We explored the longitudinal tracking of BMI z scores among children with severe obesity in the Bogalusa Heart Study.
Abstract
BACKGROUND:
Although the Centers for Disease Control (CDC) growth charts are widely used in studies of childhood obesity, BMI z scores are known to be inaccurate at values greater than the 97th percentile.
METHODS:
We used longitudinal data from 6994 children in the Bogalusa Heart Study who were examined multiple times to compare tracking of 3 BMI metrics: BMI-for-sex/age z score (BMIz), BMI expressed as a percentage of the 95th percentile (%BMIp95), and levels of BMI z score that adjust for the compression of very high z scores (adjusted z score [BMIaz]). The later 2 metrics, unlike BMIz, do not have an upper limit. The mean interval between examinations was 2.8 years. We were particularly interested in these metrics among children with obesity or severe obesity (%BMIp95 ≥120%).
RESULTS:
Although there was little difference in the tracking of the 3 metrics in the overall sample, among 247 children with severe obesity, the correlation of BMIz levels between examinations (r = 0.46) was substantially weaker than those for BMIaz and %BMIp95 (r = 0.65 and 0.61). Age-stratified analyses indicated that the weak tracking of BMIz was particularly evident before the age of 10 years (r = 0.36 vs 0.57 and 0.60). Several children with severe obesity showed BMIz decreases between examinations despite having BMI increases of over 5.
CONCLUSIONS:
Among children with severe obesity, the tracking of BMIz is weak. This is because of the constraints in converting very high BMIs into z scores based on the CDC growth charts. Rather than using BMIz, it would be preferable to express very high BMIs relative to the CDC 95th percentile or to use BMIaz.
What’s Known on This Subject:
The tracking of BMI levels among children and adolescents has been well documented. However, there is little information the usefulness of BMIz values to summarize the tracking among children who have severe obesity.
What This Study Adds:
Among children with severe obesity, BMIz traced less strongly (r = 0.46) than did metrics that expressed BMI relative to the 95th percentile or were based on z scores that did not have an upper bound (r = ∼0.6).
The 2000 Centers for Disease Control and Prevention (CDC) growth charts1,2 are widely used to classify obesity (BMI ≥95th percentile for a child’s sex and age) among 2- to 19-year-olds. In these growth charts, 10 percentiles of BMI between the third and 97th were estimated by using various smoothing methods.1,3 These percentiles were then used to derive 3 parameters (power transformation to achieve normality [L], median [M], and dispersion [S]) that allow for the calculation of a BMI-for-sex/age z score (BMIz) and percentile for any child.4,5
However, the use of the LMS parameters in the CDC growth charts for very high BMIs can result in estimates that that differ substantially from those that are actually observed3,6 and constrains the maximum BMIz that is attainable at a given sex and age.7,8 These limitations have resulted in the classification of severe obesity as a BMI ≥120% of the 95th percentile rather than a percentile greater than the 95th.6,9 A BMI of 120% of the 95th percentile corresponds to a BMI of ∼35 among 16- to 18-year-olds.
Although investigators have emphasized the limitations of analyzing BMIz,8,10–13 many continue to focus on z scores among children with very high BMIs.14–16 We have previously shown that among children with severe obesity, BMI expressed as a percentage of the 95th percentile (%BMIp95) is a better measure of adiposity than are very high BMIz values.17 The objective of the current analyses is to compare the longitudinal tracking of several BMI metrics among children. We include data from 11 638 2- to 17-year-olds who were examined in the Bogalusa Heart Study between 1973 and 1994.
Methods
Study Sample
The Bogalusa Heart Study examines the natural history of risk factors for cardiovascular disease18 in a biracial community (Ward 4 of Washington Parish, LA), with 7 cross-sectional studies of schoolchildren conducted from 1973 to 1974 through 1992 to 1994.19 The population of Washington Parish during that period was ∼20 000, and, on average, the authors of each study examined ∼3500 children. For simplicity, we refer to each study by using the year in which the examinations were first conducted.
The authors of the first (1973) study examined 5- to 14-year-olds, and the authors of subsequent studies extended the upper age through 17 years. Preschool-aged children (n = 714) were also examined in 1973. There were 27 212 examinations conducted among 11 665 children in these 7 studies. Informed consent was obtained from participants, and study protocols were approved by human subjects’ review committees.
