Abstract
Background
Several studies have examined how the implementation of behavior change techniques (BCTs) varies between different activity trackers. However, activity trackers frequently allow tracking of activity, sleep, and sedentary behaviors; yet, it is unknown how the implementation of BCTs differs between these behaviors.
Objective
The aim of this study was to assess the number and type of BCTs that are implemented by wearable activity trackers (self-monitoring systems) in relation to activity, sleep, and sedentary behaviors and to determine whether the number and type of BCTs differ between behaviors.
Methods
Three self-monitoring systems (Fitbit [Charge HR], Garmin [Vivosmart], and Jawbone [UP3]) were each used for a 1-week period in August 2015. Each self-monitoring system was used by two of the authors (MJD and BM) concurrently. The Coventry, Aberdeen, and London-Refined (CALO-RE) taxonomy was used to assess the implementation of 40 BCTs in relation to activity, sleep, and sedentary behaviors. Discrepancies in ratings were resolved by discussion, and interrater agreement in the number of BCTs implemented was assessed using kappa statistics.
Results
Interrater agreement ranged from 0.64 to 1.00. From a possible range of 40 BCTs, the number of BCTs present for activity ranged from 19 (Garmin) to 33 (Jawbone), from 4 (Garmin) to 29 (Jawbone) for sleep, and 0 (Fitbit) to 10 (Garmin) for sedentary behavior. The average number of BCTs implemented was greatest for activity (n=26) and smaller for sleep (n=14) and sedentary behavior (n=6).
Conclusions
The number and type of BCTs implemented varied between each of the systems and between activity, sleep, and sedentary behaviors. This provides an indication of the potential of these systems to change these behaviors, but the long-term effectiveness of these systems to change activity, sleep, and sedentary behaviors remains unknown.
Keywords: health behavior; public health; exercise; sleep; behavior change; fitness trackers; adult, mobile applications
Introduction
Higher levels of moderate-to-vigorous intensity activity, lower levels of sedentary behavior, and sufficient sleep on a daily basis are key components of maintaining a healthy lifestyle that is associated with improved quality of life, reduced risk of cardiovascular disease, and diabetes [1-3]. Yet, many adults are not sufficiently active for health benefits, spend considerable amounts of time in sedentary activities, and do not obtain sleep that is of a sufficient duration or quality [4-7]. There are numerous published intervention studies that aim to improve physical activity, sedentary, and sleep behaviors [8-11], and although many are effective, few are disseminated to the broader public [12].
Burgeoning technological innovations mean that mobile devices (smartphone or tablets) and wearable technology such as wrist worn activity trackers, now have increasingly sophisticated capabilities to capture, analyze, and provide feedback to users on their daily physical activity, sleep, and sedentary behaviors. Public interest in this technology is substantial, and adoption of this technology exceeds that of many interventions. Mobile device ownership is increasing, with nearly 80% of people owning a smartphone and 47% owning a tablet [13] and 10% of US adults owning an activity tracker [14]. Studies that critique the potential effectiveness of apps and websites to change behavior conclude that the majority of apps and websites do not contain features or functionality, which are thought to be effective in changing behaviors [15-18]. These critiques have been guided by the availability of behavior change techniques (BCTs) that are potentially effective in changing health behaviors such as goal-setting and self-monitoring [18-21].
The combination of apps, websites, and wearable trackers which synchronize data between them provides a “self-monitoring system,” allowing users to self-monitor their physical activity, sleep, and sedentary behaviors. Despite existing self-monitoring systems providing information on all three behaviors, previous reviews of self-monitoring systems have focused on a single behavior, in most cases physical activity [15,16,18,21-23]. As a result, it is unknown if the approaches implemented by self-monitoring systems to change behavior differ between physical activity, sleep, and sedentary behaviors. In addition, although there is emerging evidence regarding the potential of BCTs to promote behavior change, there is also debate concerning how the number of BCTs and the cooccurrence of BCTs can influence behavior change [20,24-27]. Therefore, examining differences in the number or type of BCTs included in self-monitoring systems for physical activity, sleep, and sedentary behaviors is a first step toward describing the differences in the potential effectiveness of the systems to change these behaviors. Therefore, the purpose of this study was to examine how the number and type of BCTs implemented in self-monitoring systems targeting activity, sleep, and sedentary behaviors differs for each behavior.
Methods
Self-Monitoring System Inclusion Criteria and Descriptions
Self-monitoring systems included in this review were the Fitbit Charge HR, Garmin Vivosmart2, and Jawbone UP3 and their respective mobile phone apps and websites. The Fitbit and Jawbone systems were selected for inclusion based on a 2014 review, which indicated that these systems included the highest number of BCTs in relation to physical activity of the 13 systems evaluated [18]. The Garmin system was not included in the prior review but was included in this review as the system includes a “vibration alert.” This feature is also included in the Jawbone and can be used to alert wearers to the fact that they have not taken any steps in the previous hour, which may be useful in assisting wearers to reduce their sedentary behavior. Inclusion criteria were that the self-monitoring systems include a wearable activity tracker that measured physical activity levels, sedentary behavior, and sleep; and an app and/or website that provided the user with information on their behaviors. The activity tracker in all three systems was worn on the wrist. This represents a comprehensive monitoring system. The Jawbone system included an activity tracker and app only and did not include a website that provided feedback to users on their behaviors, whereas the Fitbit and Garmin systems included all three components. This study did not require ethics committee approval, and no informed consent was required as it did not involve participants.
