In this systematic literature review, we found evidence that parents of hospitalized children who received coping support interventions had better emotional well-being.
Abstract
CONTEXT:
Parents may experience psychological distress when a child is acutely hospitalized, which can negatively affect child outcomes. Interventions designed to support parents’ coping have the potential to mitigate this distress.
OBJECTIVE:
To describe interventions designed to provide coping support to parents of hospitalized children and conduct a meta-analysis of coping support intervention outcomes (parent anxiety, depression, and stress).
DATA SOURCES:
We searched Pubmed, Embase, PsycINFO, Psychiatry Online, and Cumulative Index to Nursing and Allied Health Literature from 1985 to 2016 for English-language articles including the concepts “pediatric,” “hospitalization,” “parents,” and “coping support intervention.”
STUDY SELECTION:
Two authors reviewed titles and abstracts to identify studies meeting inclusion criteria and reviewed full text if a determination was not possible using the title and abstract. References of studies meeting inclusion criteria were reviewed to identify additional articles for inclusion.
DATA EXTRACTION:
Two authors abstracted data and assessed risk of bias by using a structured instrument.
RESULTS:
Initial searches yielded 3450 abstracts for possible inclusion. Thirty-two studies met criteria for inclusion in the systematic review and 12 studies met criteria for inclusion in the meta-analysis. The most commonly measured outcomes were parent depression, anxiety, and stress symptoms. In meta-analysis, combined intervention effects significantly reduced parent anxiety and stress but not depression. Heterogeneity among included studies was high.
LIMITATIONS:
Most included studies were conducted at single centers with small sample sizes.
CONCLUSIONS:
Coping support interventions can alleviate parents’ psychological distress during children’s hospitalization. More evidence is needed to determine if such interventions benefit children.
A child’s hospitalization is a source of anxiety, depression, and stress for parents.1–6 Better parent emotional and mental health is associated with better mental and physical health in children.7–9 If parents’ abilities to participate in a hospitalized child’s care are compromised by emotional distress, the child’s processes of care are likely to suffer. Interventions designed to provide support to parents of sick children can help parents experience lower stress and participate in a child’s medical care.10–14 In previous studies, family members of hospitalized patients report that they value education, efficient communication from hospital clinical teams, opportunities to experience empathy from clinicians or peers, and offers of assistance to help mitigate the disruption to family life caused by a hospitalization.14–18 Interventions designed to support parents in coping with the hospitalization via communication, empathy, education, concrete resources, or other means are well positioned to improve parents’ well-being during and after the child’s hospitalization.
Interventions to support parents’ emotional health have the potential to benefit children with physical illness requiring hospitalization. The authors of recent meta-analyses have examined coping support interventions for parents of children with chronic illness13 and NICU-based interventions to reduce maternal depression and anxiety.19 However, the literature describing interventions to support parents in coping with pediatric hospitalization and evidence of the effects of parent coping support interventions on outcomes have not been synthesized. Therefore, we conducted a systematic review to describe coping support interventions for parents of acutely hospitalized children and infants and a meta-analysis of the effects of such interventions on the 3 most commonly measured outcomes in the included studies: parent anxiety, depression, and stress.
Methods
Search Strategy
We used the approach recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines20 to identify studies of interventions to provide coping support to parents of hospitalized children. We searched PubMed/Medline, Embase, PsycINFO, Psychiatry Online, and Cumulative Index to Nursing and Allied Health Literature from January 1, 1985, to October 27, 2016, using search terms organized around the following key concepts: “hospitalization,” “child,” “parent,” and “coping support intervention.” Each concept was mapped to its controlled vocabularies and keywords in databases, and search terms were combined to generate refined results. Reference lists of included studies were reviewed to identify additional studies for possible inclusion. Search terms for PubMed are outlined in the Supplemental Information. The systematic review protocol was registered with the PROSPERO International Prospective Register of Systematic Reviews (available at: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015027326), registration number CRD42015027326. The Children’s Hospital of Philadelphia Institutional Review Board considered this study exempt from human subjects research review.
Study Selection
Two study authors independently reviewed titles and abstracts of studies identified in the initial search to identify studies eligible for inclusion in the full text review. Eligibility criteria for inclusion in the systematic review included: (1) study of an intervention, (2) the intervention target population included parents of acutely hospitalized children (ages 0–21 years), (3) the intervention included elements designed to provide coping support, and (4) the study was written or available in English. Studies involving parents of children in ambulatory settings, psychiatric hospital settings, or long-term residential treatment centers were excluded. If not enough information was provided in the title and abstract to make a determination, 2 authors reviewed the full text of the study. References of included studies were reviewed for possible inclusion in the review.
Inclusion in the meta-analysis was restricted to randomized controlled trials (RCTs) of interventions to improve depression, anxiety, or stress. Analyses of preintervention and postintervention data on a single group of participants, nonrandomized studies, and studies that did not evaluate parent depression, anxiety, or stress were not eligible for inclusion in the meta-analysis.
Data Abstraction, Evaluation, and Synthesis
Two authors independently extracted the following relevant information from each study: design, geographic location, characteristics of hospitalized children, characteristics of parents, elements of study intervention, intervention delivery modality (eg, in person, video, or Web site), intervention duration, and outcomes. Study design was evaluated by using methodological criteria developed by Downs and Black,21 including measures of study reporting, external validity, internal validity, and risk of bias (but not including measures regarding study power because many studies had multiple outcomes). The highest possible Downs and Black point assignment was 26 points.
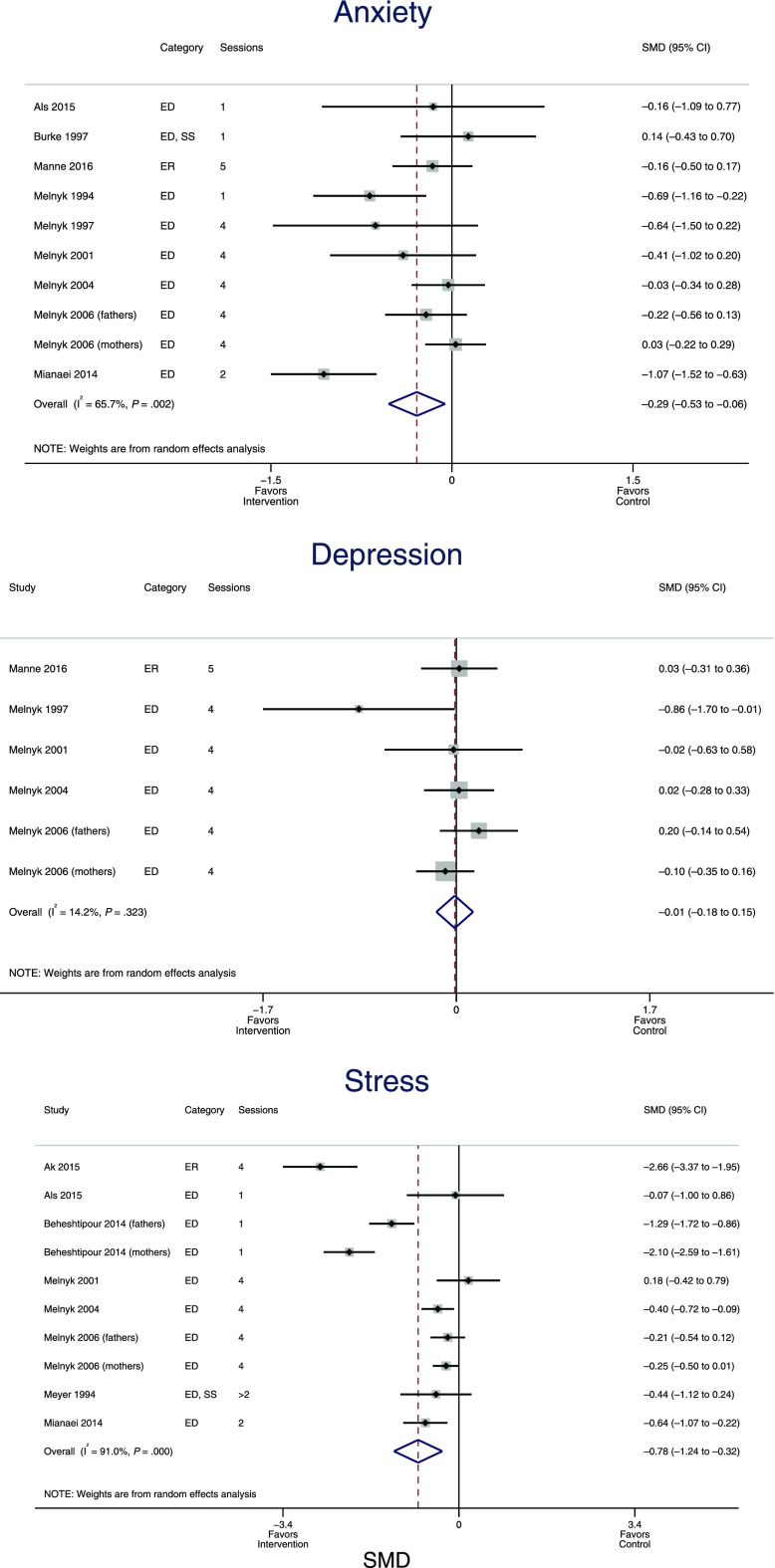
Meta-Analysis
RCTs in which validated measures were used to assess parent anxiety, depression, or stress symptom burden were eligible for inclusion in the meta-analysis. We measured effect sizes of interventions by using standardized mean differences (SMDs) between the intervention and comparison group for each outcome. For studies measuring outcomes at multiple time points, we selected the time closest to hospital discharge. Two studies examined intervention effects in mothers and fathers separately, and for those we included maternal and paternal data separately in the models and figures. For each of the 3 outcomes, we developed random effects models to calculate pooled effect estimates weighted for the inverse of the variance of the individual effects. Random effects models assume that effect sizes are representative of a distribution of effect sizes, and the pooled effect estimate from a random effects model represents the average of a distribution of effect sizes. We used I2 statistics to assess the degree to which heterogeneity in estimated effect sizes is due to differences in intervention characteristics. A high I2 statistic suggests that interventions have different effect sizes, whereas a lower I2 statistic suggests that a larger proportion of the variation in effect sizes is attributable to random variation in observed effect sizes between interventions with similar effects. We used results of random effects models to create forest plots displaying pooled effect estimates weighted for each study’s sample size.