For the current study, we excluded 95 records with missing data for weight or height and 23 records in which a girl reported being pregnant. We also excluded 18 records for which the body size measurements were considered to be implausible,20 on the basis of extreme values of the modified z scores21,22 for weight (<−5 or >8 SDs), height (<−5 or >4 SDs), or BMI (<−4 or >8 SDs). We also excluded 13 children for whom height decreased by more than 1 inch between examinations and 8 records in which BMIz differed substantially from sex- and age-adjusted levels of both arm circumference and triceps skinfold, possibly indicating a transcription error. This resulted in a sample consisting of 27 060 examinations from 11 624 children for the analyses.
The sample for the longitudinal analyses includes 6977 children who were examined in 2 or more cross-sectional studies. Because of the panel design of the Bogalusa Heart Study, ∼60% of the children who had severe obesity at one examination were not included in the longitudinal analyses because they were over 17 years of age at the time of the next examination, or they chose to not participate.
BMI Metrics
Height was measured to the nearest 0.1 cm and weight was measured to the nearest 0.1 kg; BMI was calculated as kilograms per meter squared. BMIz was calculated by expressing a child’s BMI relative to children in the CDC growth charts1 on the basis of the following formula.4,5 Values of L, M, and S varied according to a child’s sex and age.
Because values of L ranged from −1.3 to −3.5, if a child’s BMI was large relative to the M BMI, (BMI ÷ M)L would approach 0 and the maximum BMIz would therefore be (−1) ÷ (L × S). For example, the L and S values for an 8-year-old boy are −3.2 and 0.10, respectively, resulting in an 8-year-old boy with a BMI of 40 having a BMIz of 2.86 SDs. The maximum attainable BMIz for that sex and age, even if the BMI were >100, is 3.05 SDs.
Because of the upper limit of BMI-for-age results in the mapping of very high BMIs into a compressed range that varies by sex and age, we also examined the use of modified z scores.20 These modified z scores, which have been used to identify outliers, were calculated by dividing the difference between the M BMI and the observed BMI by a fixed SD (one-half of the distance between 0 and 2 z scores).21 For the current analyses, we replaced BMIz values that were <−1.88 or <1.88 (the 3rd and 97th percentiles) with these modified z scores; we referred to this metric as an adjusted z score (BMIaz). Levels of BMIz and BMIaz were identical between the 3rd and 97th percentiles.
Obesity is defined as a BMI ≥ the 95th percentile of the CDC growth charts.1,23 We referred to a BMI that is expressed as a percentage of the (sex- and age-specific) 95th percentile as %BMIp95, and severe obesity was defined as a %BMIp95 ≥120.9 For example, an 8-year-old boy (for whom the 95th percentile is 20.5) with a BMI of 25.3 would have a %BMIp95 of 124 (100 × 25.3/20.5), a BMIz of 2.3 SDs, and a BMIaz of 2.8 SDs. We referred to children who had a %BMIp95 between 100 and 119 as having moderate obesity.
Statistical Methods
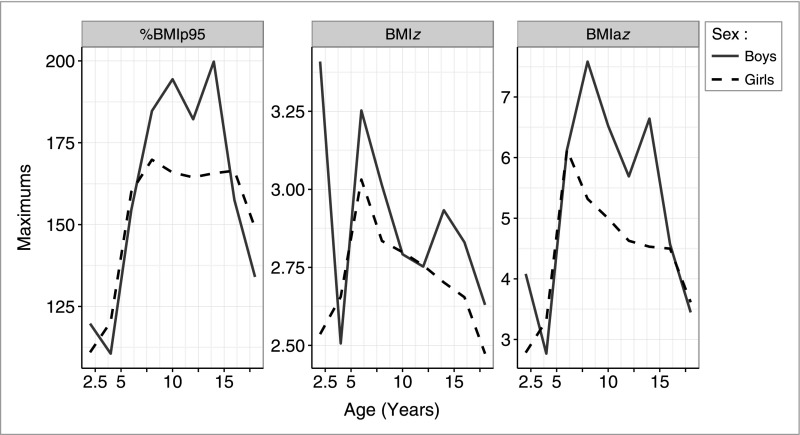
All analyses were performed in R.24 Descriptions of various characteristics were contrasted across 3 categories (children without obesity, children who had moderate obesity, and those with severe obesity) on the basis of %BMIp95. Maximum values of BMIz, BMIaz, and %BMIp95 by sex and age group are illustrated.
