In this randomized controlled trial, we examined the effect of early LGG infant supplementation in decreasing the risk of childhood eczema.
Abstract
OBJECTIVES:
To determine if probiotic administration during the first 6 months of life decreases childhood asthma and eczema.
METHODS:
We conducted a randomized, double-blind controlled trial of Lactobacillus rhamnosus GG (LGG) supplementation on the cumulative incidence of eczema (primary end point) and asthma and rhinitis (secondary end points) in high-risk infants. For the first 6 months of life, intervention infants (n = 92) received a daily dose of 10 billion colony-forming units of LGG and 225 mg of inulin (Amerifit Brands, Cromwell, CT), and control infants (n = 92) received 325 mg of inulin alone. We used survival analysis methods to estimate disease incidences in the presence or absence of LGG and to estimate the efficacy of LGG in delaying or preventing these diseases.
RESULTS:
Infants were accrued over a 6-year period (median follow-up: 4.6 years; 95% retention rate at 2 years). At 2 years of age, the estimated cumulative incidence of eczema was 30.9% (95% confidence interval [CI], 21.4%–40.4%) in the control arm and 28.7% (95% CI, 19.4%–38.0%) in the LGG arm, for a hazard ratio of 0.95 (95% CI, 0.59–1.53) (log-rank P = .83). At 5 years of age, the cumulative incidence of asthma was 17.4% (95% CI, 7.6%–27.1%) in the control arm and 9.7% (95% CI, 2.7%–16.6%) in the LGG arm, for a hazard ratio of 0.88 (95% CI, 0.41–1.87) (log-rank P = .25).
CONCLUSIONS:
For high-risk infants, early LGG supplementation for the first 6 months of life does not appear to prevent the development of eczema or asthma at 2 years of age.
What’s Known on This Subject:
On the basis of the hygiene hypothesis, probiotic exposure may affect immune system development and subsequent risk for allergic disease; however, recent trials of the probiotic Lactobacillus rhamnosus GG supplementation in decreasing the risk of childhood eczema and asthma have yielded mixed results.
What this Study Adds:
For high-risk infants, early Lactobacillus rhamnosus GG supplementation does not appear to prevent eczema or asthma development at 2 years of age.
Probiotics are defined as “live microorganisms which when administered in adequate amounts confer a health benefit on the host.”1 Researchers in recent studies of early probiotic supplementation in infancy have investigated the potential benefit in decreasing the risk of allergic disease and early markers of asthma, such as eczema. On the basis of the hygiene hypothesis, which suggests that the absence of infectious exposure at a critical point in immune system development could lead to greater risk of allergic disease, it is thought that probiotic exposure could theoretically affect immune system development and reduce the subsequent risk for the development of allergic disease.2
In a randomized, controlled, double-blind study of 159 newborns in Finland, Kalliomäki et al3 found that early Lactobacillus rhamnosus GG (LGG) exposure (1 × 1010 colony-forming units of LGG per day) as a probiotic supplement in both pregnant women and their newborns led to a lower 2-year incidence of atopic disease, including eczema. In addition, researchers of follow-up studies found that such effects were sustained past infancy.4,5 However, in a similar study from Germany, Kopp et al6 found no significant difference in the development of atopic dermatitis (odds ratio: 0.96; 95% confidence interval [CI]: 0.38–2.33) by 24 months of age. Although researchers in both studies recruited 105 women whose infants would be at high risk for asthma, the study populations differed geographically and by rates of breastfeeding exposure. For example, the average duration of breastfeeding was much longer in the study by Kopp et al6 (9.2 versus 6.4 months). The differences in these 2 study results suggest that the effects of probiotic supplementation may vary based on underlying environmental exposures.7,8
We conducted the Trial of Infant Probiotic Supplementation (TIPS) Study to determine if probiotic administration during the first 6 months of life can decrease the cumulative incidence of eczema and asthma in childhood. The study was conducted in a racially and ethnically diverse, urban area in the United States and, unlike previous studies, focused on infant supplementation only. We hypothesized that 6 months of infant probiotic supplementation would decrease the incidence of eczema in children at higher risk for allergic disease and, secondarily, would decrease the incidence of asthma and rhinitis.
Methods
The TIPS Study is a randomized, double-masked, parallel-arm, controlled trial designed to evaluate the effectiveness of daily LGG supplementation for the first 6 months of life to decrease the incidence of eczema, which is a potential early marker of asthma.
