Abstract
Caesarean section (CS) may increase the risk of asthma and allergic diseases in children, but previous studies could not preclude the potential confounding effect of underlying medical indications for CS. We aim to assess the association between CS itself (without indications) and risks of asthma and allergic rhinitis in children. The 2014 Shanghai Children’s Health, Education and Lifestyle Evaluation was a large population-based survey with cluster random probability sampling in 26 primary schools in Shanghai, China, in 2014. The mode of delivery and child history of asthma and allergic rhinitis were reported by parents. We included 12639 children in our analysis. CS without medical indication was associated with an increased risk of childhood asthma. CS without medical indication and CS for fetal complications were associated with increased risks of childhood allergic rhinitis, respectively. In children fed by exclusive breastfeeding or mixed feeding in the first four months after birth, these risks were not significant. In contrast, in children fed by exclusive formula milk, CS was highly significantly associated with childhood asthma and allergic rhinitis. In conclusion, CS without medical indication was associated with increased risks of both childhood asthma and allergic rhinitis. Breastfeeding in early infancy may attenuate these risks.
Introduction
The global prevalence of childhood asthma has increased in the last 2–3 decades. For instance, the International Study of Asthma and Allergies in Childhood phase III showed an annual increase in prevalence of asthma by 0.12% on average in most of Asia-Pacific region from 2001 to 20101. A similar trend was found in childhood allergic rhinitis1. Mounting evidence suggests that cesarean section (CS) may be a risk factor for childhood asthma and allergic rhinitis2–4. However, most CS are performed for fetal and/or maternal indications in previous studies2, 3. And these indications themselves may be risk factors for childhood allergic disorders. For example, fetal growth restriction and pre-term birth are associated with a high likelihood of both CS and childhood allergic disorders5, 6, i.e., the observed associations might be in part due to confounding by indication. Even if such fetal and maternal complications are adjusted in multivariable modeling, residual confounding may still exist, making the validity of the conclusion uncertain. On the other hand, a number of studies have shown that close contact with older siblings and pets in early life may reduce the risk of childhood asthma7–9. Therefore, postpartum exposure may mask the association.
China has one of the highest CS rate in the world10. CS without medical indication, the majority of which are due to maternal request, is very common, accounting for nearly half of all CS11. The one-child-family policy has resulted in single children in most families while having pets is still uncommon in urban areas. Therefore, the urban China provides an ideal setting to study if CS by itself is associated with the risks of childhood allergic disorders.
We carried out this population-based study based on the 2014 Shanghai Children’s Health, Education and Lifestyle Evaluation (the SCHEDULE study) to investigate whether CS without medical indication is associated with the risks of asthma and allergic rhinitis in children.
Methods
The SCHEDULE study, a population-based cross-sectional survey with cluster random sampling, was conducted in primary schools in Shanghai, China, in June 2014. The Shanghai Municipality was divided into 17 districts and counties, from which seven were randomly selected. Based on a list of all primary schools in these 7 districts, 26 schools were randomly chosen. Pupils from Grade one to five were eligible for this study. In schools with less than 1000 pupils, all of them were eligible; whereas in schools with over 1000 pupils, half of the classes were randomly selected. Once a class was included, all pupils within the class were eligible. A weight was assigned to each subject based on the probability of sampling12, 13.
The study protocol was first approved by the Institutional Review Board (Shanghai Children’s Medical Center Research Ethics Committee). All methods were performed in accordance with the declaration of Helsinki. We worked with the Shanghai Education Commission and the selected schools to obtain school permissions for this survey.
A parental informed consent was obtained for each pupil. A self-administered questionnaire was completed by the parents, which included information on parental demographic characteristics, mode of delivery of the index child, diet, physical exercise in a week, psychological behaviors, and history of asthma, allergic rhinitis, autism, attention deficit hyperactivity disorder, dysaudia and diabetes. A questionnaire on the academic performance of each pupil was completed by their teachers. Height and weight of the pupils were measured at the schools. For this analysis, our focus is on CS and childhood asthma and allergic rhinitis.
