Abstract
Objectives
Evaluation of a novel index case finding and linkage‐to‐care programme to identify and link HIV‐infected children (1–15 years) and young persons (>15–24 years) to care.
Methods
HIV‐infected patients enrolled in HIV services were screened and those who reported untested household members (index cases) were offered home‐ or facility‐based HIV testing and counselling (HTC) of their household by a community health worker (CHW). HIV‐infected household members identified were enrolled in a follow‐up programme offering home and facility‐based follow‐up by CHWs.
Results
Of the 1567 patients enrolled in HIV services, 1030 (65.7%) were screened and 461 (44.8%) identified as index cases; 93.5% consented to HIV testing of their households and of those, 279 (64.7%) reported an untested child or young person. CHWs tested 711 children and young persons, newly diagnosed 28 HIV‐infected persons (yield 4.0%; 95% CI: 2.7–5.6), and identified an additional two HIV‐infected persons not enrolled in care. Of the 30 HIV‐infected persons identified, 23 (76.6%) were linked to HIV services; 18 of the 20 eligible for ART (90.0%) were initiated. Median time (IQR) from identification to enrolment into HIV services was 4 days (1–8) and from identification to ART start was 6 days (1–8).
Conclusions
Almost half of HIV‐infected patients enrolled in treatment services had untested household members, many of whom were children and young persons. Index case finding, coupled with home‐based testing and tracked follow‐up, is acceptable, feasible and facilitates the identification and timely linkage to care of HIV‐infected children and young persons.
Keywords: case finding, paediatric HIV, linkage to care, adolescents, HIV testing
Abstract
Objectifs
Evaluation d'un nouveau programme de recherche des cas index et de liaison aux soins pour identifier et lier aux soins les enfants (1 à 15 ans) et les jeunes adultes (>15 à 24 ans) infectés par le VIH.
Méthodes
Les patients infectés par le VIH, inscrits dans les services VIH ont été dépistés et ceux qui ont déclaré des membres du ménage non dépistés (cas index) ont été offerts un dépistage et conseil du VIH à domicile ou en établissement (HTC) pour leur ménage par un agent de santé communautaire (ASC). Les membres du ménage infectés par le VIH ont été inscrits dans un programme de suivi offrant un suivi à domicile et en établissement par les ASC.
Résultats
Sur les 1567 patients inscrits dans les services VIH, 1030 (65,7%) ont été dépistés et 461 (44,8%) ont été identifiés comme cas index. 93,5% ont consenti au dépistage du VIH de leur ménage et de ceux‐ci, 279 (64,7%) ont déclaré un enfant ou un jeune adulte non dépisté. Les ASC ont testé 711 enfants et jeunes adultes, ont diagnostiqué 28 nouvelles personnes infectées par le VIH (rendement 4,0%, IC95%: 2,7 à 5,6) et identifié deux autres personnes infectées par le VIH qui n’étaient pas inscrites aux soins. Sur les 30 personnes infectées par le VIH identifiées, 23 (76,6%) étaient liées aux services VIH. 18 des 20 éligibles à l’ART (90,0%) en ont été initiées. Le délai médian (IQR) de l'identification à l'inscription dans les services VIH était de 4 jours (1 à 8) et de l'identification au début de l’ART était de 6 jours (1 à 8).
Conclusions
Près de la moitié des patients infectés par le VIH, inscrits dans les services de traitement avaient des membres du ménage non testés, dont beaucoup étaient des enfants et des jeunes adultes. La recherche des cas index, couplée aux tests à domicile et au suivi est acceptable, réalisable et facilite l'identification et la liaison opportune aux soins des enfants et les jeunes adultes infectés par le VIH.
Keywords: recherche des cas, VIH pédiatrique, liaison aux soins, adolescents, dépistage du VIH
Abstract
Objetivos
Evaluación de un nuevo programa de hallazgo de casos índice y de vinculación a la atención para identificar y derivar a niños (1‐15 años) y adultos jóvenes (>15‐24 años) infectados con VIH/SIDA.
Métodos
A los pacientes infectados con VIH e inscritos en servicios para el VIH se les realizó el cribado, y a aquellos que reportaron tener en su hogar miembros a quienes no se les habían realizado la prueba (caso índice) se les ofreció que un trabajador comunitario de salud (TCS) les realizara el asesoramiento y la prueba para el VIH en el hogar. Los miembros del hogar identificados como infectados con VIH fueron inscritos en un programa de seguimiento que ofrecía seguimiento con TCS tanto en el hogar como en el centro sanitario.
Resultados
De los 1567 pacientes inscritos en los servicios de VIH, se realizó el cribado a 1030 (65.7%) y 461 (44.8%) se identificaron como un caso índice. Un 93.5% consintió realizarse la prueba para el VIH en el hogar y de estos, 279 (64.7%) reportaron un niño o adulto joven sin testar. Los TCS realizaron la prueba a 711 niños y adultos jóvenes, con nuevo diagnóstico de 28 personas infectadas con VIH (rendimiento del 4.0%; IC 95%: 2.7‐5.6), y adicionalmente se identificaron dos personas infectadas con VIH que no estaban recibiendo atención médica. De las 30 personas infectadas con VIH, 23 (76.6%) fueron vinculadas a servicios para el VIH. 18 de los 20 elegibles para TAR (90.0%) estaban iniciados en el tratamiento. El tiempo medio (rango intercuartil) entre la identificación y la inclusión en servicios de atención para el VIH era de 4 días (1‐8) y desde la identificación hasta el comienzo del TAR, 6 días (1‐8).