We also examined that longitudinal tracking (correlation) between consecutive examinations, separated by at least 3 months, for the 6977 children who were examined multiple times; the number of examinations among these children ranged from 2 to 6 (mean: 3.7). For each child, we examined the longitudinal correlations for each BMI metric between consecutive examinations. For example, a child who was examined at ages 6, 9, and 12 years would contribute 2 observations for this analysis: the correlation between BMIs at ages 6 and 9 years, as well as that between ages 9 and 12 years. For these analyses of longitudinal correlations, we excluded 89 examinations that occurred within 3 months of the previous examination, resulting in a total of 15 303 pairs of observations.
It should be realized that because we focused on attained BMI in the longitudinal analyses, we used metrics that are based on growth charts derived from cross-sectional data. We did not assess the velocity of BMI change.25,26
Results
Table 1 shows levels of various characteristics according to BMI status in the 27 016 examinations. Approximately 91% of the examined subjects did not have obesity at the time of examination, 7% had moderate obesity, and 2% had severe obesity (%BMIp95 ≥120). As compared with subjects who did not have obesity, those with severe obesity were older (mean difference: 10 months), tended to be examined in later years of the study, and were more likely to be African American. Among children with severe obesity, the mean BMI was 32, the mean BMIz was 2.4 SDs, and the mean BMIaz was +3.0 SDs. The lower value for mean BMIz among children with severe obesity reflects the compression of very high BMIs into a narrow range that is bounded.
TABLE 1.
Descriptive Characteristics According to Obesity Status for 27 060 Examinations in the Bogalusa Heart Study
| Children Without Obesity | Children With Moderate Obesity (%BMIp95 of 100–119) | Children With Severe Obesity (%BMIp95 ≥120) | |
|---|---|---|---|
| N (examinations) | 24 603 | 1804 | 609 |
| Year of examination | 1979 (1976–1985) | 1982 (1977–1988) | 1985 (1978–1992) |
| Girls, % | 49 ± 0.3a | 49 ± 1 | 47 ± 2 |
| African Americans, % | 38 ± 0.3 | 36 ± 1 | 45 ± 2 |
| Age, y | 10.9 (7.9 to13.8)b | 11.1 (8.6 to 13.6) | 11.7 (9.2 to 14.2) |
| BMI | 17.3 (15.6 to 19.7) | 25.4 (22.6 to 28.3) | 32.0 (28.4 to 35.3) |
| BMIz (SDs) | 0.0 (−0.6 to 0.6) | 1.9 (1.8 to 2.0) | 2.4 (2.3 to 2.5) |
| BMIaz (SDs) | 0.0 (−0.6 to 0.6) | 1.8 (1.8 to 2.1) | 3.0 (2.7 to 3.5) |
| %BMIp95, % | 76.2 (69.6 to 83.6) | 106.7 (102.8 to 112.3) | 129.0 (123.7 to 136.9) |
The 27 016 examinations were from 11 624 children.
Values of categorical variables are mean ± SE.
Values of the continuous variables are M (25th and 75th percentiles).
Figure 1 shows the maximum values in the Bogalusa Heart Study for %BMIp95, BMIz, and BMIaz within sex and 2-year age groups. Although plots of maximum values are ragged, the maximum %BMIp95 value increased rapidly up to ∼10 years of age, remained constant until age 15, and then decreased. In contrast, the highest BMIz (middle panel) value (3.4 SDs) was observed for a 2-year-old boy who had a BMI of 22 and a %BMIp95 of 120. Aside from this 1 child, the maximum BMIz generally increased up to ∼8 years and then decreased. The maximum values of BMIaz (right panel) were typically 1.5 to 2 times higher than those for BMIz and more closely resembled the sex and age differences in %BMIp95 than did BMIz. The highest BMIaz value (7.6 SDs) was seen for a 7-year-old boy who had a BMI of 35.6 and a %BMIp95 of 185; his BMIz was 3.0 SDs.
FIGURE 1.
Maximum values of the BMI metrics among children in the Bogalusa Heart Study by sex and 2-year age groups.
