Abstract
Background:
The current overweight and obesity guidelines based on the Westerners are not consistent with many studies based on the Asians. The guidelines may be different because of regional diversity. This study aimed to determine the appropriate body mass index (BMI) and waist-hip ratio (WHR) cutoff points in the adults of Northeast China.
Methods:
Overall, 21206 adults were selected from Jilin Province Adult Chronic Disease and Risk Factor Survey conducted in 2012. A representative sample was collected in the Jilin Province of northeast China by a multistage stratified random cluster sampling design. The age of participants was from 20 to 79 yr old. The test items were clustered by risk factors, and receiver operating characteristic (ROC) curves were computed to analyze.
Results:
Under different risk factors, BMI cutoff points were affected greatly. Especially for diabetes, the cutoff value was apparently larger than others were. WHR increased with age in both genders. From a general view, male WHR was slightly larger than female. In the male, WHR cutoff point was near 0.88 with a tiny change, as for in the female was near 0.86.
Conclusion:
The cutoff values of sensitivity and specificity are relatively good and false positives rate is relatively low. BMI cutoffs values of overweight and obesity are 24.5 kg/m2 and 29.0 kg/m2, WHR cutoff values of the male are 0.88, the female is 0.86.
Keywords: Body mass index, Waist-hip ratio, Adult, Cutoff point, China
Introduction
Overweight and obesity, which broadly refer to access the acceptable or desirable weight, have become important public health problems. Overweight and obesity had close with diseases which involve hypertension (1), diabetes (2), hyperlipidemia (3) and so on (4, 5). Hence, preventing overweight and obesity has been the key point to control chronic diseases.
In order to predict risks of cardiovascular disease, Body Mass Index (BMI) and Waist-Hip Ratio (WHR) have been widely used to judge overweight and obesity (6–8). In epidemiology, BMI is used as the measurement of overall obesity, and WHR is the measurement of central obesity. Using the data of Westerners, WHO has classified BMI between 18.5–24.9 kg/m2 as normal weight, between 25.0–29.9 kg/m2 as overweight, and ≥30.0 kg/m2 as obese (9). In 2002, based on the data of each province of China, China Working Group on Obesity (WGOC) suggested classifying BMI between 24.0–28.0 kg/m2 as overweight, and ≥ 28.0 kg/m2 as obese in Chinese (10). However, because of the wide geographic span in China, there are significant differences in lifestyle, dietary habit, and hereditary factors etc. Compared with southerners, the northeasterners located in the North Temperate Zone, show obvious gaps in physical figure and function. Therefore, in authors’ opinion, BMI cutoff values that WGOC classified may not accurately describe the condition of northeasterners in China. At present, the specific measurement of WHR has not been given in China.
It is imperative to determine a more appropriate BMI or WHR range and the threshold of overweight and obesity for more effective prevention and control of complications of obesity in northeastern adults. In addition to determining the cutoff points, the study will analyze their associations with related disease risk factors for adults aged 20 to 79 yr in northeast China.
Methods
Ethics statement
This study was approved by the Ethics Committee of School of Public Health Jilin University and in accordance with the Helsinki Declaration. Anonymity and privacy of respondents were fully guaranteed. Participants had right to quit from the research at any time without any reason or explanation. The informed consent was obtained from each participant.
Study population
There are three provinces from north to south in northeast China. Jilin Province is located in the middle of northeast China and has a population of about 27 million people. Therefore, in consideration of representativeness, this study used data from Jilin Province Investigation Team on Adult Chronic Disease and Risk Factor. Jilin Province Adult Chronic Disease and Risk Factor Survey was conducted by the Department of health, Jilin Province and was led by a research team from the School of Public Health, Jilin University in Jun 2012. Totally, 22600 populations, which was usually adult residents from 32 survey spots covering 9 cities of Jilin Province, was investigated with multistage stratified random cluster sampling method. Of those, 21206 individuals aged 20 to 79 were selected in this study. The survey respondents were asked to answer each question face-to-face with investigators uniformly trained.
Anthropometric measurements and laboratory methods
BMI and WHR:
With a precision of 0.1kg and 0.1cm, weight, height, waist circumference (WC) and hip circumference (HC) were measured 2 times in light indoor clothing and without shoes. At the level of the abdomen just above the hip-bone, the WC measurement was taken immediately after exhalation. The HC measurement was at the level of the symphysis pubis and the place most protruding of the hip. The average of two measurements was used for analysis. BMI is calculated as weight in kilogram divided by height in m2 and WHR is the WC divided by the HC.
