Abstract
The intrinsic limits of conventional cancer therapies prompted the development and application of various nanotechnologies for more effective and safer cancer treatment, herein referred to as cancer nanomedicine. Considerable technological success has been achieved in this field, but the main obstacles to nanomedicine becoming a new paradigm in cancer therapy stem from the complexities and heterogeneity of tumour biology, an incomplete understanding of nano–bio interactions and the challenges regarding chemistry, manufacturing and controls required for clinical translation and commercialization. This Review highlights the progress, challenges and opportunities in cancer nanomedicine and discusses novel engineering approaches that capitalize on our growing understanding of tumour biology and nano–bio interactions to develop more effective nanotherapeutics for cancer patients.
The growing interest in applying nanotechnology to cancer is largely attributable to its uniquely appealing features for drug delivery, diagnosis and imaging, synthetic vaccine development and miniature medical devices, as well as the therapeutic nature of some nanomaterials themselves1–6 (BOX 1). Nanotherapies that incorporate some of these features (for example, improved circulation and reduced toxicity) are already in use today, and others show great promise in clinical development, with definitive results expected in the near future. Several therapeutic nanoparticle (NP) platforms, such as liposomes, albumin NPs and polymeric micelles, have been approved for cancer treatment, and many other nanotechnology-enabled therapeutic modalities are under clinical investigation, including chemotherapy, hyperthermia, radiation therapy, gene or RNA interference (RNAi) therapy and immunotherapy (TABLE 1).
Box 1. Distinctive features of nanotechnology in oncological applications.
Improvement of the drug therapeutic index by increasing efficacy and/or reducing toxicities
Targeted delivery of drugs in a tissue-, cell- or organelle-specific manner
Enhancement of the pharmaceutical properties (for example, stability, solubility, circulating half-life and tumour accumulation) of therapeutic molecules
Enabling of sustained or stimulus-triggered drug release
Facilitation of the delivery of biomacromolecular drugs (for example, DNA, small interfering RNA (siRNA), mRNA and protein) to intracellular sites of action
Co-delivery of multiple drugs to improve therapeutic efficacy and overcome drug resistance, by providing more precise control of the spatiotemporal exposure of each drug and the delivery of appropriate drug ratio to the target of interest
Transcytosis of drugs across tight epithelial and endothelial barriers (for example, gastrointestinal tract and the blood–brain barrier)
More sensitive cancer diagnosis and imaging
Visualization of sites of drug delivery by combining therapeutic agents with imaging modalities, and/or real-time feedback on the in vivo efficacy of a therapeutic agent
Provision of new approaches for the development of synthetic vaccines
Miniaturized medical devices for cancer diagnosis, drug screening and delivery
Inherent therapeutic properties of some nanomaterials (for example, gold nanoshells and nanorods, and iron oxide nanoparticles) upon stimulation
Table 1.
Examples of clinical-stage nanomedicines for cancer therapy
| Therapy modality |
Generic name and/or proprietary name |
Nanotechnology platform |
Active pharmaceutical ingredients |
Cancer type | Status | Refs |
|---|---|---|---|---|---|---|
| Chemotherapy: non-targeted delivery | Liposomal doxorubicin (Doxil) | Pegylated liposome | Doxorubicin | HIV-related Kaposi sarcoma, ovarian cancer, and multiple myeloma | Approved by FDA | 6 |
| Liposomal daunorubicin (DaunoXome) | Liposome | Daunorubicin | HIV-related Kaposi sarcoma | Approved by FDA | 6 | |
| Liposomal vincristine (Marqibo) | Liposome | Vincristine sulfate | Acute lymphoblastic leukaemia | Approved by FDA | 6 | |
| Liposomal irinotecan (Onivyde or MM-398) | Pegylated liposome | Irinotecan | Post-gemcitabine metastatic pancreatic cancer | Approved by FDA | 230 | |
| Liposomal doxorubicin (Myocet) | Liposome | Doxorubicin | Metastatic breast cancer | Approved in Europe and Canada | 6 | |
| Mifamurtide (Mepact) | Liposome | Muramyl tripeptide phosphatidyl-ethanolamine | Nonmetastatic, resectable osteosarcoma | Approved in Europe | 6 | |
| Nab-paclitaxel (Abraxane) | Albumin NP | Paclitaxel | Breast, lung and pancreatic cancer | Approved by FDA | 6 | |
| SMANCS | Polymer conjugate | Neocarzinostatin | Liver and renal cancer | Approved in Japan | 6 | |
| Polymeric micelle paclitaxel (Genexol-PM) | Polymeric micelle | Paclitaxel | Breast cancer and NSCLC | Approved in Korea | 6 | |
| Liposomal cisplatin (Lipoplatin) | Pegylated liposome | Cisplatin | NSCLC | Phase III | 231 | |
| NK-105 | Polymeric micelle | Paclitaxel | Metastatic or recurrent breast cancer | Phase III | 232 | |
| Liposomal paclitaxel (EndoTAG-1) | Liposome | Paclitaxel | Pancreatic cancer, liver metastases and HER2 negative and triple-negative breast cancer | Phase II | 233–236 | |
| Nab-rapamycin (ABI-009) | Albumin NP | Rapamycin | Advanced malignant PEComa and advanced cancer with mTOR mutations | Phase II | 237,238 | |
| CRLX 101 | Polymeric NP | Camptothecin | NSCLC, metastatic renal cell carcinoma and recurrent ovarian, tubal or peritoneal cancer | Phase II | 239–241 | |
| Chemotherapy: targeted delivery | MM-302 | HER2 targeting liposome | Doxorubicin | HER2-positive breast cancer | Phase II/III | 242 |
| BIND-014 | PSMA-targeting polymeric NP | Docetaxel | NSCLC and mCRPC | Phase II | 243–245 | |
| MBP-426 | TfR targeting liposome | Oxaliplatin | Gastric, oesophageal and gastro-oesophageal adenocarcinoma | Phase I/II | 246 | |
| Anti EGFR immunoliposomes loaded with doxorubicin | EGFR targeting liposome | Doxorubicin | Solid tumours | Phase I | 247 | |
| Chemotherapy: stimuli-responsive delivery | ThermoDox | Liposome | Doxorubicin | Hepatocellular carcinoma | Phase III | 248 |
| Chemotherapy: combinatorial delivery | Liposomal cytarabine–daunorubicin (CPX-351 or Vyxeos) | Liposome | Cytarabine and daunorubicin (5:1) | High-risk acute myeloid leukaemia | Phase III | 249 |
| CPX-1 | Liposome | Irinotecan and floxuridine (1:1) | Advanced colorectal cancer | Phase II | 250 | |
| Hyperthermia | NanoTherm | Iron oxide NP | NA | Glioblastoma | Approved in Europe | 6 |
| AuroLase | Silica core with a gold nanoshell | NA | Head and neck cancer, and primary and metastatic lung tumours | Pilot study | 251,252 | |
| Radiotherapy | NBTXR3 | Hafnium oxide NP | NA | Adult soft tissue sarcoma | Phase II/III | 253 |
| Gene or RNAi therapy | SGT53 | TfR targeting liposome | Plasmid encoding normal human wild-type p53 DNA | Recurrent glioblastoma and metastatic pancreatic cancer | Phase II | 254,255 |
| PNT2258 | Liposome | DNA oligonucleotide against BCL-2 | Relapsed or refractory non-Hodgkin lymphoma and diffuse large B-cell lymphoma | Phase II | 256,257 | |
| SNS01-T | Polyethylenimine NP | siRNA against eIF5A and plasmid expressing eIF5A K50R | Relapsed or refractory B cell malignancies | Phase I/II | 258 | |
| Atu027 | Liposome | siRNA against protein kinase N3 | Advanced or metastatic pancreatic cancer | Phase I/II | 259 | |
| TKM-080301 | Lipid NP | siRNA against PLK1 | Neuroendocrine tumours, adrenocortical carcinoma and advanced hepatocellular carcinoma | Phase I/II | 260,261 | |
| DCR MYC | Lipid NP | Dicer-substrate siRNA against MYC | Hepatocellular carcinoma | Phase I/II | 262 | |
| MRX34 | Liposome | miR 34 mimic | Primary liver cancer, solid tumours and haematological malignancies | Phase I | 263 | |
| CALAA-01 | TfR targeting polymeric NP | siRNA against ribonucleotide reductase M2 | Solid tumours | Phase I | 227 | |
| ALN-VSP02 | Lipid NP | siRNAs against KSP and VEGFA | Solid tumours | Phase I | 264,265 | |
| siRNA EPHA2 DOPC | Liposome | siRNA against EPHA2 | Advanced cancers | Phase I | 266 | |
| pbi shRNA STMN1 LP | Lipid NP | shRNA against stathmin 1 | Advanced and/or metastatic cancer | Phase I | 267 | |
| Immunotherapy | Tecemotide | Liposome | MUC1 antigen | NSCLC | Phase III | 268 |
| dHER2 + AS15 | Liposome | Recombinant HER2 (dHER2) antigen and AS15 adjuvant | Metastatic breast cancer | Phase I/II | 269 | |
| DPX-0907 | Liposome | Multi-tumour associated antigens | HLA-A2-positive advanced stage ovarian, breast and prostate cancer | Phase I | 270 | |
| Lipovaxin-MM | Liposome | Melanoma antigens | Malignant melanoma | Phase I | 271 | |
| JVRS 100 | Lipid NP | Plasmid DNA | Relapsed or refractory leukaemia | Phase I | 272 | |
| CYT 6091 | Colloidal gold NP | TNF | Advanced solid tumours | Phase I | 273 |
EGFR, epidermal growth factor receptor; eIF5A, eukaryotic initiation factor 5A; EPHA2, ephrin type A receptor 2; FDA, US Food and Drug Administration; HLA A2, human leukocyte antigen A2; KSP, kinesin spindle protein (also known as KIF11); mCRPC, metastatic castration resistant prostate cancer; miR, microRNA; mTOR, mammalian target of rapamycin; MUC1, membrane bound mucin 1; NA, not applicable; nab, nanoparticle albumin bound; NP, nanoparticle; NSCLC, non small cell lung cancer; PEComa, perivascular epithelioid cell tumours; PEG, poly(ethylene glycol); PLK1, polo like kinase 1; PSMA, prostate specific membrane antigen; RNAi, RNA interference; shRNA, short hairpin RNA; siRNA, small interfering RNA; SMANCS, poly(styrene co maleic acid) conjugated neocarzinostatin; TfR, transferrin receptor; TNF, tumour necrosis factor; VEGFA, vascular endothelial growth factor A.