A description of the TIPS Study protocol has been previously published.9 Because of the extended time required to recruit patients, the average age of the participants was much older than anticipated. As a result, there were some modifications to the original protocol. We originally used “wheezing” as a secondary end point because it is part of an algorithm to determine the likelihood of later development of asthma in young children.10 Because of the older average participant age and because wheezing was considered an intermediate end point to help determine the likelihood of asthma, for this analysis, we used doctor-diagnosed asthma as a more clinically meaningful secondary outcome. We studied asthma incidence through 5 years of age instead of 3 years of age.
The TIPS Study protocol was approved by the University of California, San Francisco, Committee on Human Research.
Participants
We recruited pregnant women from the San Francisco, California, metropolitan area to identify potential participants. Eligible newborns had at least 1 biological parent who reported a history of asthma. Parents had to speak and read English or Spanish. After initial recruitment occurred during pregnancy, we completed final parental written, informed consent; screening; and random assignment of infants within 4 days after the infant’s birth. Infant exclusion criteria included any major congenital birth deformities, acute illness at enrollment, or any condition affecting food intake or metabolism.
Group assignment was based on the output from a computer-generated randomization program that was accessed by the study coordinator once eligibility was confirmed and consent was obtained. Group allocation and the randomization sequence were concealed from the study staff and investigators to further eliminate conscious or unconscious selection bias. Subjects, parents, study staff, and investigators were blinded to group assignment.
Description of the Intervention
The intervention arm received a daily capsule of 10 billion colony-forming units of LGG and 225 mg of inulin for the first 6 months of life (Amerifit Brands, Cromwell, CT). This is the same probiotic strain and dose used in 2 previously published trials.4,6 The control arm received a 6-month course of daily capsules that contained 325 mg of inulin. Caregivers were instructed to dissolve the supplement (active or control) in 2 mL of pumped breast milk, infant formula, or water and feed it to the infants via oral syringe. To promote breastfeeding, all participating families were encouraged to breastfeed and were provided a breast pump. If families decided to use formula, we offered to provide a partially hydrolyzed whey infant formula, which did not have a probiotic or prebiotic supplement (Good Start Supreme; Nestlé, Vevey, Switzerland), to standardize the type of infant formula exposure and also limit the potential risk of atopic disease.11
The control capsule did not differ from the active capsule in terms of appearance, taste, smell, or texture. After the end of the intervention period at 6 months, parents were surveyed to determine if they could correctly identify whether they received the active or control capsules.
End Points
The primary outcome measure was the incidence of eczema within 2 years of birth. Secondary outcomes were incidences of asthma and allergic rhinitis within 5 years of birth.
The diagnosis of eczema was based on repeated parental reports of the diagnosis of eczema by a clinician on 2 occasions or the presence of eczema on physical examination on the basis of standard criteria.12 Similarly, diagnoses of asthma and allergic rhinitis were based on repeated parental reports of the diagnosis by a clinician on 2 occasions. The clinicians were blinded to the participants’ group assignment.
The assessment of an outcome in each participant began at randomization and continued until either the outcome was diagnosed (“failure time”), until the study ended, or until a participant discontinued follow-up without a diagnosis (“censoring time”). Because participants who were accrued earlier had more assessments, we avoided bias by using survival analysis methods that account for variable lengths of follow-up.
Data Collection
Demographic, household, and family history of allergic disease were collected from parents after the birth of an infant. Household characteristics included educational attainment of the parents, household income, and type of insurance. We reviewed each mother’s obstetric medical record to confirm the method of delivery.
To assess study outcomes, physical examinations were conducted by study clinicians at 1, 3, 6, 12, and 24 months of age to assess for the presence of eczema. Additionally, we surveyed parents by telephone monthly during the first year of life and semiannually thereafter. Parents were asked about any diagnoses of asthma, allergic rhinitis, or eczema by a health care professional. Although it is possible that a new diagnosis of eczema, asthma, or rhinitis could have been identified during a study visit, in all cases, a child’s primary care provider was the clinician who first diagnosed and documented the presence of eczema or asthma.
To assess for potential confounding factors, parents were also asked about feeding practices. Each month during the first year of life, parents were asked about infant formula exposure with the question, “How are you feeding your baby?” Options included “breast milk only,” “formula only,” “combination,” “other,” or “does not apply.” We then asked the specific name of the formula and asked the parent to “please estimate how many ounces your baby drinks (or drank) per day.” We also asked parents to estimate “how many total weeks has your baby been taking the formula since we last spoke?”
