to be the ideal way to track prevalence in behavior nationally.
For that reason, with continued sponsorship of the National Institutes of Health, we have replaced the NISP telephone survey methodology for tracking infant care practices with the new Study of Attitudes and Factors Effecting Infant Care (SAFE), which includes responses collected prospectively from a nationally representative sample of mothers recruited directly from hospital postpartum units. In addition to providing nationally representative data about the prevalence of supine sleep and other recommended safe sleep practices, the SAFE study included 2 other major advantages compared with the NISP study.
First, to understand better what drives maternal choices, we added questions on the basis of the theory of planned behavior,6 which posits that attitudes toward a behavior, subjective social norms, and perceptions about control over the behavior all have an impact on whether one has the intention to do a particular behavior. For example, attitude, subjective social norms, and perceived control might contribute to intention to exercise to lose weight,7,8 or relevant to our current report, intent to follow the recommendation to place their infant supine for sleep. Studies in which the theory of planned behavior is used are based on the supposition that behavior is a complex construct and that what people intend to do (lose weight or exercise) is not always aligned with what they actually do in practice. To our knowledge, no researchers have used behavior theory for an in-depth look at mothers’ choice of infant sleep position.
Second, as part of the SAFE survey, we collected information not only about usual sleep position chosen by the mother but also other positions the infants were placed to sleep. In this way, we extend our outcome variables beyond what has been done in previous national studies to examine intention and actual practice with regard to both the usual sleeping position and whether mothers chose to place their infants exclusively supine.
Therefore, our objectives in this current study were to, in a nationally representative sample, examine (1) the prevalence of both maternal intention regarding infant sleeping position and actual practice and (2) factors associated with their choices.
Methods
Sample
We used a 2-stage clustered design for obtaining a nationally representative sample of mothers of infants aged 2 to 6 months. In addition, to ensure an adequate sample size for making comparisons across racial and/or ethnic groups, we oversampled for Hispanic and non-Hispanic African American mothers. The first stage sampled 32 hospitals with at least 100 births reported in the past year by utilizing the 2010 American Hospital Association annual survey. Among the 32 hospitals initially selected, 69% agreed to participate; sampling procedures were used to identify replacement hospitals within the same stratum, which were based on location and population, to complete the full sample of 32 hospitals. Institutional review board approval was obtained at all participating institutions.
For the second stage, sampled hospitals were assigned targets for sampling and enrollment of Hispanic, non-Hispanic African American, and non-Hispanic other race mothers so that ∼3000 completed follow-up surveys were obtained from mothers of infants aged 2 to 6 months, including at least 25% of the surveys each from Hispanic and non-Hispanic African American mothers. Mothers were enrolled between January 2011 and March 2014. Mothers were eligible for enrollment if they spoke English or Spanish, lived in the United States, and would be caring for their infants 2 to 4 months after delivery.
Measures
At the time of enrollment, mothers who provided written informed consent completed an initial survey to collect demographics, including the mother’s age, education, and income level; pregnancy and delivery history including infant sex, birth weight, and maternal parity; and contact information for completing the follow-up survey either online or by telephone. Mothers completed the survey when their infants were >60 days old. After that point, they received weekly reminders until 180 days of age, after which time no additional reminders were sent. Mothers were allowed to complete the survey after this time and all adjusted analyses included infant age. Only 90 mothers completed the survey after 180 days, and the oldest infant was 227 days old at the time of completion of the survey.
The follow-up survey included questions about infant care practices, including information about intention and actual practice. Following the framework from the theory of planned behavior, there were also questions to assess maternal attitudes, subjective social norms, and perceived control.
About actual practice, mothers were asked: “Over the last 2 weeks, in what position have you USUALLY placed your baby to sleep?” Choices included: side, stomach, or back.
Mothers were also asked to choose all ways the infants were placed to sleep with the following statement: “Please CHECK ALL the ways that you have placed your baby to sleep over the last 2 weeks.” Choices included side, stomach, back, or other (which then required an explanation).
About doctor advice, mothers were first asked whether their infant’s doctor (or health care provider) gave advice about sleep positions (yes or no). Those who received advice from a doctor were then given 3 statements: “My baby’s doctor (or healthcare provider) thinks that I should place my baby to sleep on the side/stomach/back.” Agreement with each statement was given on a 7 point Likert scale (from definitely false to definitely true), with responses of 5, 6, and 7 categorized as the doctor endorsing a sleep position. On the basis of these questions, the doctor’s advice was categorized as no advice, advice consistent with recommendations (endorsing back sleep and not endorsing side or prone sleep), or advice not consistent with recommendations (not endorsing back sleep or endorsing side or prone sleep in addition to back sleep).
