Abstract
Introduction
Rapidly destructive osteoarthritis is characterized by a severe destruction of the hip joint developing over short periods of time. However, to date, there is no agreement on the biological process that triggers this condition. The aim of this report is to present a case of rapidly destructive osteoarthritis.
Case report
We report a case of a 76 year-old female who presented with hip pain of sudden onset and normal X-rays. Six weeks later she presented with increased pain intensity, functional limitation and evidence of a collapse of the femoral head in the X-rays.
Discussion
Rapidly destructive osteoarthritis of the hip is a complex entity that might be more frequent than previously described and which clinical course could vary between few weeks and several months. In order to make an accurate diagnosis, other causes of massive destruction of the joint should be excluded.
Keywords: Hip osteoarthritis, Rapidly destructive, Total hip replacement
1. Introduction
Rapidly destructive osteoarthritis (RDOA) is an unusual manifestation of osteoarthritis of the hip.1 It is more common in elderly female patients and is characterized by pain and functional limitation of the hip, accompanied by an extremely rapid destruction of the joint progressing over only a few months and is not attributed to traumatic, infectious, tumorous, ischemic, neuropathic or inflammatory causes.1, 2 This pathology typically develops over a period of 2–16 months from the onset of symptoms according to current studies.1, 3 Herein we present a case of RDOA of the hip that developed over a period of less than 6 weeks.
2. Case report
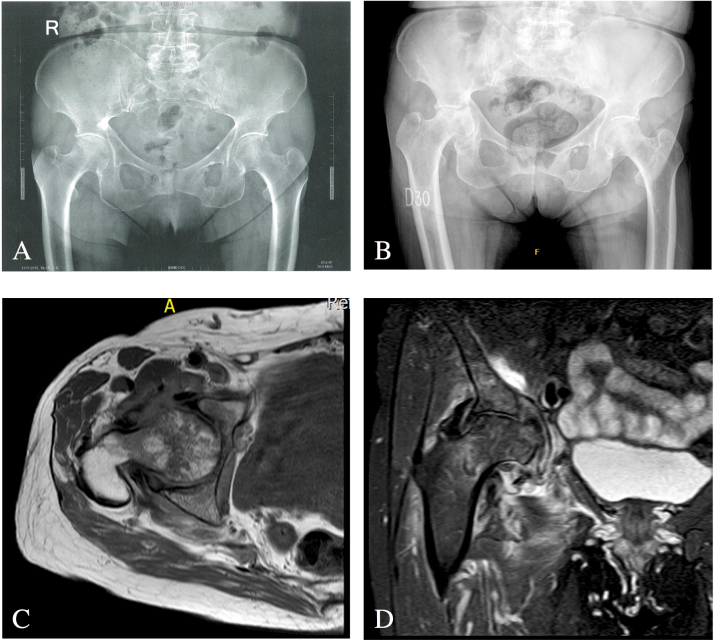
A 76 year-old female with a history of diabetes mellitus, is admitted into the emergency room with rapidly progressive pain of the right hip. X-rays of the pelvis showed bilateral narrowing of the joint space with no signs of acute trauma (Fig. 1A). The patient was discharged and symptoms were treated with non-steroidal anti-inflammatory drugs. Four weeks later, she presented severe pain in the same joint and progressive functional impairment characterized by decreased range of motion, right lower limb shortening and the need for walking aids. X-rays of the hip obtained six weeks after the initial complain, evidenced a collapse of the femoral head in its superolateral aspect, protrusio acetabuli and minimal proliferative changes (Fig. 1B). The MRI of the right hip revealed soft tissue edema in the iliopsoas, external rotators and gluteus minor, bone marrow edema in the acetabulum, femoral head and neck and the presence of irregular focal low-intensity bands on T1-weighted sequence (Fig. 1C) and high-intensity bands on T2-weighted sequence (Fig. 1D). Infectious, malignant and inflammatory pathologies were ruled out. Red blood cell count, white blood cell count, erythrocyte sedimentation rate, C-reactive protein and rheumatoid factor were normal. Joint aspiration and synovial fluid cultures for typical and atypical microorganisms were negative. Polymerase chain reaction for mycobacterium species (including M. tuberculosis) was also negative. Transcutaneous bone biopsy of the femoral head core (Tru-cut™ biopsy) also excluded neoplastic, infectious or necrotic etiologies and only reported ischemic and bone repair changes. The patient underwent total hip replacement surgery with a posterolateral approach. Post-operative x-rays can be observed in Fig. 4. Intraoperative findings are observed in Fig. 2. A ZCA® All Poly Acetabular cemented cup and a VerSys® Advocate ® cemented stem were implanted (Zimmer, Inc. Warsaw, IN, USA). Histological examination of the femoral head revealed thinning of trabeculae, microfractures, bleeding, reactive cartilage and fibrosis (Fig. 3). At the 4th-month follow-up visit after surgery, the patient was walking without external aids, was free of pain in the operated joint.