Conclusiones
Casi la mitad de los pacientes infectados con VIH y recibiendo tratamiento tenían miembros de sus hogares a los que no se les había realizado la prueba, muchos de los cuales eran niños y adultos jóvenes. El índice de hallazgo de casos, junto con las pruebas en el hogar y un seguimiento monitorizado, es aceptable, factible y facilita la identificación y la vinculación oportuna a la atención de niños y jóvenes adultos infectados con VIH.
Introduction
Significant progress has been made in paediatric and adolescent HIV treatment with an estimated 740 000 children in low‐ and middle‐income countries accessing life‐saving antiretroviral treatment (ART) as of 2014 1. Simplified guidelines and policies 2 in combination with an impressive global effort to increase accessibility of paediatric ART regimens have helped increase the number of children on ART and improve patient outcomes 3, 4. Despite these advances, less than a quarter of eligible children are receiving ART in low‐ and middle‐income countries as compared to nearly 40% of adults 1. A significant challenge to improving ART coverage amongst children is timely identification and linkage 5, without which children are at a high risk of mortality and morbidity 6, 7, 8, 9. Unfortunately, there are few studies or guidelines providing high‐quality evidence to inform child‐focused case finding interventions 10.
Index case finding interventions or strategies that use a known HIV‐infected person receiving HIV care as an index reference case to actively and systematically target partners or spouses for HIV testing have been shown to be acceptable, feasible and high yield for identifying HIV‐infected adults 11, 12, 13, 14, 15, 16. Several studies suggest that the majority of children of HIV‐infected adults in care remain untested 17, 18, 19. Nevertheless, there is a paucity of evidence describing the use of this type of index case finding for the identification and linkage to care of HIV‐infected children and young persons 17, 19, 20, 21, 22.
This study describes the implementation of an index case finding and linkage intervention and evaluates its impact on identification and linkage to care of HIV‐infected children and young persons.
Method
Setting and patient population
This study was conducted between July 2014 and April 2015 at Mponela health centre, a semi‐urban, government‐funded health facility in central Malawi, with an estimated adult (age 15–49 years) HIV prevalence of 5.2% and a catchment area of 65 300 patients 23. At the start of the intervention 1567 people were enrolled in the HIV treatment programme and 1243 of them were on ART.
Details of the intervention
The household HIV testing and counselling (HH‐HTC) programme was aimed at identifying and linking HIV‐infected children and young persons to care. The HH‐HTC programme was part of Tingathe Outreach Program activities. The Tingathe programme and details of how CHWs were selected, trained, supervised and remunerated are described elsewhere 5, 24, 25. In brief, in partnership with the Malawi Ministry of Health, Tingathe uses community health workers (CHWs) to support HIV care services. CHWs’ key roles include providing HIV testing and counselling (HTC) services, linking HIV‐infected patients to care and conducting adherence monitoring of HIV‐infected pregnant and breastfeeding mothers and their children. Further, in a focused effort to enrol and retain HIV‐infected and exposed children into HIV care, a dedicated CHW is assigned to each child to provide routine home and facility‐based follow‐up.
All patients enrolled in HIV care between July 2014 and February 2015 were eligible for HH‐HTC services. One CHW was assigned per day to screen patients to determine the HIV status of their household members. As per community and health centre recommendation, paediatric patients (defined as those 16 years and younger) were only screened if a parent or guardian was present. After screening, any patient reporting a household member with an unknown HIV status was offered the option of either home‐ or facility‐based HH‐HTC for their untested household members. An index case was defined as any patient already enrolled in HIV services who reported having an untested household member. A household member was defined as any person living within the same compound of the index case at the time of screening.
For index cases that chose home‐based testing, a CHW visited their home at a time/date most convenient for the index case. If untested household members were not at home during the initial visit, the CHW made one additional visit in an attempt to capture all members. Index cases that chose facility‐based testing were instructed to bring their untested household members to the facility and upon arrival go directly to the CHW office to receive HTC services. CHWs offered at least two phone‐based reminders to come for HIV testing for index cases that did not bring their household members to the facility for HTC.
During home‐ and facility‐based testing sessions, HTC services were offered to all household members in addition to any other person present at the testing session. HIV testing history and the individual's relationship to the index case were recorded for all persons present. Relationship status included spouse, biological child, biological sibling or other. CHWs then offered an HIV test to those with an unknown HIV status. As per national guidelines, consent was obtained prior to testing from each individual, or in the case of minors under the age of 13, from their guardian 26. All those who consented were given group pre‐test counselling followed by individual testing in accordance with Ministry of Health (MOH) HIV Testing and Counselling guidelines 26. Infants under one were referred to the health facility for DNA‐PCR testing. Family members and spouses were encouraged to receive post‐test counselling together to facilitate disclosure.
All persons newly diagnosed with HIV infection and those who were identified with a known HIV infection but not enrolled in HIV care were followed for up to three months by CHWs. The last person eligible for follow‐up was identified in January 2015 and follow‐ups were concluded in April 2015. During this time, CHWs offered in‐depth counselling, provided guidance in accessing HIV services and assisted those eligible for ART to start. Those who missed a scheduled enrolment appointment or were hesitant to enrol in HIV care services were visited at home and phoned by CHWs to follow‐up and provide additional support including adherence counselling, assistance with disclosure, and in‐depth counselling on the importance of ART to prevent transmission and promote healthy living. Outcomes were recorded for persons identified as HIV‐infected either when they enrolled into HIV care, or if not yet enrolled, at the end of the 3‐month follow‐up period. Outcomes included started ART, enrolled into HIV care (enrolled in care, but not eligible to start ART), died, moved, lost to follow‐up and refused. ART eligibility was assessed by MOH clinicians. As per Malawi Ministry of Health ART guidelines in place at the time, pregnant and breastfeeding women, children less than 5 years of age, persons with WHO Stage 3 or 4 and persons with CD4 less than or equal to 500 cells/mm3 were eligible for ART 27, 28.