The following questions about intention, attitudes, subjective social norms, and perceived control were all asked by using a Likert scale from 1 (strongly disagree) to 7 (strongly agree).
About intention, mothers were asked to respond to the following statement: “Now, over the next 2 weeks, I plan to place my baby on the: side, stomach or back to sleep.” Responses of 5, 6, and 7 were categorized as intending to place their infant in that position. Mothers could intend to place their infant in >1 position.
About attitudes toward various sleep positions, mothers were asked to rate whether placing their infant on the back, side, or stomach would: “be healthy for my baby, be pleasant for my baby, be good for my baby, make my baby safer, make my baby more comfortable, keep my baby from choking.” For each set of questions, the average response was calculated, and if the average response was >4, then the mother was categorized as having a positive attitude toward that sleep position.
About subjective social norms, mothers were asked to respond to the following: “The people who are most important to me think that I should place my baby to sleep on the (Side, Back, Stomach).” Responses of 5, 6, and 7 were categorized as perceived positive social norms.
About perceived control, mothers were asked to respond to the following: “How I place my baby to sleep is mostly up to me.” Responses of 5, 6, and 7 were categorized as having perceived control.
Statistical Analysis
In all analyses, we accounted for the stratified 2-stage cluster sample design for both parameter estimates and SEs by using SAS (SAS 9.3; SAS Institute Inc, Cary NC) procedures for complex survey designs. Data were weighted to account for sampling probabilities and dropout and to reflect the national joint distributions of maternal age and race and/or ethnicity. As a check on the representativeness of our sample, weighted demographics were compared with the national demographics of mothers delivering between 2011 and 2013 by using National Center for Health Statistics data (Table 1).9
TABLE 1.
Weighted Demographic Characteristics of Study Population (N = 3297)
| Demographic | Na | Weighted (%) | US Vital Statistics (2011–2013) |
|---|---|---|---|
| Maternal age (y) | |||
| <20 | 275 | 7.5 | 7.8 |
| 20–29 | 1788 | 52.2 | 51.6 |
| ≥30 | 1234 | 40.3 | 40.6 |
| Maternal education | |||
| <HS | 478 | 12.8 | 17.1 |
| HS or GED | 833 | 23.5 | 25.1 |
| Some college | 1041 | 30.8 | 29.0 |
| ≥College degree | 932 | 32.9 | 28.8 |
| Parity | |||
| 1 | 1215 | 37.9 | 39.7 |
| 2 | 1095 | 33.7 | 31.5 |
| ≥3 | 978 | 28.4 | 28.3 |
| Maternal race and/or ethnicity | |||
| Non-Hispanic white | 1275 | 52.3 | 54.1 |
| Non-Hispanic African American | 828 | 12.9 | 14.8 |
| Hispanic | 912 | 26.0 | 23.0 |
| Other | 281 | 8.8 | 8.0 |
| Income ($) | |||
| <20 000 | 1158 | 29.5 | NA |
| 20 000–49 999 | 838 | 24.8 | NA |
| ≥50 000 | 577 | 19.8 | NA |
| Unknown | 724 | 26.0 | NA |
| Region | |||
| Northeast | 634 | 21.2 | NA |
| Midwest | 496 | 12.8 | NA |
| South | 1383 | 41.5 | NA |
| West | 784 | 24.5 | NA |
| Infant age (wk) | |||
| 8–11 | 2026 | 62.9 | NAb |
| 12–15 | 564 | 17.0 | NAb |
| 16–19 | 323 | 9.4 | NAb |
| ≥20 | 384 | 10.7 | NAb |
| Infant sex | |||
| Girl | 1685 | 50.7 | 48.8 |
| Boy | 1608 | 49.3 | 51.2 |
| Infant birth weight (g) | |||
| <2500 | 202 | 5.7 | 8.0 |
| ≥2500 | 3076 | 94.3 | 91.9 |
GED, general education development; HS, high school; NA, not available/applicable.
Not all numbers add up to 3297 because of missing data.
US Vital Statistics Data not applicable to infant age at time of survey response.
To describe the prevalence of sleep position practices, weighted percentages are given for all sleep positions reported by usual sleep position. To describe the association between sleep positions over the past 2 weeks and intended sleep position over the next 2 weeks, weighted percentages of all positions are reported by intended position.