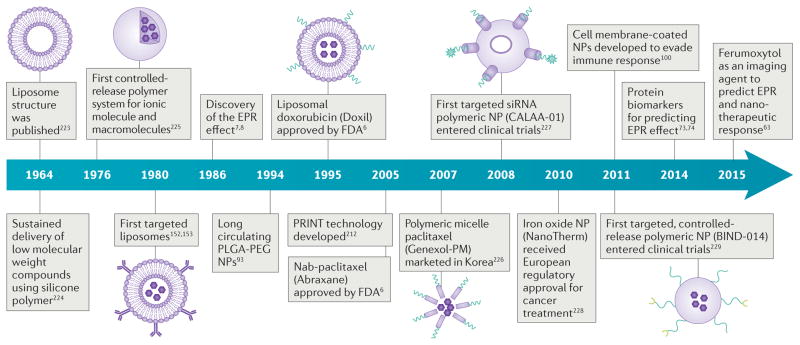
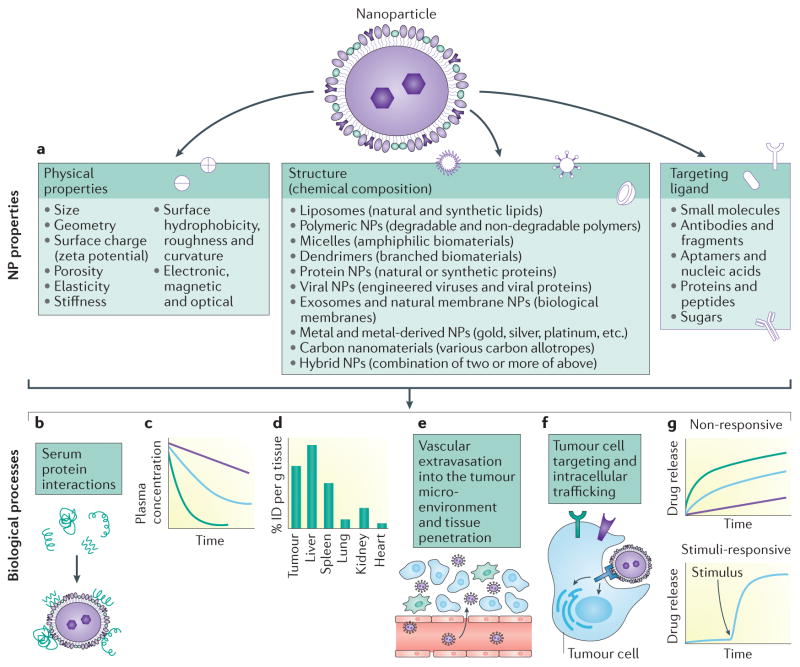
Along with enormous progress in the field of cancer nanomedicine (FIG. 1), we have also gradually realized the challenges and opportunities that lie ahead. Foremost, the complexity and the heterogeneity of tumours make it clear that careful patient selection is required to identify those most likely to benefit from a given nanotherapy. This is analogous to the targeted therapies approved or under development for use in specific biomarker-defined patient populations. Most therapeutic NPs for solid tumour treatment are administered systemically; they accumulate in the tumour through the enhanced permeability and retention (EPR) effect7–10, which is generally thought to be the product of leaky tumour vasculature and poor lymphatic drainage. However, this interpretation of EPR is somewhat oversimplified, as multiple biological steps in the systemic delivery of NPs can influence the effect, such as NP–protein interaction, blood circulation, extravasation into and interaction with the perivascular tumour microenvironment (TME), tumour tissue penetration and tumour cell internalization. In turn, NP properties (for example, size, geometry, surface features, elasticity, stiffness, porosity, composition and targeting ligand) can influence these biological processes, thus determining the EPR effect and therapeutic outcomes (FIG. 2). Nevertheless, it is important to point out that most of our current understanding of NP behaviour in vivo is based on animal data, and its translation to NP behaviour in humans remains largely unexplored. Although several studies have examined the pharmacokinetics (PK) of nanotherapeutics across species in preclinical and clinical studies11–13, relatively few have correlated data across species to determine whether and how NP safety and efficacy in humans can be better predicted from preclinical animal models.
Figure 1. Historical timeline of major developments in the field of cancer nanomedicine.
EPR, enhanced permeability and retention; FDA, US Food and Drug Administration; nab, nanoparticle albumin bound; NP, nanoparticle; PLGA-PEG, poly(D,L-lactic-co-glycolic acid)-b poly(ethylene glycol); PRINT, particle replication in non wetting template; siRNA, small interfering RNA.
Figure 2. The impact of nanoparticle properties on systemic delivery to tumours.
Nanoparticles (NPs) can be made from different materials and have various physicochemical properties (for example, size, geometry, surface features, elasticity and stiffness, among others) and can be modified with a myriad of targeting ligands of different surface density (part a). NP properties affect the biological processes involved in the delivery to tumour tissues, including interactions with serum proteins (part b), blood circulation (part c), biodistribution (part d), extravasation to perivascular tumour microenvironment through the leaky tumour vessels and penetration within the tumour tissue (part e), and tumour cell targeting and intracellular trafficking (part f). NPs can also be designed to control the release profile of payloads (part g). ID, injected dose.
This Review aims to identify gaps in our understanding of why cancer nanomedicine has yet to fulfil its promise in prolonging patient survival, and to offer an overview of our current grasp of tumour biology and nano–bio interactions as they relate to maximization of the impact of cancer nanotherapeutics. Given the presumed crucial role of EPR, we present recent progress in exploring this effect and identifying markers to predict responses to nanotherapies, and in developing new strategies to enhance systemic NP delivery for more pronounced EPR and therapeutic benefit. We also examine the fundamentals behind the development of nanotechnologies to target the TME, which has such an important role in tumour progression and metastasis14,15, and lastly, provide our perspective on challenges to the clinical translation of cancer nanomedicines.
Arsenal of nanomedicine platforms
Nanotechnology has made important contributions to oncology over the past several decades (FIG. 1; TABLE 1). Liposomes (for example, liposomal doxorubicin (LD); Doxil and Myocet) were the first class of therapeutic NPs to receive clinical approval for cancer treatment16, and along with other lipid-based NPs, still represent a large proportion of clinical-stage nanotherapeutics. Although encapsulating drugs in liposomes has been broadly shown to improve PK and biodistribution, as yet no marketed liposomal therapeutic agents have exhibited an overall survival (OS) benefit when directly compared with the conventional parent drug17. The recent phase III results of liposomal cytarabine–daunorubicin (Vyxeos; also known as CPX-351) compared with the standard of care regimen of cytarabine and daunorubicin in patients with high-risk acute myeloid leukaemia, showed improved OS of 9.56 months versus 5.95 months18. This is encouraging for the field of cancer nanomedicine and regulatory filing for the approval of Vyxeos is projected in late 2016. NP albumin-bound paclitaxel (nab-paclitaxel; Abraxane) was the second class of nanomedicines to be commercialized. The nab platform enables formulation of hydrophobic drugs while largely mitigating the need to use toxic excipients. The result may be a better-tolerated drug that can be used at higher doses and administered more quickly, thus enabling a higher drug Cmax and plasma area under the curve (AUC). Upon intravenous infusion, nab-paclitaxel rapidly dissociates into its albumin and paclitaxel constituents and has not been demonstrated to substantially alter the PK and biodistribution of paclitaxel. Although the every-3-week dosing schedule of nab-paclitaxel is superior to paclitaxel in terms of response rate and time to progression for patients with breast cancer19, a once-per-week dosing schedule did not show similar trends in progression-free survival (PFS) or OS and furthermore, showed increased toxicity20. Polymeric micelles (for example, Genexol-PM21 and NK105 (REF. 22)) and polymeric NPs (for example, CRLX101 (REF. 23), BIND-014 (REF. 11) and AZD-2811 Accurin24) are two newer classes of cancer nanotherapeutic agent. Most recently, disappointing clinical results have been reported for BIND-014, CRLX101 and NK105, underscoring the need to rethink development strategies, including potential patient selection to identify those most likely to respond to nanotherapeutics. Inorganic nanomaterials (for example, gold nanoshell25, iron oxide NP26 and hafnium oxide NP27) are also being investigated for use in cancer patients, with the iron oxide NP-based NanoTherm26 already marketed in Europe for glioblastoma.