Blood pressure:
At the sitting position, blood pressure was measured 2 times on the left arm. The first measurement was made after at least 5 min rest and the second measurement was taken after 2 min’ interval (11).
Blood lipids:
Blood samples were drawn from the antecubital vein into vacuum tubes containing EDTA in the morning after an overnight fasting period. All the collected samples were transported on dry ice at prearranged intervals to KingMedDiagnostics, a commercial clinical laboratory in China. The blood lipid was measured by Roche MODULE P800 Automatic Biochemical Analyzer (Roche Holding AG, America).
Blood glucose:
Using a drop of blood from participants’ finger, blood glucose was measured by Bayer Contour TS Blood Glucose Meter (Bayer, Germany).
Definition of risk factors
Hypertension:
Hypertension was defined as systolic blood pressure (SBP), calculated from the mean of the two readings, ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg (11). Participants who were currently on anti-hypertensive medication or diagnosed by the hospital above the county level were also classified as hypertensive cases.
Hyperlipidemia:
Hyperlipidaemia was defined as total cholesterol (TC) concentration ≥ 5.18 mmol/L, triglyceride (TG) concentration ≥ 1.70 mmol/L, LDL cholesterol (LDL-C) concentration ≥3.37 mmol/L or HDL cholesterol (HDLC) concentration ≤1.04 mmol/L (12). Participants who were currently on anti-hyperlipidemia medication or diagnosed by the hospital above the county level were also classified as hyperlipidemia cases.
Diabetes:
According to the criteria for the diagnosis of diabetes mellitus reported by the expert committee of ADA and a WHO working group, diabetes was defined as fasting plasma glucose ≥7.0 mmol/L, postprandial blood glucose ≥11.1 mmol/L, using of insulin or oral hypoglycemic agents, or a self-reported history of diabetes. Participants diagnosed by the hospital above the county level were also classified as diabetes cases (13, 14).
Clustering of risk factors:
Two or more risk factors were included.
Statistical analysis
All records were entered into EpiData version 3.1 and analyzed using SPSS version 18.0 (Chicago, IL, USA) for Windows at two-sided 5% significance level. Continuous variables were expressed as means and standard deviations, and discrete variables were expressed as quantities and proportions. Data were classified by gender and age standardized using the 2010 Jilin provincial population as the standard population. It was stratified to 12 subgroups at 20-, 30-, 40-, 50-, 60-, 70–79 yr. The Receiver Operating Characteristic (ROC) curves of BMI and WHR were drawn and the areas under the curve (AUC), 95% Confidence Interval (95%CI), sensitivity (Sens), specificity (Spec), positive likelihood ratio (PLR) and negative likelihood ratio (NLR) were tabulated to judge cutoff points. The cutoff points of WHR and overweight points of BMI were judged according to Max Youden Index (YI, equal to Sens+Spec−1) and obesity points of BMI were the point that Spec ≥ 90% (10, 15). Additionally, the cutoff value of subgroups of BMI and WHR were also calculated to observe trends.
Results
Anthropometric measurement data and risk factors prevalence of the study subjects is shown in Table 1. Overall, 21206 adults participated in the study, of whom 48.07% (10193) were female, with a mean age of 48.14± (13.65) yr. In the study, females are older than males (48.14± (13.65) vs 46.55± (12.61) yr old; P<0.001).