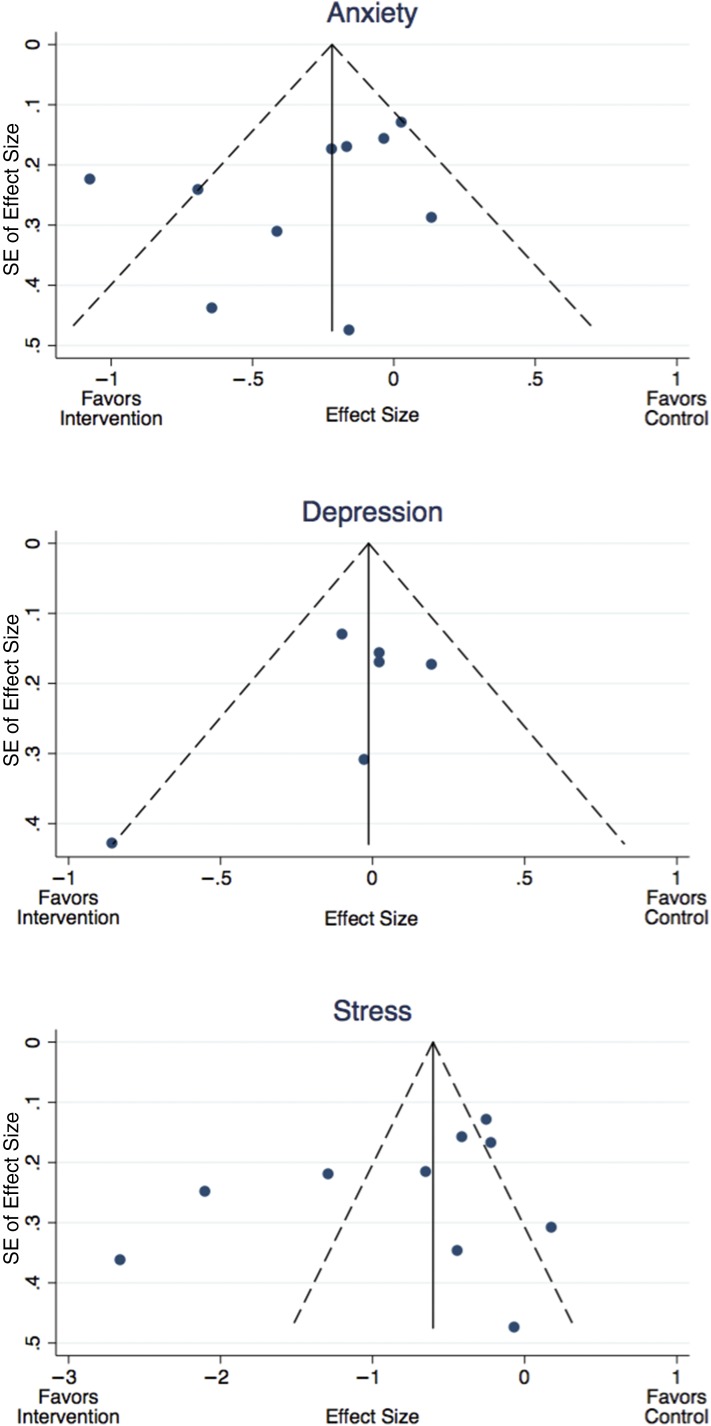
For all studies included in the random effects models and forest plots, we created funnel plots of the estimate of the intervention effect size generated in the random effects model against the SE of the effect size. Funnel plots provide a visual tool for investigating the tendency for smaller studies to show larger effect sizes. Asymmetry in a funnel plot can be seen in cases of publication bias, in which smaller studies without statistically significant effects remain unpublished, or in which true effect sizes are different between smaller and larger studies.
All analyses were completed by using Stata 13.0 (StataCorp, College Station, TX).
Results
Characteristics of Included Studies
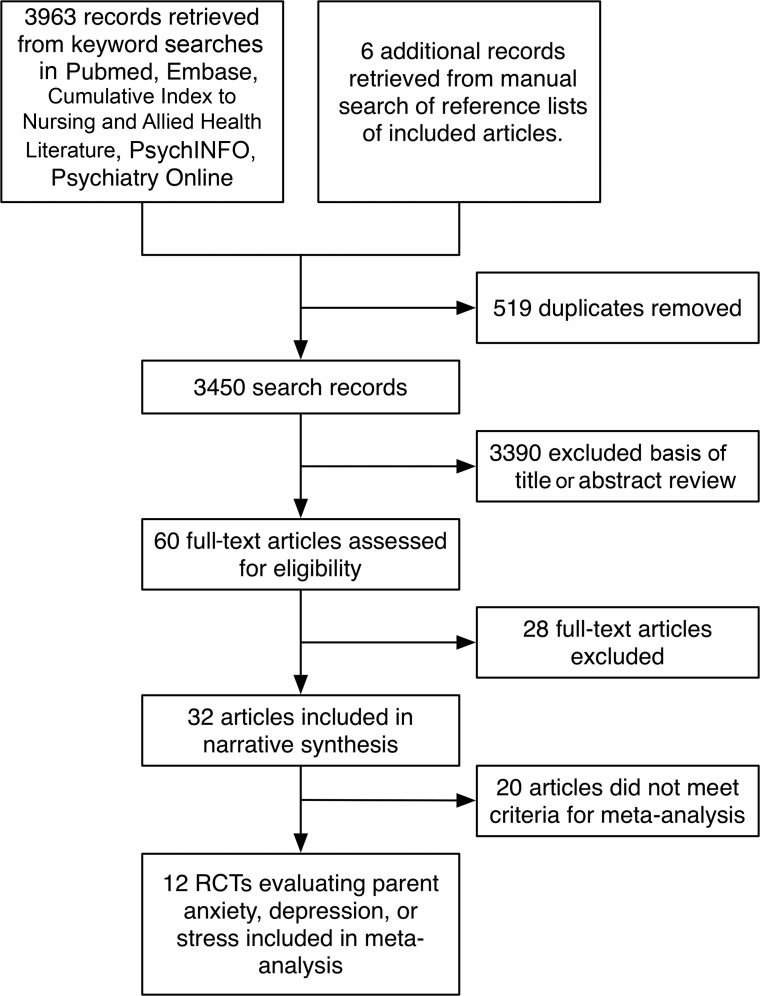
Initial searches yielded 3963 unique citations for potential inclusion in the full review. Review of references cited by the included studies identified 6 additional studies for possible inclusion. After removal of duplicates, 2 study authors reviewed titles and abstracts for 3450 unique studies. The authors who reviewed titles and abstracts identified 60 articles for full text review. On full text review, 28 studies did not meet inclusion criteria. Thirty-two articles met all inclusion criteria for the systematic review, and, of these, 12 met criteria for inclusion in meta-analysis (Fig 1). Of the 32 included studies, 17 were RCTs,22–36 6 were nonrandomized quasi-experimental studies of nonequivalent groups,37–42 and 9 included a preintervention and postintervention assessment of a single group.43–51 In Table 1, we display study characteristics and findings.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for studies of coping support interventions for parents of hospitalized children, 1985 to 2016.