To examine the degree of adherence to AAP recommendations for exclusively supine sleep, we divided mothers into 4 distinct and relatively large groups. We chose these groups because it allowed us to look at differences between mothers who intended and practiced the gold standard (intended and practiced supine) compared with those who did not. On the basis of a review of the data, we defined 4 distinct and relatively large groups in this regard. Group 1 is mothers who reported that they intended to place their infants to sleep only supine and always used this position in practice (Intend Only Supine, Practice Only Supine). Group 2 is those mothers who reported that they intended to place their infants only supine but in practice placed their infants in a position other than supine at least some of the time (Intend Only Supine, Practice Other). This group intended to follow the gold standard but did not do it. Group 3 is those mothers who reported that they intended to place their infant on the side or side and back (Intend Side or Side and Back). Group 4 is those mothers who included at least some prone sleeping as an intended position (Intend Includes Prone). Groups 3 and 4 were chosen because they did not intend to follow the gold standard. Multivariable multinomial logistic regression was used to examine associations between demographic factors, doctor advice, attitudes, subjective social norms, perceived control, and the 4 groups listed above.
Results
Study Population
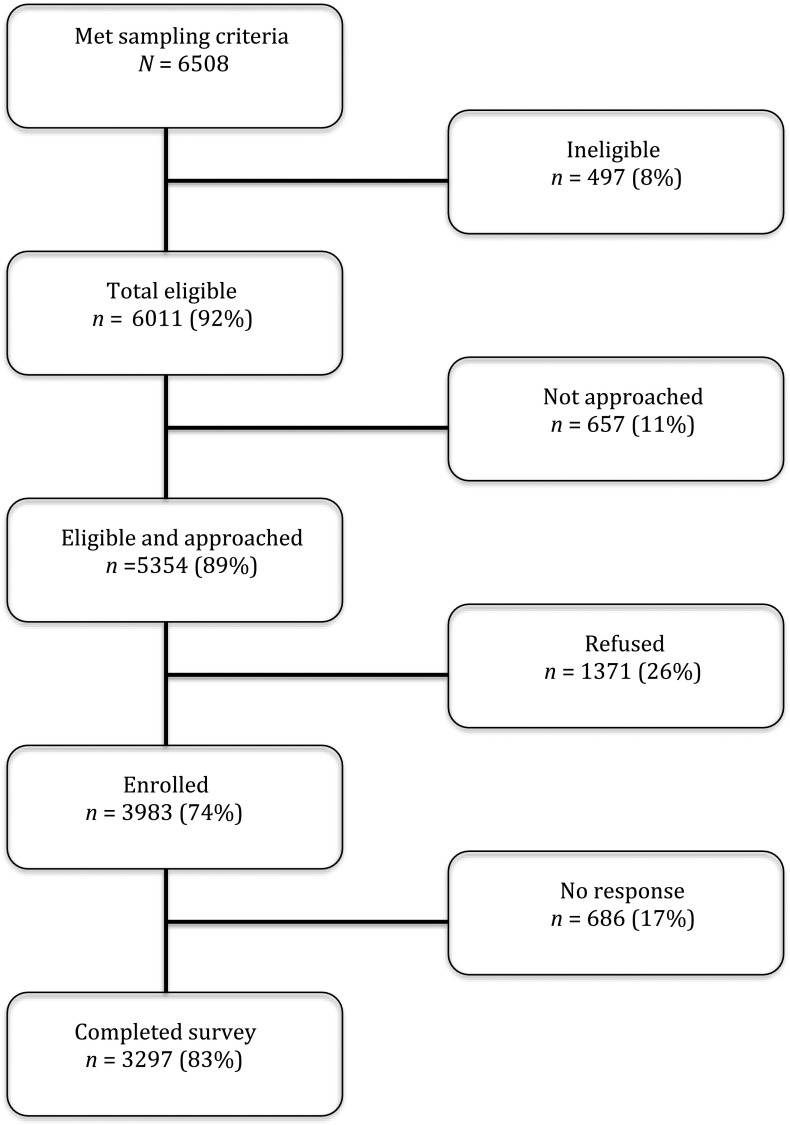
Of the 6508 mothers who met the sampling criteria, 6011 (92%) were eligible (Fig 1). Of those eligible, 5354 (89%) were approached. Of those approached, 3983 (74%) enrolled, and 3297 (83%) completed the survey. The reason for not approaching a mother was almost always related to staff availability. Mothers who were not approached did not differ from those who were approached with regards to either maternal age or maternal race and/or ethnicity, the only variables available from the study logs. After weighting and adjustment for cluster sampling, our sample demographic closely matched data from the National Center for Health Statistics from 2011 to 2013,9 except that in our sample, women with less than high school education were underrepresented (12.8% vs 17.1%) as were infants of low birth weight (5.7% vs 8.0%) (Table 1).