We then examined the longitudinal tracking (Table 2) of the BMI metrics between examinations among the 15 303 pairs of examinations from the children who were examined multiple times. (The mean interval between examinations was 2.8 years.) Among all children (top rows), there were few differences among the metrics (r = 0.86–0.89). However, among children who had had obesity (N = 909) or severe obesity (N = 247) at the initial examinations, correlations for BMIz were consistently weaker than those for BMI, BMIaz, and %BMIp95. Among children with severe obesity, for example, correlations ranged from r = 0.47 (BMIz) to r = 0.65 (BMIaz).
TABLE 2.
Longitudinal Correlations Between the Initial and Final Levels of the BMI Metrics Among 15 428 Pairs of Examinations
| BMI Metric | ||||||
|---|---|---|---|---|---|---|
| N | BMI | BMIz | BMIaz | %BMIp95 | ||
| All children | Overall | 14 147 | 0.86 | 0.89 | 0.89 | 0.88 |
| Obesitya | 909 | 0.72 | 0.61 | 0.73 | 0.70 | |
| Severe | 247 | 0.64 | 0.46 | 0.65 | 0.61 | |
| <10 y | Overall | 7448 | 0.83 | 0.87 | 0.87 | 0.87 |
| Obesity | 466 | 0.69 | 0.58 | 0.72 | 0.70 | |
| Severe | 114 | 0.66 | 0.36 | 0.60 | 0.57 | |
| ≥10 y | Overall | 6699 | 0.89 | 0.90 | 0.91 | 0.91 |
| Obesity | 443 | 0.70 | 0.64 | 0.73 | 0.72 | |
| Severe | 133 | 0.58 | 0.56 | 0.67 | 0.64 | |
Values represent the correlation between consecutive levels of each BMI metric between ages 5 and 17.9 y. For children who were examined more than 2 times, each pair of adjacent examinations contributed to the analysis.
Obesity is classified as a %BMIp95 ≥100. Of the 1156 children with obesity, 909 had moderate obesity (%BMIp95 of 100–119) and 247 had severe obesity (%BMIp95 ≥120).
Age-stratified analyses (middle and bottom sections of Table 2) indicated that the tracking of BMIz was particularly weak before age 10 years. Among the 114 children <10 years with severe obesity, the correlation between levels of BMIz over time was only r = 0.36 versus r = 0.57 to 0.66 for the other metrics. Smaller differences were seen among older children with severe obesity, but BMIz and BMI showed the weakest longitudinal correlations (r = 0.57–0.58), whereas stronger correlations were seen for %BMIp95 (r = 0.64) and BMIaz (r = 0.67).
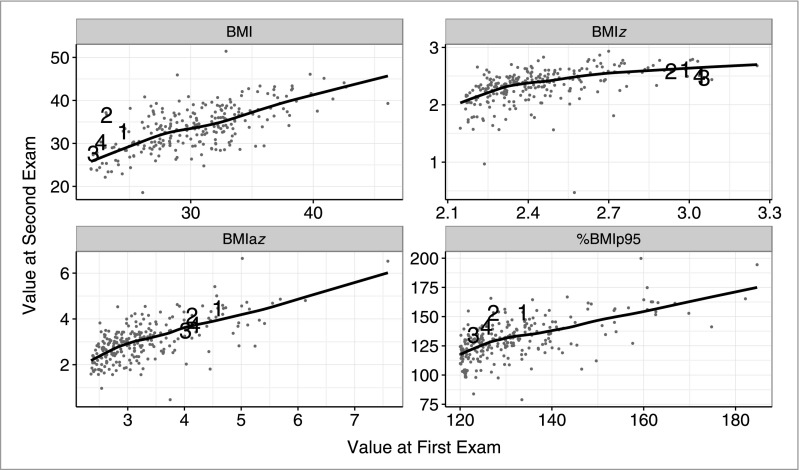
These associations among the 247 children with severe obesity are further explored in Fig 2, with levels at the second examination (y-axis) plotted against those at the initial examination (x-axis). In contrast to the plots for BMI, BMIaz, and %BMIp95, the association for BMIz was curvilinear, with the line becoming almost horizontal at very high levels of BMIz at the first examination. In addition, most of the very high BMIz values at the second examination were compressed into a relatively narrow range. Of the 23 children with the highest BMIz levels at the initial examination (≥2.75 SDs), all showed a BMIz decrease between examinations.