TABLE 1.
Characteristics of 32 Studies of Coping Support Interventions for Parents of Hospitalized Infants and Children
| Study | Design | Participants | Country | Intervention Characteristics | Outcomes | Main Findings in Group Receiving Intervention | Downs and Black Score | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Setting | Description | Duration | ||||||||
| Education-focused interventions | ||||||||||
| Als et al (2015)23 | RCT | 31 parents of children with critical illness | United Kingdom | PICU | Handbook describing child reactions to PICU hospitalization and advice about managing postdischarge problems, telephone call after hospital discharge | 1 telephone call | 1. Feasibility | 3 of 6 feasibility criteria met, lower parent depression and PTSSs, no difference in parent anxiety, and fewer child negative emotions or behavior problems at 3–6 mo. | 20 | |
| 2. Parent PTSSs | ||||||||||
| 3. Parent anxiety | ||||||||||
| 4. Parent depression | ||||||||||
| 5. Child emotions | ||||||||||
| 6. Child behaviors | ||||||||||
| Beheshtipour et al (2014)24 | RCT | 51 parents of infants in a NICU born at 28–37 wk GA | Iran | NICU | In-person education session about child’s condition for mother and father or coparent | 1 × 1-h session | 1. Maternal stress | Lower stress for both mothers (P < .001) and fathers (P < .001) on day 7 of the infant’s hospitalization. | 23 | |
| 2. Paternal stress | ||||||||||
| Carvalho et al (2009)43 | Pre/post | 59 mothers of infants born at <37 wk GA or ≤1500 g | Brazil | NICU | Educational video and manual about prematurity. Intervention and control participate in psychological support groups. | At least 2 sessions | 1. Maternal anxiety | Lower depression (P = .04) and anxiety (P < .001) symptoms after intervention. | 21 | |
| 2. Maternal depression | ||||||||||
| Macner-Licht et al (1998)51 | NRS | 17 parents of children hospitalized for leukemia | Singapore | Oncology | Weekly structured psychoeducational group meetings for parents. Children participated in structured play sessions. | 2-h parent groups, weekly × 12 wk | 1. Parent hopelessness | Parents reported more hopefulness and better coping after participation in groups. | 12 | |
| 2. Parent coping | ||||||||||
| Marsac et al (2013)36 | RCT | 100 parents of children hospitalized for accidental injury | United States | Trauma | A Web-based interactive platform including information about recovery from traumatic injury and opportunity to build an individualized care plan. | 20-min session + ongoing Web site access | 1. Parent knowledge of child injury reactions | Greater parent knowledge of child injury reactions and lower child PTSSs immediately after the intervention (P < .05). | 23 | |
| 2. Child PTSSs | No differences in parent knowledge, child PTSSs, or parent PTSSs at 6 wk (P > .05). | |||||||||
| 3. Parent PTSSs at 6 wk | ||||||||||
| Melnyk et al (1994)29 | RCT | 108 mothers of children hospitalized for non-critical illness | United States | General | Video about child behavior, parent role, or both. | 1 × <15 min session | 1. Maternal anxiety | Lower maternal anxiety and greater participation in child’s care during hospitalization (P < .05). | 22 | |
| 2. Maternal participation in child’s hospital care | Lower maternal anxiety and less child negative behavior change 1 wk after discharge (P < .05). | |||||||||
| 3. Child behavior change | ||||||||||
| Melnyk et al (1997)52 | RCT | 30 mothers of children with critical illness | United States | PICU | Audiotapes with accompanying workbook exercises. | 4 sessions | 1. Maternal participation in child’s hospital care | More maternal participation in child’s care, less maternal stress (P < .05), less anxiety and depression (P < .1). | 23 | |
| 2. Maternal anxiety | No difference in child behavior or maternal PTSSs. | |||||||||
| 3. Maternal depression | ||||||||||
| 4. Maternal stress | ||||||||||
| 5. Maternal PTSSs | ||||||||||
| 6. Child behavior change | ||||||||||
| Melnyk and Feinstein (2001)27 | RCT | 42 mothers of infants born at 28–36 wk GA and <2500 g | United States | NICU | Audiotapes with workbook exercises on how to care for and interact with child. | 4 sessions | 1. Infant cognitive development | Better infant cognitive development at 3 and 6 mo corrected GA (P < .05). | 24 | |
| 2. Maternal stress | No difference in maternal stress, anxiety, or mother-child interactions. | |||||||||
| 3. Maternal anxiety | ||||||||||
| 4. Mother-child interactions | ||||||||||
| Melnyk et al (2004)30 | RCT | 174 mothers of children with critical illness | United States | PICU | Audiotapes with accompanying workbook exercises. | 4 sessions | 1. Maternal participation in child’s hospital care | More maternal participation in child’s care (P < .05), no difference in maternal anxiety, lower maternal PTSSs, (P < .05), and no difference in child behavior change or child PTSSs. | 23 | |
| 2. Maternal anxiety | ||||||||||
| 3. Maternal PTSSs | ||||||||||
| 4. Child behavior | ||||||||||
| 5. Child PTSSs | ||||||||||
| Melnyk et al (2006)28 | RCT | Parents of 260 infants born at 26–34 wk GA and <2500 g | United States | NICU | Audiotapes with workbook exercises on how to care for and interact with child. | 4 sessions | 1. Parent depression | Lower depression and anxiety at 2 mo for mothers (P < .05) and no difference for fathers. No difference in parent stress or parent-child interactions. Shorter infant length of stay (P = .02). | 26 | |
| 2. Parent anxiety | ||||||||||
| 3. Parent stress | ||||||||||
| 4. Parent-child interactions | ||||||||||
| 5. Infant length of stay | ||||||||||
| Mianaei et al (2014)32 | RCT | 90 mothers of infants born at 26–34 wk GA and <2500 g | Iran | NICU | Audiotapes with workbook exercises on how to care for and interact with child (derived from work by Melnyk). | 2 sessions | 1. Maternal anxiety | Lower anxiety (P < .001), less stress (P < .001), and more maternal participation in the infant’s care during the NICU stay (P < .001). | 24 | |
| 2. Maternal stress | ||||||||||
| 3. Mother-child interactions | ||||||||||
| Won (2006)53 | NRS | 56 mothers of hospitalized children requiring an intravenous procedure | South Korea | General | Video modeling supportive and unsupportive behaviors. | 1 × 7-min session | 1. Parent support of child | More supportive behavior (P = .005), and better understanding of child behaviors immediately after procedure (P = .005). No difference in mood (P = .83). | 22 | |
| 2. Parent understanding of child behaviors | ||||||||||
| 3. Parent mood | ||||||||||
| ER-focused interventions | ||||||||||
| Ak et al (2015)22 | RCT | 29 Breast-feeding mothers | India | NICU | Music therapy audio recording via headphones while pumping breast milk. | 4 × 15-min sessions | 1. Volume of expressed breast milk | Greater volume of breast milk produced (P = .03), lower salivary cortisol (P = .001), and lower stress (P < .001) immediately after intervention. | 19 | |
| 2. Maternal salivary cortisol | ||||||||||
| 3. Maternal stress | ||||||||||
| DeMaso et al (2000)50 | Pre/post | 49 parents of hospitalized children with congenital heart disease | United States | Cardiac | Parents used an “experience journal” computer application to describe experiences of living with illness by using written explanation, pictures, poems, or video. | 2–4 wk | Parent satisfaction and safety | Parents reported high satisfaction and minimal harm associated with use of the experience journal. | 15 | |