The combination-fed infants were recoded into either breast milk-only or formula-only categories by using the following approach: We developed a total fluid-intake estimate for the typical infant for each month in the first year of life based on the typical weight of a male or female infant that age,13,14 the recommended energy intake for that age, and an estimate for the approximate caloric density of formula of 20 kcal/oz.15 Thus, for a 1-month-old infant, the typical fluid intake would be estimated to be 18 oz per day. If the infant’s parents described the feeding pattern as combination but fed <50% of the total expected daily volume for age from formula, then for the purposes of the analyses, the infant was considered a breastfed infant for that month; otherwise, the infant was considered a formula-fed infant for that month. No infant was considered breastfed for any month after formula-feeding began, according to this definition. In addition, if a parent reported exclusive breastfeeding in a month after a month of combination-feeding, the all previous combination months were considered breastfeeding months.
Sample Size Calculation
The study was designed to accrue participants for 2 years, follow infants for the incidence of outcomes for 2 additional years, and have 90% power by using a 2-sided 0.05-level log-rank test, which accounts for differing lengths of follow-up across participants. We based our sample size estimate on a previous study by Kalliomäki et al,3 who reported that patients exposed to a probiotic intervention were less likely to develop eczema, which is a marker of increased risk for asthma, compared with controls (23% vs 46%). At a control 2-year cumulative incidence rate of 46%, 40 patients per arm would provide 90% power to detect a hazard ratio (HR) of 0.42. Gehring et al16 studied the effects of house dust endotoxins on 1884 healthy German newborns, of which 16% developed eczema within 12 months; assuming a constant hazard, the 2-year cumulative incidence among controls would be 29.4%. At this rate, 100 patients per arm would provide 90% power to detect an HR of 0.615 (a reduction from 29% to 18%) and 80% power to detect an HR of 0.655 (a reduction from 29% to 19%). To be conservative, we relied on the lower estimate of eczema incidence among controls in selecting the sample size for the study.
Analysis
Demographic and household characteristics and the prevalence of perinatal risk factors for atopic diagnoses of infant participants are described by study arm by using percentages for categorical variables and means and SDs for continuous variables.
To determine the effects of LGG on the times to cumulative incidence of each study outcome (eczema, asthma, and rhinitis), we conducted modified intention-to-treat analyses with all participants who received treatment analyzed in the study arm to which they had been randomly assigned.17 We used survival analysis approaches to account for differing times to incident events across participants, assuming that censoring times were noninformative. Methods per arm included the Kaplan-Meier plots to estimate cumulative incidence rates and 95% CIs as landmark follow-up times, and methods to compare arms included Cox proportional hazard models to obtain maximum likelihood estimates of HRs and 95% CIs and nonparametric log-rank tests to estimate statistical significance.18
We conducted exploratory analyses to determine if LGG efficacy for prevention of atopic diagnoses (eczema or asthma) depended on risk factors. We used Cox models to examine the effect of the risk factor on the outcome and the risk-factor–adjusted treatment effect for the following 2 risk factors: the type of delivery (cesarean versus vaginal) and duration of breastfeeding exposure, treated as a time-dependent covariate to account for exposure ≤12 months of age.
To examine whether participants’ families remained blinded to study arm throughout the intervention period, we conducted within-arm tests of the null hypothesis that correct identification of study arm was random in 50% of each sample. We used SAS 9.4 (SAS Institute Inc, Cary, NC) for our analyses.
Results
From 2006 to 2012, we approached a total of 6458 potential mothers during pregnancy; of these, 3760 were not interested, and 2480 were not eligible primarily because neither parent reported a history of asthma. Of the 218 eligible mothers recruited during the third trimester, 203 (87%) allowed their eligible children to be randomly assigned into the study. Of the 203 randomly assigned infants, 10% of the mothers per arm discontinued their participation before treatment initiation, leaving 184 infants who were randomly assigned and initiated treatment of analyses. Infants were accrued over a 6-year period, resulting in a median follow-up time of 4.6 years with 95% of the infants followed for at least 2 years, 77% for at least 3 years, and 46% for at least 5 years. The last enrolled infant was followed for at least 2 years. During the course of the study, there were no major adverse events reported in either arm.
The intervention and control arms were similar in terms of the characteristics of the participants as well as their parents or households (Tables 1 and 2). Parents could select multiple races when describing their infants. For example, for 149 (81%) infants, parents selected “white”; however, for 57 of these infants, the parents selected an additional race in describing their infants. Overall, for 59 (32%) infants, the parents selected more than 1 race category. For 25% of the infants, the parents selected Hispanic in their descriptions of the infants’ ethnicity. In our study sample, parents reported high educational attainment and income. Specifically, the majority of mothers of the infants enrolled in the TIPS Study had received a college education. The mothers had mean age of 32.8 years when their children were born. Twenty one percent of households involved reported an income of up to $50 000 per year, and 12.5% reported earning >$200 000 per year.
TABLE 1.