FIGURE 2.
Initial and subsequent levels of BMI, BMIz, BMIaz, and %BMIp95 among children who had severe obesity at the initial examination. The points labeled 1 through 4 represent the children who showed a BMIz decrease of more than 0.33 SDs between examinations but an increase in %BMIp95 of more than 10 U.
The points in Fig 2 labeled 1 through 4 show data from children who had discordant changes in the BMI metrics: a BMIz decrease of more than 0.33 SDs but increases in %BMIp95 of more than 10 U. These 4 children were boys who were <6 years of age at the initial examination and who had an initial BMIz ≥2.9 SDs. The initial BMIs of these 4 boys were <24.5 and their BMI increases ranged from +5.6 (#3) to +13.5 (#2). The largest increase in %BMIp95 (#2) was from 127 (a BMI of 23 at age 5 years) to 153 (a BMI of 36.7 at age 11 years). Despite this very high BMI at age 11 years, this child’s BMIz decreased by 0.34 SDs because of the upper bound of this metric. There was no change in this child’s BMIaz (4.1 SDs) between examinations.
Discussion
Approximately 7% of 6- to 19-year-olds have a BMI ≥120% of the CDC 95th percentile and are considered to have severe obesity.27 Although the report accompanying the CDC growth charts1 noted that extrapolation at values greater than the 97th percentiles (z score of 1.88) should be interpreted cautiously, BMIz values remain widely used in analyses of children with extremely high BMI levels.14–16,28–30 Analyses of children with severe obesity have shown17 that very high BMIz levels are only weakly (r ≤ 0.20) associated with levels of circumferences and skinfolds. The current analyses reveal that, among children with obesity or severe obesity, BMIz levels at one examination are less strongly associated with values measured 2.8 (mean) years later than are levels of BMIaz and %BMIp95. Among younger boys with severe obesity, we found that there could be decreases of more than 0.33 SDs, even if theirs BMIs increased by more than 5 and their %BMIp95s increased by more than 10 U.
The differences among the BMI metrics in the current study largely result from the constraints of the LMS method. Although the growth charts for BMI originally consisted of 10 percentiles (3rd to 97th), a modification of the LMS procedure was applied to these smoothed percentiles so that the z score and percentile of any child could be calculated.1,3 On the basis of the LMS formula, the maximum attainable BMIz at a given sex and age is (−1) ÷ (L × S). Because the estimated values of L and S varied substantially by sex and age, there were corresponding differences in the maximum attainable BMIz. This resulted in very high BMIs being compressed into a narrow range of z scores that varied by sex and age.8,17
This z score attenuation was recognized by CDC, and a set of modified z scores was developed to aid in the identification of outliers.21 Because these modified z scores are based on a fixed SD (one-half of the distance between 0 and 2 z scores), they do not have an upper limit.21 The BMIaz values in the current analyses were constructed by substituting these modified z scores for LMS-estimated z scores that were <−1.88 (third percentile) or >1.88 (97th percentile). Our results revealed that, among children with severe obesity, the correlations between the BMI metrics over time were stronger for BMIaz (r = 0.65) and %BMIp95 (r = 0.61) than for BMIz (r = 0.47). A somewhat similar approach was used in the construction of z scores in the World Health Organization growth standards31 with the distance between 2 and 3 SDs extrapolated outwards for the calculation of z scores more extreme than ±3 SDs.
Several of the limitations of BMIz are highlighted in Fig 2. The BMI of 1 boy, for example, increased by more than 13 (to 37) between the ages of 5 and 11 years, resulting in a large increase in %BMIp95 but a 0.34 SD decrease in BMIz. Between ages 5 and 11 years, the maximum attainable BMIz value for boys in the CDC growth charts decreases from 4.1 to 3.1 SDs, compressing very high BMIs into a lower range of z scores. We have previously shown17 that the same BMIz value among children with severe obesity maps to substantially different levels of %BMIp95, depending on the sex and age of the child. These differences can greatly complicate comparisons of high BMIz values between boys and girls and across ages.
