Abstract
Lateral meniscus dislocation, as a cause of atraumatic knee locking, is often attributed to a discoid meniscus which can be readily diagnosed on MRI. In the absence of radiological abnormality, a dislocated lateral meniscus is a rare occurrence. We present a case of a 14 year old male who presented with atraumatic sequential locking of bilateral knees 6 months apart. Although on both occasions, MRI was normal, arthroscopy demonstrated dislocating lateral menisci that were subsequently surgically stabilised. To date, there have been no reports describing this phenomenon bilaterally in the same patient. A high index of suspicion is needed to evaluate a locked knee in an adolescent in the absence of trauma or a radiological abnormality. Furthermore there is a probability of a similar occurrence in the opposite knee.
Keywords: Knee, Lateral meniscus, Dislocation, Subluxation, Locking
1. Introduction
Knee locking is a common presentation of meniscal pathology or an intra-articular loose body.4 Lateral meniscal pathology contributing to knee locking is often associated with meniscal tears or congenital discoid menisci. Atraumatic meniscal dislocation of an apparently structurally normal lateral meniscus is uncommon. 3 We report a case of a 14 year old male presenting with atraumatic sequential locking of both knees with no radiological abnormality. Arthroscopy demonstrated dislocating lateral menisci. To date, no report has described this phenomenon occurring in both knees of a single patient.
2. Case report
A 14 year old male presented to our clinic complaining of 2 episodes of knee locking. The first episode was getting up from a chair and the second whilst walking at normal pace. During both episodes, the knee locked in a flexed position and reduced to full extension with an audible pop. He denied any history of trauma or injury. His past medical history included polycystic kidney disease.
On examination, a small effusion was present without clinical evidence of a mechanical block to extension. Lateral joint line tenderness was present and range of movement was from full extension to 60 ° flexion limited by pain. Collateral ligaments were stable. Cruciate ligament and provocative testing was abandoned due to pain.
He underwent Magnetic Resonance Imaging (MRI) of the left knee revealing no intra-articular pathology. Subsequently, a knee arthroscopy was performed. Examination under anaesthesia did not reveal hyper-laxity. Intra-operatively no static structural abnormality was detected however, probing the lateral meniscus revealed a hypermobile dislocating posterior horn of the lateral meniscus with a defect in the menisco-capsular junction (Fig. 1a, b). No other meniscal or ligamentous pathology was identified. Consequently, repair by an all-inside technique using suture anchors was performed. (Fast-Fix 360 meniscal repair system – Smith and Nephew Plc, London) (Fig. 1c)
Fig. 1.
(a) Arthroscopic image showing dislocating lateral meniscus – Left Knee. (b) Abrthroscopic image showing defect in the Menisco-capsular junction posterior horn lateral meniscus – Left Knee. (c) Acrthroscopic image showing surgically stabilised lateral meniscus using suture anchors – Left Knee.
Post-operatively full weight bearing was recommended with range of movement controlled from 0 to 45 ° for 4 weeks using a brace. Thereafter, full range of movement physiotherapy was commenced leading to complete resolution of symptoms and return to full function.
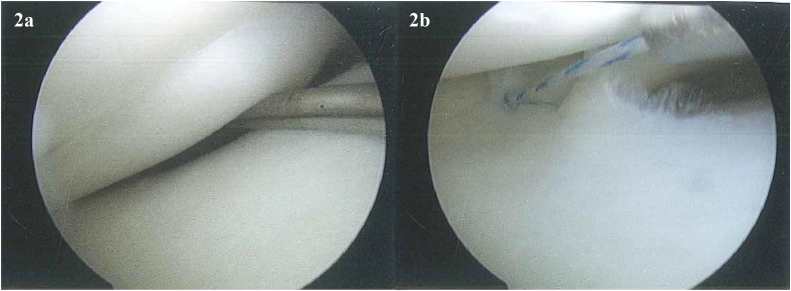
He re-presented 6 months later complaining of similar symptoms of locking and audible popping in his opposite right knee. Clinical examination was similar to the left knee and MRI was unremarkable. He underwent arthroscopy for his right knee and findings were identical to the opposite side (Fig. 2a). The same treatment (Fig. 2b) and post-operative management was advocated. Subsequently, his right knee also returned to full function.
Fig. 2.
(a) Aarthroscopic image showing dislocating lateral meniscus – Right Knee. (b) Abrthroscopic image showing surgically stabilised lateral meniscus using suture anchors – Right Knee..
3. Discussion
A limited number of reports discuss non-discoid lateral meniscal dislocation causing knee locking; all of which have been unilateral.1, 2, 3, 4, 5 Some have been atraumatic similar to our case.2, 4 However, our report is first to present this phenomenon occurring bilaterally in a single patient. Authors for this paper have defined meniscal dislocation as complete displacement of the meniscus from normal anatomical position.