FIGURE 1.
Enrollment and follow-up.
Prevalence of Sleep Position Practices
In Table 2, we show weighted percentages for the practice the mothers reported using during the past 2 weeks. We show both usual practice and the practice used at least once. Of those surveyed, 2491 (77.3%) reported that they usually placed their infants supine for sleep, 14.1% side, and 7.8% prone. However, only 49.2% of mothers reported that they place their infants exclusively in the supine position.
TABLE 2.
All Sleep Positions Reported During Past 2 Weeks and Usual Position for the Same Period
| Usual Position During Past 2 wka | All Positions Reported to Be Used at Least Once During Past 2 wkb (N = 3297) | |||||||
|---|---|---|---|---|---|---|---|---|
| Only Supine (n = 1566) (49.2%), % | Supine and Side (n = 777) (23.0%), % | Only Side (n = 150) (4.6%), % | Supine and Prone (n = 231) (7.2%), % | Side and Prone (n = 106) (3.0%), % | Supine, Side, and Prone (n = 300) (8.0%), % | Only Prone (n = 88) (2.5%), % | Any Other (n = 79) (2.5%), % | |
| Supine (n = 2491) (77.3%) | 49.2 | 17.4 | 0.0 | 5.2 | 0.0 | 4.3 | 0.0 | 1.2 |
| Side (n = 491) (14.1%) | 0.0 | 5.6 | 4.6 | 0.0 | 1.3 | 2.3 | 0.0 | 0.3 |
| Prone (n = 284) (7.8%) | 0.0 | 0.0 | 0.0 | 2.1 | 1.7 | 1.3 | 2.5 | 0.2 |
| Other (n = 30) (0.8%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.8 |
Reported percentages are of all infants. All percentages are weighted. For all positions, any mother indicating “Other,” regardless of whether they also indicated supine, side, or prone, is included in the “Other” column.
This column contains actual N’'s, and column percentages, which total to 100% for the column.
Percentages from the overall sample.
Intention Versus Actual Practice
In Table 3, we show weighted percentages for the sleep position(s) mothers intended to use and their actual practice (any position used over the past 2 weeks). Of the respondents, 57.6% reported that they intended to place their infants only in supine position; however, in actual practice, only 43.7% of mothers reported intention and in actual practice followed the gold standard of placing their infants only in the supine position for sleep. Another relatively large group was the 26.1% (21.9% + 4.2%) of mothers who did not intend only supine (the gold standard) but rather intended to place their infants in the side or side and supine position. Finally, a smaller but important group was the 14.9% (2.5% + 1.9% + 8.1% + 2.4%) of mothers who intended some use of the prone position for placing their infants to sleep.
TABLE 3.
All Sleep Positions Reported During Past 2 Weeks and Intended Position During the Next 2 Weeks
| Intended Position(s) During Next 2 wks | All Positions Reported to Be Used at Least Once During Past 2 wka (N = 3297) | |||||||
|---|---|---|---|---|---|---|---|---|
| Only Supine (n = 1566) (49.2%), % | Supine and Side (n = 777) (23.0%), % | Only Side (n = 150) (4.6%), % | Supine and Prone (n = 231) (7.2%), % | Side and Prone (n = 106) (3.0%), % | Supine, Side, and Prone (n = 300) (8.0%), % | Only Prone (n = 88) (2.5%), % | Other (n = 79) (2.5%), % | |
| Only supine (n = 1811) (57.6%) | 43.7b | 7.3c | 0.2c | 3.7c | 0.1c | 1.3c | 0.2c | 1.2c |
| Supine and side (n = 758) (21.9%) | 3.8d | 13.4d | 1.5d | 0.5d | 0.1d | 1.9d | 0.1d | 0.5d |
| Only side (n = 133) (4.2%) | 0.1d | 0.8d | 2.3d | 0.1d | 0.5d | 0.3d | 0.1d | 0.1d |
| Supine and prone (n = 93) (2.5%) | 0.4e | 0.1e | 0.0e | 1.4e | 0.1e | 0.2e | 0.3e | 0.0e |
| Side and prone (n = 68) (1.9%) | 0.0e | 0.1e | 0.2e | 0.1e | 1.1e | 0.1e | 0.3e | 0.1e |
| Supine, side, and prone (n = 305) (8.1%) | 1.0e | 1.0e | 0.4e | 0.5e | 0.6e | 3.8e | 0.4e | 0.5e |
| Only prone (n = 82) (2.4%) | 0.1e | 0.0e | 0.0e | 0.7e | 0.5e | 0.1e | 1.0e | 0.1e |
| No intended position (n = 47) (1.4%) | 0.2 | 0.3 | 0.1 | 0.2 | 0.1 | 0.3 | 0.2 | 0.1 |
All percentages are weighted.