More intriguingly, our understanding of nano–bio interactions and the arsenal of nanomedicine platforms are expanding rapidly. The total number of papers related to ‘nanoparticle’ on PubMed nearly doubled every 2 years between 2000 and 2014, surpassing the remarkable rise of the number of publications on ‘monoclonal antibody’ (mAb) in the 1980s. In the case of mAb this translated to the development of important therapeutics, and we expect a similar transformative impact from the rise of nanomedicine in the years to come.
Beyond their widely reported use as carriers for chemotherapeutics, NPs have shown potential for the delivery of various new anticancer therapeutic agents, including molecularly targeted agents24, antisense oligonucleotides28,29, small interfering RNA (siRNA)30–33, mRNA34 and DNA inhibitor oligonucleotides35. Furthermore, the use of viral NPs for therapeutic delivery has been facilitated by genetic and chemical engineering techniques36. Examples include the use of adeno-associated virus, approved by the European Commission for lipoprotein lipase deficiency37, lentivirus currently in various clinical trials for cell-based gene therapy and immunotherapy of various diseases including cancer38, and engineered plant viruses (for example, tobacco mosaic virus and potato virus X) for cancer therapy in animal models39,40. With their endogenous origin and organ tropism, exosomes have also been proposed for carrying anticancer payloads to target tumours41. Lastly, novel inorganic NPs such as nanodiamond42,43 and graphene44,45 have received considerable attention for cancer therapy.
We are also already seeing in-depth innovation in nanomedicine strategies. By integrating diagnostic and therapeutic functions into a single NP formulation, theranostic nanomedicine offers a promising strategy to monitor the PK and accumulation of therapeutics and the progression of disease, giving important insights into heterogeneities both within tumours and between patients for potential personalized treatment46,47. By co-delivering multiple active pharmaceutical ingredients (APIs), NPs have also facilitated synergistic cancer therapy and avoided some mechanisms of drug resistance, as evidenced by the large number of in vivo examples (TABLE 2). In addition to drug delivery, nanotechnology is gaining momentum in the area of cancer immunotherapy. NPs have become increasingly attractive as potent antigen or adjuvant carriers for the development of synthetic vaccines, with enhanced tissue penetration and/or access to lymphatics, preferential uptake by antigen-presenting cells, sustained release of antigens or adjuvants and NP-mediated phagosome escape of antigens for cross-presentation4,48–50.
Table 2.
In vivo examples of nanoparticle-mediated combination therapies for cancer treatment in mouse tumour models
| Nanotechnology platform | Active pharmaceutical ingredients | Therapeutic mechanism | Tumour model | Refs |
|---|---|---|---|---|
| Organic NPs | ||||
| Liposomes or lipid-based NPs | Irinotecan and cisplatin | Combination of chemotherapies | SCLC | 274 |
| Combretastatin and doxorubicin | Combining anti-angiogenesis and chemotherapy | Melanoma | 275 | |
| Doxorubicin and antisense oligonucleotides | Combination of chemotherapy and antisense therapy (targeting MRP1 and BCL 2) | NSCLC | 54 | |
| Vorinostat and siRNA | Combination of chemotherapy and RNAi therapy (targeting MCL1) | Cervical cancer | 276 | |
| Docetaxel and DNA | Combination of chemotherapy and gene therapy using survivin suppressor | Hepatocellular carcinoma | 277 | |
| siRNAs | RNAi therapies against MDM2, MYC and VEGFA | NSCLC | 278 | |
| Oligonucleotide G3139 and D-(KLAKLAK)2 peptide | Combining antisense therapy (targeting BCL-2) and peptide-enhancing apoptosis | Melanoma | 279 | |
| Polymeric micelles or NPs | Doxorubicin and paclitaxel | Combination of chemotherapies | NSCLC | 280 |
| Doxorubicin and disulfiram | Combination of chemotherapy and anti-drug resistance | Drug-resistant breast cancer | 281 | |
| Paclitaxel and siRNAs | Combination of chemotherapy and RNAi therapy (targeting SNAIL and TWIST) | Breast cancer | 282 | |
| Camptothecin and DNA | Combination of chemotherapy and gene therapy using TRAIL encoded plasmid | Colon cancer | 283 | |
| Paclitaxel and DNA | Combination of chemotherapy and gene therapy using IL-12-encoded plasmid | Breast cancer | 284 | |
| siRNAs | RNAi therapies against VEGFA and BCL 2 | Prostate cancer | 285 | |
| Antisense oligonucleotides | Antisense therapies against miRNAs miR 10b and miR 21 | Triple-negative breast cancer | 286 | |
| Lipid–polymer hybrid NPs | Combretastatin and doxorubicin | Combining anti-angiogenesis and chemotherapy | Melanoma and Lewis lung carcinoma | 197 |
| Cisplatin and siRNAs | Combination of chemotherapy and RNAi therapy (targeting REV1 and REV3L) | Prostate and breast cancer | 287 | |
| Doxorubicin and siRNA | Combination of chemotherapy and RNAi therapy against MRP1 | Triple-negative breast cancer | 288 | |
| Doxorubicin and TRAIL | Combination of chemotherapy and cytokine-induced apoptosis | Breast cancer | 289 | |
| TGFβ inhibitor SB505124 and IL-2 | Enhancing tumour immunotherapy | Melanoma | 199 | |
| siRNAs and miRNA | Combination of RNAi therapy (targeting MYC, MDM2 and VEGFA) and miR 34a induced apoptosis | Lung metastasis | 166 | |
| Cisplatin and pyrolipid | Combination of chemotherapy and photodynamic therapy | Head and neck cancer | 290 | |
| Paclitaxel and yittrium-90 | Combination of chemotherapy and radiotherapy | Ovarian intraperitoneal metastasis | 291 | |
| Dendrimers | Doxorubicin and DNA | Combination of chemotherapy and gene therapy using TRAIL encoded plasmid | Liver cancer | 292 |
| Doxorubicin and CpG oligonucleotides | Combination of chemotherapy and immunotherapy | Prostate cancer | 293 | |
| Inorganic NPs | ||||
| Iron oxide NP | Doxorubicin and curcumin | Combination of chemotherapies | Glioma | 294 |
| Graphene | Doxorubicin and TRAIL | Combination of chemotherapy and cytokine-induced apoptosis | NSCLC | 44 |
| Carbon nanotube | siRNA | Combination of hyperthermia and RNAi therapy | Prostate cancer | 295 |
| Gold nanorod | Doxorubicin | Combination of hyperthermia and chemotherapy | Cervical cancer | 296 |
| MoS2 nanosheet | Doxorubicin | Combination of hyperthermia and chemotherapy | Breast cancer | 297 |
IL, interleukin; MCL1, myeloid cell leukaemia 1; MoS2, molybdenum sulfide; miRNA, microRNA; MRP1, multi drug resistance associated protein 1 (also known as ABCC1); NPs, nanoparticles; NSCLC, non small cell lung cancer; RNAi, RNA interference; SCLC, small cell lung cancer; siRNA, small interfering RNA; TGFβ, transforming growth factor-β; TRAIL, tumour necrosis factor (TNF) related apoptosis inducing ligand; VEGFA, vascular endothelial growth factor A.
Nanotechnology may also hold great potential for addressing the shortcomings associated with biologics, including mAbs that are used for cancer immunotherapy. For example, the administration of biologic drugs can induce the formation of antidrug antibodies (ADAs) that may adversely affect their safety and efficacy51. Recently engineered tolerogenic NPs carrying rapamycin were shown to abolish the formation of ADAs for biologics in mice and non-human primates52, and human clinical trials are currently ongoing53. Our expectation is that by gaining a deeper insight into nano–bio interactions and the personalization of nanomedicines, and through the application of nanotechnology to existing and emerging therapeutic modalities, we will begin to realize the true potential of nanomedicine in cancer and beyond.
The EPR effect in predictive nanomedicine
Despite efforts to develop non-invasive administration (for example, oral, pulmonary, nasal and transdermal) of NPs54–56, most cancer nanotherapeutics are delivered intravenously for systemic transport to tumours. The preferential accumulation of NPs in tumours is generally ascribed to defective tumour vessels and impaired lymphatics in the tissue: enhanced permeability of the abnormal tumour microvasculature enables NPs to enter the tumour interstitial space, while suppressed lymphatic drainage causes retention within the tissue. The EPR effect7–10 has become the foundation of NP delivery to solid tumours. Nevertheless, it is increasingly clear that EPR varies substantially between both patients and tumour types, and even within the same patient or tumour type over time. However, little effort has been made to address the effect of EPR on nanotherapeutic efficacy. Several preliminary clinical studies have already suggested the value of stratifying subpopulations of cancer patients according to their likelihood of accumulating NPs through EPR57–59, implying that predictive markers for EPR may have a role in the clinical success of cancer nanotherapies.