Infant Participant Characteristics by Study Arm
| Control (n = 92) | Probiotic (n = 92) | |
|---|---|---|
| Boys | 48 (52%) | 44 (48%) |
| Racea | ||
| White | 77 (85%) | 72 (78%) |
| African American | 10 (11%) | 14 (15%) |
| American Indian, Alaskan Native | 12 (13%) | 10 (11%) |
| Asian | 19 (21%) | 22 (24%) |
| Pacific Islander | 4 (4%) | 3 (3%) |
| Other | 8 (32%) | 18 (20%) |
| Hispanic ethnicity | 19 (21%) | 27 (29%) |
| Gestational age, wk (SD) | 38.9 (1.3) | 39.0 (1.4) |
| Birth weight, g (SD) | 3440 (442) | 3427 (506) |
| Cesarean delivery | 21 (23%) | 27 (29%) |
| Mean number of months breastfeeding in first year of life (SD) | 7.5 (5.1) | 7.7 (4.9) |
| Breastfeeding exposure | ||
| None | 20 (22%) | 16 (17%) |
| <12 mo | 31 (34%) | 29 (32%) |
| ≥12 mo | 41 (45%) | 47 (51%) |
The percentage of infants in each race category is >100%. Fifty-nine (32%) parents of these infants selected more than 1 race when describing their infants.
TABLE 2.
Parental and Household Characteristics
| Control (n = 92) | Probiotic (n = 92) | |
|---|---|---|
| Paternal historya | ||
| Mean age at delivery, y | 34.9 (5.7) | 34.6 (6.9) |
| History of asthma | 35 (40%) | 42 (47%) |
| History of rhinitis | 29 (33%) | 30 (34%) |
| History of eczema | 15 (17%) | 22 (25%) |
| Maternal history | ||
| Mean age at delivery, y | 33.0 (5.2) | 32.6 (5.8) |
| History of asthma | 68 (74%) | 68 (74%) |
| History of rhinitis | 41 (45%) | 41 (45%) |
| History of eczema | 34 (37%) | 25 (27%) |
| Maternal educationb | ||
| Up to high school, vocational school | 8 (9%) | 11 (12%) |
| Some college | 17 (18%) | 14 (15%) |
| College graduate | 29 (32%) | 31 (34%) |
| Graduate school | 38 (41%) | 36 (39%) |
| Household income per y, $ | ||
| <10 000 | 5 (6%) | 8 (9%) |
| 10 001–50 000 | 13 (15%) | 12 (14%) |
| 50 001–100 000 | 16 (18%) | 18 (21%) |
| 100 001–150 000 | 24 (27%) | 19 (22%) |
| 150 001–200 000 | 20 (23%) | 19 (22%) |
| >200 000 | 11 (12%) | 12 (14%) |
| Household insurance | ||
| Self-pay | 0 | 0 |
| Private insurance | 74 (81.5%) | 69 (75.0%) |
| Medicaid, SCHIP, HFP | 17 (18.5%) | 22 (23.9%) |
| Military or other | 0 | 1 (1.1%) |
HFP, Healthy Families Program; SCHIP, State Children’s Health Insurance Program.
Data missing from 9 fathers.
Data missing from 1 mother.
In terms of the perinatal and postnatal course, ∼1 in 4 infants (26%) were born via cesarean delivery. For the 184 infants who did not withdraw before treatment initiation, the median duration of breastfeeding was 10.5 months and was similar in both arms (log-rank P = .48). By arm, 22% and 17% of infants in the control and probiotic arms, respectively, were weaned during the first month of life; 60% per arm were breastfed for at least 6 months; and 45% and 51% of the infants in the control and probiotic arms were breastfed for at least 12 months, respectively.
Analyses of Outcomes
Among 184 participants over the entire 6-year observation period, eczema was diagnosed in 68 as of age 2 years, and asthma was diagnosed in 27 as of age 5 years. Because there were few cases of allergic rhinitis (n = 9; with 5 in the control arm and 4 in the intervention arm), we did not analyze the cumulative incidence.