Data collection and analysis
Programme data from paper medical records of consenting index cases and those tested aged 1–24 years were extracted and included in the analysis. Infants under one were excluded from the analysis because early infant diagnosis (EID) required a DNA‐PCR test at the health facility. Due to the nature of existing EID interventions at the health facility, it was impossible to determine whether the testing was a result of the HH‐HTC intervention. Testing and HH‐HTC outcome data were stratified by age group into children (age 1–15 years old) and young persons (>15–24 years old). The 15‐year cut‐off is in line with Malawi Ministry of Health and UNICEF definitions, facilitating comparison with other studies 29, 30.
Data were anonymised before analysis. Aggregate data were reported as mean with standard deviation (SD) if normally distributed and median with interquartile range (IQR) otherwise.
Analyses were performed using Stata Version 13 (StataCorp LP, College Station, Texas). The Malawi National Health Sciences Research Committee and the Baylor College of Medicine institutional review board granted ethics approval.
Results
Index cases and uptake of HH‐HTC
During the intervention, of the 1567 patients enrolled in HIV services, 1030 (65.7%) were screened for eligibility for HH‐HTC services (Figure 1). Of those screened, 461 (44.8%) were eligible for HH‐HTC (index cases). Uptake of HH‐HTC was high amongst index cases with 431 (93.5%) consenting, of whom 380 (88.2%) preferred home‐based over facility‐based testing.
Figure 1.
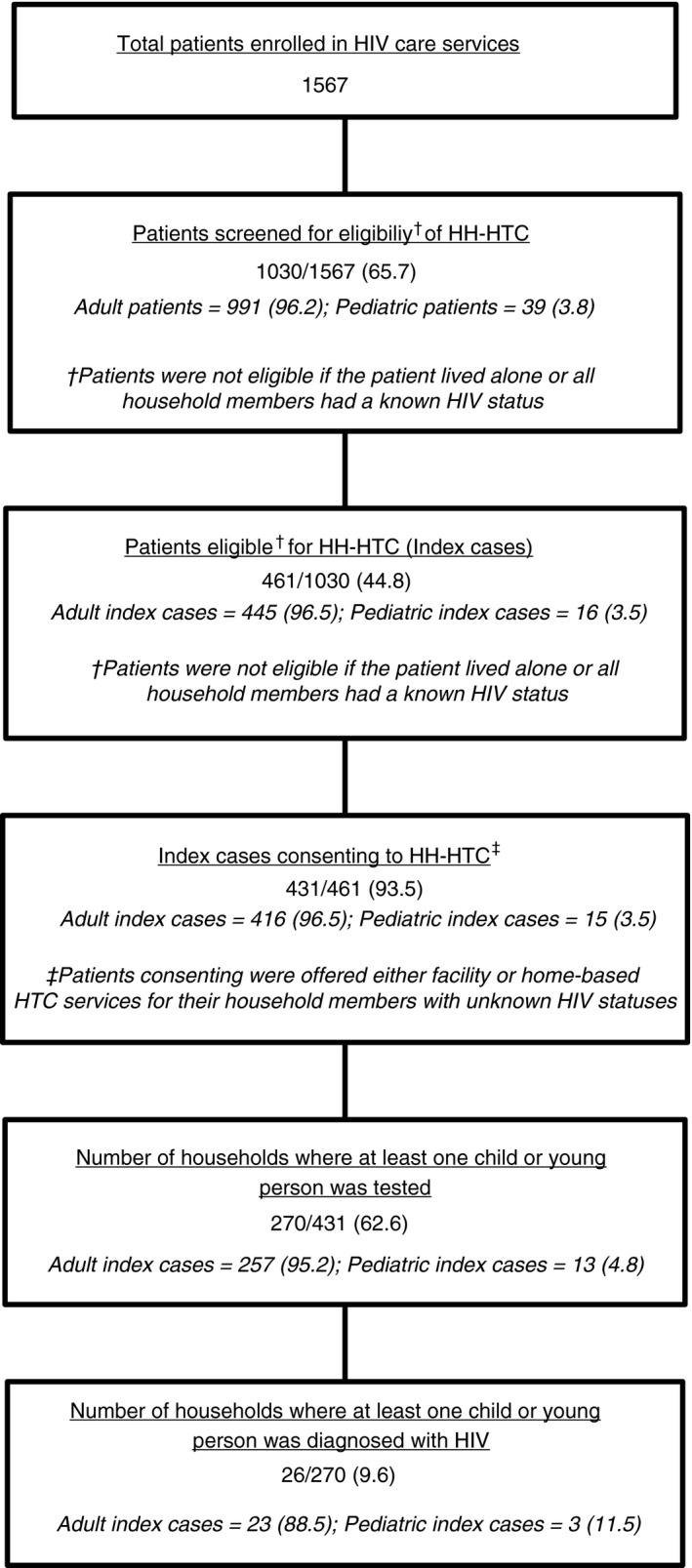
Summary of screening, enrolment and testing of Household‐HTC (HH‐HTC) programme.