Fig. 1.
(A) X-rays of the pelvis at the onset of symptoms: mild narrowing of the joint space in both hips. (B) X-rays of the hip six weeks after the onset of symptoms: collapse of the right femoral, protrusio acetabuli and minimal proliferative changes (C) MRI T1-sequence right hip: bone marrow edema in the acetabulum, femoral head and neck and the irregular focal low-intensity bands. (D) MRI T2-sequence right hip: bone marrow edema in the acetabulum, femoral head and neck and the irregular focal high-intensity bands.
Fig. 4.

Post-operative x-ray of the affected hip.
Fig. 2.
Intraoperative findings (A) Acetabular fracture and (B), (C) and (D) collapsed femoral head.
Fig. 3.
Histopathology findings of the femoral head: (A) Cartilage thinning, (B) Fibrosis, formation of new bone, trabeculae thinning, hemorrhage, (C) Zones of bone necrosis compromising 20% of the whole sample and (D) Reactive changes.
3. Discussion
Although first described in 1957, the term “rapidly destructive osteoarthritis” was only introduced two decades later, when Lequesne established the following diagnostic criteria: chondrolysis >2 mm in 1 year, or 50% joint-space narrowing in 1 year and no evidence of other forms of rapidly destructive arthropathy.3
Since then, several case reports have been published and many attempts have been carried out to elucidate the physiopathology of this entity1, 2 The most accepted theory is that the coexistence of rapidly developing chondrolysis and subchondral bone fractures is responsible for this massive, and rapid, destruction of the hip joint.1, 2, 3 However there is no agreement on the biological process that might trigger this condition.
This destruction of the hip joint occurring over short periods of time has drawn the attention of orthopedic surgeons, rheumatologists, radiologists and pathologists.1 As previously mentioned, RDOA mostly affects elderly women’s functionality and quality of life. Diagnosis requires studies that exclude other pathologies such as tumors or infections.3 Notwithstanding, it might not be as infrequent as some authors describe, mainly due to the number of cases reported during the last 30 years.1, 2, 4
Patients do not seem to share any baseline characteristics that might explain this type of presentation of osteoarthritis or an association of this pathology with race or ethnicity. However, it seems to affect more elderly females. Some authors have proposed that alterations such as inversion of the acetabular labrum,3 a posterior tilt of the pelvis4 and mechanical abnormalities of the hip5 may possibly trigger RDOA. Other authors believe that this pathology can be explained by the coexistence of rapidly developing chondrolysis and poor bone stock leading to subchondral bone fractures.1, 2, 3 Nevertheless, a number of studies assessing the bone mineral density of these patients conclude that there is no correlation between RDOA and generalized osteopenia or osteoporosis.3 Therefore, it is not clear whether these fractures trigger joint destruction or if the damage of the cartilage produces subchondral fractures.
Several other theories have attempted to explain the appearance of RDOA of the hip: the presence of mature osteoclasts in the synovial tissue,6 altered microvasculature,7 elevated levels of collagen in serum and urine,8 bone ischemia9 and metabolic diseases.10 However, none of these descriptions is conclusive and the exact mechanism by which this entity occurs remains to be understood.
We presented a case of RDOA of the hip that occurred within six weeks after the onset of the symptoms, faster than typically reported.1 Also, this patient had compromise of both the femoral head and the acetabulum. This mirror-like lesion might be the result of an increase in the load over the bearing zone of the acetabulum resulting from the collapse of the femoral head.