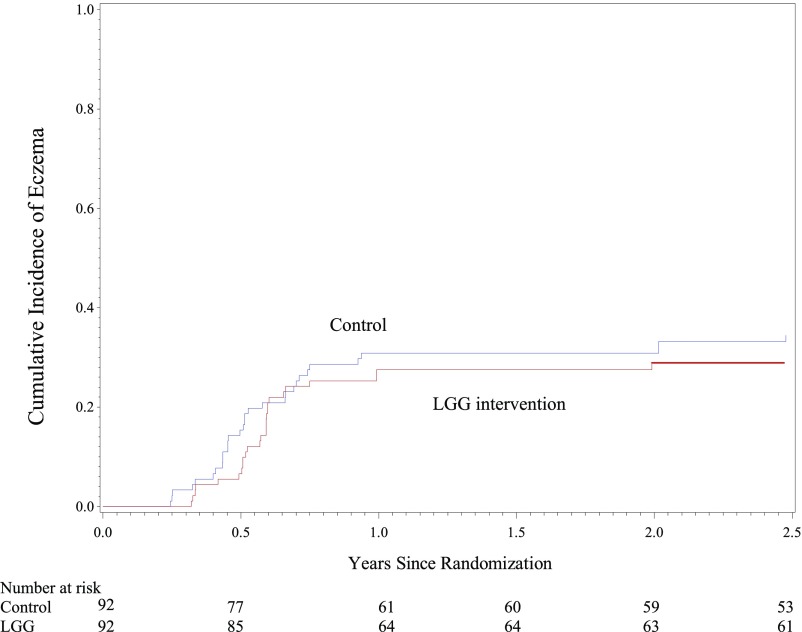
The cumulative incidence of eczema increased during the first year of life and then plateaued (Fig 1). At 6 months of age, the estimated cumulative incidence of eczema was 15.4% (95% CI, 8.0%–22.8%) in the control arm and 6.6% (95% CI, 1.5%–11.7%) in the LGG arm. By 2 years of age, the estimated cumulative incidence of eczema was 30.9% (95% CI, 21.4%–40.4%) in the control arm and 28.7% (95% CI, 19.4%–38.0%) in the LGG arm, yielding an HR of 0.95 (95% CI, 0.59–1.53; log-rank P = .83).
FIGURE 1.
Cumulative incidence of eczema by the Kaplan-Meier method. At 2 years of age, the estimated cumulative incidence of eczema was 30.9% (95% CI, 21.4%–40.4%) for the control arm and 28.7% (95% CI, 19.4–38.0%) for the LGG arm, for an HR of 0.95 (95% CI, 0.59–1.53) (log-rank P = .83).
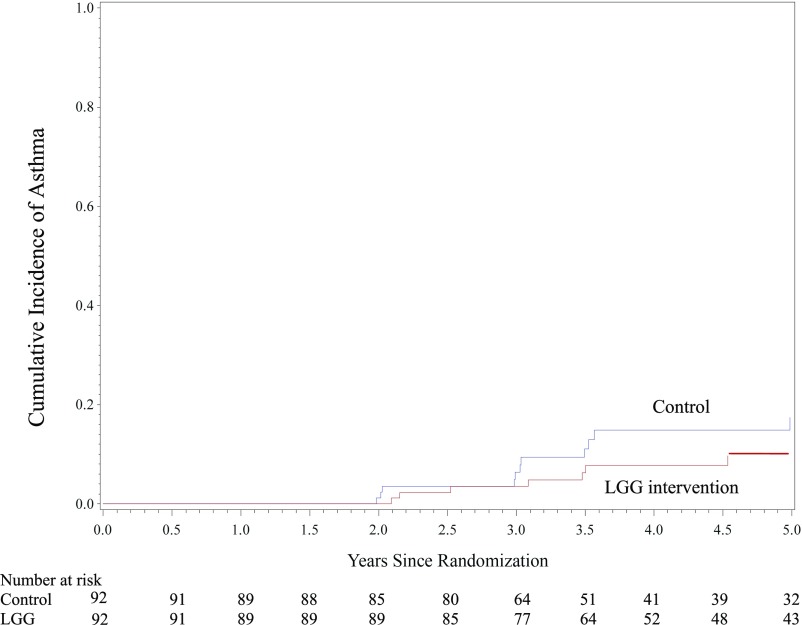
In contrast to eczema, the first case of asthma was diagnosed in a 2-year-old child (Fig 2). As of 5 years of age, the cumulative incidence of asthma was 17.4% (95% CI, 7.6%–27.1%) in the control arm and 9.7% (95% CI, 2.7%–16.6%) in the LGG arm. The mean HR for asthma over the course of 5 years of follow-up was 0.88 (95% CI, 0.41–1.87; log-rank P = .25).
FIGURE 2.
Cumulative incidence of asthma by the Kaplan-Meier method. At 5 years of age, the cumulative incidence of asthma was 17.4% (95% CI, 7.6%–27.1%) in the control arm and 9.7% (95% CI, 2.7%–16.6%) in the LGG arm, for an HR of 0.88 (95% CI, 0.41–1.87) (log-rank P = .25).
Among the 27 participants diagnosed with asthma, 18 (67%) had an earlier diagnosis of eczema compared with 50 (32%) of 157 not diagnosed with asthma during follow-up. As expected, the risk of asthma was greater among children who previously had eczema (HR 3.64; 95% CI, 1.66–7.96).