Of the 416 consenting adult index cases, 259 (66.6%) were on ART for more than one year, 258 (62.0%) were non‐pregnant females and 299 (71.9%) had only primary‐level education. The median (IQR) age of the adults was 37 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45 years. The remaining 15 consenting were paediatric index cases. Of these, the majority (57.1%) were on ART for less than one year and were females (66.7%) with a mean (SD) age of 7 years (0.89). Of the adult index cases, 272 (65.4%) reported an untested biological child and 7 (46.7%) of the paediatric index cases reported an untested biological sibling.
Testing, identification and characteristics of HIV‐infected children and young persons tested
CHWs conducted testing sessions at 358 households in total. Of those, 270 (75.4%) had at least one child or young person tested. In 26 (9.6%) of those households where a child or young person was tested, at least one child or young person was newly diagnosed with HIV. In total, 711 children and young persons were tested, and 28 were newly diagnosed with HIV, resulting in a 4.0% yield [95% CI: 2.7–5.6] (Table 1). The average number of individuals who needed to be tested to yield one new case was 25.4 (28/711).
Table 1.
Characteristics of children and young persons who received a HIV test
| Characteristic | Children Tested 1–15 years n = 546 (%) | Young Persons Tested >15–24 years n = 165 (%) | Total Tested 1–24 years n = 711 (%) |
|---|---|---|---|
| Index case type | |||
| Paediatric | 16 (2.9) | 4 (2.4) | 20 (2.8) |
| Adult | 530 (97.1) | 161 (97.6) | 691 (97.2) |
| Sex | |||
| Male | 280 (51.3) | 67 (40.6) | 347 (48.8) |
| Female, Non‐pregnant | 266 (48.7) | 93 (56.4) | 358 (50.5) |
| Female, Pregnant | 0 (0.0) | 5 (3.0) | 5 (0.7) |
| Median Age, years (IQR) | 8 (5–11) | 21 (18–23) | 10 (6–15) |
| Relation to Index | |||
| Biological Child | 355 (65.0) | 35 (21.2) | 390 (54.8) |
| Sibling | 20 (3.7) | 10 (6.0) | 30 (4.2) |
| Spouse | 0 (0.0) | 9 (5.5) | 9 (1.3) |
| Other | 171 (31.3) | 111 (67.3) | 282 (39.7) |
| Rapid test result | |||
| Positive | 21 (3.8) | 7 (4.2) | 28 (4.0) |
| Negative | 523 (95.8) | 157 (95.2) | 680 (95.6) |
| Inconclusivea | 2 (0.4) | 1 (0.6) | 3 (0.4) |
Inconclusive: both sets (first pass and immediate repeat) of tests were discordant.
Characteristics and outcomes of HIV‐infected children and young persons identified during HH‐HTC
During home‐based testing sessions, CHWs also identified two additional children that had a known HIV infection but were not enrolled in care, resulting in a total of 30 HIV‐infected children and young persons in need of linkage to care. The mean (SD) age of those identified was 10 years (7.6), and the majority were a biological child to the index case (56.7%), had never been tested for HIV (66.7%) and were eligible for ART (66.7%) (Table 2).
Table 2.
Characteristics of HIV‐infected children and young persons identified
| Characteristic | Children 1–15 years n = 23 (%) | Young Persons >15–24 years n = 7 (%) | Total 1–24 years n = 30 (%) |
|---|---|---|---|
| Index case type | |||
| Paediatric | 2 (8.7) | 2 (28.6) | 4 (13.3) |
| Adult | 21 (91.3) | 5 (71.4) | 26 (86.7) |
| HIV status at identification | |||
| New RapidPositive | 21 (91.3) | 7 (100) | 28 (93.3) |
| Known Infected, not in care | 2 (8.7) | 0 (0.0) | 2 (6.7) |
| Relationship to index case | |||
| Biological Child | 17 (73.9) | 0 (0.0) | 17 (56.7) |
| Biological Sibling | 1 (4.4) | 1 (14.3) | 2 (6.7) |
| Spouse | 0 (0.0) | 4 (57.1) | 4 (13.3) |
| Other | 5 (21.7) | 2 (28.6) | 7 (23.3) |
| HIV testing history | |||
| Never Tested | 18 (78.3) | 2 (28.6) | 20 (66.6) |
| Last Negative | 3 (13.0) | 3 (42.8) | 6 (20.0) |
| Last Positive | 2 (8.7) | 0 (0.0) | 2 (6.7) |
| Missing/Unknown | 0 (0.0) | 2 (28.6) | 2 (6.7) |
| Sex, Male | 10 (43.5) | 2 (28.6) | 12 (40.0) |
| Mean Age, years (SD) | 6.1 (4.6) | 21 (1.9) | 10 (7.6) |
| Eligible for ART reason | |||
| Not Eligible | 4 (17.4) | 1 (14.3) | 5 (16.7) |
| Yes, under five | 12 (52.2) | 0 (0.0) | 12 (40.0) |
| Yes, breastfeeding | 0 (0.0) | 1 (14.3) | 1 (3.3) |
| Yes, CD4 < 500 | 3 (13.0) | 2 (28.6) | 5 (16.7) |
| Yes, WHO Stage 3 or 4 | 2 (8.7) | 0 (0.0) | 2 (6.6) |
| Unknown Eligibility | 2 (8.7) | 3 (42.8) | 5 (16.7) |
| WHO stage | |||
| Stage 1 | 11 (47.8) | 3 (42.9) | 14 (46.7) |
| Stage 2 | 2 (8.7) | 0 (0.0) | 2 (6.7) |
| Stage 3 | 4 (17.4) | 0 (0.0) | 4 (13.3) |
| Not donea | 6 (26.1) | 4 (57.1) | 10 (33.3) |
Was not done because did not return to see a clinician after identification or normally do not stage if patient is universally eligible or staging was not recorded.