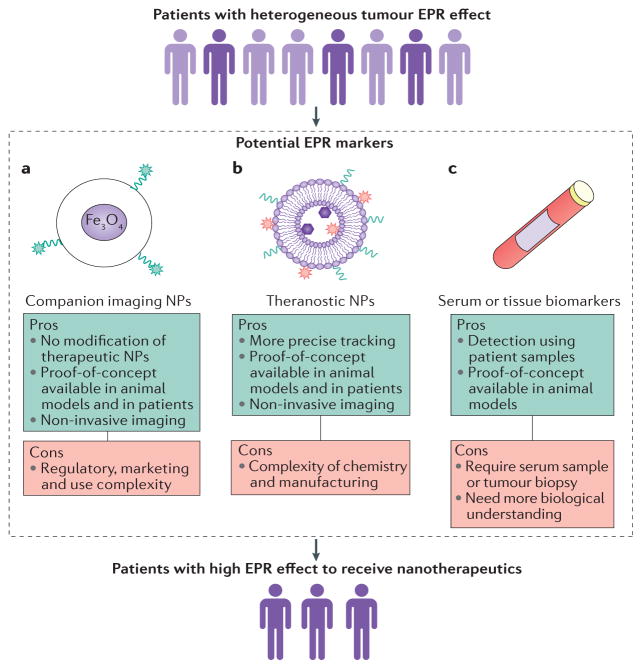
In our previous review of EPR9, we discussed the parameters of the TME, some of which are well characterized for their interactions with NPs, whereas others are considered a ‘black box’ requiring extensive investigation. Recently, there has been growing emphasis on the role of tumour-associated macrophages (TAMs) in NP–TME interactions60–63. TAMs have also been proposed as a reservoir of nanotherapeutics from which the payload is gradually released to neighbouring tumour cells62. Using high-resolution intravital imaging microscopy, a recent work systematically studied the extravasation and intratumoural distribution of two different types of NP63: the clinically approved 30 nm magnetic NP (MNP) ferumoxytol64 and a 90 nm polymeric NP composed of poly(D,L-lactic-co-glycolic acid)-b-poly(ethylene glycol) (PLGA-PEG)11,65,66. Despite differences in both size and composition, MNP and polymeric NP exhibited similar PK after simultaneous intravenous injection, and colocalized to varying degrees in cancer cells and TAMs. Furthermore, after co-administration of MNPs and docetaxel-encapsulated PLGA-PEG NPs, tumour MNP levels showed a significant correlation with NP payload levels. Consequently, the MNP accumulation level successfully predicted the anticancer efficacy of the therapeutic polymeric NPs. A pilot clinical study was also recently initiated to assess ferumoxytol as a marker to predict tumour response to the nanoliposomal irinotecan MM-398 (REFS 57,61,67). Preliminary analysis of lesion size reduction in six cancer patients suggests a positive association with ferumoxytol levels in the lesions at 24 hours57, although a larger study is required for validation. We expect further similar findings to pave the way for companion imaging particles, such as ferumoxytol, to be used in patient selection and predictive nanomedicine (FIG. 3a).
Figure 3. Potential markers for predicting EPR effect and nanotherapeutic efficacy.
a | Companion imaging agents (for example, ferumoxytol nanoparticle (NP)) have been applied to predict the accumulation of poly(D,L-lactic-co-glycolic acid)-b-poly(ethylene glycol) (PLGA-PEG) NP-encapsulated docetaxel and its anticancer activity in solid tumours, and ferumoxytol is currently in clinical trials to determine its feasibility as a predictive marker for the liposomal irinotecan MM-398. b | Therapeutic NPs labelled with imaging agents (for example, radioisotopes), also called theranostic NPs, have been used to monitor their biodistribution and tumour accumulation using various imaging techniques both preclinically and clinically. c | Serum and tissue biomarkers may also serve as surrogate markers for the enhanced permeability and retention (EPR) effect, as suggested by one recent example showing strong correlation of liposome accumulation in tumours with the relative ratio of matrix metalloproteinase 9 (MMP9) to tissue inhibitor of metalloproteinase 1 (TIMP1) in the circulation.
Therapeutic NPs labelled with radioisotopes (for example, 111In, 99mTc, 123I and 64Cu) have also been used to monitor biodistribution and tumour accumulation through non-invasive imaging techniques that include single-photon emission computed tomography (SPECT), computed tomography (CT) and positron emission tomography (PET)58,59,68–71. A recent clinical study demonstrates that high tumour accumulation of LD as determined by quantitative imaging of [99mTc]LD, is positively associated with the response and survival of patients with unresectable pleural mesothelioma treated with a combination of LD and cisplatin59. A high degree of heterogeneity in tumour accumulation was also revealed by PET–CT imaging of 64Cu-loaded liposomes in canine cancers, with six of seven carcinomas compared with only one of four sarcomas displaying high uptake of liposomes72. These results highlight the potential of radioisotope-labelled therapeutic NPs to assess patient suitability for nanotherapies (FIG. 3b). Although incorporation of contrast agents in therapeutic NPs can provide important insights into tumour heterogeneities and EPR, the development of such theranostic NPs may pose additional complexity in terms of design, synthesis, scaling and regulatory considerations47.
Aside from developing imaging NPs as potential markers of therapeutic efficacy, few studies have aimed to identify EPR-predictive gene, protein or cell biomarkers (FIG. 3c). The ratio of matrix metalloproteinase 9 (MMP9) to tissue inhibitor of metalloproteinase 1 (TIMP1) in the circulation, as well as vessel wall collagen content, has been shown to predict EPR for liposomes73,74. Various circulating biomarkers associated with angiogenesis, such as angiogenic factors (for example, vascular endothelial growth factor A (VEGFA), fibroblast growth factor 2 (FGF2), MMP9, interleukin-8 (IL-8), IL-6 and hepatocyte growth factor (HGF)), proteins and peptides (for example, endostatin and tumstatin), and endothelial cells and endothelial progenitor cells, have been described75,76. However, their role, along with other potential biomarkers in predicting EPR, needs further investigation in preclinical and correlative clinical studies.
Enhancing drug delivery to the tumour
NP–protein interactions
When a NP enters a biological environment (for example, blood, interstitial fluid or extracellular matrix (ECM)), its surface is rapidly covered by various biomolecules (typically proteins), leading to the formation of a ‘corona’ (REFS 77–81) (FIG. 2b). The adsorption of proteins alters the particle size, stability and surface properties and, more importantly, provides the NPs with a biological identity that determines the physiological responses they elicit, ranging from cellular uptake and intracellular trafficking to PK, biodistribution and toxicity (FIG. 2c–f). For instance, the binding of opsonins can trigger recognition and clearance by the mononuclear phagocyte system (MPS)79. Conversely, it has also been suggested that a corona rich in dysopsonin proteins (for example, apolipoproteins and albumin), which inhibit phagocytic uptake, could contribute to the stealth effect of NPs82–84. While ligand-functionalized NPs might lose targeting capability when a protein corona forms on their surface85, decoration of NPs with some particular plasma proteins could improve delivery to specific organs. One recent example is the finding that apolipoprotein E is essential for some siRNA lipoplexes to target hepatocytes in vivo86. In contrast, NP–protein interactions in clinical settings can also trigger hypersensitivity reactions in patients by activating the complement system87.
Using various analytical techniques, several studies have extensively characterized the protein corona (for example, its composition, density, conformation, thickness, affinity and dynamics) on certain nanomaterials (for example, gold, silica and polystyrene NPs and liposomes)88. It is now clear that NP–protein interactions are highly dependent on the NP physicochemical properties, exposure time as well as protein source and concentration. However, we still do not have a clear picture of how NP properties (FIG. 2a) and protein adsorption patterns (FIG. 2b) correlate with specific physiological responses (FIG. 2c–f). With high-throughput characterization of the serum protein corona fingerprint in a library of 105 different gold NPs, a quantitative multivariate model was developed to predict interaction of NPs with cells89. Protein corona fingerprints and physicochemical properties of 17 liposomal formulations were recently used to predict multiple biological interactions including cellular uptake and viability of various tumour cells90. Attention was also paid to the crucial role of human disease type on the composition of the protein corona and its effects on cellular uptake and toxicity of NPs91. Nevertheless, most of these studies were focused on NP–protein interactions in vitro, and little effort has been made to study protein corona formation in vivo and its correlation with PK, biodistribution and therapeutic efficacy. It is noteworthy that the very few in vivo evaluations of the protein corona demonstrated significant differences between in vitro and in vivo results92.
Moreover, we think that this field could be further advanced by addressing the following questions. Do we need specific protein-knockout mouse models to validate and explain the observations from in vitro studies and normal mice? In addition to the widely studied proteins in serum, how do the proteins in other biological environments, such as the TME, affect the corona, NP interactions with tumour cells and NP penetration across the tumour ECM? What new techniques will we need to more precisely characterize and quantify the in situ protein corona? We expect that by extending the methodology of quantitative structure–activity relationships to diverse NP platforms and biological responses, such nanomics approaches could facilitate a deeper understanding and better control of the nano–bio interface and prompt more rational design of safe, effective and even patient-specific nanomedicines.