Coding and Data Extraction
Two trackers for each system were available, so two authors (MJD and BM) could concurrently use each system for a 1-week period. This included wearing the activity tracker and using the app and website (if available). Each author wore the same model of activity tracker, used the same version—the most recent version available at the time of wearing—of the app software on an Apple-based device (mobile phone and tablet), over the same 1-week period. Each activity tracker was worn during all daytime and sleep periods, except for when engaged in water-based activities, if the units were not water proof. At the end of each wear period, the features and content of the systems were independently coded using the Coventry, Aberdeen, and London-Refined (CALO-RE) taxonomy that contains a list of 40 BCTs [19]. The presence or absence of each BCT was coded specifically for the behavior of interest. For coding purposes, physical activity was defined as steps and/or moderate-to-vigorous intensity physical activity; sleep was defined as sleep quality, sleep duration, and/or sleep timing; and sedentary behavior was defined as sitting or standing stationary. This definition of sedentary behavior differs to other definitions which would not classify standing stationary as sedentary [28]; however, this operational definition was necessary as previous experience using the systems showed that standing stationary is classified as sedentary by the systems. For instance, to be coded as allowing users to set goals for sedentary behavior, the system had to allow the user to specifically set goals for that behavior (eg, maximum amount of sedentary behavior performed each day or hour). Agreement between coders on the number of BCTs present for each behavior within each system was calculated using Kappa statistics, and the magnitude of agreement was interpreted using the following criteria: 0.00=poor, 0.01-0.20=slight, 0.21-0.40=fair, 0.41-0.60=moderate, 0.61-0.80=substantial, and 0.81-1.00=almost perfect [29]. The coders then met to discuss any discrepancies in coding, and all discrepancies were resolved to produce a coding summary that is presented in Tables 1 and 2. All use of the systems and coding was conducted in August 2015.
Table 1.
Summary of the number of behavior change techniques (BCTs) implemented in relation to physical activity, sleep, and sedentary behaviors.
| System and behavior | CALO-REa | |||
| Rater 1 No. BCTb | Rater 2 No. BCT | Kappa | Summary No. BCT | |
| Fitbit Charge HRc | ||||
| Activity | 23 | 27 | 0.68 | 25 |
| Sleep | 10 | 12 | 0.75 | 10 |
| Sedentary | 0 | 0 | 1.00 | 0 |
| Garmin Vivosmart2d | ||||
| Activity | 18 | 19 | 0.95 | 19 |
| Sleep | 2 | 4 | 0.64 | 4 |
| Sedentary | 10 | 10 | 1.00 | 10 |
| Jawbone Up3e | ||||
| Activity | 33 | 33 | 1.00 | 33 |
| Sleep | 29 | 28 | 0.82 | 29 |
| Sedentary | 7 | 7 | 1.00 | 7 |
aCALO-RE: Coventry, Aberdeen, and London-Refined.
bBCT: behavior change technique.
cFitbit app version 84.
dGarmin app version 2.13.1.
eJawbone Up3 app version 4.7.0.121.
Table 2.
Presence of specific behavior change techniques (BCTs) in relation to activity, sleep, and sedentary behavior.