Percentages are overall percentages.
This cell includes mothers who intended Only Supine and reported Only Supine (ie, the gold standard).
These cells include mothers who intended Only Supine, but reported practices other than Only Supine.
These cells include mothers who intended either Only Side or Supine and Side.
These cells include mothers who intended either Only Prone or Prone plus some other position(s).
Factors Associated With Intention and Practice
In Table 4, we show factors associated with the 4 intention and practice categories identified above:
TABLE 4.
Multivariate Analysis of Factors Associated with Intentions and Practice
| Variablesa | n | All Positions Reported as Intended to Be Used (N = 3297)b | aORc Intend Only Supine, Practice Other (95% CI) | aORc Intend Side or Side and Supine (95% CI) | aORc Intend include Prone (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| % Intend Only Supine, Practice Only Supine | % Intend Only Supine, Practice Other | % Intend Side or Side and Supine | % Intend Includes Prone | |||||
| n = 1379 (43.7%) | n = 432 (13.9%) | n = 891 (26.1%) | n = 548 (14.9%) | |||||
| Maternal race | ||||||||
| White | 1275 | 51.2 | 15.9 | 18.8 | 12.5 | Ref | Ref | Ref |
| African American | 828 | 32.4 | 10.7 | 29.0 | 26.5 | 1.2 (0.83–1.71) | 1.7 (1.23–2.43) | 2.5 (1.57–3.85) |
| Hispanic | 912 | 33.9 | 11.6 | 39.1 | 14.7 | 1.5 (0.95–2.21) | 2.2 (1.42–3.28) | 1.5 (0.80–2.65) |
| Other | 281 | 43.9 | 13.5 | 27.4 | 13.0 | 1.0 (0.56–1.67) | 1.6 (0.74–3.34) | 1.4 (0.58–3.30) |
| Maternal age (y) | ||||||||
| 14–19 | 275 | 36.3 | 14.9 | 30.5 | 16.9 | 1.8 (0.81–4.17) | 1.2 (0.53–2.87) | 1.0 (0.42–2.62) |
| 20–24 | 795 | 37.7 | 13 | 31.2 | 17.2 | 1.6 (0.96–2.67) | 1.7 (0.97–3.17) | 1.4 (0.87–2.33) |
| 25–29 | 993 | 45.7 | 13.1 | 24.0 | 15.9 | Ref | Ref | Ref |
| 30–34 | 777 | 49.5 | 12.5 | 23.9 | 12.0 | 0.8 (0.52–1.10) | 1.0 (0.68–1.51) | 0.7 (0.37–1.35) |
| ≥35 | 457 | 42.8 | 18.8 | 24.0 | 13.3 | 1.2 (0.89–1.60) | 0.7 (0.38–1.19) | 0.7 (0.35–1.39) |
| Education | ||||||||
| <HS | 478 | 28 | 9.2 | 40.9 | 19.6 | 1.4 (0.78–2.47) | 1.7 (0.92–3.09) | 2.1 (1.16–3.73) |
| HS or GED | 833 | 41.5 | 10.5 | 30.5 | 16.7 | Ref | Ref | Ref |
| Some college | 1041 | 45.7 | 14.4 | 24.5 | 13.8 | 1.4 (0.99–1.88) | 1.1 (0.75–1.57) | 0.7 (0.42–1.31) |
| College grad | 624 | 49.4 | 15.7 | 19.0 | 14.7 | 1.6 (0.91–2.94) | 1.2 (0.69–2.02) | 1.2 (0.60–2.60) |
| Grad school | 308 | 49.6 | 22.0 | 18.0 | 9.1 | 3.0 (1.46–6.26) | 1.8 (0.87–3.92) | 1.2 (0.42–3.54) |
| Perceived control | ||||||||
| Up to mother | 3034 | 43.6 | 13.7 | 26.3 | 15.1 | Ref | Ref | Ref |
| Not up to mother | 254 | 44.8 | 16.4 | 24.6 | 12.5 | 1.0 (0.67–1.64) | 1.3 (0.60–2.81) | 3.5 (1.70–7.25) |
| Subjective norms | ||||||||
| Only supine | 1589 | 71.7 | 17.3 | 7.9 | 2.7 | Ref | Ref | Ref |
| Side or side and supine | 772 | 12.0 | 8.9 | 69.7 | 8.9 | 1.3 (0.84–2.11) | 9.0 (5.15–13.1) | 6.2 (3.39–11.2) |
| Any prone | 520 | 11.6 | 6.8 | 26.6 | 53.5 | 0.9 (0.50–1.58) | 4.0 (2.34–6.85) | 11.6 (7.24–18.7) |
| No positive | 255 | 27.4 | 14.7 | 24.2 | 25.2 | 1.6 (0.88–2.99) | 3.3 (1.87–5.81) | 5.4 (2.93–10.1) |
| Positive attitudes | ||||||||
| Only supine | 1474 | 79.4 | 14.2 | 4.5 | 1.6 | Ref | Ref | Ref |
| Side or side and supine | 1046 | 14.1 | 15.3 | 62.8 | 6.6 | 5.4 (3.63–7.96) | 26.3 (18.1–38.2) | 8.3 (5.24–13.3) |
| Any prone | 604 | 6.4 | 9.0 | 23.6 | 58.2 | 7.3 (3.84–13.8) | 29.6 (17.0–51.7) | 130 (71.8–236) |
| No positive | 56 | 36.9 | 11.5 | 10.3 | 29.3 | 1.3 (0.42–4.21) | 3.8 (0.96–15.0) | 18.2 (5.30–52.8) |
| Doctor advice | ||||||||