Many of the limitations of expressing BMI values as z scores have been emphasized by the authors of previous studies,8,10–12 and it has been concluded that LMS-based z scores should not be used to assess BMI changes among children with very high BMIs. Although it is difficult to make a recommendation concerning the use of BMIaz versus %BMIp95, the former may be useful in studies that include children who have a wide range of BMI values. Values of BMIz and BMIaz differ only at the tails of the distributions, with BMIaz values not being compressed into a bounded range. In contrast, when examining changes in body size among children with severe obesity, changes in %BMIp95 might be the better metric.6 Our longitudinal analyses (Table 2) indicated that the longitudinal correlations for BMIaz were somewhat stronger than for %BMIp95, but the differences were small. For some analyses, such as intervention studies, investigators could also consider using multilevel regression,32,33 in which sex and age are included as covariates, and focus on changes in BMI.
There are several limitations that should be considered when interpreting our results. Our longitudinal analyses were based on data collected in various cross-sectional studies, and, therefore, only children who participated in 2 or more studies were included. Furthermore, these data were collected, on average, almost 40 years ago, and the prevalence of severe obesity was much lower (2%) than the current estimate of ∼6%.27 The lower prevalence of severe obesity in the current study may have reduced the magnitudes of the observed differences among the BMI metrics than those we observed. It should also be realized that although the mean interval between examinations in the current study was 2.8 years (SD = 1.4), there was more than a 5-year interval for ∼5% of the consecutive examinations. Furthermore, our results apply to attained levels of BMI, not to the velocity of BMI change. Although difficult to obtain,25,26,34,35 it would be useful if there were more information on longitudinal changes (velocity) in weight, height, and BMI over specified intervals among schoolchildren.
Extrapolated z scores based on the CDC growth charts are often used among children who have very high BMIs.14,28–30,36,37 However, these BMIz values should not be used among children with severe obesity because these values can differ substantially from the empirical estimates,6 have an effective upper limit,8 and are strongly influenced by sex and age. Focusing on BMIz in longitudinal studies may be particularly problematic because changes in this metric could simply reflect age differences in the L and S parameters rather than changes in body size. Rather than being expressed as LMS-based z scores, very high BMIs should be should expressed as z scores on the basis of linear extrapolations of a fixed SD or as a percentage of the CDC 95th percentile. In longitudinal analyses, the use of multilevel models to adjust for sex and age could also be considered. In contrast to BMIz levels based on the CDC growth charts, these other BMI metrics will provide more accurate information on body size over time among children with very high BMIs.
Glossary
- %BMIp95
BMI expressed as a percentage of the 95th percentile
- BMIaz
adjusted z score
- BMIz
BMI-for-sex/age z score
- CDC
Centers for Disease Control and Prevention
- L
power transformation to achieve normality
- M
median
- S
dispersion
Footnotes
Dr Freedman performed most analyses, drafted the initial manuscript, and revised the manuscript; Dr Berenson directed the collection of data and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by National Institute on Aging grant AG-16592 and National Heart, Lung, and Blood Institute grant HL-38844. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2017-2148.