| Kadivar et al (2015)38 | NRS | 70 mothers of infants born at <37 wk GA | Iran | NICU | Unguided narrative writing at least 3 times a week between days 3 and 10 of hospitalization. | 7 d | Parent stress | Lower stress on day 10 of NICU stay (P < .001). | 21 | |
| Lai et al (2006)26 | RCT | 30 mothers of infants born at <37 wk GA, >1500 g, not critically ill | Taiwan | NICU | Daily lullaby music recording played via speakers during a kangaroo-care session. | 1h | 1. Maternal anxiety | Lower maternal anxiety (P < .01), more infant sleep (P < .01), less infant crying (P < .05), and no difference in infant physiology after intervention session. | 22 | |
| 2. Infant behaviors | ||||||||||
| 3. Infant physiologic status | ||||||||||
| Macnab et al (1998)49 | Pre/post | 73 parents with high school education | Canada | NICU | Pamphlet to guide parents through process of writing a journal. | 6 wk | 1. Feasibility | 32% of parents completed journal; of these, 50% made daily entries. 73% of parents perceived journaling was helpful. | 11 | |
| 2. Parent experiences | ||||||||||
| Manne et al (2016)35 | RCT | 218 parents of children hospitalized for stem cell transplant | United States | Oncology | Parents learned relaxation techniques, coping techniques, and cognitive and social processing strategies for managing stress. | 5 × 60-min sessions and a CD-ROM | 1. Parent depression | Significantly lower anxiety and distress at 1 mo (P < .05). | 22 | |
| 2. Parent anxiety | ||||||||||
| 3. Parent PTSSs | ||||||||||
| 4. Parent well-being | ||||||||||
| Mouradian et al (2013)48 | Pre/post | 40 parents of infants in a NICU | United States | NICU | Facilitated group scrapbooking activity. | 1 session | Parent anxiety | Lower state anxiety (P < .001) immediately after activity. | 21 | |
| Thygeson et al (2010)47 | Pre/post | 33 parents of children hospitalized for any cancer | United States | Oncology | Yoga class including active and restful yoga poses. | 1 × 45-min session | Parent anxiety | Lower parent anxiety immediately after intervention (P < .001). Qualitative analyses identified themes of relaxation and stress-relief. | 19 | |
| Mixed interventions: education and SS | ||||||||||
| Burke et al (1997)33 | RCT | 25 parents of 1–17 y children with a scheduled hospitalization | Canada | General | Home visit 2 wk before the hospitalization to develop coping strategies and identify resources. Access to a nurse by telephone during the study period. | 1 home visit + periodic telephone calls | 1. Parent anxiety | Lower anxiety (P < .05), higher coping (P < .001), and higher satisfaction with family functioning (P < .001) at 3 mo. | 22 | |
| 2. Parent coping | No child behavior differences and better developmental gains (P < .001) at 3 mo. | |||||||||
| 3. Family functioning | ||||||||||
| 4. Child behavior problems | ||||||||||
| 5. Child developmental progress | ||||||||||
| Meyer et al (1994)31 | RCT | 34 parents of infants born at <1500 g | United States | NICU | Structured family psychosocial assessment and individualized interventions to address identified needs. | 3–17 sessions | 1. Parent stress | Lower stress (P < .05), lower depression (P < .05), and better mother-infant feeding interactions (0.001) at hospital discharge. | 24 | |
| 2. Parent depression | ||||||||||
| 3. Mother-child interactions | ||||||||||
| Preyde and Ardal (2003)39 | NRS | 60 mothers of infants born at <30 wk GA or <1500 g | United States, Canada | NICU | Mothers received telephone support from a trained peer mentor who was a parent of a preterm infant. | Average of 9 1-h phone calls | 1. Maternal stress | Lower stress at 4 wk (P < .001). | 17 | |
| 2. Maternal anxiety | Lower state anxiety (P < .05), lower depression (P < .01), and better social support (P < .01) at 16 wk. | |||||||||
| 3. Maternal depression | ||||||||||
| 4. Social support | ||||||||||
| Segre et al (2013)45 | Pre/post | 23 mothers of infants born at <32 wk GA | United States | NICU | Visits from a neonatal nurse practitioner trained in empathic listening. | 6 × 1-h sessions | 1. Maternal depression | Lower maternal depression, anxiety, and better quality of life at 1 mo (P < .001). | 20 | |
| 2. Maternal anxiety | ||||||||||
| 3. Maternal quality of life | ||||||||||
| Svavars-dottir and Sigurdardottir (2013)46 | Pre/post | 19 caregivers of children with cancer and their partners | Iceland | Oncology | Therapeutic conversations with a study nurse and an oncology nurse. | 2–3 × 1-h sessions | 1. Family functioning | Better rating of family functioning and family support in primary caregivers (P < .05). | 20 | |
| 2. Social support | ||||||||||
| Mixed interventions: education and ER | ||||||||||
| Burke et al (2001) 34 | RCT | 44 parents of 1–15 yo children with a chronic medical condition | Canada | General | Prehospital in-person assessment, written plan for dealing with needs during the hospitalization, and a nurse visit during hospitalization. | 2 nurse visits | 1. Family functioning | Better family functioning (P = .005), social support (P = .06), and coping (P = .016) at 3 mo after hospitalization. | 24 | |
| 2. Parent coping | ||||||||||
| Cobiella et al (1990)25 | RCT | 30 mothers of infants born at <37 wk GA and <2500 g | United States | NICU | Video modeling either problem-focused or emotion-focused coping. | 1 × 15-min session | 1. Mother-child interaction | Lower depression and anxiety at 2 wk for problem-focused and for emotion-focused coping groups. No effect on mother-child interaction or mother’s stress. | 24 | |
| 2. Maternal depression | ||||||||||
| 3. Maternal anxiety | ||||||||||
| 4. Maternal stress | ||||||||||
| Feeley et al (2008)44 | Pre/post | 24 mothers of infants born at <1500 g | Canada | NICU | Educational sessions to teach mothers to recognize and reduce anxiety and interact with infants. | 6 × 1-h sessions | 1. Adherence to intervention delivery | 20 of 24 participants (83%) attended all intervention sessions, and 14 of 20 (70%) were “very satisfied.” | 15 | |
| 2. Acceptability | ||||||||||
| Mixed interventions: education, ER, and SS | ||||||||||
| Curley (1988)40 | NRS | 33 parents of children with critical illness | United States | PICU | Bedside nurses trained to include parents in patient care, reinforce parent nurturing role, and teach them about PICU. | Daily during hospitalization | Parent stress | Lower parent stress on hospital day 2 (P < .001). | 19 | |
| Curley and Wallace (1992)41 | NRS | 56 parents of children with critical illness | United States | PICU | All PICU nurses were trained to include parents in patient care, reinforce parent caretaker role, and teach them about PICU. | 1 × 1-h staff education | Parent stress | Lower parent stress throughout PICU stay (P < .001). | 16 | |
| Jotzo and Poets (2005)37 | NRS | 50 mothers of infants born at <37 wk GA | Germany | NICU | Individual supportive counseling within 5 d of hospitalization. | 1 initial session, 2 × weekly 15-min follow-up visits | Maternal PTSSs | Lower PTSSs at NICU discharge (P = .013). | 21 | |
| Starks et al (2016)54 | RCT | 220 family members of children hospitalized with critical illness | United States | NICU or PICU | Palliative care team consult including initial assessment, at least twice weekly check-ins, goals of care, and care coordination discussions. | Duration of hospitalization (mean 40 d) | 1. Enrollment and retention | 50% of all eligible children enrolled. Retention rate was 92%. Burdens of participation were low. | 20 | |
| 2. Burdens and benefits of participation | ||||||||||
GA, gestational age; LOS, length of stay; NRS, nonrandomized controlled study; yo, years old.