Histopathological studies were necessary in order to diagnose RDOA of the hip. Most of the necrosis, reactive bone changes, formation of new bone and alterations in blood vessels were related to the subchondral bone fracture. Additionally, we observed that all trabecular bone was thinned, which corresponds to osteoporotic bone. This finding is not normally seen in femoral heads that are routinely studied for osteoarthrosis. Therefore, concur that one of the triggering mechanisms for RDOA is a poor bone stock that is transitory or purely local.
Consequently, we consider that the mechanism leading to weak subchondral bone might be dependent on humoral pathways leading to a rapid alteration in the osseous environment and consequently an increase in bone reabsorption.
In conclusion, RDOA of the hip is a complex entity of which the exact pathophysiological mechanism has not yet been determined. However, it might not be as infrequent as previously described and its clinical course could vary between weeks to several months. Even though RDOA of the hip is successfully treated with joint replacement surgery, in order to determine that the patient’s signs and symptoms are due to this entity, infectious, neurological, metabolic, endocrine, or inflammatory diseases must be ruled out.
Conflict of interest
The authors have none to declare.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Informed consent
Local IRB did not request the consent form patients as per the study design.
Funding
This study did not receive any funding.
Acknowledgments
The authors wish to thank Camilo Gutierrez for his invaluable service in the editing, modifications and assembling of this paper.
References
- 1.Mavrogenis A.F., Flevas D.A., Panagopoulos G.N. Rapid destructive arthritis of the hip revisited. Eur J Orthop Surg Traumatol. 2015;25(7):1115–1120. doi: 10.1007/s00590-015-1676-4. [DOI] [PubMed] [Google Scholar]
- 2.Bock W., Greenway D., Major P.A. Imaging hip disease: abnormalities. Radiology. 2017:461–466. doi: 10.1148/radiology.186.2.8421751. [DOI] [PubMed] [Google Scholar]
- 3.Fukui K., Kaneuji A., Fukushima M., Matsumoto T. Early MRI and intraoperative findings in rapidly destructive osteoarthritis of the hip: a case report. Int J Surg Case Rep. 2015;8:13–17. doi: 10.1016/j.ijscr.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Homma Y., Baba T., Sumiyoshi N. Rapid hip osteoarthritis development in a patient with anterior acetabular cyst with sagittal alignment change. Case Rep Orthop. 2014;2014:1–5. doi: 10.1155/2014/523426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Motomura G., Yamamoto T., Nakashima Y., Shuto T., Jingushi S., Iwamoto Y. Outcome of the contralateral hip in rapidly destructive arthrosis after total hip arthroplasty. A preliminary report. J Arthroplasty. 2006;21(7):1026–1031. doi: 10.1016/j.arth.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Ogawa K., Mawatari M., Komine M. Mature and activated osteoclasts exist in the synovium of rapidly destructive coxarthrosis. J Bone Miner Metab. 2007;25(6):354–360. doi: 10.1007/s00774-007-0761-0. [DOI] [PubMed] [Google Scholar]
- 7.Yamakawa T., Sudo A., Tanaka M., Uchida A. Microvascular density of rapidly destructive arthropathy of the hip joint. J Orthop Surg (Hong Kong) 2005;13(1):40–45. doi: 10.1177/230949900501300107. [DOI] [PubMed] [Google Scholar]
- 8.Garnero P., Charni N., Juillet F., Conrozier T., Vignon E. Increased urinary type II collagen helical and C telopeptide levels are independently associated with a rapidly destructive hip osteoarthritis. Ann Rheum Dis. 2006;65(1):1639–1644. doi: 10.1136/ard.2006.052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryu K.N., Kim E.J., Yoo M.C., Park Y.K., Sartoris D.J., Resnick D. Ischemic necrosis of the entire femoral head and rapidly destructive hip disease: potential causative relationship. Skeletal Radiol. 1997;26(3):143–149. doi: 10.1007/s002560050210. [DOI] [PubMed] [Google Scholar]
- 10.Reference C. Regular case report ochronotic arthropathy: rapid destructive hip osteoarthritis associated with metabolic disease. 2011;474–477. [DOI] [PubMed]