Lateral meniscal dislocation can be difficult to diagnose clinically and specific tests such as McMurrays may be negative.2, 3 If the dislocation is reduced, MRI may be normal due to the static nature of imaging as demonstrated by our case and previous reports.2, 5 Authors in this paperDislocation in this paper has been defined as the complete displacement
Simonian et al.,5 reported 3 cases of lateral meniscal instability defined by completely displaced bucket handle meniscal separation. There was no tear in the substance of meniscus. These cases had normal initial MRI imaging. However, at arthroscopy 2 patients were found to have displaced bucket handle tears of the lateral meniscus and 1 patient had meniscal dislocation with chronical ACL insufficiency. In contrast, our case had isolated dislocating lateral meniscus with no other intra-articular pathology.
Mechanism behind dislocation of the lateral meniscus is still unclear. Two studies using MRI analysis for meniscal instability postulate that disruption of the popliteomeniscal fascicles between the lateral meniscus and popliteus may cause increased mobility of the meniscus.5, 6 One report discussed posterior meniscular-capsular separation as a cause.4
Breitenseher et al. 1 performed MRI evaluation of 60 symptomatic knees and found 4 medial menisci and 1 lateral meniscus subluxation defined as a distance of ≥ 3 mm between the peripheral border of the meniscus and edge of the tibial plateau. A significant correlation between meniscal dislocation and joint effusion was found. A hypothesis was made that effusion may lead to distension of the joint capsule with retraction of meniscotibial and meniscofemoral ligaments leading to subluxation. However, it was noted that a large number of patients (n = 55) with knee effusion did not exhibit meniscal displacement. Garafalo et al.,2 reported lateral meniscal dislocation in a 19 year old male and hypothesised that a subluxing lateral meniscus could be a congenital anatomical variant, which may have loose menisco-tibial ligaments leading to ligamentous failure and subluxation with minimal trauma.
In previous reports lateral meniscal dislocation was treated by surgical fixation, using sutures, with resolution of symptoms and good functional outcomes.2, 3, 4, 5 Excellent outcomes from our case, after using suture anchors for both lateral menisci, provides further evidence that lateral meniscal dislocation should be treated by surgical fixation.
4. Conclusion
Lateral meniscal dislocation as a cause of atraumatic knee locking is rare. Our case is first to highlight that it is possible for a patient to have this phenomenon in both knees. Clinical examination and MRI may be equivocal or normal with this pathology, hence a high index of suspicion is warranted. Early arthroscopic exploration and surgical fixation is recommended for prompt diagnosis and treatment with good outcome.
Conflict of interest
The authors have none to declare.
Authors contributions
All authors contributed to the final manuscript and were involved in the patient’s care. MS and DS performed the surgery. ZH and MS prepared the manuscript with literature search.
Contributor Information
Zakir Haider, Email: zakirhaider10@gmail.com.
Mujahid Ali Syed, Email: masyed@doctors.org.uk.
Deepak Saran, Email: sarands@hotmail.co.uk.
References
- 1.Breitenseher M.J., Trattnig S., Dobrocky I. MR imaging of meniscal subluxation in the knee? Acta Radiol. 1997;38(5):876–879. doi: 10.1080/02841859709172428. [DOI] [PubMed] [Google Scholar]
- 2.Garofalo R., Kombot C., Borens O., Djahangiri A., Mouhsine E. Locking knee caused by subluxation of the posterior horn of the lateral meniscus? Knee Surg Sports Traumatol Arthrosc. 2005;13(7):569–571. doi: 10.1007/s00167-004-0581-x. [DOI] [PubMed] [Google Scholar]
- 3.George M., Wall E.J. Locked knee caused by meniscal subluxation: magnetic resonance imaging and arthroscopic verification? Arthroscopy. 2003;19(8):885–888. doi: 10.1016/s0749-8063(03)00749-7. [DOI] [PubMed] [Google Scholar]
- 4.Pinkowsky G.J., Lynch S. Locked knee caused by lateral meniscal capsular disruption: verification by magnetic resonance imaging and arthroscopy? Am J Orthop. 2013;42(12):E116–E117. [PubMed] [Google Scholar]
- 5.Simonian P.T., Sussmann P.S., Wickiewicz T.L. Popliteomeniscal fasciculi and the unstable lateral meniscus: clinical correlation and magnetic resonance diagnosis? Arthroscopy. 1997;13(5):590–596. doi: 10.1016/s0749-8063(97)90185-7. [DOI] [PubMed] [Google Scholar]
- 6.Suganuma J., Mochizuki R., Inoue Y., Yamabe E., Ueda Y., Kanauchi T. Magnetic resonance imaging and arthroscopic findings of the popliteomeniscal fascicles with and without recurrent subluxation of the lateral meniscus? Arthroscopy. 2012;28(4):507–516. doi: 10.1016/j.arthro.2011.08.311. [DOI] [PubMed] [Google Scholar]