Of the 32 included studies, 21 took place in the United States or Canada, 7 in Asia, 3 in Europe, and 1 in South America. Researchers for 16 studies investigated coping support interventions for parents of children hospitalized in an NICU. In the 16 studies of interventions for parents of children hospitalized for other indications, children were hospitalized for critical illness in 6 studies, cancer in 4 studies, cardiac conditions in 1 study, physical injury in 1 study, and other general, noncritical conditions in 4 studies. Sample sizes for studies included in the review ranged from a study of 17 parents51 to a study of parents of 260 children.28 Most were single-center studies, with the exception of 3 studies that included parents from 2 NICUs28,32,39 and 1 study that included parents of children receiving stem cell transplants at 4 centers.35
Intervention Subjects
All interventions included at least 1 parent or guardian of a hospitalized child. Of the 16 NICU studies, 11 were focused on interventions for mothers only,25–27,32,37–39,43–45 and 5 were focused on interventions involving mothers, fathers, and/or other caregivers.24,28,31,48 Of the 16 studies involving older children outside the neonatal period, 4 were focused on interventions for mothers only29,30,42,52 and 12 were focused on interventions for mothers, fathers, and/or other caregivers.23,33–36,40,41,46,47,51 With the exception of 2 studies involving educational interventions delivered to PICU nursing staff,40,41 all other studies directly involved parents and guardians in receipt of the intervention. Certain interventions for parents of older hospitalized children also included the child in the intervention; for example, yoga sessions were offered to the child hospitalized for cancer and his or her family members47 (Supplemental Table 2).
Theoretical Framework of Interventions
Coping support interventions varied in the theoretical framework used to inform the intervention and in the focus of intervention content. Theoretical frameworks referenced in the design of the interventions included: theories of problem-focused and emotion-focused coping,55 a transactional model of early intervention,56 a model of the role of trauma in the development of a parent-child relationship,57 self-regulation theory,58 control theory,59 the Nursing Mutual Participation Model of Care,40 and the Calgary Family Intervention Model theory of family nursing.60 After review of the included articles, we categorized study intervention elements in 3 broad categories: education, emotion regulation (ER), and social or structural support (SS). Some interventions involved elements in >1 of these 3 domains.
Education interventions focused on providing education in skills and knowledge about caring for a child with a serious illness. For example, in 1 study, videos were used to educate parents about child behavior and the parents’ role in caring for the child.29 ER interventions were designed to provide opportunities for emotional self-care. For example, in 3 studies, parents were invited to participate in narrative writing to process emotions and experiences.38,49,50 SS interventions were based on the principle that providing concrete resources and opportunities for social relationships for parents of sick children may help mitigate the time and resource demands of a hospitalization. For example, 2 studies involved nurse visits to help families develop a plan for managing demands of family life during a child’s planned hospitalization.39,45
Intervention Content
Education
Educational interventions taught parents skills and knowledge potentially beneficial in caring for a hospitalized child in 3 ways: (1) structured didactics in the form of workbooks, videos, audio recordings, or other educational materials; (2) focused training for clinical staff who could model skills and support parents in practicing them; and (3) opportunities for parents to meet with clinical staff to address gaps in skills or knowledge. Structured didactics were offered in a 2013 study by Marsac et al,36 in which a trained staff person guided parents of children hospitalized for physical traumatic injuries through a 20-minute Web-based activity providing information about physical traumatic injury, traumatic stress reactions, and coping strategies, and then parents continued to use the Web site after hospital discharge.36 Focused training for clinical staff was a key component of 2 studies by Curley et al40,41 published in 1988 and 1992, in which PICU staff were trained in how to coach parents in caregiving for a critically ill child. Parents received structured in-person education from clinicians to address knowledge gaps about their child’s condition in studies by Beheshtipour et al24 and Carvalho et al.43 One intervention bundle that was focused primarily on parent education was studied in 5 articles included in this review: the Creating Opportunities for Parent Empowerment program.28–30,32,52 The Creating Opportunities for Parent Empowerment program evolved over >10 years across several of the included studies, and the program includes audio recordings and workbook exercises to teach parents about behaviors and emotions that children experience during hospitalization and to provide parents with strategies for engaging in the child’s care and recovery.
ER
ER interventions were focused on emotional self-care. Intervention content included: (1) activities to promote relaxation or distraction; (2) teaching parents skills for managing depression, anxiety, and stress; and (3) encouraging adaptive emotional expression. Studies in which the effects of activities to promote relaxation or distraction were investigated included studies of yoga groups,47 music therapy sessions,22,26 and a scrapbooking session.48 Researchers for studies in which parents were taught emotion and stress management skills used diverse methods including individual counseling,37,46 videos modeling different coping strategies,25,42 and training for nurses in empathic communication to promote parents’ adaptive emotional expression.40,41 Studies in which opportunities for emotion expression were offered included 2 studies of empathic listening as a technique for encouraging parents to express emotions45,46 and 3 studies of journaling or other narrative writing.38,49,50
SS
SS interventions that were focused on helping parents identify resources for social support and addressing practical considerations related to a child’s hospitalization (eg, child care for other children, transportation, or missed days at work). All SS interventions were part of multifaceted interventions that also included education or ER elements. For example, in 1997 and 2001 studies by Burke et al,33,34 the authors evaluated the effect of prehospitalization nurse visits to help families identify concrete resources to manage logistical challenges related to meeting home responsibilities while a child is hospitalized. Nurses also helped families develop coping plans and provided psychoeducation by exploring the stressors surrounding hospitalization.33,34 The only study in which a social support intervention was primarily offered was a 2003 study by Preyde and Ardal.39 In the study, parents of preterm infants participated in a “buddy” program, in which they were partnered with another parent who had a previous experience of having an infant hospitalized in the NICU.34
Intervention Delivery Methods, Timing, and Duration
The modes of intervention delivery included audio recordings, videos, written exercises, workbooks, one-on-one interviews, phone calls, and Web sites for parents. The least intensive interventions consisted of a single brief video or audio recording, such as a 7-minute video in which helpful and unhelpful behaviors at the time of IV placement were modeled42 or listening to 15-minute music therapy audio recordings during breast milk pumping sessions.22 Slightly more intensive were single in-person participatory interventions led by staff, such as a 1-hour yoga session,47 a 1-hour facilitated group scrapbooking session,48 and a 20-minute Web-based educational activity with in-person guidance.61 Others asked parents to spend considerable time completing activities independently.28,30,32,35 The most intensive interventions required multiple sessions in which parents participated in individualized, in-person counseling sessions or other activities with a clinical staff member.31,33,34,45 Most interventions took place while the child was in the hospital, but some began before a planned hospitalization33,34 or followed the family after discharge.23,36,46
Description of Outcomes
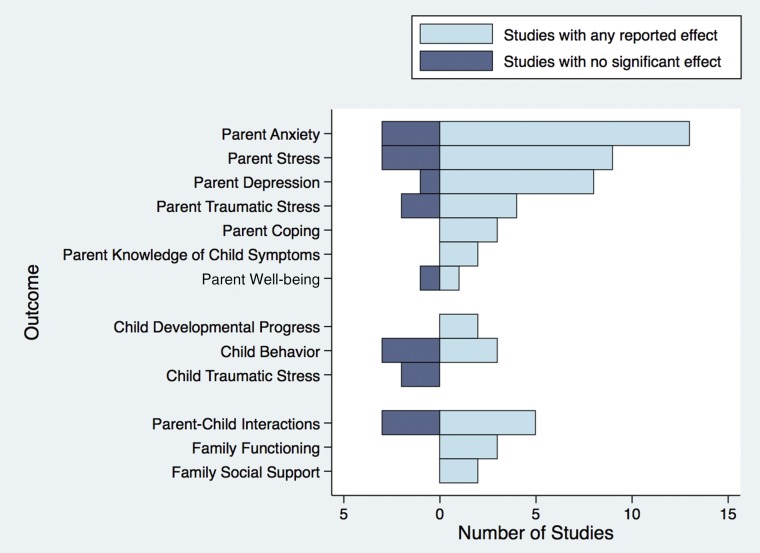
In Fig 2, we summarize measured outcomes and the proportion of interventions showing a statistically significant effect on each outcome. Parent outcomes included measures of stress, anxiety, posttraumatic stress, depression, and coping skills. Child outcomes included measures of posttraumatic stress, child behavior, and child development. Family outcomes included measures of family functioning, parent-child interactions, and family communication. The authors of 5 studies reported outcomes related to the feasibility of the intervention, including acceptability to parents and adherence to intervention components.23,44,49,50,54
FIGURE 2.
Outcomes of coping support interventions for parents of hospitalized children. Includes outcomes reported in ≥2 studies of coping support interventions (published between 1985 and 2016) for parents of hospitalized children.