Table 1:
Anthropometric measurement data and risk factors prevalence
| Age (yr) | Sample (n) | BMI (mean ± sd) | WHR (mean ± sd) | Hypertension n(%) | Hyperlipidaemia n(%) | Diabetes n(%) | Clustering of risk factors | |
|---|---|---|---|---|---|---|---|---|
| Male | 20∼ | 1371 | 23.6±4.4 | 0.84±0.06 | 165(12.0) | 444(32.4) | 13(0.9) | 92(6.7) |
| 30∼ | 1822 | 24.7±4.0 | 0.88±0.06 | 406(22.3) | 915(50.2) | 66(3.6) | 311(17.1) | |
| 40∼ | 2697 | 24.8±3.6 | 0.89±0.06 | 1039(38.5) | 1514(56.1) | 246(9.1) | 830(30.8) | |
| 50∼ | 2386 | 24.4±3.3 | 0.90±0.06 | 1167(48.9) | 1389(58.2) | 332(13.9) | 911(38.2) | |
| 60∼ | 1421 | 24.0±3.4 | 0.90±0.06 | 795(55.9) | 809(56.9) | 232(16.3) | 600(42.2) | |
| 70∼79 | 496 | 23.6±3.5 | 0.91±0.07 | 311(62.7) | 276(55.6) | 83(16.7) | 218(44.0) | |
| Total | 10193 | 24.4±3.7 | 0.89±0.07 | 3883(38.1) | 5347(52.5) | 972(9.5) | 2962(29.1) | |
| Female | 20∼ | 915 | 21.8±3.6 | 0.79±0.06 | 34(3.7) | 160(17.5) | 8(0.9) | 19(2.1) |
| 30∼ | 1792 | 23.2±3.7 | 0.81±0.06 | 158(8.8) | 504(28.1) | 39(2.2) | 92(5.1) | |
| 40∼ | 3395 | 24.3±3.6 | 0.84±0.07 | 874(25.7) | 1509(44.4) | 172(5.1) | 585(17.2) | |
| 50∼ | 2713 | 24.8±3.6 | 0.87±0.06 | 1190(43.9) | 1827(67.3) | 350(12.9) | 1013(37.3) | |
| 60∼ | 1696 | 24.9±3.7 | 0.89±0.07 | 1014(59.8) | 1196(70.5) | 321(18.9) | 864(50.9) | |
| 70∼79 | 502 | 25.1±2.8 | 0.92±0.06 | 344(68.5) | 366(72.9) | 94(18.7) | 290(57.8) | |
| Total | 11013 | 24.1±3.7 | 0.85±0.07 | 3614(32.8) | 5562(50.5) | 984(8.9) | 2863(26.0) |
For both female and male, the prevalence of hypertension obviously raised with the increase of age. Under sixty, male patients were more than female patients were, and over sixty is opposite. Likewise, the prevalence of hyperlipidemias and diabetes is higher with higher age, which rises quickly and then levels off.
Body Mass Index
In male adults, mean of BMI began to rise and it was a peak in the group 40-year-old, and then declines from the peaks. In the female, BMI rises continuously with age, meanwhile, after 40 yr old, BMI is larger than male (Table 1).
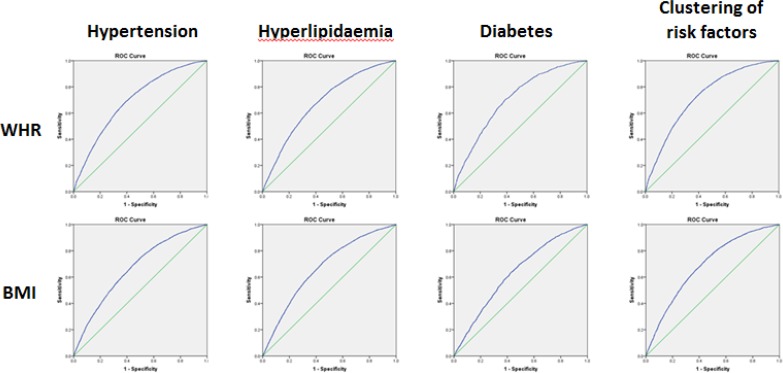
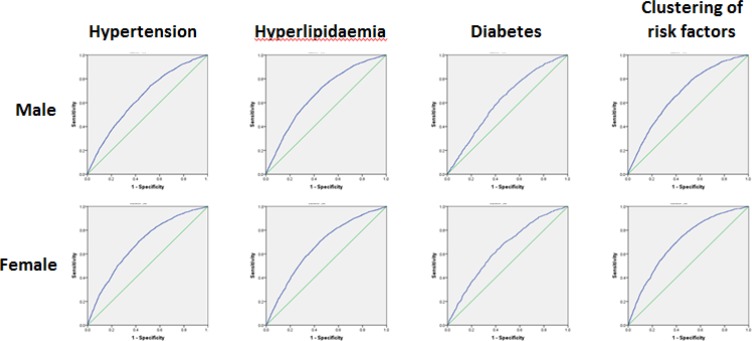
The result of ROC curves for BMI cutoffs across all the samples was presented in Table 2 and Fig. 1. Cutoff points whose YI are largest are chosen. Under the different risk factors, BMI was affected greatly. Especially for diabetes, the cutoff point was apparently larger than others were. Categorized by age and gender, a series of ROC curves were obtained (Table 3 and Fig. 2).