Blood circulation
There is a relationship between blood circulation half-life (FIG. 2c) and the efficiency with which a NP passively extravasates from the microvasculature into the TME. For tissues with relatively large blood flow and particles that efficiently extravasate from the microcirculation, a relatively short blood circulation half-life may be sufficient for the desired accumulation in the tumour. Conversely, for poorly perfused tissues or particles with low extravasation efficiency, a longer circulation half-life may be necessary to enhance exposure in the tumour microvasculature, enabling extravasation to occur progressively.
One major factor limiting circulation time is the non-specific interaction between NPs and serum proteins discussed above, which can promote opsonization and recognition by the MPS. Among various approaches to developing long-circulating NPs, the most widely used is PEG grafting on to the NP surface93,94, such as Doxil, a ‘stealth liposome’ with a circulation half-life of approximately 2 days95. Although pegylation can reduce protein adsorption through hydrophilicity and steric repulsion effects to avoid MPS clearance, such a simplistic view of ‘stealth’ long-circulating particles, which was coined more than 25 years ago (‘Stealth’ being a trademark of Liposome Technology, Inc., Menlo Park, California, USA), is becoming outdated. For example, increasing the density of PEG on a gold NP surface can decrease the amount and change the types of protein that bind to the NPs, reducing macrophage uptake in vitro82. More recently, pegylation of polystyrene NPs has been shown to selectively enrich the adsorption of clusterin to the NP surface, contributing to the decreased nonspecific macrophage uptake in vitro96. The mechanical stiffness and elasticity of particles has also been recognized to influence MPS sequestration97,98.
Another biologically inspired strategy to extend residence time in blood is to modify NPs with ‘self’ markers that prevent normal cells from activating the MPS. The bottom-up approach is chemical conjugation of self markers such as CD47 peptides99 to the NP surface, which can inhibit phagocytosis. The top-down method is to coat NPs with a membrane of erythrocytes, leukocytes or thrombocytes, thus ‘camouflaging’ them to help reduce MPS elimination100–103. Although the circulation half-life of cell membrane-coated NPs is longer than that of ‘bare’ NPs, it is still much shorter than that of the cells themselves. Therefore, more efforts are required to examine the changes in the cell membrane, including its components and elasticity, after the NP surface has been coated.
Extravasation to the TME
Extravasation of NPs from the systemic circulation to tumours (FIG. 2d,e) can be influenced by aberrant tumour vasculature, the perivascular TME and the NP itself. The metabolic demands of rapidly dividing cancer cells result in the formation of neovasculature that is architecturally abnormal and exhibits a ‘leakiness’ distinct from that occurring with inflammation. Unlike the endothelial lining of normal vasculature, which has a turnover of approximately 1,000 days, the endothelium in tumours can double approximately every 10 days104, and the resulting microvasculature does not have clearly defined morphology with distinct venules, arterioles or capillaries. In the case of inflammation, the extravasation of immune cells occurs primarily at the level of the venules105. However, the exact contribution of various segments of the tumour neovasculature to permeability remains poorly understood. In addition to an arsenal of inflammatory mediators such as histamine106,107, the interaction of tight junction modulators such as cationic polymers with endothelium can also induce endothelial contraction and tight junction disassembly, leading to vascular leakiness108. For tumours, both vascular permeability and blood velocity are complex and kinetically variable from segment to segment109. The spatiotemporal changes in vascular permeability can also be in part explained by the recent observation of transient opening and closing of pores, referred to as ‘dynamic vents’, in the walls of tumour vessels110. With an adequate NP circulation half-life, the dynamic vents could potentially improve delivery to tumours (in particular for large NPs). Furthermore, vascular mediators such as nitric oxide and angiotensin II could enhance tumour vascular permeability for more effective NP extravasation10,111. There is also considerable variability in blood viscosity and oncotic pressure in various segments of the vasculature and TME, influencing the movement of NPs into and out of the tumour interstitium. Further studies will help to elucidate the mechanisms involved in NP extravasation into tumours, improving engineering and design schemes for efficient NP accumulation.
The impact of NP physicochemical properties on tumour extravasation and accumulation has also been examined. For example, in hyperpermeable murine colon adenocarcinoma, 30, 50, 70 and 100 nm polymeric micelles all demonstrated similar extravasation and anticancer activity, whereas in hypopermeable pancreatic tumours, only the 30 nm micelles showed sufficient accumulation112. This study further indicates the influence of tumour heterogeneity on nanotherapeutic efficacy, underscoring the need for personalized nanomedicine. Compared with nanospheres, some elongated nanostructures (for example, the nanoworm113 and the nanorod114) improve tumour accumulation. Non-spherical particles also tend to accumulate and adhere to the endothelial cells that line vessel walls better than spherical or quasi-hemispherical particles, enhancing site-specific delivery115,116. However, the effect of NP shape on extravasation can be very complicated, depending on the tumour models studied117.
Other unique strategies have also been proposed to enhance extravasation of NPs to the tumour interstitial space. Exploiting the ‘tumour-tropic’ property of certain cells (for example, mesenchymal stem cells, macrophages and monocytes)118–121, therapeutic NPs can either be attached to the cell surface or loaded into the cells for homing to tumours. Recently, an innovative approach used two types of communicating NP to amplify tumour targeting and accumulation122: the photothermal heating of ‘signalling’ gold nanorods disrupts tumour blood vessels to initiate extravascular coagulation, which can be recognized by the ‘receiving’ NPs in circulation, which bind to the resulting clot.
Tumour penetration
Despite the emphasis on extravasation and accumulation in NP delivery, it is now known that, depending on the therapeutic payload, deep and uniform tumour penetration of nanotherapeutics may also be crucial for optimal outcomes. Studies of macrmolecules (for example, dextrans123 and antibodies124) demonstrate that size and binding affinity affect both diffusion kinetics and depth of tissue penetration. For instance, higher-affinity antibodies that bind to target antigens on cancer cells penetrate tissue less efficiently than lower-affinity antibodies against the same target124. This is because during tissue penetration higher-affinity antibodies tend to bind tightly to the target and become internalized, whereas lower-affinity antibodies tend to bypass their target and thus penetrate deeper. Much can be learned from antibody studies to aid in the design of nanotechnologies for cancer targeting, such as the pros and cons of adding targeting ligands on the NP surface47; although this may enhance cellular uptake and lengthen tissue residence, it may also reduce the depth of tumour penetration.
Therapeutic NPs, nearly always larger than antibodies, tend to become trapped in the ECM around the microvessels from which they extravasate125 (FIG. 2e). Challenges include the physiological barriers intrinsic to the TME, such as the dense interstitial matrix composed of collagen fibres and other proteins, and the elevated interstitial fluid pressure (IFP) induced by hyperpermeability of abnormal vasculature and lack of functional lymphatics deep in the tumour tissue125,126. These in turn reduce convective transport of NPs across the vessel wall and into the interstitial space. Nonspecific uptake by perivascular stromal cells such as TAMs60–63 can further limit the diffusion of nanotherapeutics. It is also noteworthy that mean tumour intercapillary distances generally range from approximately 80 to hundreds of micrometres127–129, presenting another obstacle to NPs reaching tumour cells that are further from vessels.
For enhanced tumour penetration, one possible solution is to tune the physicochemical properties of NPs to penetrate diffusional barriers in the interstitial matrix. Smaller NPs could more readily diffuse throughout the tumour tissue130–132, but very small particles (for example, <5 nm) may be quickly cleared by renal filtration. Moreover, small NPs have a large surface area to volume ratio and a short diffusion distance for encapsulated drugs, limiting their drug-carrying and controlled-release capabilities. Nanorods (15 nm × 54 nm) have also exhibited more rapid tumour penetration than 35 nm nanospheres114, possibly related to their shorter dimension, although both have a 33–35 nm hydrodynamic diameter and nearly identical diffusion rates in water. In addition, surface modification with tumour-specific penetrating peptides, such as the cyclic peptide CRGDK/RGPD/EC (also called iRGD), has also been shown to substantially increase the depth of NP delivery into tumour parenchyma133,134. Further systematic study of NP–TME interactions through real-time in vivo imaging techniques, such as intravital microscopy135, may identify the optimal particle properties for rapid diffusion. TME-modification approaches, such as degrading the tumour ECM and inhibiting the activity of tumour-associated fibroblasts to reduce their production of matrix components, which were previously overviewed136, could likewise assist NPs in permeating tumour tissues.
Recently, an alternative novel multistage delivery strategy has been proposed to address the penetration problem137. Small-molecule drug conjugates (SMDCs)138 and miniaturized biologic drug conjugates (mBDCs), including peptide–drug conjugates139, were developed to address the large size shortcoming of antibody–drug conjugates (ADCs), which limits their tumour tissue penetrability. SMDCs and mBDCs can also enhance retention and cellular uptake by tumours compared with free drug alone. However, their considerable drawbacks include poor PK, which may limit their tumour exposure and therapeutic impact. By incorporating SMDCs and mBDCs into controlled-release polymeric NPs for multistep delivery to tumours, it may be possible to combine the superior PK and tumour accumulation of NPs with the deep penetration and specific tumour cell targeting of released SMDCs and mBDCs for optimal targeted cancer therapy137.