We found the numbers of participants who were exclusively formula fed (n = 36) or born via cesarean delivery (n = 48) were too low to draw any firm conclusions from any exploratory analyses of the combined effect of LGG and the lack of breastfeeding or LGG and cesarean delivery. There were no major adverse events in either group.
Blinding of Participants to Study Arm
After the intervention period was complete (when a child was 6 months of age), we asked parents if they thought their children had been randomly assigned to the control or the probiotic arm. In the control arm, 38 of 92 (41.2%) correctly guessed their assignment (P > .05). In the probiotic arm, 46 of 92 (50%) correctly guessed their assignment (P > .05).
Discussion
Environmental factors during early infancy can affect immune system development and subsequent risk for allergic disease.19 The hygiene hypothesis suggests that the absence of infectious exposure at a critical point in immune system development leads to a greater risk for later development of atopic disease and asthma.20 In addition, a dearth of diversity in the infant intestinal microbiota has been associated with later increased risk of allergic disease.21 Early infant supplementation with specific probiotic strains may be one potential mechanism to take advantage of the hygiene hypothesis and influence the risk of allergic disease early in life. However, we found that in infants with a parent with asthma, probiotic supplementation during the first 6 months of life did not affect the incidence of eczema or asthma at 2 years of age.
There have been mixed results regarding the effectiveness of early infant LGG supplementation in decreasing the likelihood of eczema.3,6 In this study, the LGG supplementation only occurred in the postnatal phase, and prenatal intervention combined with postnatal intervention may be important in ensuring the effect of LGG. Maternal supplementation with LGG during the third trimester may be required to prime the maternal gastrointestinal and genitourinary tracts because the subsequent infant gastrointestinal colonization is associated with the characteristics of the maternal vaginal and intestinal microbiota.22 Similarly, a postnatal component may also be important for an effect. A randomized controlled trial of prenatal LGG supplementation, but not postnatal supplementation, for 250 pregnant women carrying infants at high risk for allergic disease did not have an effect on later risk of eczema.23
Other environmental factors also may affect the success of the LGG intervention. For example, mode of birth may influence the establishment of the infant gut microbiota and later risk for atopic disease.24 In addition, researchers in several studies suggest that elective cesarean delivery is associated with an increased risk of asthma.25 Similarly, breastfeeding has a major influence on infant gut colonization through a variety of mechanisms, including vertical transfer of breast milk–associated microbial species.26,27 Continued breastfeeding may overshadow the effect of daily supplementation with a single probiotic stain. The LGG intervention conducted by Kopp et al,6 which had a negative result, included a study population with an average duration of breastfeeding of more than 9 months, compared with the positive results from Kalliomäki et al,3 which included a study population with an average duration of breastfeeding of 6.4 months. In our study population, a large proportion of infants were exclusively breastfed for the first 6 months. In addition, the median duration of breastfeeding was 10.5 months, which more closely matches the population studied by Kopp et al.6 Given the multitude of factors that may affect the risk of allergic disease, the effect of supplementation with a single probiotic species may only be discernable in high-risk infants who are also born into high-risk scenarios because of altered gastrointestinal microbiota development (eg, cesarean delivery, early broad spectrum antibiotic exposure,28,29 and perhaps lack of breast milk exposure).
A strength of this study evolved from its slow accrual, which extended the expected median follow-up time from 2 to 4.3 years and allowed for estimation of the incidence of asthma among children who were at high risk of eczema at birth. In addition, the TIPS Study retention rates were high, as indicated by the long median follow-up time, which ensured absence of confounding because of select bias associated with loss to follow-up. Compared with similar studies, the TIPS Study sample of infants was more ethnically and racially diverse than other studies of LGG in infants to date, reflecting a large, urban population in the United States. However, the infants’ mothers were older, more affluent, and more educated than the typical population. As a result, it is difficult to extrapolate the results of this study to rural communities or low-income, urban settings. Finally, parents appeared to remain blinded to study arm throughout the intervention period.
Among the limitations of this study, the sample size calculation relied on previous findings reported by Kalliomäki et al3 and Gehring et al.16 Our control-arm, 2-year cumulative incidence of eczema (31%) measured in San Francisco was similar to that of Gehring et al16 (29%), which was measured in Munich and Leipzig, Germany, but was much lower that of Kalliomäki et al3 (46%), which was measured in Turku, Finland. The TIPS Study was designed to have 80% power to detect an HR <0.66, corresponding with a 10% absolute reduction in the 2-year cumulative incidence of eczema attributed to probiotic use.