Table 2:
The result of ROC curves for BMI and WHR cutoffs across all the samples
| AUC(95%CI) | P value | Sens | Spec | PLR | NLR | Cutoff | ||
|---|---|---|---|---|---|---|---|---|
| WHR | Hypertension | 0.668 (0.657–0.678) | <0.001 | 0.688 | 0.568 | 1.59 | 0.55 | 0.88 |
| Hyperlipidaemia | 0.674 (0.664–0.685) | <0.001 | 0.686 | 0.575 | 1.61 | 0.55 | 0.88 | |
| Diabetes | 0.679 (0.662–0.697) | <0.001 | 0.722 | 0.567 | 1.67 | 0.49 | 0.89 | |
| Clustering of riskfactors | 0.726 (0.718–0.733) | <0.001 | 0.767 | 0.576 | 1.81 | 0.41 | 0.86 | |
| BMI | Hypertension | 0.647 (0.636–0.658) | <0.001 | 0.735 | 0.484 | 1.42 | 0.55 | 23.2 |
| Hyperlipidaemia | 0.674 (0.663–0.684) | <0.001 | 0.723 | 0.541 | 1.58 | 0.51 | 23.2 | |
| Diabetes | 0.618 (0.601–0.636) | <0.001 | 0.629 | 0.563 | 1.44 | 0.66 | 24.6 | |
| Clustering of risk factors | 0.689 (0.682–0.697) | <0.001 | 0.741 | 0.543 | 1.62 | 0.48 | 23.7 |
Sens: sensitivity; Spec: specificity; PLR: positive likelihood ratio; NLR: negative likelihood ratio.
Fig. 1:
ROC curves for BMI and WHR across all the samples
Table 3:
The result of ROC curves for BMI cutoffs across the subgroups of samples
| Age | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AUC(95%CI) | P-value | Overweight | Obesity | AUC(95%CI) | P-value | Overweight | Obesity | ||
| Hypertension | 20∼ | 0.691 (0.668–0.715) | <0.001 | 24.1 | 28.8 | 0.724 (0.685–0.763) | <0.001 | 24.5 | 27.3 |
| 40∼ | 0.655 (0.640–0.671) | <0.001 | 23.8 | 27.9 | 0.673 (0.659–0.688) | <0.001 | 23.8 | 28.0 | |
| 60∼79 | 0.643 (0.618–0.669) | <0.001 | 22.1 | 27.1 | 0.620 (0.595–0.644) | <0.001 | 23.6 | 28.3 | |
| Total | 0.647 (0.636–0.658) | <0.001 | 23.2 | 28.2 | 0.686 (0.676–0.697) | <0.001 | 23.7 | 27.8 | |
| Hyperlipidaemia | 20∼ | 0.699 (0.680–0.718) | <0.001 | 23.1 | 28.2 | 0.682 (0.658–0.705) | <0.001 | 22.8 | 26.8 |
| 40∼ | 0.665 (0.649–0.680) | <0.001 | 23.8 | 27.9 | 0.640 (0.626–0.654) | <0.001 | 24.3 | 28.0 | |
| 60∼79 | 0.648 (0.623–0.673) | <0.001 | 22.8 | 27.2 | 0.597 (0.570–0.624) | <0.001 | 22.6 | 28.7 | |
| Total | 0.674 (0.663–0.684) | <0.001 | 23.2 | 27.9 | 0.667 (0.656–0.667) | <0.001 | 23.2 | 27.7 | |
| Diabetes | 20∼ | 0.652 (0.598–0.706) | <0.001 | 22.7 | 29.5 | 0.679 (0.596–0.761) | <0.001 | 25.0 | 27.6 |
| 40∼ | 0.627 (0.603–0.651) | <0.001 | 24.6 | 28.8 | 0.627 (0.602–0.652) | <0.001 | 25.1 | 28.9 | |
| 60∼79 | 0.609 (0.576–0.642) | <0.001 | 23.7 | 28.2 | 0.585 (0.556–0.615) | <0.001 | 24.9 | 29.1 | |
| Total | 0.618 (0.601–0.636) | <0.001 | 24.6 | 28.9 | 0.645 (0.627–0.662) | <0.001 | 24.5 | 28.7 | |
| Clustering of Risk factors | 20∼ | 0.719 (0.694–0.744) | <0.001 | 24.5 | 29.1 | 0.756 (0.708–0.805) | <0.001 | 24.6 | 27.4 |
| 40∼ | 0.682 (0.667–0.698) | <0.001 | 25.0 | 28.0 | 0.693 (0.679–0.708) | <0.001 | 25.0 | 28.2 | |
| 60∼79 | 0.679 (0.655–0.703) | <0.001 | 23.2 | 27.2 | 0.633 (0.609–0.656) | <0.001 | 23.6 | 28.5 | |
| Total | 0.677 (0.666–0.688) | <0.001 | 23.2 | 28.3 | 0.700 (0.689–0.711) | <0.001 | 23.7 | 28.0 | |
Fig. 2:
ROC curves for BMI across the subgroups of samples
Points of largest YI were chosen as the overweight points and the points of Spec ≥ 90% were chosen as the obesity points. In consideration of reliability of data and being easy to memorize, authors suggest determining 24.5 as the overweight cutoff points and 29.0 as the obesity points.