Parent Outcomes
The most commonly measured parent outcomes were anxiety, stress, depression, and posttraumatic stress symptoms (PTSSs). Researchers for all studies in which parent emotional outcomes were measured relied on parent self-report to measure outcomes, and many measured outcomes at multiple points in time. Of the 16 studies whose authors reported parent anxiety as an outcome, 13 revealed a statistically significantly lower burden of anxiety symptoms in intervention participants.* Similarly, for studies whose authors reported parent stress as an outcome, 9 of 12 revealed evidence that stress was statistically significantly lower among intervention participants.† For depression, 7 of 8 studies revealed that parent depression was statistically significantly lower in parents who received the intervention.23,25,28,31,39,43,45,52 PTSSs were statistically significantly lower after intervention participation in 3 of the 5 studies in which parent posttraumatic stress was measured.30,35,37
Child Outcomes
Researchers measured child outcomes less frequently than parent outcomes. Of the 32 studies included in this review, the authors of 9 measured child outcomes. Child outcomes included child behavior, developmental progress, PTSSs, and hospital length of stay. Neither of the studies in which child PTSSs was measured revealed lower posttraumatic stress in children whose parents received the intervention.30,36 The authors of 3 of 6 studies in which child behavior was measured found a statistically significant difference with fewer undesirable behaviors observed in children of parents receiving the intervention.23,29,51 The authors of both studies in which child progress toward achieving developmental milestones was measured found that children of parents receiving the intervention had more developmental progress.
Family Outcomes
In addition to parent-specific and child-specific outcomes, the authors of 13 of 32 studies measured family outcomes. Of the 8 studies whose authors measured parent-child interactions as an outcome, 5 revealed better parent-child interactions in the intervention group.29–32,52 In all 3 of the studies whose authors measured family functioning, the intervention resulted in improved family functioning.33,34,46 The authors of both studies in which family social support was measured found that the intervention resulted in improved family social support.34,46
Feasibility
The authors of 5 studies evaluated feasibility. The authors of 1 study found that a palliative care consultation program was feasible to implement in the PICU.54 In another study, authors found that enrolling families in a PICU study of a psychoeducational support tool was feasible and that families perceived the intervention to be beneficial. The authors of 2 studies found that journaling or narrative writing interventions were acceptable to families,49,50 although in 1 study participation in journaling was low (32%).44 The authors of 1 study found that participant attendance at educational sessions was 83% for 6 1-hour sessions and that 70% of participants were “very satisfied” with the contents of the intervention.44 In each of these studies, parents reported that they perceived the intervention to be beneficial.
Assessment of Risk of Bias
The range of scores on the Downs and Black21 checklist was from 11 to 26 out of a possible 26 points. The median score was 21 points, indicating that most studies were well designed. Lower scores tended to occur in studies designed as feasibility or pilot studies with small sample sizes. Risks of bias common to many of the included studies were related to the inability to blind participants to intervention or control group status and a lack of specification as to whether those assessing outcomes were blinded to subjects’ intervention or control group status.
Meta-Analyses of Parent Outcomes
In Fig 3, we present forest plots of SMDs between intervention and control groups for RCTs by using validated measures to evaluate the intervention effects on parent anxiety, depression, or stress. For anxiety and stress, the pooled intervention effect was statistically significant and in the direction of lower symptom burden among the intervention group (anxiety SMD: −0.29, 95% confidence interval [CI]: −0.53 to −0.57; stress SMD: −0.78, 95% CI: −1.24 to −0.32). Heterogeneity was high, with I2 statistics of 65.7% for anxiety and 91.0% for stress, indicating that the variation in effect estimates between studies was more than would be expected to occur by chance (ie, true effect sizes likely differ between studies). For depression, we found no evidence of lower symptom burden (depression SMD: −0.014, 95% CI: −0.18 to 0.15), and heterogeneity was low (I2 = 14.2%).
FIGURE 3.
Pooled effect sizes for RCTs of coping interventions for parents of hospitalized children. Weights are from random effects models. ED, educational intervention.
Meta-Analyses of Risk of Bias
In Fig 4, we present funnel plots of the RCTs included in the pooled effect estimates and forest plots. The funnel plots for anxiety and depression are largely symmetric, suggesting low risk of publication bias, although each plot contains 1 point outside the lower pseudo-95% confidence limits representing a small study with large SE and large effect size. The plot for stress contains numerous outliers: 3 representing studies with large effect sizes and 3 representing studies with small effect sizes. The presence of outliers suggests that risk of bias is present. A possible source of bias is reporting bias (ie, researchers may be more likely to report stress results when findings are statistically significant). Because stress was often a secondary outcome, the risk of reporting bias is higher than for primary outcomes.
FIGURE 4.
Funnel plots for RCTs measuring anxiety, depression, and stress, with pseudo-95% confidence limits.
Discussion
In this literature review, we identified 32 studies of coping support interventions for parents of hospitalized children published in English between 1985 and 2016. Interventions varied in their content, but all included at least one of the following elements: education, opportunities for ER and self-care, and provision of SS. The authors of all studies included in the systematic review found evidence that coping support interventions had some effect on improving parent, child, or family outcomes, or that coping support interventions were feasible to implement. The results of meta-analyses of RCTs of coping support interventions revealed that parents who received coping support interventions had lower anxiety and stress symptoms than controls but not statistically significantly lower depression symptoms.
The present finding that participation in coping support interventions improved parent anxiety and stress is consistent with findings of a systematic review and meta-analysis of coping interventions for parents of children with chronic illness in community settings.13 In contrast, in a recent meta-analysis by Mendelson et al,19 the authors found that NICU-based maternal depression- and anxiety-reduction interventions reduced depression symptoms but not anxiety symptoms, and interventions including cognitive behavior therapy were most effective at reducing depression. Several key differences between the present review and Mendelson’s likely account for differences in findings. First, the present review did not include the cognitive behavior therapy–based interventions found to be most effective at reducing depression symptoms in Mendelson’s meta-analyses. Second, Mendelson’s analyses were limited to interventions for mothers of critically ill neonates, who are at higher risk for postpartum depression than the heterogeneous group of parents included in the present systematic review. Both the present review and Mendelson’s findings revealed that treatments effective for depression are not effective for reducing parent anxiety associated with a child’s hospitalization. Neither review revealed evidence that interventions designed to provide education or coping support are effective at reducing parent depression.
Parents value services to support their emotional well-being as they cope with a child’s hospitalization.14,18,44,49,50 However, the shortage of mental health clinicians62 and the lack of reimbursement mechanisms for provision of mental health care to parents of hospitalized children63 may present challenges to implementation of such services. For hospitals and clinical teams unable to invest substantial resources in parent coping support programs, knowledge of effective interventions requiring limited time and resource investment may help inform development of interventions that are feasible to implement. Future multicenter investigations and studies involving diverse populations of parents could bolster the case for reimbursement mechanisms for parent coping support services.
In this present review, we found limited evidence that parent coping supports improved child hospital outcomes, in part because few studies measured child outcomes. Nevertheless, knowledge that children of parents with poor emotional health are less likely to thrive6–9,64–67 provides support for the idea that parent interventions have the potential to improve child hospital outcomes. Possible mechanisms by which better parent emotional health may improve child health include increasing parents’ ability to participate in a child’s hospital care, preparedness to receive information, and empowerment when participating in shared decision-making. The following practices could facilitate future study of child outcomes: research to investigate the mediating effect of parent emotional health on child outcomes, multicenter studies, use of a common set of child outcome measures, and use of a common schedule for outcomes measurement.
Several limitations of this review warrant consideration. First, findings from studies included in this review may not generalize to other populations. The majority of studies included in this review were single-center studies with small sample sizes. Second, most interventions were designed for parents of children with specific illnesses (eg, premature infants, children with a traumatic injury, or children hospitalized for stem cell transplants). Both the small sample sizes and the strict inclusion criteria for parent participation limit generalizability of the studies’ findings to other populations. In addition, results from the meta-analyses should be interpreted in the context that findings from diverse groups of parents of children with different types of conditions were aggregated. Third, many researchers used convenience samples or did not report refusal rates, raising questions about possible sampling bias. Finally, other unpublished studies relevant to this question may exist; we did not search the gray literature or conference abstracts to identify such studies.
Conclusions
Interventions to support parents in coping with a child’s hospitalization varied in their scope and content, and in this review we found evidence that coping support interventions can improve parent emotional outcomes. In particular, meta-analyses showed that coping support interventions are effective for improving parents’ anxiety and stress symptom burden. Generalizability of existing studies of parent coping support interventions is limited, and future research is needed, including multicenter studies, studies of diverse parent populations, and studies of the effects of parent coping support interventions on child outcomes.