|
Behavior change technique |
Fitbit Charge HR | Garmin Vivosmart | Jawbone UP3 | Total | ||||||||
| Activity | Sleep | Sedentry | Activity | Sleep | Sedentry | Activity | Sleep | Sedentry | Activity | Sleep | Sedentry | |
| Provide information on consequences of behavior in general | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| Provide information on consequences of behavior to the individual | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| Provide information about others’ approval | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | 1 | 0 |
| Provide normative information about others’ behavior | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | 1 | 0 |
| Goal-setting (behavior) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 3 | 2 | 1 |
| Goal-setting (outcome) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 3 | 2 | 1 |
| Action Planning | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 |
| Barrier identification or problem solving | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| Set graded tasks | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 |
| Prompt review of behavioral goals | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 2 | 1 |
| Prompt review of outcome goals | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 2 | 1 |
| Prompt rewards contingent on effort or progress toward behavior | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 1 | 1 |
| Provide rewards contingent on successful behavior | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 2 | 1 |
| Shaping | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 |
| Prompting generalization of a target behavior | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Prompt self-monitoring of behavior | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 2 |
| Prompt self-monitoring of behavioral outcome | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 2 |
| Prompting focus on past success | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 3 | 3 | 1 |
| Provide feedback on performance | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 3 | 2 |
| Provide information on where and when to perform the behavior | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 |
| Provide instruction on how to perform the behavior | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 |
| Model or demonstrate the behavior | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Teach to use prompts or cues | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 2 | 1 | 2 |
| Environmental restructuring | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 |
| Agree behavioral contract | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 |
| Prompt practice | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 2 | 1 | 2 |
| Use of follow-up prompts | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| Facilitate social comparison | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | 1 | 0 |
| Plan social support or social change | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | 1 | 0 |
| Prompt identification as role model or position advocate | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 |
| Prompt anticipated regret | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fear arousal | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Prompt self talk | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Prompt use of imagery | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Relapse prevention or coping planning | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | 1 | 0 |
| Stress management or emotional control training | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| Motivational interviewing | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Time management | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| General communication skills training | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stimulate anticipation of future rewards | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 2 | 2 | 0 |
| Total | 25 | 10 | 0 | 19 | 4 | 10 | 33 | 29 | 7 | 77 | 43 | 17 |
Results
Summary of Behavior Change Techniques (BCTs) Implemented
Table 1 summarizes the number of BCTs coded as present for each behavior within each system. The version of the software used for each system is detailed in Table 1 footnotes. Between-rater agreement ranged from 0.64 to 1.00, representing substantial to almost perfect agreement. From a possible range of 40 BCTs, the number of BCTs present for physical activity ranged from 19 (Garmin) to 33 (Jawbone), from 4 (Garmin) to 29 (Jawbone) for sleep, and 0 (Fitbit) to 10 (Garmin) for sedentary behavior. When averaged across systems, self-monitoring systems implemented the highest number of BCTs for physical activity (n=26), a smaller number of BCTs were implemented for sleep (n=14), and the fewest BCTs were implemented for sedentary behavior (n=6). The total number of BCTs included within a system also varied (Table 1). The system that included the highest number of BCTs (n=69) across the three behaviors was Jawbone, followed by Fitbit (n=35), and then Garmin (n=33).
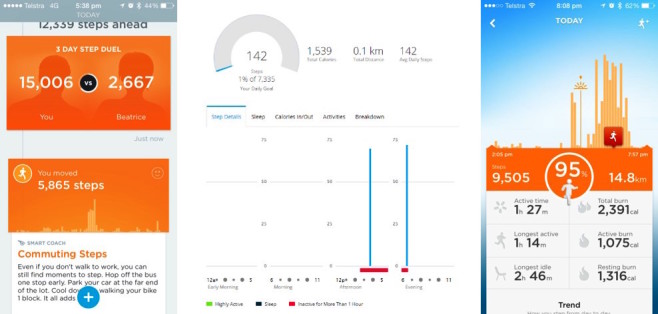
Activity
Table 2 displays which of the 40 BCTs were present within each system for monitoring physical activity. All three systems implemented the following 18 BCTs: providing information about others’ approval, providing normative information about others behavior, goal setting (behavioral and outcome), goal review (behavioral and outcome), prompt rewards contingent on progress toward goal, prompt rewards contingent on successful behavior, shaping, self-monitoring (behavior and outcome), prompting focus on past success, providing feedback on performance, agreeing to behavioral contracts, facilitate social comparison, plan social support, prompt identification of role model, and relapse prevention. Table 2 also details the 6 BCTs that were not implemented in any of the three self-monitoring systems. These were model or demonstrate the behavior, prompt anticipated regret, prompt self-talk, fear arousal, prompt use of imagery, and general communication skills training.
The activity tracker for all three systems measured physical activity, which was then integrated into the app and/or website to provide users with additional feedback on activity levels. For example, self-monitoring systems frequently implemented BCTs related to social support and social comparisons by allowing peers to offer each other social support through the use of app messaging systems and emoji (Figure 1), peer leader boards (Figure 1), and/or challenges which displayed to users a history (amount or pattern) of their peer’s physical activity (Figure 1). Challenges may offer users a “behavioral contract”; this can be used to prevent relapse, as physical activity is required to be performed over multiple days and plan necessary actions to achieve this (Figure 1). Self-monitoring, goal setting, evaluating activity in relation to goals, providing rewards on past success, progress toward goals (Figure 1), and providing feedback were typically delivered by graphical display of the volume of physical activity performed on a daily basis in comparison to a specified physical activity goal (Figures 1). Feedback to users on achieving a goal was typically highlighted by changing the color or pattern of a progress bar or adding a unique identifying feature to the progress bar (eg, a “star” or textured bar graph). In addition, the activity trackers of all systems vibrated and provided visual feedback to users’ when the daily activity goal was achieved. The Garmin system automatically generated a goal for the user, whereas the Fitbit and Jawbone systems allowed users to set their own goal. The Garmin and Jawbone systems also automatically (Garmin) prompted a user (Jawbone) to increase their activity goal if they reached it consistently.
Figure 1.

Screenshots of the app or website displaying how various behavior change techniques (BCTs) related to physical activity were implemented.