| Advice consistent with recommendation | 1773 | 62.5 | 16.2 | 12.9 | 7.7 | 0.8 (0.53–1.11) | 0.5 (0.36–0.67) | 0.6 (0.39–0.93) |
| No advice | 660 | 33.5 | 14.2 | 31.3 | 18.2 | Ref | Ref | Ref |
| Advice not consistent with recommendation | 819 | 8.8 | 7.9 | 53.5 | 28.5 | 1.3 (0.57–3.00) | 1.9 (1.07–3.32) | 2.6 (1.52–4.47) |
N = 47 mothers with no intended position included in the analysis but not included in the table because of small sample size. GED, general education development; HS, high school; Ref, reference.
In addition to all variables in the table the model adjusted for: maternal parity and marital status and infant sex, age, and birth weight categories.
The numbers associated with the demographics do not always add up to 3297 because of some missing data.
All aORs are compared with Intend Only Supine, Practice Only Supine group.
maternal intention to place the infant only supine and actual practice of only supine position (Intend Only Supine, Practice Only Supine);
maternal intention to place the infant only supine but actual practice is not only supine (intend only Supine, practice other);
maternal intention to place the infant on the side or side and supine (Intend Side or Side and Supine); and
maternal intention includes at least some prone as an intended position (Intend Includes Prone).
This multivariable analysis is shown in Table 4 and is adjusted for all variables in Table 4, including marital status and infant sex, age, and birth weight categories. All adjusted odds ratios (aORs) compare the indicated intention and practice to the gold standard (Intend Only Supine, Practice Supine). Of particular note, compared with white mothers, African American mothers were significantly more likely to intend to place their infants in the prone position at least some of the time (aOR 2.5; 95% confidence interval [CI], 1.57–3.85). Compared with those who did, those who did not complete high school were significantly more likely to intend to place their infants prone (aOR 2.1; 95% CI, 1.16–3.73).
Regarding receiving advice from a doctor compared with those who did not receive advice about sleep position from a doctor, those who received advice consistent with recommendations were less likely to report placement of their infants prone (aOR 0.6; 95% CI, 0.39–0.93) or side (aOR 0.5; 95% CI, 0.36–0.67), whereas those who received advice that was not consistent with recommendations were more likely to report placement of their infants prone (aOR 2.6; 95% CI, 1.52–4.47) or side (aOR 1.9; 95% CI, 1.07–3.32).
Examining the theory of planned behavior variables, we found that mothers who reported that the placement of their infant was not up to them (perceived control) were more likely to intend to place their infants in the prone position (aOR 3.5; 95% CI, 1.70–7.25). Of all the variables, subjective social norms and attitudes were most strongly associated with behaviors. Of particular note, those who reported that their social norms supported placing the infant in the prone position were much more likely to do so compared with those who felt that their social norms supported using only the supine position (aOR 11.6; 95% CI, 7.24–18.7). And, most remarkably, those who had positive attitudes about the prone sleep position (ie, agreed with the statements that putting the infant in the prone position for sleep would be healthy for the infant, be pleasant for the infant, be good for the infant, make the infant safer, make the infant more comfortable, and/or keep the infant from choking) were much more likely to choose the prone position (aOR 130; 95% CI, 71.8–236).