Of the 30 HIV‐infected children and young persons identified, 23 (76.7%) were enrolled in HIV services, two (6.7%) died, two (6.7%) moved, one (3.3%) was lost and two (6.7%) refused HIV care. Of the 23 that were enrolled in HIV services, 18 were eligible for ART and started (Table 3). Median time (IQR) from identification to enrolment into HIV services was 4 days (1–8) and from identification to ART start was 6 days (1–8).
Table 3.
Outcomes of HIV‐infected children and young persons identified
| Children 1–15 years n = 23 (%) | Young Persons >15–24 years n = 7 (%) | Total 1–24 years n = 30 (%) | |
|---|---|---|---|
| Outcomea | |||
| Started ART | 15 (65.2) | 3 (42.8) | 18 (60.0) |
| Enrolled in HIV care programme (not eligible for ART) | 4 (17.4) | 1 (14.3) | 5 (16.6) |
| Died | 2 (8.7) | 0 (0.0) | 2 (6.7) |
| Moved | 2 (8.7) | 0 (0.0) | 2 (6.7) |
| Lost | 0 (0.0) | 1 (14.3) | 1 (3.3) |
| Refused | 0 (0.0) | 2 (28.6) | 2 (6.7) |
| Median number of days from identification to enrolment into HIV servicesc (IQR) | 4 (1–8) | 4 (0.5–37) | 4 (1–8) |
| Median number of days from identification to start of ARTb (IQR) | 6 (1–8) | 6 (0–37) | 6 (1–8) |
Outcome was recorded once the patient was enrolled in HIV services and if eligible started ART, or if not enrolled at the end of the 3‐month follow‐up period.
Using data from only those that started ART.
Using data only from those that started ART and those enrolled in HIV care programme.
Testing yield and outcomes of children and young persons by HIV testing location
Of the 711 HIV tests conducted on children and young persons, 679 (95.5%) were conducted at the index case's home. Home‐based testing yielded 19 (2.8% of those tested) new HIV infections and facility‐based testing yielded 9 (28.1% of those tested) (Table 4). Of the 19 children and young persons newly diagnosed through home‐based testing, 15 (78.9%) were linked to care, whereas six (66.7%) of the nine diagnosed in the facility were linked.
Table 4.
Testing yield and outcomes of children and young persons by HIV testing location
| Home‐Based n = 679 (%) | Facility‐Based n = 32 (%) | |
|---|---|---|
| HIV tests done | ||
| Children (1–15 years) | 523 (77.0) | 23 (71.9) |
| Young Persons (>15–24 years) | 156 (23.0) | 9 (28.1) |
| Total (1–24 years) | 679 (100.0) | 32 (100.0) |
| New HIV infections diagnosed | ||
| Children (1–15 years) | 17 (2.5) | 4 (12.5) |
| Young Persons (>15–24 years) | 2 (0.3) | 5 (15.6) |
| Total (1–24 years) | 19 (2.8) | 9 (28.1) |
| Linked to HIV Carea , b | n = 19 | n = 9 |
| Children (1–15 years) | 14 (73.7) | 3 (33.3) |
| Young Persons (>15–24 years) | 1 (5.3) | 3 (33.3) |
| Total (1–24 years) | 15 (78.9) | 6 (66.7) |
n is the number of patients identified as eligible to be linked to HIV care (equal to number of new HIV infections diagnosed).
Linked to HIV care includes ART initiation for those eligible, or if not eligible, enrolment into HIV care programme.
Discussion
To improve ART coverage in children and young persons, novel approaches to identifying and linking them to care, such as index case finding interventions, are needed. Despite country and international guidelines that encourage testing of family members of persons living with HIV 27, 28, our study suggests that household HIV testing of people enrolled in HIV care is not routinely performed. More than half of the index cases screened reported having an untested household member and nearly two‐thirds of those consenting to HH‐HTC reported the untested household member as being a biological child. Further, unlike similar studies that only used HIV‐infected adults as index cases 14, 15, 16, 19, 31, 32, we included paediatric patients and found that 18% of those screened reported an untested sibling. With a 93% acceptance rate of household testing, reinforcing the importance of family testing and offering it either at home or the health facility to patients at every clinic visit represents a crucial opportunity for reaching this high‐risk population.
A recent systematic review of HIV testing strategies of children and adolescents including 21 studies conducted in sub‐Saharan Africa found the average yield of home‐based and family‐centred testing efforts to be 2.3% [95% CI: 0.7–4.0] and 3.3% [95% CI: 1.7–4.9], respectively 10. In a similar index case study by Wagner et al., yield was 7.4% ([95% CI: 3.3–14.1%] 19. Our 4.0% [95% CI: 2.7–5.6] yield is within the upper level of those described in the systematic review, though on the lower range of the Wagner study. However, our 3.8% [CI: 2.5–5.8] yield in children is higher than the national estimated prevalence of 1.6% [95% CI: 1.2–2.0] according to a recent national survey 33. Further, this yield is comparable to programmatic data from Tingathe's provider‐initiated testing and counselling (PITC) paediatric inpatient yields in Malawi of 3.3–4.1% 34 in areas where HIV prevalence is approximately 16% 33. Thus, the yield from this study is likely higher than what could be achieved with universal testing and is comparable to the yield from targeted interventions in high prevalence areas. This suggests an approach similar to the one used in this present study which actively screens, then tracks both paediatric and adult HIV‐infected patients with untested household members is a more effective strategy for identifying HIV‐infected children and young persons than universal testing alone.