Sleep
All three systems implemented the following four BCTs: prompt self-monitoring (behavior and outcome), prompt focus on past success, and provide feedback on performance (Table 2). In terms of how these BCTs were implemented in each system, the activity tracker component of all systems provided a measure of sleep volume and quality. This information was then used to generate feedback to users, focus on past success, and providing feedback were implemented by providing graphical display on the volume and quality of sleep (Figure 2). In addition, Fibit and Jawbone systems also implemented the following 6 BCTs: goal setting (behavior and outcome), prompting review of goals (behavior and outcome), providing rewards contingent on successful behavior, and stimulate anticipation of future rewards. These were operationalized by identifying whether the volume and/or quality of sleep (Figure 2) met a user’s goal or not (Figure 2) and by altering the graphical feedback provided by changing the color or pattern of a progress bar or adding a unique identifying feature to the progress bar (eg, a “star” or textured bar graph). The Jawbone system also implemented action planning, prompting, relapse prevention, time management (Figure 2), and environmental restructuring (Figure 2). Table 2 details the 11 BCTs that were not implemented by any of the self-monitoring systems.
Figure 2.
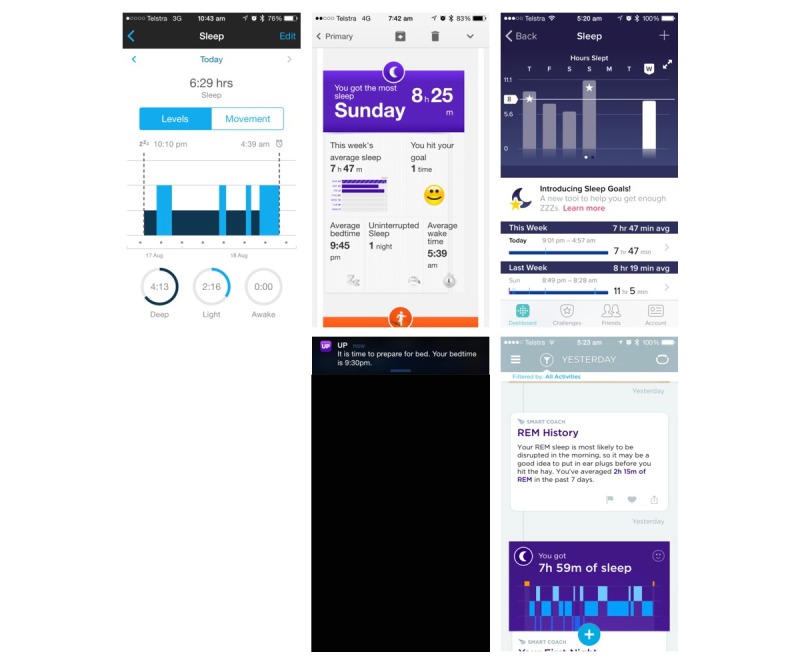
Screenshots of the app or website displaying how various behavior change techniques (BCTs) related to sleep were implemented.
Sedentary Behavior
The Fitbit system did not implement any BCT in relation to sedentary behavior. The Garmin and Jawbone systems both applied the following five BCTs: prompt self-monitoring (behavior and outcome), provide feedback on performance, teach prompts, and prompt practice. These BCTs were implemented by the activity tracker monitoring periods of no physical activity or steps and then displaying this information to users in terms of the volume of sedentary behavior (Figure 3) and specifically identifying periods of “long” sedentary behavior (Figure 3). Both Garmin and Jawbone units provided feedback to users via the activity tracker, vibrating to indicate if they had been sedentary for a “long” period of time. The Garmin system had a default setting of 1 hour of sedentary activity, which could not be altered by users, whereas the Jawbone system allowed this to be defined by the user. This difference resulted in the Garmin being coded as absent for goal setting (behavioral and outcome) in relation to sedentary behavior, whereas the Jawbone was coded as present. Table 2 displays the 28 BCTs that were not implemented by any of the systems in relation to sedentary behavior.
Figure 3.
Screenshots of the app or website displaying how various behavior change techniques (BCTs) related to sedentary behaviour were implemented.
Discussion
Principal Findings
This study assessed the number and type of BCT that three self-monitoring systems implemented to support users in changing their physical activity, sleep, and sedentary behaviors and summarized how the most prevalent BCTs were implemented. The number of BCTs implemented varied between these behaviors. On average, the greatest number of BCTs were implemented in relation to physical activity, followed by sleep and sedentary behavior. All three systems provided self-monitoring of physical activity and sleep and provided feedback to allow the user to focus on their previous success with changing the behavior.