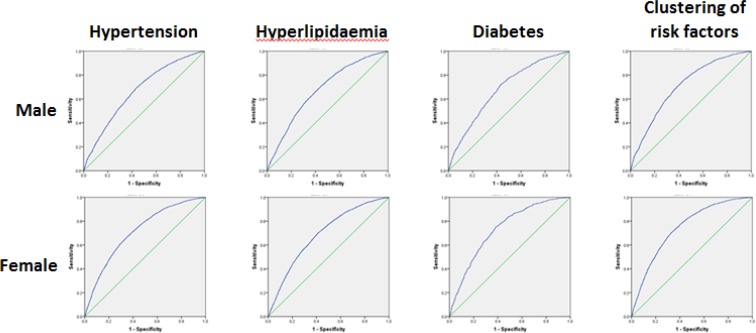
Waist-to-hip ratio
WHR increased with age in both genders. From a general view, male WHR was slightly larger than female (Table 1). The WHR cutoff points with largest YI were chosen (Table 2 and 4, Fig. 1 and 3). In the male, WHR was near 0.88 with tiny changing, as for female near 0.86. Therefore, authors suggested 0.88 and 0.86 as the WHR cutoff values of male and female respectively (Table 5).
Table 4:
The result of ROC curves for WHR cutoffs across the subgroups of samples
| Age (yr) | Male | Female | |||||
|---|---|---|---|---|---|---|---|
| AUC(95%CI) | P-value | Cutoff point | AUC(95%CI) | P-value | Cutoff point | ||
| Hypertension | 20∼ | 0.667 (0.642–0.691) | <0.001 | 0.88 | 0.708 (0.670–0.747) | <0.001 | 0.82 |
| 40∼ | 0.639 (0.623–0.655) | <0.001 | 0.88 | 0.656 (0.641–0.670) | <0.001 | 0.87 | |
| 60∼79 | 0.668 (0.657–0.678) | <0.001 | 0.88 | 0.714 (0.704–0.724) | <0.001 | 0.85 | |
| Total | 0.706 (0.649–0.763) | <0.001 | 0.88 | 0.686 (0.676–0.697) | <0.001 | 0.87 | |
| Hyperlipidaemia | 20∼ | 0.694 (0.675–0.714) | <0.001 | 0.85 | 0.656 (0.633–0.680) | <0.001 | 0.80 |
| 40∼ | 0.664 (0.648–0.680) | <0.001 | 0.87 | 0.646 (0.632–0.660) | <0.001 | 0.84 | |
| 60∼79 | 0.634 (0.608–0.660) | <0.001 | 0.91 | 0.590 (0.563–0.617) | <0.001 | 0.87 | |
| Total | 0.674 (0.664–0.685) | <0.001 | 0.88 | 0.690 (0.680–0.699) | <0.001 | 0.84 | |
| Diabetes | 20∼ | 0.652 (0.598–0.708) | <0.001 | 0.88 | 0.731 (0.655–0.809) | <0.001 | 0.84 |
| 40∼ | 0.660 (0.636–0.683) | <0.001 | 0.89 | 0.708 (0.685–0.730) | <0.001 | 0.86 | |
| 60∼79 | 0.621 (0.587–0.654) | <0.001 | 0.89 | 0.604 (0.575–0.633) | <0.001 | 0.88 | |
| Total | 0.679 (0.662–0.697) | <0.001 | 0.89 | 0.733 (0.717–0.748) | <0.001 | 0.86 | |
| Clustering of Risk factors | 20∼ | 0.712 (0.685–0.738) | <0.001 | 0.88 | 0.767 (0.727–0.807) | <0.001 | 0.83 |
| 40∼ | 0.686 (0.671–0.702) | <0.001 | 0.89 | 0.702 (0.688–0.716) | <0.001 | 0.86 | |
| 60∼79 | 0.675 (0.650–0.699) | <0.001 | 0.90 | 0.618 (0.594–0.641) | <0.001 | 0.88 | |
| Total | 0.708 (0.697–0.719) | <0.001 | 0.88 | 0.744 (0.734–0.754) | <0.001 | 0.86 | |
Fig. 3:
ROC curves for WHR across the subgroups of samples
Table 5:
The suggestion of appropriate BMI and WHR cutoffs in Northeast China
| BMI | WHR | ||
|---|---|---|---|
| Overweight | Obesity | Male | Female |
| 24.5kg/m2 | 29.0kg/m2 | 0.88 | 0.86 |
Discussion
To our knowledge, this was the first study to examine the appropriate BMI and WHR cutoff for overweight and obesity among adults in northeast China. However, in other areas, there have been many studies about the predictive value of BMI and WHR to multiple risk factors (16–21). There are different optimal BMI or WHR cutoffs in different populations. The relationship of BMI or WHR with risk factors is approximately continuous linearity without significantly fold point or threshold, so it is hard to avoid quite a part of overlap between population at high risk and the healthy. Thus, all the cutoffs are artificial and relative but scientific.