Information on mode of delivery (CS vs. vaginal delivery) and breastfeeding was reported by parents. We further inquired whether the CS was performed due to woman or family request without medical indication, fetal complications, maternal diseases or pregnant complications, or other reasons. The fetal indications included dystocia, fetal distress, suspected macrosomia or fetal growth restriction, fetal malposition, multiple gestation. The maternal indications consisted of severe maternal chronic diseases or pregnancy complications such as congenital heart disease and severe hypertensive disorders in pregnancy. The other reasons for CS included the history of previous CS, placenta praevia, placental abruption, nuchal cord, premature aging of the placenta, and uterine malformation. Parents were asked if the index child was ever diagnosed by a doctor as having asthma or allergic rhinitis.
We first examined the association between maternal and infant demographic characteristics and mode of delivery. We then explored the associations between CS and the risks of childhood allergic diseases. We further examined the modifiable effect of postpartum breastfeeding on the association between CS and childhood allergic disorders in a stratified analysis. We defined a confounder as a covariant that changed the association between exposure and outcome by 10% or more. The potential confounders were included in the multivariate model. We identified the following potential confounders: maternal education levels (≤9, 10–12, 13–16, or ≥17 years), paternal education levels (≤9, 10–12, 13–16, or ≥17 years), family income (<3.0, 3.0–9.9, 10.0–29.9, or ≥30.0 in ten thousand RMB/year), gender (boy/girl), maternal history of gestational diabetes (including impaired glucose tolerance) (no/yes), and newborn resuscitation (no/yes). Missing data of the confounders were included as a separate category in the analysis. Logistic regression models with SURVEYLOGISTIC procedure and strata with district, school, grade and class in SAS 9.2 (SAS Institute Inc., Cary, North Carolina) were used. The results were presented as odds ratios (OR) and 95% confidence intervals (CI).
Results
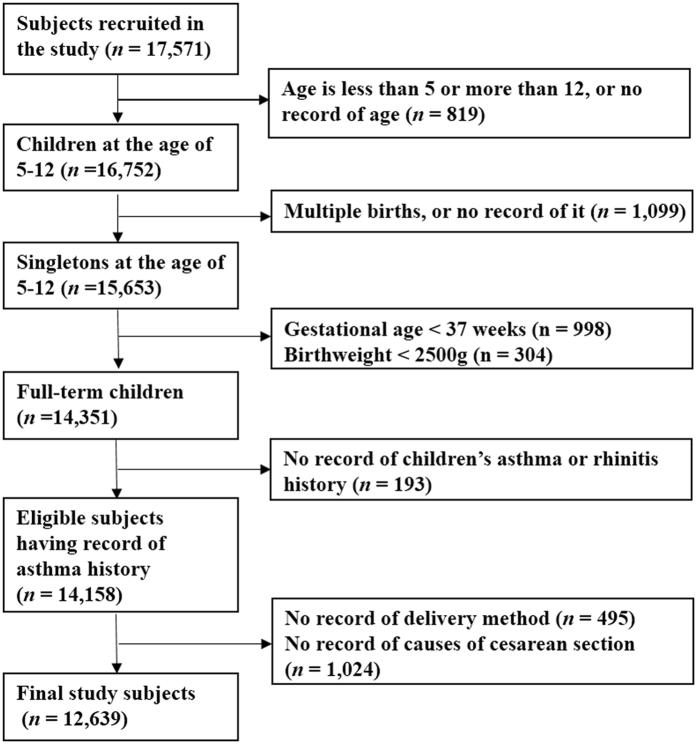
A total of 17571 pupils completed this population-based survey (response rate 99%). Figure 1 illustrates the population selection process. The final sample included 12639 pupils. We compared the 1519 excluded subjects with those remained in the analysis with regard to baseline characteristics and the prevalence of asthma and allergic rhinitis (Table S1). They look similar. Among them, 47% were delivered by CS (N = 5962). CS without medical indication, for fetal complications, maternal disorders, and other reasons accounted for 19% (N = 2369), 19% (N = 2424), 2% (N = 267), and 7% (N = 902), respectively (Table 1).
Figure 1.
Population flow chart of the population-based study.