There have also been reports of similar multistage delivery platforms130,140 in which very small NPs (for example, approximately 10 nm quantum dots) are first loaded into large particles, such as approximately 3.5 μm hemispherical mesoporous silicon140 or approximately 100 nm gelatin NPs130. When the large particles reach the tumour vasculature or are exposed to the TME, the released smaller NPs can then readily diffuse throughout the interstitial space of the tumour. Other stimuli-responsive multistage delivery platforms have recently been developed for various hard-to-treat solid tumours141,142.
Cellular uptake and intracellular trafficking
Effective cell internalization may also have an important role in enhancing NP retention, EPR and therapeutic efficacy, as many nanomedicines act on intracellular targets. This is particularly true for biomacromolecule payloads such as those involved in the RNAi pathway (for example, siRNA and microRNA (miRNA)), which require cytosolic delivery for bioactivity143–145. To improve cellular uptake, one approach is to decorate the NPs with targeting ligands that recognize specific receptors on the tumour cell surface9,146,147 (FIG. 2f). Moreover, active targeting is of importance when tissue accumulation does not depend on EPR (for example, vascular targeting)148 or when the delivery of therapeutic agents requires active transcytosis of physiological barriers such as the intestinal mucosa or the blood–brain barrier149–151. Since the concept of active NP targeting was introduced more than 30 years ago152,153, a few examples have made their way into clinical trials9, including targeted liposomes (for example, HER2 (also known as ERBB2) single-chain variable fragment (scFv)-targeted liposome (MM-302)154), the first targeted and controlled-release polymeric NP (BIND-014)11 and the first targeted siRNA NP (CALAA-01)30. Even without targeting ligands, NPs can still be engineered for increased uptake by tumour cells by exploiting size- and shape-dependent cell internalization155,156.
In addition, it may be important to investigate the effect of cancer cell mutations on NP internalization. Pancreatic cancer cells with KRAS mutations show elevated macropinocytosis of proteins such as albumin, and the ability of extracellular albumin to enhance the proliferation of cancer cells after glutamine starvation is also dependent on oncogenic KRAS expression157. This study indicates that macropinocytosis might enhance the uptake of drugs such as paclitaxel when it is bound to albumin, partly explaining the recent success of nab-paclitaxel in treating advanced pancreatic cancer largely driven by oncogenic KRAS158. Whether such an oncogenic mutation effect also applies to NP endocytosis remains unclear. It should also be noted that our current understanding of NP–cell interactions is generally based on in vitro studies, which may not reflect the heterogeneity of tumour cells in vivo. Recent advances in high-resolution cellular in vivo imaging methods have enabled the detailed analysis of single-cell PK and cell-to-cell variability in tumours159–162, and are expected to provide insights into NP interaction with tumour cells and the TME in vivo.
After internalization, NPs must either release their therapeutic payload for diffusion through the cellular compartments to reach the target, or be directed through intracellular trafficking pathways to release therapeutics in the appropriate subcellular location. For cytosolic delivery of biomacromolecules such as siRNA, NP endosomal escape is crucial. Cationic lipid-, lipid-like material- and polymer-based NPs have shown great promise in siRNA delivery163–165. Notably, most RNAi nanotherapeutic agents in clinical trials for cancer treatment are composed of liposomes or lipid NPs (TABLE 1). Although these lipid-based NPs are currently not functionalized with ligands for active targeting, targeted NP delivery could further enhance tumour accumulation and retention and cellular uptake of siRNA144,166. Despite clinical trial success, the efficiency of lipid NP-mediated siRNA release from endosomes remains low (1–2%)167, and approximately 70% of the internalized siRNA may undergo Niemann–Pick type C1-mediated exocytosis168. Thus, alternative strategies will be necessary to develop NP platforms with highly efficient endosomal escape. Besides cytosolic delivery, targeting intracellular organelles such as the nucleus, mitochondria, endoplasmic reticulum and Golgi has also been pursued. Whereas some NPs have been developed for specific uptake by these subcellular compartments169–174, the underlying barriers of organelle membranes to the transport of NPs need to be further explored.
Controlled drug release
An equally important yet often overlooked consideration is that systemically administered NPs may gradually release their payload during circulation (FIG. 2g), such that long-circulating particles with slow tumour extravasation may hold relatively small payloads by the time they reach the TME. Therefore, simultaneous consideration of drug release, NP PK and NP extravasation is required to achieve optimal outcomes.
We think that the design of optimal NP systems requires a deep understanding of several complex parameters: the interplay between NP PK and drug PK, between encapsulated drug and released drug in plasma, between drug Cmax and NP Cmax, between drug plasma AUC and NP plasma AUC; and factors that may differentially affect plasma versus tumour PK and AUC. Conventional small-molecule drugs generally reach their plasma Cmax during the intravenous infusion period, followed by a reduction in plasma drug concentration. Similarly, for drug-encapsulated controlled-release NPs, Cmax will be reached during infusion, yet the plasma concentration of the released drug will in general be very low initially and progressively increase, reaching its Cmax after some period of NP circulation. Importantly, the drug Cmax achieved through release from NPs is unlikely to ever reach the levels achieved with intravenous administration of free drug. Therefore, drug-associated toxicities related to Cmax may be mitigated using NPs. On the other hand, plasma AUC will be relatively similar for free drug and NP-released drug, with one key difference: the AUC of NP-released drug will be generally broad and flat, whereas the AUC for free drug is likely to be peaked, with a tail. The implications are that although certain toxicities may be reduced with the use of NPs, the AUC-related toxicity may be harder to overcome with NPs even though the total dose is released over a longer period of time. When drugs are delivered by NPs, the tumour PK and AUC are dramatically different from those of drugs given in the conventional form, in part because EPR results in differential tumour accumulation of NPs to a greater extent than free drugs and the drug released from NPs localized to tumours can lead to higher tumour drug concentrations over a longer period of time. Most publications demonstrate that NPs enhance delivery of drugs to tumours. A subset of studies show that over time, tumour drug Cmax, PK and/or AUC175–178 are improved compared with conventional dosage. However, these increases in tumour drug accumulation have not always translated into improved patient OS, begging several questions. Does the increase in tumour drug concentration broadly occur in patients or is patient selection needed to identify the subpopulation likely to accumulate NPs? Is increased tumour dose universally beneficial for all drugs or does that depend on the drug?
To precisely control drug release, various stimuli-responsive NPs have been developed and are summarized in a recent review article179. In general, these NPs are designed to recognize subtle environmental changes associated with the TME and tumour cells (for example, pH, redox state and enzymes) or to be activated by external stimuli (for example, heat, light, magnetic field or ultrasound), triggering the release of the payload (FIG. 2g). To some degree, external stimulation enables tailored drug-release profiles with temporal and spatial control. Thermosensitive liposomes (for example, the LD ThermoDox) for heat-mediated drug release are the most advanced clinical stage platform to date. In 2013, ThermoDox failed to meet its primary end point of PFS in a phase III study for hepatocellular carcinoma, and is now undergoing a phase III study with OS as the primary end point (see TABLE 1). More recent stimuli-responsive nanomaterials being investigated include pH- or redox-sensitive polymeric NPs142,180–182, ultrasound-responsive polymer-grafted silica NPs183 and near-infrared light-responsive graphene oxide nanosheets184, among others. The clinical potential of these newer systems remains to be determined.
Overall, with continuous improvements in our understanding of the biological steps in systemic NP delivery, a myriad of new strategies have been developed for enhancing drug delivery to tumours and therapeutic responses. As most of these results are from animal studies, further clinical validation is necessary.
Targeting the TME and the premetastatic niche
As the TME has an important role in tumour development, progression and metastasis and in the emergence of drug resistance, it has also been considered a target for cancer treatment14,15,185. As discussed above, TME modification also offers an alternative strategy for enhancing the tumour accumulation and penetration of NPs107,136. Compared with cancer cells, one advantage of targeting non-tumoural cells in the TME is that they are likely to be more genetically stable and thus less prone to develop drug resistance185. However, targeting non-tumoural cells raises the challenge of achieving a therapeutic effect while minimizing toxicity to normal cells; how TME modification affects tumour growth and metastasis needs more careful examination. Beyond the TME of the primary tumour, the environmental conditions required for metastatic cells to survive and proliferate have also received considerable attention in the development of new therapeutic avenues186. Early interference with the formation of the premetastatic niche may be particularly beneficial in the treatment of malignancies that tend to metastasize.