Glossary
- CI
confidence interval
- ER
emotion regulation
- PTSS
posttraumatic stress symptom
- RCT
randomized controlled trial
- SMD
standardized mean difference
- SS
social or structural support
Footnotes
Dr Doupnik conceptualized and designed the study, participated in manuscript review for inclusion in the study and data extraction, conducted data synthesis, and drafted the initial manuscript; Drs Hill and Palakshappa participated in study conceptualization and design, assisted with data synthesis, drafted portions of the manuscript, and reviewed and revised the manuscript; Ms Bae, Shaik, and Worsley participated in study conceptualization and design, manuscript review for inclusion in the study and data extraction, assisted with data synthesis, and reviewed and revised the manuscript; Ms Qiu assisted in developing the literature search strategy, provided methodological oversight for manuscript review for inclusion in the study and data extraction, drafted portions of the submitted manuscript, assisted with data synthesis, and reviewed and revised the manuscript; Drs Marsac and Feudtner participated in study conceptualization and design, participated in data synthesis, provided oversight for the literature search, manuscript review, and data extraction, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This project was made possible with a Mapping the Landscape, Journeying Together grant from the Arnold P. Gold Foundation. Dr Doupnik was supported by a Ruth L. Kirschstein National Research Service Award institutional training grant T32-HP010026-11, funded by the National Institutes of Health. Drs Hill and Feudtner were supported by grant 15-1392 from the Aetna Foundation. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Oxley R. Parents’ experiences of their child’s admission to paediatric intensive care. Nurs Child Young People. 2015;27(4):16–21 [DOI] [PubMed] [Google Scholar]
- 2.Franck LS, Wray J, Gay C, Dearmun AK, Lee K, Cooper BA. Predictors of parent post-traumatic stress symptoms after child hospitalization on general pediatric wards: a prospective cohort study. Int J Nurs Stud. 2015;52(1):10–21 [DOI] [PubMed] [Google Scholar]
- 3.Rapoport A, Weingarten K. Improving quality of life in hospitalized children. Pediatr Clin North Am. 2014;61(4):749–760 [DOI] [PubMed] [Google Scholar]
- 4.Diaz-Caneja A, Gledhill J, Weaver T, Nadel S, Garralda E. A child’s admission to hospital: a qualitative study examining the experiences of parents. Intensive Care Med. 2005;31(9):1248–1254 [DOI] [PubMed] [Google Scholar]
- 5.Bent KN, Keeling A, Routson J. Home from the PICU: are parents ready? MCN Am J Matern Child Nurs. 1996;21(2):80–84 [DOI] [PubMed] [Google Scholar]
- 6.Placencia FX, McCullough LB. Biopsychosocial risks of parental care for high-risk neonates: implications for evidence-based parental counseling. J Perinatol. 2012;32(5):381–386 [DOI] [PubMed] [Google Scholar]
- 7.National Research Council (U.S.), Committee on Depression and the Healthy Development of Children Depression in Parents, Parenting, and Children Opportunities to Improve Identification, Treatment, and Prevention. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 8.Landolt MA, Ystrom E, Sennhauser FH, Gnehm HE, Vollrath ME. The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. J Child Psychol Psychiatry. 2012;53(7):767–774 [DOI] [PubMed] [Google Scholar]
- 9.Als LC, Picouto MD, Hau S-M, et al. Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med. 2015;16(5):e141–e149 [DOI] [PubMed] [Google Scholar]
- 10.Dionigi A, Sangiorgi D, Flangini R. Clown intervention to reduce preoperative anxiety in children and parents: a randomized controlled trial. J Health Psychol. 2014;19(3):369–380 [DOI] [PubMed] [Google Scholar]
- 11.Chui WY, Chan SW. Stress and coping of Hong Kong Chinese family members during a critical illness. J Clin Nurs. 2007;16(2):372–381 [DOI] [PubMed] [Google Scholar]
- 12.Svavarsdottir EK, Sigurdardottir AO. Developing a family-level intervention for families of children with cancer. Oncol Nurs Forum. 2006;33(5):983–990 [DOI] [PubMed] [Google Scholar]
- 13.Eccleston C, Fisher E, Law E, Bartlett J, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2015;(4):CD009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davidson JE, Powers K, Hedayat KM, et al. ; American College of Critical Care Medicine Task Force 2004-2005, Society of Critical Care Medicine . Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine task force 2004-2005. Crit Care Med. 2007;35(2):605–622 [DOI] [PubMed] [Google Scholar]
- 15.Eggenberger SK, Nelms TP. Being family: the family experience when an adult member is hospitalized with a critical illness. J Clin Nurs. 2007;16(9):1618–1628 [DOI] [PubMed] [Google Scholar]
- 16.Verhaeghe S, Defloor T, Van Zuuren F, Duijnstee M, Grypdonck M. The needs and experiences of family members of adult patients in an intensive care unit: a review of the literature. J Clin Nurs. 2005;14(4):501–509 [DOI] [PubMed] [Google Scholar]
- 17.Gallop KH, Kerr CEP, Nixon A, Verdian L, Barney JB, Beale RJ. A qualitative investigation of patients’ and caregivers’ experiences of severe sepsis. Crit Care Med. 2015;43(2):296–307 [DOI] [PubMed] [Google Scholar]
- 18.Barling JA, Stevens JA, Davies KM. The reality of hospitalisation: stories from family members of their hospital experience for adolescents and young adults living with and dying from cancer. Contemp Nurse. 2014;46(2):150–160 [DOI] [PubMed] [Google Scholar]
- 19.Mendelson T, Cluxton-Keller F, Vullo GC, Tandon SD, Noazin S. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics. 2017;139(3):e20161870. [DOI] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(1):b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ak J, Lakshmanagowda PB, G C M P, Goturu J. Impact of music therapy on breast milk secretion in mothers of premature newborns. J Clin Diagn Res. 2015;9(4):CC04–CC06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Als LC, Nadel S, Cooper M, Vickers B, Garralda ME. A supported psychoeducational intervention to improve family mental health following discharge from paediatric intensive care: feasibility and pilot randomised controlled trial. BMJ Open. 2015;5(12):e009581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beheshtipour N, Baharlu SM, Montaseri S, Razavinezhad Ardakani SM. The effect of the educational program on Iranian premature infants’ parental stress in a neonatal intensive care unit: a double-blind randomized controlled trial. Int J Community Based Nurs Midwifery. 2014;2(4):240–250 [PMC free article] [PubMed] [Google Scholar]
- 25.Cobiella CW, Mabe PA, Forehand RL. A comparison of two stress-reduction treatments for mothers of neonates hospitalized in a neonatal intensive care unit. Child Health Care. 1990;19(2):93–100 [DOI] [PubMed] [Google Scholar]
- 26.Lai H-L, Chen C-J, Peng T-C, et al. Randomized controlled trial of music during kangaroo care on maternal state anxiety and preterm infants’ responses. Int J Nurs Stud. 2006;43(2):139–146 [DOI] [PubMed] [Google Scholar]
- 27.Melnyk BM, Feinstein NF. Mediating functions of maternal anxiety and participation in care on young children’s posthospital adjustment. Res Nurs Health. 2001;24(1):18–26 [DOI] [PubMed] [Google Scholar]
- 28.Melnyk BM, Feinstein NF, Alpert-Gillis L, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5). Available at: www.pediatrics.org/cgi/content/full/118/5/e1414 [DOI] [PubMed] [Google Scholar]
- 29.Melnyk BM. Coping with unplanned childhood hospitalization: effects of informational interventions on mothers and children. Nurs Res. 1994;43(1):50–55 [PubMed] [Google Scholar]
- 30.Melnyk BM, Alpert-Gillis L, Feinstein NF, et al. Creating opportunities for parent empowerment: program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113(6). Available at: www.pediatrics.org/cgi/content/full/113/6/e597 [DOI] [PubMed] [Google Scholar]