The objective of the study is to provide a theoretical basis for designing preventive measures and treatments of overweight and obesity. For above purpose, the principle of choosing cutoff values is that the cutoffs not only can serve, as a reliable index to prevent the increase of most chronic disease early, but also will not give public too much mental pressure, and reduce the burden of preventions and treatments. Therefore, authors chose the points of which Sens and Spec are relatively well and false positive rate is relatively low. Comparing the analysis results with the standard WGOC classified in 2002 (BMI between 24.0–28.0 kg/m2 as overweight, and ≥28.0 kg/m2 as obesity), both the overweight and obesity cutoffs are higher than the average level in China. In theory, the northeastern population is stronger and has a lower risk for chronic diseases such as hypertension than the southern population with the same BMI. However, prevalence rate of hypertension (35.4% VS 26.6 % (22)) is significantly higher than the average level in China and the situation of diabetes (9.68% VS 11.6% (23)) is optimistic. The authors consider the phenomenon may be related to the cold environment, dietary habit, aware of hypertension prevention and hereditary factors. Among them, inheritance may play a key role, reported in domestic and overseas literature (24–27).
Analyzing the data of ROC curves, the cutoffs of Hypertension and clustering of risk factors continuously decline with age. Therefore, the elderly should attach great importance to keep normal weight. As for diabetes and hyperlipidemia, they should be paid attention to as a youth. Although there are some differences on the numerical between male and female subgroups, trends with the age are identical.
Because of the relatively low Sens and Spec in this study, the results have a few limitations. Cutoffs should be used as screening criteria among northeastern Chinese, and diseases diagnosis would still need a further examination.
Conclusion
The suggestion of appropriate BMI cutoffs measuring overall obesity and waist-hip ratio cutoffs measuring central obesity in Northeast China are listed in Table 5. Our findings would be useful for policy makers for the development of strategies to prevent chronic diseases that are gradually increasing in China.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
The authors would like to thank all participants from the Jilin Province of China and the interviewers from Jilin University and Department of Health, Jilin Province and School of Public Health Jilin University for providing the data source used in this study.
This work was supported by the Young Scholars Program of Norman Bethune Health Science Center of Jilin University (No. 2013202018), the Youth Scientific Research Foundation of the Health Bureau of Jilin Province, China (Grant Number: 2014Q027), and Norman Bethune Program of Jilin university (2015227).