Discussion
In this nationally representative sample of mothers of infants, we found (as in our previous work) that ∼70% of the participants reported usually placing their infants in the supine position for sleep.4 In this study, we expanded on that finding by examining other sleeping positions and found that fewer than half chose the supine position exclusively. Position changes are of particular concern given studies revealing that infants who are unaccustomed to prone sleeping are especially at risk when placed in that position and that those placed to sleep on their sides can easily roll to the prone position.10
In addition, we found that the intention to place infants exclusively in the supine position does not always reflect what is done in practice. Only just <44% of mothers practiced what would be considered the gold standard, which is the intention to place the infant in the supine position for sleep and following that intention exclusively in actual practice. These results may not be surprising given our previous qualitative work, which showed that although many caregivers are aware that infants should be placed supine for sleep, they are not always able to do so for a variety of reasons, including concerns about infant comfort, choking, and general safety.11 Our findings are similar to those of other researchers related to intention versus practice.7 To our knowledge, ours is the first to show the difference between intention and practice with choice of infant sleeping position.
In the multiple logistic regression analysis, we found that compared with white mothers, African American mothers were significantly more likely to intend to place their infants in a position other than supine, expanding on our previous work, which showed similar results for usual sleep position.4 In addition, those with less than a high school education were more likely to intend to use the prone position for sleep. As in our previous work, we also found that the advice from a doctor influenced choice.4 Those who reported receiving advice from a doctor consistent with AAP recommendations were less likely to intend to place their infants in the prone or side positions.
The factors most strongly associated with sleep position were those from the theory of planned behavior highlighting that the mothers’ perception of control, subjective social norms, and attitudes impacted both intention and usual practice. Mothers who believed the choice of infant sleeping position was not in their control had >3 times the odds of including prone sleep in their intended practice. It is possible this may relate to the influence of other caretakers such as grandmothers or day care providers who are known to choose other than the supine position for sleep.12–14
Those who had positive attitudes toward the prone position had >100 times the odds of intending to use that position. Positive attitudes were determined by the answers to questions about infant safety, comfort, and choking. This finding supports findings from previous studies in which we found that these beliefs were important in determining choice of infant sleeping position.4 In addition, Gaydos et al15 showed that concerns about safety and other cultural norms were important in parent decisions about infant sleep. These beliefs persist and are potentially modifiable, so they should be considered an important part of any intervention to change practice.
Although the results of the study expand on the current understanding of the choice to place an infant in the supine position for sleep, several limitations should be acknowledged. First, the data come from maternal reports, which can be biased toward the desired response. It is reassuring that some of the results, such as usual supine sleep position, are similar to those found in previous studies.4 In addition, in the case of such a bias, we might be underestimating the use of unsafe sleep practices. Also, although this sample is strikingly close to nationally representative numbers on the basis of the National Center for Health Statistics,9 it does slightly underrepresent low birth weight infants and those mothers with less than a high school education. Finally, it is also important to recognize that although the intention to place an infant in the supine position for sleep and then actually placing that infant in that position is the gold standard for sleep position, it does not mean that all AAP infant care practice recommendations were being followed.
Conclusions
In this study, we demonstrate that it is still common for infants to be placed in unsafe sleep positions, and the use of unsafe sleeping positions increases when expanded beyond the usual choice. Mothers may intend to follow recommendations, but some do not follow through with these intentions. Maternal race and education continue to be factors associated with choice of infant sleeping position as does advice from a doctor. Factors that appear to be of equal or greater importance are those related to attitudes, subjective social norms, and perceived control, all of which can potentially be altered through educational interventions. Future research can be aimed at using these findings to inform and then to test the efficacy of educational interventions to change practice.
Acknowledgments
We thank the study staff at all 32 of the participating hospitals for their role in data collection and mother enrollment: Baylor University Medical Center, Texas; Baystate Medical Center, Massachusetts; Ben Taub General Hospital, Texas; Bethesda Memorial Hospital and Kidz Medical Services, Florida; Brookdale Hospital and Medical Center, New York; CamdenClark Medical Center, West Virginia; Delaware County Memorial Hospital, Pennsylvania; Geisinger Regional Medical Center, Pennsylvania; Genesys Regional Medical Center, Michigan; Hamilton Medical Center, Georgia; Jersey Shore University Medical Center, New Jersey; Johns Hopkins Hospital and Medical Center, Maryland; Kaweah Δ Health Care District, California; Lake Charles Memorial Hospital, Louisiana; Medical Center of Arlington, Texas; Moreno Valley Community Hospital, California; Mount Carmel, Ohio; Natchitoches Regional Medical Center, Louisiana; Nashville General Hospital, Tennessee; Northcrest Medical Center, Tennessee; Riverside County Regional Medical Center, California; Riverside Regional Medical Center, Virginia; Rush-Copley Medical Center, Illinois; Saint Francis Hospital and Medical Center, Connecticut; Saint Joseph Hospital, California; Saint Mary’s Health Care, Michigan; Socorro General Hospital, New Mexico; Sutter Roseville Medical Center, California; Tacoma General Hospital, Washington; Texas Health Presbyterian Hospital Plano, Texas; University of California, Davis Medical Center, California; and Wheaton Franciscan Healthcare, Wisconsin.