- 31.Meyer EC, Coll CT, Lester BM, Boukydis CF, McDonough SM, Oh W. Family-based intervention improves maternal psychological well-being and feeding interaction of preterm infants. Pediatrics. 1994;93(2):241–246 [PubMed] [Google Scholar]
- 32.Mianaei SJ, Karahroudy FA, Rassouli M, Tafreshi MZ. The effect of creating opportunities for parent empowerment program on maternal stress, anxiety, and participation in NICU wards in Iran. Iran J Nurs Midwifery Res. 2014;19(1):94–100 [PMC free article] [PubMed] [Google Scholar]
- 33.Burke SO, Handley-Derry MH, Costello EA, Kauffmann E, Dillon MC. Stress-point intervention for parents of repeatedly hospitalized children with chronic conditions. Res Nurs Health. 1997;20(6):475–485 [DOI] [PubMed] [Google Scholar]
- 34.Burke SO, Harrison MB, Kauffmann E, Wong C. Effects of stress-point intervention with families of repeatedly hospitalized children. J Fam Nurs. 2001;7(2):128–158 [Google Scholar]
- 35.Manne S, Mee L, Bartell A, Sands S, Kashy DA. A randomized clinical trial of a parent-focused social-cognitive processing intervention for caregivers of children undergoing hematopoetic stem cell transplantation. J Consult Clin Psychol. 2016;84(5):389–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marsac ML, Hildenbrand AK, Kohser KL, Winston FK, Li Y, Kassam-Adams N. Preventing posttraumatic stress following pediatric injury: a randomized controlled trial of a web-based psycho-educational intervention for parents. J Pediatr Psychol. 2013;38(10):1101–1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jotzo M, Poets CF. Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics. 2005;115(4):915–919 [DOI] [PubMed] [Google Scholar]
- 38.Kadivar M, Seyedfatemi N, Akbari N, Haghani H. The effect of narrative writing on maternal stress in neonatal intensive care settings. J Matern Fetal Neonatal Med. 2015;28(8):938–943 [DOI] [PubMed] [Google Scholar]
- 39.Preyde M, Ardal F. Effectiveness of a parent “buddy” program for mothers of very preterm infants in a neonatal intensive care unit. CMAJ. 2003;168(8):969–973 [PMC free article] [PubMed] [Google Scholar]
- 40.Curley MA. Effects of the nursing mutual participation model of care on parental stress in the pediatric intensive care unit. Heart Lung. 1988;17(6, pt 1):682–688 [PubMed] [Google Scholar]
- 41.Curley MA, Wallace J. Effects of the nursing mutual participation model of care on parental stress in the pediatric intensive care unit–a replication. J Pediatr Nurs. 1992;7(6):377–385 [PubMed] [Google Scholar]
- 42.Daeyoung W. Effects of programmed information on coping behavior and emotions of mothers of young children undergoing IV procedures. Taehan Kanho Hakhoe Chi. 2006;36(8):1301–1307 [DOI] [PubMed] [Google Scholar]
- 43.Carvalho AE, Linhares MB, Padovani FH, Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. Span J Psychol. 2009;12(1):161–170 [DOI] [PubMed] [Google Scholar]
- 44.Feeley N, Zelkowitz P, Charbonneau L, et al. Assessing the feasibility and acceptability of an intervention to reduce anxiety and enhance sensitivity among mothers of very low birth-weight infants. Adv Neonatal Care. 2008;8(5):276–284 [DOI] [PubMed] [Google Scholar]
- 45.Segre LS, Chuffo-Siewert R, Brock RL, O’Hara MW. Emotional distress in mothers of preterm hospitalized infants: a feasibility trial of nurse-delivered treatment. J Perinatol. 2013;33(12):924–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Svavarsdottir EK, Sigurdardottir AO. Benefits of a brief therapeutic conversation intervention for families of children and adolescents in active cancer treatment. Oncol Nurs Forum. 2013;40(5):E346–E357 [DOI] [PubMed] [Google Scholar]
- 47.Thygeson MV, Hooke MC, Clapsaddle J, Robbins A, Moquist K. Peaceful play yoga: serenity and balance for children with cancer and their parents. J Pediatr Oncol Nurs. 2010;27(5):276–284 [DOI] [PubMed] [Google Scholar]
- 48.Mouradian LE, DeGrace BW, Thompson DM. Art-based occupation group reduces parent anxiety in the neonatal intensive care unit: a mixed-methods study. Am J Occup Ther. 2013;67(6):692–700 [DOI] [PubMed] [Google Scholar]
- 49.Macnab AJ, Beckett LY, Park CC, Sheckter L. Journal writing as a social support strategy for parents of premature infants: a pilot study. Patient Educ Couns. 1998;33(2):149–159 [DOI] [PubMed] [Google Scholar]
- 50.DeMaso DR, Gonzalez-Heydrich J, Erickson JD, Grimes VP, Strohecker C. The experience journal: a computer-based intervention for families facing congenital heart disease. J Am Acad Child Adolesc Psychiatry. 2000;39(6):727–734 [DOI] [PubMed] [Google Scholar]
- 51.Macner-Licht B, Rajalingam V, Bernard-Opitz V. Childhood leukaemia: towards an integrated psychosocial intervention programme in Singapore. Ann Acad Med Singapore. 1998;27(4):485–490 [PubMed] [Google Scholar]
- 52.Melnyk BM, Alpert-Gillis LJ, Hensel PB, Cable-Beiling RC, Rubenstein JS. Helping mothers cope with a critically ill child: a pilot test of the COPE intervention. Res Nurs Health. 1997;20(1):3–14 [DOI] [PubMed] [Google Scholar]
- 53.Won D. Effects of programmed information on coping behavior and emotions of mothers of young children undergoing IV procedures. J Korean Acad Nurs. 2006;36(8):1301–1307 [DOI] [PubMed] [Google Scholar]
- 54.Starks H, Doorenbos A, Lindhorst T, et al. The Family Communication study: a randomized trial of prospective pediatric palliative care consultation, study methodology and perceptions of participation burden. Contemp Clin Trials. 2016;49:15–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publ; 1984 [Google Scholar]
- 56.Sameroff A, Fiese B. Transactional regulation and early intervention In: Shonkoff JP, Meisels SJ, eds. Handbook of Early Childhood Intervention. Cambridge, UK: Cambridge University Press; 1990 [Google Scholar]
- 57.Jotzo M. Trauma Fruehgeburt? Ein Programm Zur Krisenintervention Bei Eltern [The Trauma of Premature Birth? A Crisis Intervention Program for Parents]. Frankfurt am Main, Germany: Peter Lang; 2004 [Google Scholar]
- 58.Carver C. A cybernetic model of self-attention processes. J Pers Soc Psychol. 1979;37(8):1251–1281 [Google Scholar]
- 59.Johnson J, Fieler V, Jones L, Wlasowicz G, Mitchell M. Self-Regulation Theory: Applying Theory to Your Practice. Pittsburgh, PA: Oncology Nursing Press; 1997 [PubMed] [Google Scholar]
- 60.Wright L, Leahey M. Nurses and Families: A Guide to Family Assessment and Intervention. Philadelphia, PA: F.A. Davis Company; 2012 [Google Scholar]
- 61.Marsac ML, Funk JB, Nelson L. Coping styles, psychological functioning and quality of life in children with asthma. Child Care Health Dev. 2007;33(4):360–367 [DOI] [PubMed] [Google Scholar]
- 62.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323–1328 [DOI] [PubMed] [Google Scholar]
- 63.Bierenbaum ML, Katsikas S, Furr A, Carter BD. Factors associated with non-reimbursable activity on an inpatient pediatric consultation-liaison service. J Clin Psychol Med Settings. 2013;20(4):464–472 [DOI] [PubMed] [Google Scholar]
- 64.Pak L, Allen PJ. The impact of maternal depression on children with asthma. Pediatr Nurs. 2012;38(1):11–19, 30 [PubMed] [Google Scholar]
- 65.Barker DH, Quittner AL. Parental depression and pancreatic enzymes adherence in children with cystic fibrosis. Pediatrics. 2016;137(2):e20152296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Board R, Ryan-Wenger N. State of the science on parental stress and family functioning in pediatric intensive care units. Am J Crit Care. 2000;9(2):106–122, quiz 123–124 [PubMed] [Google Scholar]
- 67.Guevara JP, Mandell D, Danagoulian S, Reyner J, Pati S. Parental depressive symptoms and children’s school attendance and emergency department use: a nationally representative study. Matern Child Health J. 2013;17(6):1130–1137 [DOI] [PMC free article] [PubMed] [Google Scholar]