Table 1.
Demographic, perinatal and child characteristics by mode of delivery in the population-based study.
| Characteristics | Vaginal delivery | CS without indications | CS for fetal complications | CS for maternal complications | CS for other reasons | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| Gender (boys) | 3541 | 53 | 1234 | 52 | 1307 | 54 | 142 | 53 | 490 | 54 |
| Age (yrs) | ||||||||||
| 5–6 | 304 | 5 | 158 | 7 | 130 | 5 | 12 | 4 | 61 | 7 |
| 7–8 | 2639 | 40 | 1010 | 43 | 1051 | 43 | 118 | 44 | 368 | 41 |
| 9–10 | 2639 | 40 | 896 | 38 | 897 | 37 | 107 | 40 | 342 | 38 |
| 11–12 | 1095 | 16 | 305 | 13 | 346 | 14 | 30 | 11 | 131 | 15 |
| Birth weight (g) | ||||||||||
| 2500–2999 | 838 | 13 | 257 | 11 | 289 | 12 | 74 | 28 | 103 | 11 |
| 3000–3499 | 2989 | 45 | 1048 | 44 | 876 | 36 | 103 | 39 | 396 | 44 |
| 3500–3999 | 1848 | 28 | 808 | 34 | 766 | 32 | 78 | 29 | 291 | 32 |
| ≥4000 | 515 | 8 | 188 | 8 | 452 | 19 | 8 | 3 | 87 | 10 |
| Newborn resuscitation | 25 | 0 | 53 | 2 | 1 | 0 | 23 | 9 | 102 | 11 |
| Feeding in the first 4 months | ||||||||||
| exclusive breastfeeding | 4492 | 67 | 1270 | 54 | 1373 | 57 | 134 | 50 | 537 | 60 |
| mixed feeding | 1341 | 20 | 684 | 29 | 715 | 29 | 80 | 30 | 224 | 25 |
| exclusive formula feeding | 775 | 12 | 399 | 17 | 319 | 13 | 53 | 20 | 134 | 15 |
| Passive smoking | ||||||||||
| no | 1835 | 27 | 595 | 25 | 739 | 30 | 72 | 27 | 237 | 26 |
| occasionally | 3462 | 52 | 1218 | 51 | 1199 | 49 | 129 | 48 | 444 | 49 |
| frequently | 1327 | 20 | 550 | 23 | 472 | 19 | 66 | 25 | 219 | 24 |
| Asthma | 177 | 3 | 111 | 5 | 92 | 4 | 14 | 5 | 34 | 4 |
| Allergic rhinitis | 427 | 6 | 465 | 20 | 64 | 3 | 64 | 24 | 153 | 17 |
| Gestational diabetes | 80 | 1 | 64 | 3 | 86 | 4 | 45 | 17 | 28 | 3 |
| Maternal educational level (yrs) | ||||||||||
| ≤9 | 2650 | 40 | 445 | 19 | 442 | 18 | 53 | 20 | 244 | 27 |
| 10–12 | 1765 | 26 | 633 | 27 | 631 | 26 | 55 | 21 | 206 | 23 |
| 13–16 | 1902 | 28 | 1155 | 49 | 1223 | 50 | 138 | 52 | 397 | 44 |
| ≥17 | 147 | 2 | 88 | 4 | 98 | 4 | 14 | 5 | 35 | 4 |
| Paternal education level (yrs) | ||||||||||
| ≤9 | 2320 | 35 | 393 | 17 | 366 | 15 | 42 | 16 | 219 | 24 |
| 10–12 | 2021 | 30 | 688 | 29 | 673 | 28 | 70 | 26 | 233 | 26 |
| 13–16 | 1890 | 28 | 1112 | 47 | 1167 | 48 | 131 | 49 | 371 | 41 |
| ≥17 | 292 | 4 | 146 | 6 | 186 | 8 | 18 | 7 | 60 | 7 |
| Family income (10 thousand RMB/yr) | ||||||||||
| <3.0 | 687 | 10 | 130 | 5 | 105 | 4 | 20 | 7 | 58 | 6 |
| 3.0–9.9 | 2257 | 34 | 655 | 28 | 676 | 28 | 77 | 29 | 268 | 30 |
| 10.0–29.9 | 1472 | 22 | 730 | 31 | 745 | 31 | 80 | 30 | 250 | 28 |
| ≥30.0 | 2089 | 31 | 793 | 33 | 842 | 35 | 85 | 32 | 305 | 34 |
CS: caesarean section.