The vast majority (88%) of index cases in our study preferred home‐based testing. Similar to another study in Kenya 35, we found that both men and women preferred home‐based testing to facility‐based testing. However, in some cases, CHWs were unable to provide home‐based testing because no one was present at home, or the homes could not be found due to poor directions. Despite this, home‐based testing remains a viable option for many patients because of its convenience and privacy. In higher prevalence, more densely populated areas or in areas where home visits could be more accurately planned, this strategy could have greater yield. Further, with 75% of index case households tested providing testing of a child or young person, home‐based testing provides an opportunity to reach this population of young adults that may not be found in a facility‐based setting 36.
Facility‐based testing found 28% of persons tested to be HIV positive, which was eightfold greater than home‐based testing and threefold greater than similar facility‐based outpatient testing efforts in children and adolescents 10. We believe our higher yield may be due to index cases being prompted to test their household members while already suspecting their positive status. However, routine facility‐based testing efforts, including provider‐initiated testing and counselling (PITC) and interventions that systematically track untested children of HIV‐infected patients and provide referrals for testing, can increase paediatric HIV testing. These strategies remain an important method of identifying children and young persons living with HIV in areas where human resources are inadequate for home‐based testing 10, 19, 32, 37, 38, 39, 40.
A systematic review of linkage‐to‐care programmes in sub‐Saharan Africa estimates that less than one‐third of people identified with HIV are retained in care between the time they are tested and the time they commence ART treatment 41. The multifaceted linkage approach used in this intervention which combined in‐depth counselling, phone call reminders and home‐ and facility‐based follow‐ups resulted in over 75% of those identified with HIV being enrolled into HIV care services. In studies specifically looking at linkage from home‐based testing initiatives 42, 43, 44, 45, linkage rates range from 42% to 96%. Our study's linkage rate was on the higher end of the spectrum at 78.9%, a result we believe to be due in part to the family‐based approach to pre‐ and post‐test counselling. Several studies have suggested that family‐based approaches such as this improve intrafamily disclosure and communication surrounding HIV care, thus improving linkage and response to treatment 31, 46. Another reason for our high linkage rate could be the continued support and follow‐up of CHWs. Qualitative data from a study by Ware et al. suggests that home‐based testing combined with follow‐up reduces linkage barriers by building supportive, ‘social‐bridges’ between the CHW and the patient 47, 48.
To improve paediatric outcomes, those identified as HIV‐infected need timely entry into care. Our results show a median time to ART initiation of 6 days (IQR: 1–8), a marked improvement to the standard of care demonstrated in a similar clinic in Malawi with median time to ART initiation of 59 days (IQR: 10–330) 49. Long waiting times, poor staff–patient relationships and inadequate counselling 50, 51 have all been cited as barriers to ART initiation. In our study, CHWs helped with the initiation process at the facility, provided targeted counselling, prioritised children and guided patients through ART initiation procedures. However, linkage to care is only one step in the continuum. Recent systematic studies have shown younger age to be a predictor for non‐adherence 52 and paediatric retention in care to be suboptimal 53. To achieve viral suppression in children and adolescents, further research on improving adherence and retention post‐linkage need to be explored.
The strengths of our study included that we were able to evaluate both identification and linkage outcomes of the intervention with our multifaceted strategy. We also included young persons, addressing a gap in adolescent‐focused testing strategies. However, some limitations must be taken into consideration when interpreting the results. First, we cannot be sure that patients honestly reported their household members’ HIV status or those members in need of testing, leading to potential response bias. Some patients may have underreported household members in need of testing for reasons such as fear of disclosure or stigma by family or community members and/or fear of knowing the HIV status of their household members. Overreporting may have been caused by participants thinking that falsely reporting untested members and participation in the activity would bring them additional incentives. To avoid this, it was clearly communicated during screening that no incentives or special treatment would be given to participating patients. Further, the HH‐HTC intervention took place within the Tingathe Programme's routine intervention. This may have influenced the uptake of household testing as patients were already accustomed to CHWs and their involvement within the community. Therefore, they may have been more likely to consent and choose home‐based vs. facility‐based testing. This study was conducted at one health facility and may not be generalisable.
Conclusions
Early identification and timely linkage to care are essential to improve outcomes of children and young persons living with HIV. In our study, almost half of HIV‐infected patients enrolled in treatment services had untested household members. A family‐centred, index case finding approach, coupled with home‐based testing and tracked follow‐up is acceptable and feasible, and facilitates the identification and timely linkage to care of HIV‐infected children and young persons.
Acknowledgements
We thank the Malawi Ministry of Health for their partnership in this endeavour, and the team of CHWs, nurses, clinicians and other staff at Mponela Health Centre for their careful data collection and support. We are grateful to all the HIV‐infected patients enrolled in our programme and the CHWs and clinicians who helped care for them. This publication was made possible by support from USAID cooperative agreement number 674‐A‐00‐10‐00093‐00. MHK was supported by the Fogarty International Center of the National Institutes of Health under award number K01 TW009644. The funders had no role in study design, data collection and analysis, decision to publish or preparation of this manuscript. The contents are the responsibility of the authors and do not necessarily reflect the views of the funders, including the National Institutes of Health, USAID and the United States Government. This study was present in part as a poster at the International AIDS Society Conference in Durban, July 2016 Abstract #TUPEE484.