The type of BCT implemented in each system for monitoring physical activity was similar to that observed in other studies [18]. A major difference in the BCT implemented between physical activity, sleep, and sedentary behaviors was the use of challenges, leader boards, and peer to peer “messaging” for physical activity and not for sleep or sedentary behavior. These features operationalize BCTs related to action planning, providing information about others behaviors, social support, shaping, peer approval, and relapse prevention, which may be useful in changing behaviors [19]. These differences may reflect the inherent differences between behaviors and approaches to changing them. For example, the more physical activity people perform, the greater their health benefits [30], and this lends itself to the concept of leader boards and challenges, which can involve frequent peer-to-peer interactions. Yet, for sleep duration, more is not always better as sleep duration has a U-shaped curve in relation to health [31,32], and the concept of “good” sleep is highly individualistic resulting from a complex interaction between the duration, timing, and quality of sleep [1]. As such, whereas goal setting and feedback can be implemented in relation to sleep duration and quality as observed in the systems evaluated (see Figure 2), if leader board and challenge concepts are implemented in relation to sleep, they likely need to be configured around parameters of sleep that are more under the control of the individual, such as sleep hygiene behaviors. For example, the number of days or nights a person went to sleep and woke up at times that “matched” their goals for these behaviors. Alternatively, the concept of leader boards may not be appropriate for sleep. Furthermore, it is important to implement any BCT that seek to improve sleep behaviors in ways which do not increase worry and anxiousness regarding sleep, as this may be detrimental to improving sleep [33].
For sedentary behavior, in light of growing evidence that regular activity breaks are beneficial in comparison with continuous sitting, it may be useful to configure the concept of leader boards and challenges around this premise [34,35]. Leader boards and challenges were implemented in all three systems evaluated in this study in relation to physical activity and are also increasingly implemented in physical activity promotion websites [16]. These features were coded as BCT related to social support, shaping, and relapse prevention; yet, it is unknown how this type of electronic social support compares with in-person peer support and how this influences the efficacy of these strategies. A review of “online social networks” concluded that there was only modest evidence regarding their efficacy to increase physical activity, and continued research is required to clarify their efficacy [36]. Similarly, the evaluated systems implemented “badges” to reward users on their accomplishments, as do many physical activity promotion websites [16]. To date, little is known about how users perceive these features and their effectiveness to change behaviors.
Sleep hygiene education is an effective strategy to improve sleep behaviors in populations with clinical sleep disorders and is also thought to be useful in a public health context to improve the sleep for those people who have sleep complaints but do not have a clinical sleep disorder [37,38]. The Jawbone system implemented the greatest number of BCTs in relation to sleep and did so in a way that was broadly consistent with sleep hygiene guidelines on the timing of sleep, stress reduction, and restructuring the sleep environment to promote sleep [37,38]. It achieved this by measuring sleep and providing feedback on goals using the mobile device notification system to prompt the user to begin getting ready for bed and that their goal time to sleep was approaching. When combined with further education and strategies, these features could help users initiate prebed routines including relaxation techniques to reduce stress and also achieve regularity in the timing of sleep. There is some evidence of the efficacy of these approaches in the literature [37-39], yet, their effectiveness when implemented as part of self-monitoring systems is unknown. These are examples of the BCTs implemented within the Jawbone system that were not implemented within the other systems and highlight how the number and type of BCT implemented vary between the evaluated self-monitoring systems for given behaviors.
Two of the three systems (Jawbone and Garmin) included a vibration alert in the wrist worn activity to alert the user that they had been sedentary for a period of time. This may be a useful prompt to engage in physical activity and reduce sitting time and similar strategies have been implemented as part of ongoing interventions [40]. Although this is an example of a behavioral prompt, it is was not coded as present for goal-setting in the Garmin unit as the user could not set the timing of this feature and therefore adjust their goal. It must also be acknowledged that the two systems that provided feedback on sedentary behavior did so from the perspective of a lack of stepping or movement behavior which does not align with recommended definitions of sedentary behavior [41] and is a function of the technical limitations associated with the activity trackers being worn on the wrist and may have influenced the implementation of BCT for this behavior. Goal-setting is a BCT that is frequently implemented in interventions and is associated with behavior change [8,19,24-26,42]. The Garmin system automatically created a step-based goal for individuals based on the activity level (low, medium, and high) entered when creating a user profile and adjusts the goal based on activity levels the previous day. The Garmin system also used a default 1 hour goal for sedentary behavior, which could not be adjusted by the user, and the inability to adjust this goal was why it was coded as absent for this behavior in the Garmin system. It is unclear how the activity level specified when creating a user profile is translated into a step goal, as is how this automatically created goal relates to existing step-based recommendations [43,44]. The Fitbit and Jawbone systems allowed users to specify their own goals. However, a more useful approach to goal setting for self-monitoring systems may be to provide users with information on the level of behavior for optimum health, information on the goal setting process (eg, promote attainable goals and prompt revision of goals in light of performance), and engage them in the goal setting process (eg, personalized goals) to facilitate users setting goals that move them toward improved health, are attainable, and meaningful to the individual. This approach could be translated to activity, sedentary, and sedentary behaviors in efforts to enhance the way in which goal-setting strategies are implemented.
A total of 18 BCTs were implemented by all three systems in relation to physical activity (Table 2), including those previously associated with increased physical activity, such as providing information on the consequences of the behavior (individual and general), goal setting (behavior and outcome), prompt self-monitoring (behavior and outcome), facilitate social support, prompt practice, and prompt rewards contingent on effort or progress [25,42]. Setting behavioral goals, providing unspecified forms of social support, and adding objects to the environment have been identified as promising BCTs for reducing sedentary time [8]. BCTs related to social support were not present in any of the systems in relation to sedentary behavior and provides an opportunity to expand the capability of the systems to include BCTs that are promising to reduce sedentary time. We are unaware of any previous studies examining BCTs in relation to changes in sleep in either self-monitoring systems or intervention studies; therefore, the insights provided in this study are novel. Although the systems included a number of BCTs which are associated with improved behaviors, to date, there is limited effectiveness surrounding the use of self-monitoring systems to improve these target behaviors [45,46].