Compared with children delivered by vaginal birth, CS births due to maternal disorders had a higher prevalence of birthweight less than 3000 g, and gestational diabetes. In contrast, children delivered by CS for fetal complications were more likely to be macrosomia. Vaginal births were more likely to receive exclusive breastfeeding in the first 4 month after birth, and their parents’ educational levels and family income levels were lower than those delivered by CS. The prevalence of asthma and allergic rhinitis was 3.4% (428/12 639) and 15.3% (1941/12 639) in our study, respectively, and 1.7% (214/12 639) had both asthma and allergic rhinitis.
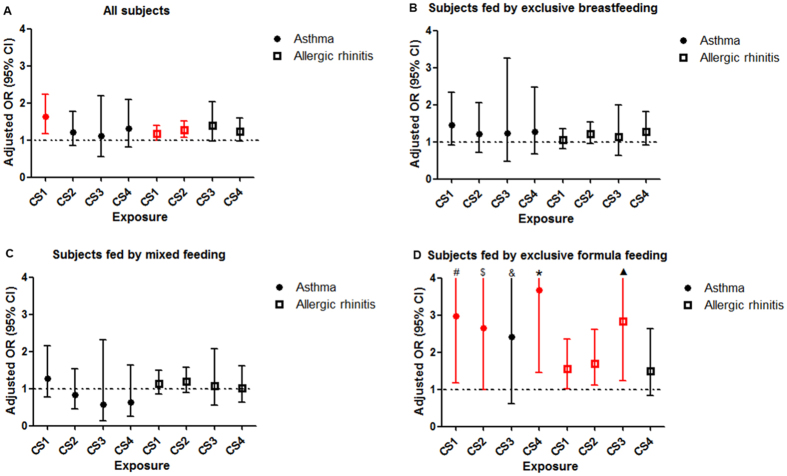
Figure 2 shows that CS without medical indication was associated with an increased risk of childhood asthma after adjusting for potential confounders (adjusted OR = 1.63 [95% CI 1.18–2.24]). CS without medical indication and CS for fetal complications were also associated with increased risks of childhood allergic rhinitis (adjusted OR = 1.18 [95% CI 1.00–1.40] and 1.27 [95% CI 1.08–1.51], respectively) (Fig. 2). These findings were consistent in children with both asthma and allergic rhinitis (Table 2).
Figure 2.
Adjusted and unadjusted relative risk of asthma and allergic rhinitis in children exposed to different modes of delivery. (A) All subjects. Asthma: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy; allergic rhinitis: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy. (B) Subjects fed by exclusive breastfeeding. Asthma: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy, gender; allergic rhinitis: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy. (C) Subjects fed by mixed feeding. Asthma: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy; allergic rhinitis: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy. (D) Subjects fed by exclusive formula feeding. Asthma: adjusted for maternal education level, paternal education level, family income, maternal history of diabetes in pregnancy, gender; allergic rhinitis: adjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy, birth weight, gender. CS1: CS without indications; CS2: CS for fetal complications; CS3: CS for maternal complications; CS4: CS for other reasons. #: upper limit was 7.50; $: upper limit was 6.98; &: upper limit was 9.52; *: upper limit was 9.33; ▲: upper limit was 6.55.
Table 2.