Footnotes
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1. Rahmouni K. (2014). Obesity-associated hyper-tension: recent progress in deciphering the pathogenesis. Hypertension, 64:215–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Riobó Serván P. (2013). Obesity and diabetes. Nutr Hosp, 28 Suppl 5:138–43. [DOI] [PubMed] [Google Scholar]
- 3. Cybulska B, Klosiewicz-Latoszek L. (2013). Management of severe hypertriglyceridaemia. Kardiol Pol, 71:1007–12. [DOI] [PubMed] [Google Scholar]
- 4. Segula D. (2014). Complications of obesity in adults: a short review of the literature. Malawi Med J, 26:20–4. [PMC free article] [PubMed] [Google Scholar]
- 5. Kim HG, Han J. (2012). Obesity and Pancreatic Diseases. Korean J of Gastroenterol, 59:35–9. [DOI] [PubMed] [Google Scholar]
- 6. Adair LS, Gordon-Larsen P, Du SF, et al. (2014). The emergence of cardiometabolic disease risk in Chinese children and adults: consequences of changes in diet, physical activity and obesity. Obes Rev, 15 Suppl 1:49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Friedemann C, Heneghan C, Mahtani K, et al. (2012). Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ, 345:e4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coutinho T, Goel K, Correa de Sa D, et al. (2011). Central obesity and survival in subjects with coronary artery disease: a systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol, 57:1877–86. [DOI] [PubMed] [Google Scholar]
- 9. Consultation WHO (2000). Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser, 894:i–xii. [PubMed] [Google Scholar]
- 10. Zhou B. (2002). Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Zhonghua Liu Xing Bing Xue Za Zhi, 23:5–10 (in Chinese). [PubMed] [Google Scholar]
- 11. Liu LS. (2011). 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi, 39:579–615 (in Chinese). [PubMed] [Google Scholar]
- 12. Zhang C, Yu L, Xu T, et al. (2013). Association of Dyslipidemia with Renal Cell Carcinoma: A 1: 2 Matched Case-Control Study. PloS One, 8:e59796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Consultation WHO (1985). Diabetes mellitus. Report of a WHO Study Group. World Health Organ Tech Rep Ser, 727:1–113. [PubMed] [Google Scholar]
- 14. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003). Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care, 26 Suppl 1:S5–20. [DOI] [PubMed] [Google Scholar]
- 15. Akobeng AK. (2007). Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr, 96:644–7. [DOI] [PubMed] [Google Scholar]
- 16. Pan S, Yu ZX, Ma YT, et al. (2013). Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Uighur adults in Xinjiang. PLoS One, 8:e80185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. An Y, Yi S, Fitzpatrick A, et al. (2013). Appropriate body mass index and waist circumference cutoff for overweight and central obesity among adults in Cambodia. PLoS One, 8:e77897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Padua Cintra I, Zanetti Passos MA, Dos Santos LC, et al. (2014). Waist-to-height ratio percentiles and cutoffs for obesity: a cross-sectional study in brazilian adolescents. J Health Popul Nutr, 32:411–9. [PMC free article] [PubMed] [Google Scholar]
- 19. Araneta MR, Kanaya AM, Hsu WC, et al. (2015). Optimum BMI Cut Points to Screen Asian Americans for Type 2 Diabetes. Diabetes Care, 38:814–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lucha-López MO, Lucha-López AC, Vidal-Peracho C, et al. (2014). Analysis of a sample of type 2 diabetic patients with obesity or overweight and at cardiovascular risk: a cross sectional study in Spain. BMC Res Notes, 7:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu Y, Tong G, Tong W, Lu L, Qin X. (2011). Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health, 11:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gao Y, Chen G, Tian HM, et al. (2013). Prevalence of hypertension in china: a cross-sectional study. PLoS One, 8:e65938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Xu Y, Wang LM, He J, et al. (2013). Prevalence and control of diabetes in Chinese adults. JAMA, 310:948–59. [DOI] [PubMed] [Google Scholar]
- 24. Zhang C, Wang LY, Liao Q, et al. (2013). Genetic associations with hypertension: meta-analyses of six candidate genetic variants. Genet Test Mol Biomarkers, 17:736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang Y, Zhang Y, Zhang J, et al. (2013). Association of a functional single-nucleotide polymorphism in the ALDH2 gene with essential hypertension depends on drinking behavior in a Chinese Han population. J Hum Hypertens, 27:181–6. [DOI] [PubMed] [Google Scholar]
- 26. Liang M, Cowley AW, Jr, Mattson DL, et al. (2013). Epigenomics of hypertension. Semin Nephrol, 33:392–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vaněčková I, Maletínská L, Behuliak M, et al. (2014). Obesity-related hypertension: possible pathophysiological mechanisms. J Endocrinol,223:R63–78. [DOI] [PubMed] [Google Scholar]