A number of BCTs were not implemented in any of the evaluated systems for any of the behaviors (Table 2), and many of these same BCTs are also absent from interventions on other lifestyle behaviors [20,24,26]. Several possibilities may explain this. Designers of self-monitoring systems may simply be unaware of the BCTs literature and implement features guided by the functionality of the system (eg, activity trackers measure amount of movement so systems focus on provided feedback on this), features based on app or website design principles, or features desired by users. Alternatively, omissions of certain BCTs may reflect decisions to implement fewer BCTs as effectively as possible rather than to implement as many as possible in a less effective manner. Furthermore, there is a debate concerning dose-response relationships between the number of BCTs and behavior change and if specific clusters of BCTs are more efficacious than other clusters or if certain BCTs are required to cooccur to maximize potential behavior change [20,24-26]. In light of this, decisions on BCT inclusion and implementation in interventions or self-monitoring systems should be based on addressing the specific behavioral determinants of a behavior. Furthermore, it is unknown how the different combinations of BCTs present in the self-monitoring systems for a specific behavior are related to behavior change. This may also explain differences in the number of BCTs implemented between behaviors, as there is a richer literature on the determinants of physical activity compared with sedentary behavior and sleep [8,47-49]. Furthermore, the mere presence of a BCT does not indicate the way in which it is implemented, which has important implications for behavior change.
Limitations
Limitations of this study include using a behavior change taxonomy that is directed toward changing physical activity and dietary behaviors to assess sleep and sedentary behaviors. Although this was offset by coding the presence or absence of a BCT specifically to the behavior in question. Furthermore, this study did not assess the features and functionality of the systems in relation to sleep hygiene recommendations which are useful in changing sleep behaviors [37,38]. There are many systems currently available, and it is unknown how systems not included in this study compare on their use and implementation of BCTs. All systems were only used over a 1-week period, which is consistent with previous evaluations [18], and a longer period of use may have resulted in a different user experience resulted in additional BCTs being coded as present. However, there are currently no recommendations regarding how long an intervention or self-monitoring system should be used for before coding.
Conclusions
In conclusion, the number and type of BCT implemented varied between the evaluated self-monitoring systems and the number and type of BCT varied between activity, sleep, and sedentary behaviors. The greatest number of BCTs was implemented in relation to physical activity, followed by sleep and sedentary behavior. However, the number of BCTs does not reflect how a BCT is implemented and presented to users, or the cooccurrence of a particular BCT with other BCT, which may influence the potential effectiveness of the self-monitoring system to actually change behavior [27]. It is important to note that this study was evaluating the “potential” of these self-monitoring systems to change activity, sleep, and sedentary behaviors and further research is required to establish their effectiveness to change these behaviors. Such evaluations could also examine the actual usage patterns of these devices and the different types of BCTs that users make use of.
Acknowledgments
The use of brand names is for identification purposes only and does not constitute endorsement by the authors. MJD is supported by a Future Leader Fellowship (ID 100029) from the National Heart Foundation of Australia. CV is supported by a Future Leader Fellowship (ID 100427) from the National Heart Foundation of Australia. CES (1090517), SS (GNT1125586) and AR (GNT1105926) are supported by a National Health and Medical Research Council Early Career Fellowship. SS (ID 101240) is also supported by a Postdoctoral Fellowship from the Australian Heart Foundation of Australia. All data used in this study is provided in Table 2 and is accessible as part of this article.
Abbreviations
- BCTs
behavior change techniques
- CALO-RE
Coventry, Aberdeen, and London-Refined
Footnotes
Authors' Contributions: All authors provided critical review of the manuscript. MJD, CV, and MK conceptualized the study, MJD and BM undertook data collection.
Conflicts of Interest: None declared.