Adjusted and unadjusted relative risks of having history of both asthma and allergic rhinitis in children exposed to different modes of delivery.
| Exposure Categories | No. | Unadjusted OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|---|
| All subjects a | |||||
| Vaginal delivery | 6677 | Ref. | \ | Ref. | \ |
| CS without indications | 2369 | 2.14 | 1.35–3.41 | 1.64 | 1.01–2.68 |
| CS for fetal complications | 2424 | 1.96 | 1.23–3.12 | 1.50 | 0.93–2.43 |
| CS for maternal disorders | 267 | 3.37 | 1.53–7.44 | 2.06 | 0.90–4.71 |
| CS for other reasons | 902 | 2.01 | 1.08–3.72 | 1.71 | 0.92–3.17 |
| Subjects fed by exclusive breastfeeding b | |||||
| Vaginal delivery | 4492 | Ref. | \ | Ref. | \ |
| CS without indications | 1270 | 1.67 | 0.80–3.46 | 1.25 | 0.58–2.69 |
| CS for fetal complications | 1373 | 1.99 | 1.06–3.72 | 1.51 | 0.80–2.86 |
| CS for maternal disorders | 134 | 2.90 | 0.88–9.57 | 2.13 | 0.60–7.59 |
| CS for other reasons | 537 | 1.63 | 0.66–4.06 | 1.36 | 0.57–3.25 |
| Subjects fed by mixed feeding c | |||||
| Vaginal delivery | 1341 | Ref. | \ | Ref. | \ |
| CS without indications | 684 | 1.49 | 0.74–3.02 | 1.26 | 0.61–2.62 |
| CS for fetal complications | 715 | 1.20 | 0.56–2.56 | 0.97 | 0.44–2.16 |
| CS for maternal disorders | 80 | 1.73 | 0.46–6.55 | 1.24 | 0.27–5.81 |
| CS for other reasons | 224 | 1.15 | 0.39–3.41 | 0.98 | 0.31–3.09 |
| Subjects fed by exclusive formula feeding d | |||||
| Vaginal delivery | 775 | Ref. | \ | Ref. | \ |
| CS without indications | 399 | 11.91 | 3.96–35.83 | 10.49 | 2.63–41.93 |
| CS for fetal complications | 319 | 9.51 | 2.49–36.39 | 8.61 | 2.27–32.64 |
| CS for maternal disorders | 53 | 24.34 | 4.57–129.56 | 14.06 | 2.27–86.95 |
| CS for other reasons | 134 | 17.04 | 5.04–57.65 | 15.25 | 3.94–58.96 |
aAdjusted for maternal education level, paternal education level, family income, maternal history of diabetes in pregnancy.
bAdjusted for maternal education level, paternal education level, family income, maternal history of diabetes in pregnancy, birth weight.
cAdjusted for maternal education level, paternal education level, maternal history of diabetes in pregnancy.
dAdjusted for maternal education level, paternal education level, family income, maternal history of diabetes in pregnancy, birth weight, gender.
CS: caesarean section.
When subjects were stratified by feeding pattern within four months after birth, the risks of having childhood asthma, allergic rhinitis, or both were all substantially higher in children fed by exclusive formula feeding than those fed by exclusive breastfeeding. We examined potential interactions between CS and breastfeeding. No meaningful interactions were found (Tables S2 and S3).
Discussion
Our study shows that CS without medical indication is associated with increased risks of childhood asthma and allergic rhinitis. CS for fetal complications is also associated with an increased risk of allergic rhinitis in children. This result is consistent with previous studies in general3, 14, 15. Breastfeeding may attenuate these risks.
In a recent population-based data-linkage study of 321,287 term singleton first-born offspring in Scotland, United Kingdom, Black et al.14 found that in comparison with children born vaginally, offspring born by planned CS were at an increased risk of asthma requiring hospital admission (adjusted hazard ratio = 1.22 [95% CI, 1.11–1.34]) and salbutamol inhaler prescription at age 5 years (adjusted hazard ratio = 1.13 [95% CI, 1.01–1.26]). This finding is consistent with that of a meta-analysis, in which CS was associated with a 20% increase in the risk of asthma3.