In our study, the cumulative incidence of asthma at 5 years of age was estimated to be 17.4% in the control group and 9.7% in the probiotic group; however, the HR based on this difference was not statistically significant. A much larger sample size might be able to provide sufficient power to detect a difference in the cumulative incidence of asthma at 5 years of age.
Although we anticipated that the effect of LGG may be modified by the type of delivery, we did not stratify by delivery mode before randomization, and the study included only a limited number of infants born by cesarean delivery (n = 48); furthermore, the percentage of infants born via cesarean delivery in our study population was lower than the US national average (26% vs 32%).30 As a result, we did not have sufficient power to fully explore this issue. Finally, similar to other studies, we recruited children at high risk to increase the likelihood of seeing an effect in the intervention. Although the results of this study can only be extrapolated to those children born to at least 1 parent with asthma, it is assumed that any effects for lower-risk infants (eg, infants born to parents without asthma) are probably lower.
Conclusions
In this study, which included infants with high breastfeeding rates and low cesarean delivery rates, our results do not support the use of early-life LGG probiotic supplementation for the prevention of asthma or eczema for all children at high risk.
Glossary
- CI
confidence interval
- HR
hazard ratio
- LGG
Lactobacillus rhamnosus GG
- TIPS
Trial of Infant Probiotic Supplementation
Footnotes
Dr Cabana conceptualized and designed the study, designed the data collection instruments, and drafted the initial manuscript; Ms McKean designed the study, supervised and coordinated the overall data collection, and critically reviewed the manuscript; Drs Caughey, Wong, and Leong supervised the data collection at one of the sites and critically reviewed the manuscript; Drs Fong and Lynch helped design the study and critically reviewed the manuscript; Dr Boushey helped design the study, designed the data collection instruments, and critically reviewed the manuscript; Dr Hilton designed the study analysis plan and critically reviewed the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered at ww.clinicaltrials.gov (identifier NCT00113659).
FINANCIAL DISCLOSURE: Amerifit Brands (Cromwell, CT) provided complimentary Lactobacillus rhamnosus GG and placebo capsules to the study investigators; Nestlé (Vevey, Switzerland) provided complimentary, partially hydrolyzed whey infant formula for those infants enrolled who were not exclusively breastfed; and the authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the Clinical and Translational Science Institute (UL1 RR024131) at the University of California, San Francisco, and by the National Institutes of Health, HL 080074. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Lynch is a co-founder and serves on the board of directors for Siolta Therapeutics, a microbiome therapeutics company; Dr Cabana has served as a paid scientific consultant to BioGaia, Mead Johnson Nutrition, Nestlé, and Wyeth (unrelated to the current study), has received grant funding from Nestec (unrelated to the current study), and has served on the Merck Speakers Bureau for topics focused on medication adherence (unrelated to the current study); and the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Hill C, Guarner F, Reid G, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroentrol Hepatol. 2014;11(8):506–514 [DOI] [PubMed] [Google Scholar]
- 2.Noverr MC, Huffnagle GB. The ‘microflora hypothesis’ of allergic diseases. Clin Exp Allergy. 2005;35(12):1511–1520 [DOI] [PubMed] [Google Scholar]
- 3.Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. 2001;357(9262):1076–1079 [DOI] [PubMed] [Google Scholar]
- 4.Kalliomäki M, Salminen S, Poussa T, Arvilommi H, Isolauri E. Probiotics and prevention of atopic disease: 4-year follow-up of a randomised placebo-controlled trial. Lancet. 2003;361(9372):1869–1871 [DOI] [PubMed] [Google Scholar]
- 5.Kalliomäki M, Salminen S, Poussa T, Isolauri E. Probiotics during the first 7 years of life: a cumulative risk reduction of eczema in a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2007;119(4):1019–1021 [DOI] [PubMed] [Google Scholar]
- 6.Kopp MV, Hennemuth I, Heinzmann A, Urbanek R. Randomized, double-blind, placebo-controlled trial of probiotics for primary prevention: no clinical effects of Lactobacillus GG supplementation. Pediatrics. 2008;121(4). Available at: www.pediatrics.org/cgi/content/full/121/4/e850 [DOI] [PubMed] [Google Scholar]