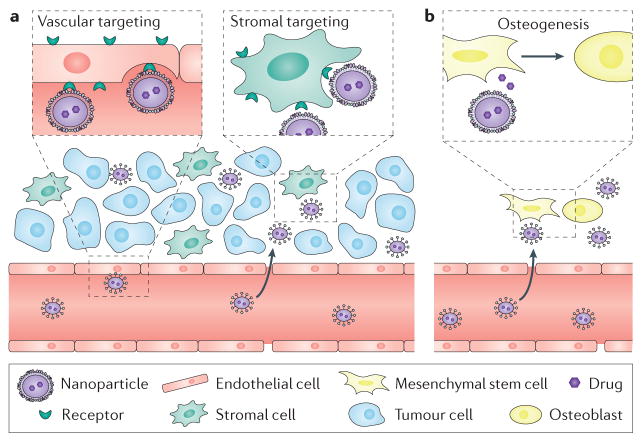
Tumour vasculature
Much effort has focused on NP-mediated selective drug delivery to the tumour vasculature (FIG. 4a), which is crucial to tumour growth and metastasis148. This is commonly achieved by coating NPs with ligands that bind specifically to overexpressed receptors such as αvβ3 integrin187 on the surface of tumour endothelial cells. In vivo studies in mice revealed that inhibiting angiogenesis can cause regression of established tumours or suppression of metastasis188,189. Besides targeted NPs, several non-targeted cationic lipid or polymeric NP platforms have been designed for preferential delivery of siRNA to vascular endothelium190–192. A recent unique formulation called 7C1 specifically reduced the expression of target endothelial genes at low siRNA doses without substantially reducing their expression in pulmonary immune cells, hepatocytes or peritoneal immune cells192. By silencing VEGF receptor 1 (VEGFR1) or delta-like protein 4 (DLL4) involved in angiogenesis, 7C1 RNAi NPs reduced growth and metastasis of Lewis lung carcinoma in mouse models in vivo192. This interesting system could also be used to study how interactions with serum proteins direct nanomaterials to endothelial cells in vivo.
Figure 4. Nanoparticle targeting of the tumour microenvironment and the premetastatic niche.
Targeting of the tumour vasculature or stromal cells in the tumour microenvironment (part a) and the premetastatic microenvironments such as the bone marrow niche, where induction of the osteogenic differentiation of mesenchymal stem cells enhances bone strength and volume (part b). Cell-specific targeting can be achieved via the modification of nanoparticles (NPs) with ligands that bind to specific receptors (for example, αvβ3 integrin and mannose receptor) on the surface of tumour endothelial cells, stromal cells or other target cells. It should be noted that even without targeting ligands, NPs can be engineered for preferential cellular uptake. The payloads released from NPs localized in tumours or premetastatic tissues can also be nonspecifically taken up by these cells.
Stromal cells
Targeting stromal cells such as tumour-associated fibroblasts and macrophages has also been proposed for cancer treatment (FIG. 4a). A unique docetaxel-conjugated NP platform called Cellax significantly depleted α-smooth muscle actin (α-SMA)-expressing fibroblasts, reducing tumour ECM and IFP, increasing vascular permeability and suppressing metastasis193. This effect is presumably through the adsorption of serum albumin on Cellax, followed by specific interaction with α-SMA+ fibroblasts that also express elevated levels of the albumin-binding protein, secreted acidic cysteine-rich glycoprotein (SPARC). Differentiation of TAMs to a pro-tumorigenic or immunosuppressive (M2-like) phenotype has commonly been associated with tumour progression and poor patient outcome194. By inhibiting the activity of signal transducer and activator of transcription 3 (STAT3), hydrazinocurcumin-loaded NPs can ‘re-educate’ TAMs to transform from an M2-like into an antitumorigenic M1 phenotype for inhibited tumour growth195. PEG-sheddable, mannose-modified NPs have also been developed to efficiently target TAMs that have elevated expression of mannose receptors, while minimizing uptake by macrophages of the MPS196. Furthermore, NP-based co-delivery of multiple agents targeting both TME and tumour cells has produced synergistic anticancer effects197–199. However, TME-targeting strategies must be pursued with care, as tumour stroma exhibits bipolar activity in tumorigenesis200.
Metastatic microenvironment
NP delivery to the major sites of metastasis (for example, lungs, liver, lymph nodes, brain and bone) and metastatic tumour cells themselves have been comprehensively discussed elsewhere201. A newly developed system of polymeric micelles formulated from polymer–drug conjugates has shown promising therapeutic efficacy in a mouse model of colon cancer with lung metastasis202, and in a pilot study of one patient with castration-resistant prostate cancer with lung and bone metastases203. Comparatively little effort has been devoted to exploiting nanotechnology to modify the premetastatic microenvironmental niche and suppress tumour growth. In a recent study, a bone-homing polymeric NP platform was engineered for spatiotemporally controlled delivery of therapeutic agents204 (FIG. 4b). After pretreatment with alendronate-conjugated, bortezomib-loaded polymeric NPs, mice showed significantly slower myeloma tumour growth and prolonged survival. The application of such pretreatment strategies for protecting the organs vulnerable to metastasis could be accelerated by revealing which microenvironmental factors control the intravasation, adhesion and growth of metastatic tumour cells and how this is achieved.
Challenges in clinical translation
Controllable and reproducible synthesis
The determination of optimal physicochemical parameters is crucial for the successful development of therapeutic NPs. A considerable amount has been learnt regarding individual factors that can confer effective immune evasion, tumour extravasation and diffusion, cell targeting and internalization, and controlled drug release65,66,78,205,206. Nevertheless, systematic parallel screening of the myriad of NP properties remains difficult, owing to the challenge of rapid, precise and reproducible synthesis of NP libraries with distinct features. Compared with traditional bulk techniques, which generally form NPs with high polydispersity, microfluidic technologies have recently attracted attention for high-speed self-assembly of NPs with narrower size distribution, tunable physical and chemical characteristics and greater batch-to-batch reproducibility207–211. Similarly, particle replication in non-wetting template (PRINT) technology has enabled the synthesis of monodisperse NPs with precise control over size, shape, chemical composition, drug loading and surface properties212,213. Such advances could eventually facilitate NP discovery, analogous to the way high-throughput screening of small molecules advanced drug discovery.
Evaluation and screening
With the rapid emergence of NPs composed of novel biomaterials or nanostructures, in vitro evaluation is important to identify biocompatible candidates before animal testing is pursued. In vitro assays can also improve our understanding of NP–cell interactions. However, as conventional in vitro models using cells cultured in multiwell plates lack the complexity of biological tissues and control over fluid flow, such platforms may not capture the intricate interplay of NPs with physiological barriers. Recent efforts to develop biomimetic ‘organ/tumour-on-a-chip’ tools214–216 may avoid the limitations of current in vitro models. The incorporation of tumour-like spheroids into a microfluidic channel could offer insights into the effects of interstitial flow, cell binding and particle size on NP accumulation and diffusion216. Comparison of NP behaviours in such chip systems with animal models may offer a preview of the potential of these biomimetic microdevices.
To assess in vivo NP performance (for example, PK, biodistribution, efficacy and safety), the use of animal models is obligatory. Whereas some studies have demonstrated PK scaling across different species (including humans) for different nanotherapeutics11–13,32, one well-recognized obstacle is the discrepancy between the efficacies obtained in preclinical studies and the outcomes from clinical trials, in large part owing to the lack of tumour models that can recapitulate human cancers217,218. Diverse animal models are currently available, including cell line-based subcutaneous and orthotopic xenografts, patient-derived xenografts (PDXs) and genetically engineered mouse models (GEMMs). However, no single model can fully reproduce all aspects of human malignancy, and EPR is generally more consistent in animal models than in cancer patients9. Furthermore, considering the major contribution of tumour metastases to cancer mortality, models of human tumour metastasis will be invaluable for the evaluation of EPR and NP penetration and targeting in metastatic tissues compared with primary tumours. The translation of nanotherapeutics may be greatly improved by the development of animal models that mimic closely the heterogeneity and anatomical histology of human tumours, such as high-fidelity PDXs219, humanized mouse models220 and GEMMs with aggressive metastasis221.
Scalable manufacturing
Another challenge to clinical development stems from the escalating complexity in the chemistry, manufacturing and controls (CMC) and good manufacturing practice (GMP) requirements as NP technologies transition from preclinical to clinical development, subsequent commercialization and beyond, as long as the product is on the market. Although the shared goal of CMC and GMP is to assure that a product consistently meets a predetermined standard of quality, they involve different but overlapping approaches and regulation. The scale-up of simple NPs, including liposomes and polymeric systems with small-molecule APIs that have desirable physicochemical properties, can be achieved using manufacturing unit operations readily available and widely used in the pharmaceutical industry. The scale-up of more complex nanomedicines may pose additional CMC and GMP challenges, and require modification of existing unit operations or development of novel manufacturing processes. Examples include nanomedicines that integrate biological targeting ligands or biological components, carry a combination of two or more therapeutics, are formulated through layer-by-layer assembly or comprise multiple functional units such as theranostics or multistage systems.
In general, large-scale and reproducible synthesis will be more difficult when NP formulation involves multiple steps or complicated technologies. Indeed, the transition from laboratory to clinic is nearly always accompanied by the optimization of formulation parameters, or even a change in formulation methods, making forward thinking of scale-up considerations an important aspect of early NP design and engineering. The PRINT technology is amenable to reproducible fabrication of NPs213, yet scaling to kilograms remains to be demonstrated. A coaxial turbulent jet mixer technology, which has the advantages of homogeneity, reproducibility and tunability normally accessible only in microscale mixing techniques such as microfluidics, has recently been developed for mass production of polymeric NPs (potential of ~3 kg/day per channel)222. Although today the mainstay of NP manufacturing remains bulk synthesis, robust and versatile approaches such as PRINT and turbulent jet mixer technologies, which can prepare NPs at throughputs suitable for industrial-scale production, may accelerate clinical translation.