Glossary
- AAP
American Academy of Pediatrics
- aOR
adjusted odds ratio
- CI
confidence interval
- NISP
National Infant Sleep Position
- SAFE
Study of Attitudes and Factors Effecting Infant Care
- SIDS
sudden infant death syndrome
Footnotes
Dr Colson conceptualized and designed the study and drafted the manuscript; Ms Geller was involved in overseeing data gathering, helped conceptualize the design of the study, and reviewed and revised the manuscript; Dr Heeren conceptualized the methods of the study, conducted the analyses, and reviewed and revised the manuscript; Dr Corwin conceptualized and designed the study, was involved with the design of the methods and analyses, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, grant U10HD059207. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2017-2068.
References
- 1.Matthews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat Rep. 2015;64(9):1–30 [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention Infant Deaths. Available at: https://wonder.cdc.gov/lbd.html. Accessed July 6, 2017
- 3.Moon RY; Task Force on Sudden Infant Death Syndrome . SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162940. [DOI] [PubMed] [Google Scholar]
- 4.Colson ER, Rybin D, Smith LA, Colton T, Lister G, Corwin MJ. Trends and factors associated with infant sleeping position: the national infant sleep position study, 1993-2007. Arch Pediatr Adolesc Med. 2009;163(12):1122–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathews AA, Joyner BL, Oden RP, Alamo I, Moon RY. Comparison of infant sleep practices in African-American and US Hispanic families: implications for sleep-related infant death. J Immigr Minor Health. 2015;17(3):834–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211 [Google Scholar]
- 7.Plotnikoff RC, Lubans DR, Costigan SA, McCargar L. A test of the theory of planned behavior to predict physical activity in an overweight/obese population sample of adolescents from Alberta, Canada. Health Educ Behav. 2013;40(4):415–425 [DOI] [PubMed] [Google Scholar]
- 8.McDermott MS, Oliver M, Simnadis T, et al. The theory of planned behaviour and dietary patterns: a systematic review and meta-analysis. Prev Med. 2015;81:150–156 [DOI] [PubMed] [Google Scholar]
- 9.Center for Disease Control and Prevention About Natality, 2007-2015. Available at: https://wonder.cdc.gov/natality-current.html. Accessed April 10, 2017
- 10.Mitchell EA, Thach BT, Thompson JMD, Williams S. Changing infants’ sleep position increases risk of sudden infant death syndrome. New Zealand Cot Death Study. Arch Pediatr Adolesc Med. 1999;153(11):1136–1141 [DOI] [PubMed] [Google Scholar]
- 11.Colson ER, McCabe LK, Fox K, et al. Barriers to following the back-to-sleep recommendations: insights from focus groups with inner-city caregivers. Ambul Pediatr. 2005;5(6):349–354 [DOI] [PubMed] [Google Scholar]
- 12.Ottolini MC, Davis BE, Patel K, Sachs HC, Gershon NB, Moon RY. Prone infant sleeping despite the “Back to Sleep” campaign. Arch Pediatr Adolesc Med. 1999;153(5):512–517 [DOI] [PubMed] [Google Scholar]
- 13.Moon RY, Patel KM, Shaefer SJ. Sudden infant death syndrome in child care settings. Pediatrics. 2000;106(2 pt 1):295–300 [DOI] [PubMed] [Google Scholar]
- 14.Aitken ME, Rose A, Mullins SH, et al. Grandmothers’ beliefs and practices in infant safe sleep. Matern Child Health J. 2016;20(7):1464–1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaydos LM, Blake SC, Gazmararian JA, Woodruff W, Thompson WW, Dalmida SG. Revisiting safe sleep recommendations for African-American infants: why current counseling is insufficient. Matern Child Health J. 2015;19(3):496–503 [DOI] [PubMed] [Google Scholar]