It has been a concern in previous studies that the association between CS and asthma may be due to confounding by indication because the vast majority of CS in those studies were performed for clinical indications. Our studies are the first to specifically examine the association in CS without medical indication. The findings were consistent with previous investigations in general. Although the exact underlying biological mechanism is unclear, it has been hypothesized that fetuses delivered by CS are mainly exposed to microflora that is predominately on maternal skin after birth, but not in maternal vagina16. The microbial types and colonization in children delivered by CS may lead to an altered gut microbiota in early life, which may impair natural development of immune system and then promote the development of immune-mediated asthma and allergic disorders16. Preliminary evidence suggests that manually exposing newborns delivered by CS to maternal vaginal microbes may partially restore the microbiota of these infants17. The protective effect of exclusive breastfeeding on the risks of asthma and allergic rhinitis due to CS in our study, may confirm that microflora-related mechanism, considering that breastfeeding could prevent allergy through regulating infant gut barrier function and microbiota18.
Nonetheless, our studies cannot directly prove a causal relationship. Indeed, a sibling analysis using Swedish medical registry data failed to confirm the association between CS and childhood asthma19. On the other hand, if gut microflora dysbiosis is causally related to childhood asthma, it is reasonable to question whether the matched sibling design may mask the impact of mode of delivery because the microbial exposure continues after birth. A number of studies have shown that close contact with older siblings and pets may reduce the risk of asthma7–9. In Shanghai, China, due to the one-child-family policy, most of our study subjects were single child20, and few families have pets at home.
Several limitations of our studies are worth noting. First, information on CS and its indications were self-reported. A previous study demonstrated that the accuracy of maternal recall of CS 3 to 9 years ago was 100%, and maternal recall of severe obstetric complications was also rather reliable21. Moreover, the prevalence of CS in our study was 47%, which was consistent with the previous survey in Shanghai (48%)22. The rate of CS without medical indications (18%) in our study is also similar to that in a previous report where the rate of CS on maternal request was 20%11. Therefore, the self-reported CS and its indications may be reasonably accurate in our study.
Second, asthma and allergic rhinitis in the index children were also reported by the parents. Thus, inaccuracy in the outcome is possible. In our study, the prevalence of asthma was 3.4%, which is lower than 5.81–7.57% reported in previous studies from Shanghai23, 24. But the prevalence of allergic rhinitis in our study (15%) was consistent with a previous report (13%)25. Discrepancy in asthma prevalence may be partly due to the incompatibility of our study population and the previous ones. In our population-based study, we randomly selected subjects from all 17 districts and counties and included those from suburb and rural areas in Shanghai, whereas the previous studies only selected children from urban areas23, 24. Since asthma prevalence in children of rural area in Shanghai is lower than those in urban area (3.7% vs. 6.2%)26, the lower prevalence of childhood asthma in our study may be partially expected.
On the other hand, the underestimation of asthma prevalence can’t be completely ruled out, which may be due to underreporting by the parents. It is possible that some parents may not want the school know the child history as this survey was conducted through the school, even though we ensured the parents in the informed consent that the information they provided would be strictly confidential. And we were unable to verify the self-report. On the other hand, we purposefully placed the questions on CS history far apart from those on child disease history in the questionnaire. Thus, we speculate that the misclassification of the outcomes of interest was less likely to be differential. We further controlled for maternal and paternal education and family income in the analysis.
Third, the data on feeding in infancy was recalled by parents. In our study, the prevalence of exclusive breastfeeding was similar to that previously reported in Shanghai, around 50%27. Thus, this recall may not be seriously biased.
Finally, our study did not collect data on family history of allergic disorders. Previous study found that children with family history of allergy had a higher risk of asthma than those without family history28. Since family history of asthma isn’t related with CS, it may not confound the association between CS and the risks of childhood asthma and allergic rhinitis.
Conclusions
In conclusion, CS without medical indication is associated with an increased risk of both asthma and allergic rhinitis in children. Our study avoided the challenge of potential residual confounding by CS indications and protective effects by having older siblings and pets29–31. In many parts of China, both CS and childhood asthma and allergic disorders are common22, 32. CS may have contributed to the increased prevalence of childhood allergic disorders. Fortunately, breastfeeding may attenuate these risks. These findings may have important clinical and public health implications.