References
- 1. WHO . Global Update on the Health Sector Response to HIV. World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- 2. WHO, UNICEF, UNAIDS . Global Update on HIV Treatment 2013: Results, Impact and Opportunities. World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- 3. Kabue MM, Buck WC, Wanless SR et al Mortality and clinical outcomes in HIV‐infected children on antiretroviral therapy in Malawi, Lesotho, and Swaziland. Pediatrics 2012: 130: e591–e599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brady MT, Oleske JM, Williams PL et al Declines in mortality rates and changes in causes of death in HIV‐1‐infected children during the HAART era. J Acquir Immune Defic Syndr 2010: 53: 86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahmed S, Kim MH, Dave AC et al Improved identification and enrolment into care of HIV‐exposed and ‐infected infants and children following a community health worker intervention in Lilongwe, Malawi. J Int AIDS Soc 2015: 18: 19305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cotton MF, Violari A, Otwombe K et al Early time‐limited antiretroviral therapy versus deferred therapy in South African infants infected with HIV: results from the children with HIV early antiretroviral (CHER) randomised trial. Lancet 2013: 382: 1555–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cotton MF, Rabie H. Impact of earlier combination antiretroviral therapy on outcomes in children. Curr Opin HIV AIDS 2015: 10: 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Innes S, Lazarus E, Otwombe K et al Early severe HIV disease precedes early antiretroviral therapy in infants: are we too late? J Int AIDS Soc 2014: 17: 18914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Violari A, Cotton MF, Gibb DM et al Early antiretroviral therapy and mortality among HIV‐infected infants. New Engl J Med 2008: 359: 2233–2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Govindasamy D, Ferrand RA, Wilmore SM et al Uptake and yield of HIV testing and counselling among children and adolescents in sub‐Saharan Africa: a systematic review. J Int AIDS Soc 2015: 18: 20182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jurgensen M, Sandoy IF, Michelo C, Fylkesnes K. Effects of home‐based voluntary counselling and testing on HIV‐related stigma: findings from a cluster‐randomized trial in Zambia. Soc Sci Med 2013: 81: 18–25. [DOI] [PubMed] [Google Scholar]
- 12. Helleringer S, Kohler HP, Frimpong JA, Mkandawire J. Increasing uptake of HIV testing and counseling among the poorest in sub‐Saharan countries through home‐based service provision. J Acquir Immune Defic Syndr 2009: 51: 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wachira J, Kimaiyo S, Ndege S, Mamlin J, Braitstein P. What is the impact of home‐based HIV counseling and testing on the clinical status of newly enrolled adults in a large HIV care program in Western Kenya? Clin Inf Dis 2012: 54: 275–281. [DOI] [PubMed] [Google Scholar]
- 14. Rosenberg NE, Mtande TK, Saidi F et al Recruiting male partners for couple HIV testing and counselling in Malawi's option B+ programme: an unblinded randomised controlled trial. Lancet HIV. 2015: 2: e483–e491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brown LB, Miller WC, Kamanga G et al HIV partner notification is effective and feasible in Sub‐Saharan Africa: opportunities for HIV treatment and prevention. J Acquir Immune Defic Syndr 2011: 56: 437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Henley C, Forgwei G, Welty T et al Scale‐up and case‐finding effectiveness of an HIV partner services program in Cameroon: an innovative HIV prevention intervention for developing countries. Sex Transm Dis 2013: 40: 909–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cohen D, Lungu M, van Oosterhout JJ. HIV testing coverage of family members of adult antiretroviral therapy patients in Malawi. AIDS Care 2010: 22: 1346–1349. [DOI] [PubMed] [Google Scholar]
- 18. Were WA, Mermin JH, Wamai N et al Undiagnosed HIV infection and couple HIV discordance among household members of HIV‐infected people receiving antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr 2006: 43: 91–95. [DOI] [PubMed] [Google Scholar]
- 19. Wagner AD, Mugo C, Njuguna IN et al Implementation and operational research: active referral of children of HIV‐positive adults reveals high prevalence of undiagnosed HIV. J Acquir Immune Defic Syndr 2016: 73: e83–e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chhagan MK, Kauchali S, Arpadi SM et al Failure to test children of HIV‐infected mothers in South Africa: implications for HIV testing strategies for preschool children. Trop Med Int Health 2011: 16: 1490–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. O'Donnell K, Yao J, Ostermann J et al Low rates of child testing for HIV persist in a high‐risk area of East Africa. AIDS Care 2014: 26: 326–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ng'eno B, Mwangi A, Ng'ang'a L et al Burden of HIV infection among children aged 18 months to 14 years in Kenya: results from a nationally representative population‐based cross‐sectional survey. J Acquir Immune Defic Syndr 2014: 66(Suppl 1): S82–S88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. UNAIDS . Malawi Developing Subnational Estimates of HIV Prevalence and the Number of People Living With HIV. UNAIDS: Geneva, Switzerland, 2014. [Google Scholar]
- 24. Kim MH, Ahmed S, Buck WC et al The Tingathe programme: a pilot intervention using community health workers to create a continuum of care in the prevention of mother to child transmission of HIV (PMTCT) cascade of services in Malawi. J Int AIDS Soc 2012: 15(Suppl 2): 17389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim MH, Ahmed S, Preidis GA et al Low rates of mother‐to‐child HIV transmission in a routine programmatic setting in Lilongwe, Malawi. PLoS ONE 2013: 8: e64979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Malawi Ministry of Health . Guidelines for HIV Testing and Counselling. Malawi Ministry of Health: Lilongwe, Malawi, 2009. [Google Scholar]
- 27. WHO . The use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. World Health Organization: Geneva, Switzerland; 2013. [PubMed] [Google Scholar]
- 28. Malawi Ministry of Health . Clinical Management of HIV in Children and Adults. Malawi Ministry of Health: Lilongwe, Malawi, 2014. [Google Scholar]
- 29. Malawi Ministry of Health . Clinical Management of HIV in Children and Adults (3rd edn), Malawi Ministry of Health: Lilongwe, Malawi, 2016. [Google Scholar]
- 30. UNDESA . Definition of Youth. United Nations Department of Economic and Social Affairs; 2013.