References
- 1.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014 Jan 01;37(1):9–17. doi: 10.5665/sleep.3298. http://europepmc.org/abstract/MED/24470692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010 Jun;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. http://europepmc.org/abstract/MED/19932976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, Lancet Physical Activity Series Working Group Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012 Jul 21;380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9. http://europepmc.org/abstract/MED/22818936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altman NG, Izci-Balserak B, Schopfer E, Jackson N, Rattanaumpawan P, Gehrman PR, Patel NP, Grandner MA. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012 Dec;13(10):1261–70. doi: 10.1016/j.sleep.2012.08.005. http://europepmc.org/abstract/MED/23141932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duncan MJ, Kline CE, Rebar AL, Vandelanotte C, Short CE. Greater bed- and wake-time variability is associated with less healthy lifestyle behaviors: a cross-sectional study. J Public Health. 2016 Feb;24(1):31–40. doi: 10.1007/s10389-015-0693-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, Pratt M, Venugopal K, Chau J, Sjöström M, IPS Group The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ) Am J Prev Med. 2011 Aug;41(2):228–35. doi: 10.1016/j.amepre.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Bauman A, Bull F, Chey T, Craig CL, Ainsworth BE, Sallis JF, Bowles HR, Hagstromer M, Sjostrom M, Pratt M, IPS Group The international prevalence study on physical activity: results from 20 countries. Int J Behav Nutr Phys Act. 2009 Mar 31;6:21. doi: 10.1186/1479-5868-6-21. https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89–112. doi: 10.1080/17437199.2015.1082146. http://europepmc.org/abstract/MED/26315814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P, Brown JS. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012 Jun 01;35(6):769–81. doi: 10.5665/sleep.1872. http://europepmc.org/abstract/MED/22654196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, Ding H, Hooker C, Karunanithi M, Maeder AJ, Noakes M, Tague R, Taylor P, Viljoen P, Mummery WK. Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. J Med Internet Res. 2014 Jun 12;16(6):e136. doi: 10.2196/jmir.3107. http://www.jmir.org/2014/6/e136/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritterband LM, Thorndike FP, Gonder-Frederick LA, Magee JC, Bailey ET, Saylor DK, Morin CM. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009 Jul;66(7):692–8. doi: 10.1001/archgenpsychiatry.2009.66. http://europepmc.org/abstract/MED/19581560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glasgow RE, Lichtenstein E, Marcus AC. Why don't we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003 Aug;93(8):1261–7. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Insight GlobalWebIndex. 2017. [2017-07-20]. GWI Device: GlobalWebIndex's quarterly report on the latest trends for smartphones, tablets, smart TVs and wearables: Summary http://insight.globalwebindex.net/hubfs/Reports/Device_Q1_2017_Summary/GWI-Device-Q1-2017-Summary.pdf?t=1493137444621 .
- 14.Ledger D, McCaffrey D. Endeavour Partners. 2014. [2017-07-20]. Inside Wearables:How the science of human behavior change offers the secret to long-term engagement https://blog.endeavour.partners/inside-wearable-how-the-science-of-human-behavior-change-offers-the-secret-to-long-term-engagement-a15b3c7d4cf3?gi=8f4caa271090 .
- 15.Cowan LT, Van Wagenen SA, Brown BA, Hedin RJ, Seino-Stephan Y, Hall PC, West JH. Apps of steel: are exercise apps providing consumers with realistic expectations?: a content analysis of exercise apps for presence of behavior change theory. Health Educ Behav. 2013 Apr;40(2):133–9. doi: 10.1177/1090198112452126. [DOI] [PubMed] [Google Scholar]
- 16.Vandelanotte C, Kirwan M, Rebar A, Alley S, Short C, Fallon L, Buzza G, Schoeppe S, Maher C, Duncan MJ. Examining the use of evidence-based and social media supported tools in freely accessible physical activity intervention websites. Int J Behav Nutr Phys Act. 2014 Aug 17;11:105. doi: 10.1186/s12966-014-0105-0. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-014-0105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doshi A, Patrick K, Sallis JF, Calfas K. Evaluation of physical activity web sites for use of behavior change theories. Ann Behav Med. 2003;25(2):105–11. doi: 10.1207/S15324796ABM2502_06. [DOI] [PubMed] [Google Scholar]
- 18.Lyons EJ, Lewis ZH, Mayrsohn BG, Rowland JL. Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. J Med Internet Res. 2014 Aug 15;16(8):e192. doi: 10.2196/jmir.3469. http://www.jmir.org/2014/8/e192/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011 Nov;26(11):1479–98. doi: 10.1080/08870446.2010.540664. [DOI] [PubMed] [Google Scholar]
- 20.Hill B, Skouteris H, Fuller-Tyszkiewicz M. Interventions designed to limit gestational weight gain: a systematic review of theory and meta-analysis of intervention components. Obes Rev. 2013 Jun;14(6):435–50. doi: 10.1111/obr.12022. [DOI] [PubMed] [Google Scholar]
- 21.Mercer K, Li M, Giangregorio L, Burns C, Grindrod K. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth. 2016 Apr 27;4(2):e40. doi: 10.2196/mhealth.4461. http://mhealth.jmir.org/2016/2/e40/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014 May;44(5):671–86. doi: 10.1007/s40279-014-0142-5. [DOI] [PubMed] [Google Scholar]