Electronic supplementary material
Acknowledgements
The work was supported by the National Natural Science Foundation of China (81422040, 81172685, 81273091, 81530086); MOE New Century Excellent Talents (China) (NCET-13-0362); Shanghai Science and Technology Commission (12411950405, 14441904004, 13QH1401800); Shanghai Health and Family Planning Commission (GWIV-26, GWIV-36, 15GWZK0401); Shanghai Municipal Education Commission (D1502); and the Ministry of Science and Technology (China) (2010CB535000).
Author Contributions
F.J., J.Z. and S.C. designed the study. Y.Z., Y.J., W.S. and Q.Z. coordinated the overall undertaking of the SCHEDULE study. J.Z. and S.C. developed the analysis plan; J.Z. supervised the analysis. S.C. and B.W. performed statistical analyses, and took responsibility for the integrity of the data and the accuracy of the data analysis. S.C. wrote the manuscript. All authors contributed to the revision and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-10206-3
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Fan Jiang, Email: fanjiang@shsmu.edu.cn.
Jun Zhang, Email: zhangjun@xinhuamed.com.cn.
References
- 1.Wong GW, Leung TF, Ko FW. Changing prevalence of allergic diseases in the Asia-pacific region. Allergy Asthma Immunol Res. 2013;5:251–257. doi: 10.4168/aair.2013.5.5.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disease: meta-analyses. Clin Exp Allergy. 2008;38:634–42. doi: 10.1111/j.1365-2222.2008.02939.x. [DOI] [PubMed] [Google Scholar]
- 3.Thavagnanam S, Fleming J, Bromley A, Shields MD, Cardwell CR. A meta-analysis of the association between Caesarean section and childhood asthma. Clin Exp Allergy. 2008;38:629–633. doi: 10.1111/j.1365-2222.2007.02780.x. [DOI] [PubMed] [Google Scholar]
- 4.Li Y, et al. Pre- and postnatal risk factors in relation to allergic rhinitis in school-aged children in China. PLoS One. 2015;10 doi: 10.1371/journal.pone.0114022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner SW, et al. Associations between fetal size, maternal {alpha}-tocopherol and childhood asthma. Thorax. 2010;65:391–397. doi: 10.1136/thx.2008.111385. [DOI] [PubMed] [Google Scholar]
- 6.Tedner SG, Örtqvist AK, Almqvist C. Fetal growth and risk of childhood asthma and allergic disease. Clin Exp Allergy. 2012;42:1430–1447. doi: 10.1111/j.1365-2222.2012.03997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ball TM, et al. Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. N Engl J Med. 2000;343:538–543. doi: 10.1056/NEJM200008243430803. [DOI] [PubMed] [Google Scholar]
- 8.Strachan DP, et al. Siblings, asthma, rhinoconjunctivitis and eczema: a worldwide perspective from the International Study of Asthma and Allergies in Childhood. Clin Exp Allergy. 2015;45:126–136. doi: 10.1111/cea.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collin SM, et al. Pet ownership is associated with increased risk of non-atopic asthma and reduced risk of atopy in childhood: findings from a UK birth cohort. Clin Exp Allergy. 2015;45:200–210. doi: 10.1111/cea.12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feng, X. L., Xu, L., Guo, Y. & Ronsmans, C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ90, 30–39, 39A (2012). [DOI] [PMC free article] [PubMed]
- 11.Zhang J, et al. Cesarean delivery on maternal request in southeast China. Obstet Gynecol. 2008;111:1077–1082. doi: 10.1097/AOG.0b013e31816e349e. [DOI] [PubMed] [Google Scholar]
- 12.Fuller, W. A. Sampling Statistics. Wiley series in survey methodology. John Wiley & Sons, Inc., New Jersey. 455–456 (2009).