- 31. Lewis Kulzer J, Penner JA, Marima R et al Family model of HIV care and treatment: a retrospective study in Kenya. J Int AIDS Soc 2012: 15: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mongare J, Odhiambo F, Ojoo S et al Client‐centered HIV testing and counseling as a strategy for scaling up access to HIV prevention and care services 7th IAS Conference on HIV Pathogenesis. Kuala Lumpur, Malaysia: International AIDS Society (IAS); 2013.
- 33. MPHIA . Malawi Population‐Based HIV Impact Assessment Summary Sheet: Preliminary Findings. Malawi Population‐Based HIV Impact Assessment: Lilongwe, Malawi; December 2016. [Google Scholar]
- 34. BCM‐CFM, Tingathe . Annual Report FY2016: Tingathe‐ Community Health Workers as a Bridge Between PMTCT, EID and Pediatric HIV Services. Baylor College of Medicine Children's Foundation Malawi – Tingathe: Lilongwe, Malawi, 2016. [Google Scholar]
- 35. Osoti AO, John‐Stewart G, Kiarie JN et al Home‐based HIV testing for men preferred over clinic‐based testing by pregnant women and their male partners, a nested cross‐sectional study. BMC Infect Dis 2015: 15: 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Idele P, Gillespie A, Porth T et al Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr 2014: 66(Suppl 2): S144–S153. [DOI] [PubMed] [Google Scholar]
- 37. Ferrand RA, Meghji J, Kidia K et al Implementation and operational research: the effectiveness of routine opt‐out HIV testing for children in Harare, Zimbabwe. J Acquir Immune Defic Syndr 2016: 71: e24–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McCollum ED, Preidis GA, Kabue MM et al Task shifting routine inpatient pediatric HIV testing improves program outcomes in urban Malawi: a retrospective observational study. PLoS ONE 2010: 5: e9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McCollum ED, Preidis GA, Golitko CL et al Routine inpatient human immunodeficiency virus testing system increases access to pediatric human immunodeficiency virus care in sub‐Saharan Africa. Pediatr Infect Dis J 2011: 30: e75–e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cohn J, Whitehouse K, Tuttle J, Lueck K, Tran T. Paediatric HIV testing beyond the context of prevention of mother‐to‐child transmission: a systematic review and meta‐analysis. Lancet HIV 2016: 3: e473–e481. [DOI] [PubMed] [Google Scholar]
- 41. Rosen S, Fox MP. Retention in HIV care between testing and treatment in Sub‐Saharan Africa: a systematic review. PLoS Med 2011: 8: e1001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Naik R, Doherty T, Jackson D et al Linkage to care following a home‐based HIV counselling and testing intervention in rural South Africa. J Int AIDS Soc 2015: 18: 19843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hatcher AM, Turan JM, Leslie HH et al Predictors of linkage to care following community‐based HIV counseling and testing in rural Kenya. AIDS Behav 2012: 16: 1295–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Medley A, Ackers M, Amolloh M et al Early uptake of HIV clinical care after testing HIV‐positive during home‐based testing and counseling in western Kenya. AIDS Behav 2013: 17: 224–234. [DOI] [PubMed] [Google Scholar]
- 45. van Rooyen H, Barnabas RV, Baeten JM et al High HIV testing uptake and linkage to care in a novel program of home‐based HIV counseling and testing with facilitated referral in KwaZulu‐Natal, South Africa. J Acquir Immune Defic Syndr 2013: 64: e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. van Rooyen H, Essack Z, Rochat T et al Taking HIV testing to families: designing a family‐based intervention to facilitate HIV testing, disclosure, and intergenerational communication. Frontiers Front Public Health 2016: 4: 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ware NC, Wyatt MA, Asiimwe S et al How home HIV testing and counselling with follow‐up support achieves high testing coverage and linkage to treatment and prevention: a qualitative analysis from Uganda. J Int AIDS Soc 2016: 19: 20929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Qiao S, Li X, Stanton B. Disclosure of parental HIV infection to children: a systematic review of global literature. AIDS Behav 2013: 17: 369–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brown JP, Ngwira B, Tafatatha T, Crampin AC, French N, Koole O. Determinants of time to antiretroviral treatment initiation and subsequent mortality on treatment in a cohort in rural northern Malawi. AIDS Res Ther 2016: 13: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Patel RC, Odoyo J, Anand K et al Facilitators and barriers of antiretroviral therapy initiation among HIV discordant couples in Kenya: qualitative insights from a pre‐exposure prophylaxis implementation study. PLoS ONE 2016: 11: e0168057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nakigozi G, Atuyambe L, Kamya M et al A qualitative study of barriers to enrollment into free HIV care: perspectives of never‐in‐care HIV‐positive patients and providers in Rakai, Uganda. Biomed Res Int 2013: 2013: 470245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Brown LB, Havlir DV, Ayieko J et al High levels of retention in care with streamlined care and universal test and treat in East Africa. AIDS 2016: 30: 2855–2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fox MP, Rosen S. Systematic review of retention of pediatric patients on HIV treatment in low and middle‐income countries 2008‐2013. AIDS 2015: 29: 493–502. [DOI] [PubMed] [Google Scholar]