- 7.Lodge CJ, Tan DJ, Lau MX, et al. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):38–53 [DOI] [PubMed] [Google Scholar]
- 8.Wegienka G, Havstad S, Zoratti EM, Kim H, Ownby DR, Johnson CC. Combined effects of prenatal medication use and delivery type are associated with eczema at age 2 years. Clin Exp Allergy. 2015;45(3):660–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cabana MD, McKean M, Wong AR, Chao C, Caughey AB. Examining the hygiene hypothesis: the trial of infant probiotic supplementation. Paediatr Perinat Epidemiol. 2007;21(suppl 3):23–28 [DOI] [PubMed] [Google Scholar]
- 10.Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med. 2000;162(4 pt 1):1403–1406 [DOI] [PubMed] [Google Scholar]
- 11.von Berg A, Filipiak-Pittroff B, Krämer U, et al. ; GINIplus Study Group . Allergies in high-risk schoolchildren after early intervention with cow’s milk protein hydrolysates: 10-year results from the German Infant Nutritional Intervention (GINI) study. J Allergy Clin Immunol. 2013;131(6):1565–1573 [DOI] [PubMed] [Google Scholar]
- 12.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol. 1980;92:s44–s47 [Google Scholar]
- 13.Centers for Disease Control and Prevention Boys weight-for-age percentiles, birth to 12 months. 2010. Available at: www.cdc.gov/growthcharts/who/boys_length_weight.htm. Accessed August 23, 2016
- 14.Centers for Disease Control and Prevention Girls weight-for-age percentiles, birth to 12 months. 2010. Available at: www.cdc.gov/growthcharts/who/girls_length_weight.htm. Accessed August 23, 2016
- 15.Engorn B, Flerlage J. The Harriet Lane Handbook, 20th Edition. Table 23.4. Philadelphia, PA: Elsevier, Saunders; 2015 [Google Scholar]
- 16.Gehring U, Bolte G, Borte M, et al. ; LISA Study Group. Lifestyle-Related Factors on the Immune System and the Development of Allergies in Childhood . Exposure to endotoxin decreases the risk of atopic eczema in infancy: a cohort study. J Allergy Clin Immunol. 2001;108(5):847–854 [DOI] [PubMed] [Google Scholar]
- 17.Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011;2(3):109–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481 [Google Scholar]
- 19.Prescott SL, Macaubas C, Smallacombe T, Holt BJ, Sly PD, Holt PG. Development of allergen-specific T-cell memory in atopic and normal children. Lancet. 1999;353(9148):196–200 [DOI] [PubMed] [Google Scholar]
- 20.Strachan DP, Taylor EM, Carpenter RG. Family structure, neonatal infection, and hay fever in adolescence. Arch Dis Child. 1996;74(5):422–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arrieta MC, Stiemsma LT, Dimitriu PA, et al. ; CHILD Study Investigators . Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med. 2015;7(307):307ra152. [DOI] [PubMed] [Google Scholar]
- 22.Rautava S, Luoto R, Salminen S, Isolauri E. Microbial contact during pregnancy, intestinal colonization and human disease. Nat Rev Gastroenterol Hepatol. 2012;9(10):565–576 [DOI] [PubMed] [Google Scholar]
- 23.Boyle RJ, Ismail IH, Kivivuori S, et al. Lactobacillus GG treatment during pregnancy for the prevention of eczema: a randomized controlled trial. Allergy. 2011;66(4):509–516 [DOI] [PubMed] [Google Scholar]
- 24.Penders J, Gerhold K, Stobberingh EE, et al. Establishment of the intestinal microbiota and its role for atopic dermatitis in early childhood. J Allergy Clin Immunol. 2013;132(3):601–607.e8 [DOI] [PubMed] [Google Scholar]
- 25.Huang L, Chen Q, Zhao Y, Wang W, Fang F, Bao Y. Is elective cesarean section associated with a higher risk of asthma? A meta-analysis. J Asthma. 2015;52(1):16–25 [DOI] [PubMed] [Google Scholar]
- 26.Gueimonde M, Laitinen K, Salminen S, Isolauri E. Breast milk: a source of bifidobacteria for infant gut development and maturation? Neonatology. 2007;92(1):64–66 [DOI] [PubMed] [Google Scholar]
- 27.Cabrera-Rubio R, Collado MC, Laitinen K, Salminen S, Isolauri E, Mira A. The human milk microbiome changes over lactation and is shaped by maternal weight and mode of delivery. Am J Clin Nutr. 2012;96(3):544–551 [DOI] [PubMed] [Google Scholar]
- 28.Sun W, Svendsen ER, Karmaus WJ, Kuehr J, Forster J. Early-life antibiotic use is associated with wheezing among children with high atopic risk: a prospective European study. J Asthma. 2015;52(7):647–652 [DOI] [PubMed] [Google Scholar]
- 29.Russell SL, Gold MJ, Hartmann M, et al. Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep. 2012;13(5):440–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin JA, Hamilton BE, Osterman MJ. Births in the United States, 2014. NCHS Data Brief. 2015;(216):1–8 [PubMed] [Google Scholar]