- 13.Robins JM, Rotnitzky A, Zhao LP. Estimation of regression coefficients when some regressors are not always observed. J Am Stat Assoc. 1994;89:846–866. doi: 10.1080/01621459.1994.10476818. [DOI] [Google Scholar]
- 14.Black M, Bhattacharya S, Philip S, Norman JE, McLernon DJ. Planned cesarean delivery at term and adverse outcomes in childhood health. JAMA. 2015;314:2271–2279. doi: 10.1001/jama.2015.16176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung JY, Li AM, Leung GM, Schooling CM. Mode of delivery and childhood hospitalizations for asthma and other wheezing disorders. Clin Exp Allergy. 2015;45:1109–1117. doi: 10.1111/cea.12548. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan JL, Shi HN, Walker WA. The role of microbes in developmental immunologic programming. Pediatr Res. 2011;69:465–472. doi: 10.1203/PDR.0b013e318217638a. [DOI] [PubMed] [Google Scholar]
- 17.Dominguez-Bello MG, et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 2016;22:250–253. doi: 10.1038/nm.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munblit D, Verhasselt V. Allergy prevention by breastfeeding: possible mechanisms and evidence from human cohorts. Curr Opin Allergy Clin Immunol. 2016;16(5):427–433. doi: 10.1097/ACI.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 19.Almqvist C, Cnattingius S, Lichtenstein P, Lundholm C. The impact of birth mode of delivery on childhood asthma and allergic diseases–a sibling study. Clin Exp Allergy. 2012;42:1369–1376. doi: 10.1111/j.1365-2222.2012.04021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bao L. Ratio of only children and age model of childcare pattern. China Youth Study. 2007;4:42–47. [Google Scholar]
- 21.Sou SC, Chen WJ, Hsieh WS, Jeng SF. Severe obstetric complications and birth characteristics in preterm or term delivery were accurately recalled by mothers. J Clin Epidemiol. 2006;59:429–435. doi: 10.1016/j.jclinepi.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 22.Deng W, et al. Cesarean section in Shanghai: women’s or healthcare provider’s preferences? BMC Pregnancy Childbirth. 2014;14 doi: 10.1186/1471-2393-14-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Cooperative Group on Childhood Asthma; Institute of Environmental Health and Related Product Safety, Chinese Center for Disease Control and Prevention; Chinese Center for Disease Control and Prevention. Third nationwide survey of childhood asthma in urban areas of China. Zhonghua Er Ke Za Zhi51, 729–735 (2013).
- 24.Respiratory Disease Group, Pediatric Committee of Shanghai Medical Association. Epidemiological survey of asthma in children aged 0–14 years in seven districts of Shanghai. Zhonghua Er Ke Za Zhi52, 17–22 (2014). [PubMed]
- 25.Li F, et al. Prevalence and risk factors of childhood allergic diseases in eight metropolitan cities in China: a multicenter study. BMC Public Health. 2011;11 doi: 10.1186/1471-2458-11-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Niu C, Wu J, Zhuang Z, Lu G, Tang C. Prevalence of Respiratory Symptoms and Diseases Among Children and Adolescent in Urban Shanghai. Chinese Journal of School Health. 2010;31:708–710. [Google Scholar]
- 27.Ma JQ, et al. A summary index of infant and child feeding practices is associated with child growth in urban Shanghai. BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danansuriya MN, Rajapaksa LC, Weerasinghe A. Genetic, familial and environmental correlates of asthma among early adolescents in Sri Lanka: a case control study. World Allergy Organ J. 2015;8 doi: 10.1186/s40413-015-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang R. China’s Only Children: The Quantity, Structure and Risk. Journal of Nanjing College for Population Programme Management. 2009;25(1):5–10. [Google Scholar]
- 30.Nie Y, Wyman RJ. The One-Child Policy in Shanghai: Acceptance and Internalization. Population and Development Review. 2005;31(2):313–336. doi: 10.1111/j.1728-4457.2005.00067.x. [DOI] [Google Scholar]
- 31.Huang C, Hu Y, Liu W, Zou ZJ, Jan S. Pet-keeping and its impact on asthma and allergies among preschool children in Shanghai, China. Chinese Science Bulletin. 2013;34:4203–4210. doi: 10.1007/s11434-013-5679-4. [DOI] [Google Scholar]
- 32.National Cooperative Group on Childhood Asthma; Institute of Environmental Health and Related Product Safety, Chinese Center for Disease Control and Prevention; Chinese Center for Disease Control and Prevention. Third nationwide survey of childhood asthma in urban areas of China. Zhonghua Er Ke Za Zhi51, 729–735 (2013).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.