- 23.Breton ER, Fuemmeler BF, Abroms LC. Weight loss-there is an app for that! But does it adhere to evidence-informed practices? Transl Behav Med. 2011 Dec;1(4):523–9. doi: 10.1007/s13142-011-0076-5. http://europepmc.org/abstract/MED/24073074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lara J, Evans EH, O'Brien N, Moynihan PJ, Meyer TD, Adamson AJ, Errington L, Sniehotta FF, White M, Mathers JC. Association of behaviour change techniques with effectiveness of dietary interventions among adults of retirement age: a systematic review and meta-analysis of randomised controlled trials. BMC Med. 2014 Oct 07;12:177. doi: 10.1186/s12916-014-0177-3. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-014-0177-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009 Nov;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 26.Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Obes Rev. 2011 Jul;12(7):e602–20. doi: 10.1111/j.1467-789X.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 27.Peters GJ, de Bruin M, Crutzen R. Everything should be as simple as possible, but no simpler: towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychol Rev. 2015;9(1):1–14. doi: 10.1080/17437199.2013.848409. http://europepmc.org/abstract/MED/25793484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012 Jun;37(3):540–2. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 29.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–74. [PubMed] [Google Scholar]
- 30.Powell KE, Paluch AE, Blair SN. Physical activity for health: What kind? How much? How intense? On top of what? Annu Rev Public Health. 2011;32:349–65. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 31.Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010 Oct;24(5):731–43. doi: 10.1016/j.beem.2010.07.001. http://europepmc.org/abstract/MED/21112022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011 Nov 01;34(11):1487–92. doi: 10.5665/sleep.1382. http://europepmc.org/abstract/MED/22043119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Does cognitive-behavioral insomnia therapy alter dysfunctional beliefs about sleep? Sleep. 2001 Aug 01;24(5):591–9. doi: 10.1093/sleep/24.5.591. [DOI] [PubMed] [Google Scholar]
- 34.Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr. 2013 Aug;98(2):358–66. doi: 10.3945/ajcn.112.051763. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=23803893. [DOI] [PubMed] [Google Scholar]
- 35.Bailey DP, Locke CD. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. 2015 May;18(3):294–8. doi: 10.1016/j.jsams.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 36.Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res. 2014 Feb 14;16(2):e40. doi: 10.2196/jmir.2952. http://www.jmir.org/2014/2/e40/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003 Jun;7(3):215–25. doi: 10.1053/smrv.2001.0246. [DOI] [PubMed] [Google Scholar]
- 38.Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015 Aug;22:23–36. doi: 10.1016/j.smrv.2014.10.001. http://europepmc.org/abstract/MED/25454674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Buysse DJ, Cheng Y, Germain A, Moul DE, Franzen PL, Fletcher M, Monk TH. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Med. 2010 Jan;11(1):56–64. doi: 10.1016/j.sleep.2009.02.010. http://europepmc.org/abstract/MED/19962939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilmot EG, Davies MJ, Edwardson CL, Gorely T, Khunti K, Nimmo M, Yates T, Biddle SJ. Rationale and study design for a randomised controlled trial to reduce sedentary time in adults at risk of type 2 diabetes mellitus: project stand (Sedentary Time ANd diabetes) BMC Public Health. 2011 Dec 08;11:908. doi: 10.1186/1471-2458-11-908. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-11-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pate RR, O'Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008 Oct;36(4):173–8. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 42.Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals' physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2013 Mar 03;10:29. doi: 10.1186/1479-5868-10-29. https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tudor-Locke C, Craig CL, Aoyagi Y, Bell RC, Croteau KA, De Bourdeaudhuij I, Ewald B, Gardner AW, Hatano Y, Lutes LD, Matsudo SM, Ramirez-Marrero FA, Rogers LQ, Rowe DA, Schmidt MD, Tully MA, Blair SN. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011 Jul 28;8:80. doi: 10.1186/1479-5868-8-80. https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tudor-Locke C, Craig CL, Brown WJ, Clemes SA, De Cocker K, Giles-Corti B, Hatano Y, Inoue S, Matsudo SM, Mutrie N, Oppert J, Rowe DA, Schmidt MD, Schofield GM, Spence JC, Teixeira PJ, Tully MA, Blair SN. How many steps/day are enough? For adults. Int J Behav Nutr Phys Act. 2011 Jul 28;8:79. doi: 10.1186/1479-5868-8-79. https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Finkelstein EA, Haaland BA, Bilger M, Sahasranaman A, Sloan RA, Nang EE, Evenson KR. Effectiveness of activity trackers with and without incentives to increase physical activity (TRIPPA): a randomised controlled trial. Lancet Diabetes Endocrinol. 2016 Dec;4(12):983–995. doi: 10.1016/S2213-8587(16)30284-4. [DOI] [PubMed] [Google Scholar]
- 46.Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, Morey BL. Randomized trial of a fitbit-based physical activity intervention for women. Am J Prev Med. 2015 Sep;49(3):414–8. doi: 10.1016/j.amepre.2015.01.020. http://europepmc.org/abstract/MED/26071863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, Lancet Physical Activity Series Working Group Correlates of physical activity: why are some people physically active and others not? Lancet. 2012 Jul 21;380(9838):258–71. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 48.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012 Mar;42(3):e3–28. doi: 10.1016/j.amepre.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 49.Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease? Int Rev Psychiatry. 2014 Apr;26(2):155–76. doi: 10.3109/09540261.2014.911148. http://europepmc.org/abstract/MED/24892892. [DOI] [PMC free article] [PubMed] [Google Scholar]