The findings and conclusions in this report do not represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;11(246):1–190 [PubMed] [Google Scholar]
- 2.Ogden CL, Kuczmarski RJ, Flegal KM, et al. . Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60 [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Rep. 2013;9(63):1–3 [PubMed] [Google Scholar]
- 4.Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44(1):45–60 [PubMed] [Google Scholar]
- 5.Cole TJ, Green PJ. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med. 1992;11(10):1305–1319 [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314–1320 [DOI] [PubMed] [Google Scholar]
- 7.Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2- to 4-year-old children [published online ahead of print April 19, 2017]. J Pediatr. 10.1016/j.jpeds.2017.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woo JG. Using body mass index z-score among severely obese adolescents: a cautionary note. Int J Pediatr Obes. 2009;4(4):405–410 [DOI] [PubMed] [Google Scholar]
- 9.Kelly AS, Barlow SE, Rao G, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, and Council on Clinical Cardiology . Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–1712 [DOI] [PubMed] [Google Scholar]
- 10.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59(3):419–425 [DOI] [PubMed] [Google Scholar]
- 11.Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol. 2007;19(4):487–494 [DOI] [PubMed] [Google Scholar]
- 12.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17(1):44–50 [DOI] [PubMed] [Google Scholar]
- 13.Kakinami L, Henderson M, Chiolero A, Cole TJ, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child. 2014;99(11):1020–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Y, Cai L, Wu Y, et al. . What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16(7):547–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siwik V, Kutob R, Ritenbaugh C, et al. . Intervention in overweight children improves body mass index (BMI) and physical activity. J Am Board Fam Med. 2013;26(2):126–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCormick EV, Dickinson LM, Haemer MA, Knierim SD, Hambidge SJ, Davidson AJ. What can providers learn from childhood body mass index trajectories: a study of a large, safety-net clinical population. Acad Pediatr. 2014;14(6):639–645 [DOI] [PubMed] [Google Scholar]
- 17.Freedman DS, Butte NF, Taveras EM, et al. . BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999-2000 to 2013-2014. Obesity (Silver Spring). 2017;25(4):739–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berenson GS, McMahan CA, Voors AW, et al. . Cardiovascular Risk Factors in Children: The Early Natural History of Atherosclerosis and Essential Hypertension. New York, NY: Oxford University Press; 1980 [Google Scholar]
- 19.Frerichs RR, Srinivasan SR, Webber LS, Berenson GRS. Serum cholesterol and triglyceride levels in 3,446 children from a biracial community: the Bogalusa Heart Study. Circulation. 1976;54(2):302–309 [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) A SAS program for the 2000 CDC growth charts. Available at: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed June 26, 2017
- 21.Centers for Disease Control and Prevention (CDC) Modified z-scores in the CDC growth charts. Available at: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/biv-cutoffs.pdf. Accessed April 25, 2017
- 22.Freedman DS, Lawman HG, Skinner AC, McGuire LC, Allison DB, Ogden CL. Validity of the WHO cutoffs for biologically implausible values of weight, height, and BMI in children and adolescents in NHANES from 1999 through 2012. Am J Clin Nutr. 2015;102(5):1000–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Rep. 2010;(25):1–5 [PubMed] [Google Scholar]
- 24.R Core Team R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. Available at: https://www.R-project.org/. Accessed June 26, 2017
- 25.Cole TJ. The development of growth references and growth charts. Ann Hum Biol. 2012;39(5):382–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brannsether B, Eide GE, Roelants M, Bjerknes R, Júlíusson PB. BMI and BMI SDS in childhood: annual increments and conditional change. Ann Hum Biol. 2017;44(1):28–33 [DOI] [PubMed] [Google Scholar]
- 27.Ogden CL, Carroll MD, Lawman HG, et al. . Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kreier F, Genco ŞM, Boreel M, et al. . An individual, community-based treatment for obese children and their families: the solution-focused approach. Obes Facts. 2013;6(5):424–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Savoye M, Nowicka P, Shaw M, et al. . Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics. 2011;127(3):402–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hampl S, Odar Stough C, Poppert Cordts K, Best C, Blackburn K, Dreyer Gillette ML. Effectiveness of a hospital-based multidisciplinary pediatric weight management program: two-year outcomes of PHIT Kids. Child Obes. 2016;12(1):20–25 [DOI] [PubMed] [Google Scholar]
- 31.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003 [Google Scholar]
- 33.UCLA, IDRE: Institute for Digital Research and Education Statistical computing seminars: analyzing longituidinal data using multilevel modeling. Available at: www.ats.ucla.edu/stat/seminars/mlm_longitudinal/. Accessed December 15, 2016
- 34.Zemel BS. A commentary on the construction of weight velocity charts. Nutr Clin Pract. 2009;24(5):651–653 [DOI] [PubMed] [Google Scholar]
- 35.WHO Department of Nutrition for Health and Develpment WHO child growth standards. Growth velocity based on weight, length and head circumference Methods. Methods and development. 2009. Available at www.who.int/childgrowth/standards/velocity/tr3_velocity_report.pdf. Accessed May 17, 2017
- 36.Baughcum AE, Gramling K, Eneli I. Severely obese preschoolers in a tertiary care obesity program: characteristics and management. Clin Pediatr (Phila). 2015;54(4):346–352 [DOI] [PubMed] [Google Scholar]
- 37.The Children’s Hospital of Philadelphia Pediatric z-score calculator. Available at: http://stokes.chop.edu/web/zscore/. Accessed May 13, 2016