Conclusion
Like most other scientific advances that have revolutionized medicine over the past decades, cancer nanomedicine must also mature before its full impact can be realized. Improving our understanding of tumour heterogeneity and identifying EPR markers will enable selection of patients maximally responsive to nanotherapies. A full understanding of nano–bio interactions, systemic transport of NPs to tumour cells and targeting of NPs to the TME or premetastatic niche will lead to safer and more efficacious nanotherapeutics. Addressing the challenges of controllable, reproducible and scalable NP synthesis, as well as NP screening and evaluation, will facilitate clinical development. Although most approved nanomedicines have used existing drugs as payloads, we expect the next generation of nanomedicines to increasingly incorporate new molecular entities (for example, kinase inhibitors24) and novel classes of therapeutic agent (for example, siRNA, mRNA and gene editing).
In summary, we are rapidly acquiring a much deeper understanding of the challenges and opportunities presented by cancer nanomedicine. This Review has explored the importance of the convergence of nanotechnology and tumour biology for more successful development and clinical translation of nanotherapeutics. We expect that nanomedicines will shift the paradigm of cancer treatment, and that the true goal of cancer nanomedicine — dramatic improvement in patient survival — will become a reality in the foreseeable future.
Acknowledgments
We thank R. Weissleder, R. K. Jain, U. H. von Andrian and M. Mahmoudi for helpful discussions. This work was supported by the grants US National Institutes of Health (NIH) CA151884 (O.C.F.), EB015419 (O.C.F.), R00CA160350 (J.S.) and CA200900 (J.S.); US Department of Defense (DoD) Prostate Cancer Research Program (PCRP) Synergistic Idea Development Award W81XWH-15-1-0728 (O.C.F. and J.S.); David Koch–Prostate Cancer Foundation (PCF) Award in Nanotherapeutics (O.C.F. and P.W.K.); Movember–PCF Challenge Award (O.C.F. and J.S.); PCF Young Investigator Award (J.S.); and National Research Foundation of Korea (K1A1A2048701) (O.C.F.).
Glossary
- Nanoparticle (NP)
Particle of any shape with dimensions in the 1–100 nm range, as defined by the International Union of Pure and Applied Chemistry (IUPAC). Despite this size restriction, the term nanoparticles commonly applies to structures that are up to several hundred nanometres in size, although key is that design of the nanostructure produces a unique function and property.
- Enhanced permeability and retention (EPR) effect
The mechanism resulting from pathophysiological processes (for example, leaky tumour vasculature, poor lymphatic drainage and tumour microenvironment interactions) that leads to the accumulation and retention of nanoparticles or macromolecules in tumours.
- Nano–bio interactions
The interactions between nanoparticles and biological systems (for example, serum proteins, extracellular matrix, cells and organelles) that determine the biological fates of nanoparticles, such as circulation half-life, biodistribution, tumour accumulation, tumour cell internalization and tumour microenvironment distribution.
- Excipients
Substances other than the active pharmaceutical ingredient (API) that are included in the manufacturing process of a medication or are contained in a finished pharmaceutical product dosage form.
- Cmax
The maximum serum concentration that a drug or nanoparticle achieves after administration.
- Area under the curve (AUC)
The area between the curve and the x-axis in a plot of drug or nanoparticle blood plasma concentration against time.
- Payloads
The therapeutic or diagnostic agents carried by nanoparticles.
- Opsonins
Plasma proteins (for example, immunoglobulins, complement proteins and fibrinogen) that coat a foreign particle to facilitate its uptake and destruction by phagocytic cells.
- Mononuclear phagocyte system (MPS)
Part of the immune system composed of scavenging monocytes and macrophages, located in reticular connective tissue surrounding, for example, the liver, spleen, lung and bone marrow.
- Nanomics
The collective study and characterization of the interactions between nanomaterials and biological systems.
- Circulation half-life
The period required for drugs or nanoparticles in the blood to be reduced by one-half of a given concentration or amount.
- Oncotic pressure
A form of osmotic pressure exerted by colloids in a solution, such as proteins in the plasma of a blood vessel.
- Polydispersity
The heterogeneity of particle or molecule size in a mixture.
Footnotes
Competing interests statement
The authors declare competing interests: see Web version for details.
References
- 1.Ferrari M. Cancer nanotechnology: opportunities and challenges. Nat Rev Cancer. 2005;5:161–171. doi: 10.1038/nrc1566. [DOI] [PubMed] [Google Scholar]
- 2.Peer D, et al. Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol. 2007;2:751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 3.Shi J, Votruba AR, Farokhzad OC, Langer R. Nanotechnology in drug delivery and tissue engineering: from discovery to applications. Nano Lett. 2010;10:3223–3230. doi: 10.1021/nl102184c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swartz MA, Hirosue S, Hubbell JA. Engineering approaches to immunotherapy. Sci Transl Med. 2012;4:148rv9. doi: 10.1126/scitranslmed.3003763. [DOI] [PubMed] [Google Scholar]
- 5.Kearney CJ, Mooney DJ. Macroscale delivery systems for molecular and cellular payloads. Nat Mater. 2013;12:1004–1017. doi: 10.1038/nmat3758. [DOI] [PubMed] [Google Scholar]
- 6.Smith AD. Big moment for nanotech: oncology therapeutics poised for a leap. OncLive. 2013 http://www.onclive.com/publications/Oncology-live/2013/June-2013/Big-Moment-for-Nanotech-Oncology-Therapeutics-Poised-for-a-Leap.
- 7.Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986;46:6387–6392. This paper described the EPR effect in cancer, which has become the foundational underpinning for the delivery of NPs and macromolecules to solid tumours. [PubMed] [Google Scholar]
- 8.Gerlowski LE, Jain RK. Microvascular permeability of normal and neoplastic tissues. Microvasc Res. 1986;31:288–305. doi: 10.1016/0026-2862(86)90018-x. This study demonstrated higher microvascular permeability of macromolecules into tumours than into normal tissues, providing a rational basis for the use of large-size therapeutic agents in cancer treatment. [DOI] [PubMed] [Google Scholar]
- 9.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv Drug Deliv Rev. 2014;66:2–25. doi: 10.1016/j.addr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maeda H. Toward a full understanding of the EPR effect in primary and metastatic tumors as well as issues related to its heterogeneity. Adv Drug Deliv Rev. 2015;91:3–6. doi: 10.1016/j.addr.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Hrkach J, et al. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci Transl Med. 2012;4:128ra39. doi: 10.1126/scitranslmed.3003651. First-in-human testing of a targeted, controlled-release polymeric NP for cancer chemotherapy. [DOI] [PubMed] [Google Scholar]
- 12.Eliasof S, et al. Correlating preclinical animal studies and human clinical trials of a multifunctional, polymeric nanoparticle. Proc Natl Acad Sci USA. 2013;110:15127–15132. doi: 10.1073/pnas.1309566110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zuckerman JE, et al. Correlating animal and human phase Ia/Ib clinical data with CALAA-01, a targeted, polymer-based nanoparticle containing siRNA. Proc Natl Acad Sci USA. 2014;111:11449–11454. doi: 10.1073/pnas.1411393111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joyce JA. Therapeutic targeting of the tumor microenvironment. Cancer Cell. 2005;7:513–520. doi: 10.1016/j.ccr.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 15.Meads MB, Gatenby RA, Dalton WS. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat Rev Cancer. 2009;9:665–674. doi: 10.1038/nrc2714. [DOI] [PubMed] [Google Scholar]
- 16.Barenholz Y. Doxil®—the first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160:117–134. doi: 10.1016/j.jconrel.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 17.Petersen GH, Alzghari SK, Chee W, Sankari SS, La-Beck NM. Meta-analysis of clinical and preclinical studies comparing the anticancer efficacy of liposomal versus conventional non-liposomal doxorubicin. J Control Release. 2016;232:255–264. doi: 10.1016/j.jconrel.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 18.Celator Pharmaceuticals, Inc. Celator announces phase 3 trial for VYXEOS™ (CPX-351) in patients with high-risk acute myeloid leukemia demonstrates statistically significant improvement in overall survival. prnewswire. 2016 http://www.prnewswire.com/news-releases/celator-announces-phase-3-trial-for-vyxeos-cpx-351-in-patients-with-high-risk-acute-myeloid-leukemia-demonstrates-statistically-significant-improvement-in-overall-survival-300235620.html.
- 19.Gradishar WJ, et al. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol. 2005;23:7794–7803. doi: 10.1200/JCO.2005.04.937. [DOI] [PubMed] [Google Scholar]
- 20.Rugo HS, et al. Randomized phase III trial of paclitaxel once per week compared with nanoparticle albumin-bound nab-paclitaxel once per week or ixabepilone with bevacizumab as first-line chemotherapy for locally recurrent or metastatic breast cancer: CALGB 40502/NCCTG N063H (Alliance) J Clin Oncol. 2015;33:2361–2369. doi: 10.1200/JCO.2014.59.5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahn HK, et al. A phase II trial of Cremorphor EL-free paclitaxel (Genexol-PM) and gemcitabine in patients with advanced non-small cell lung cancer. Cancer Chemother Pharmacol. 2014;74:277–282. doi: 10.1007/s00280-014-2498-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kato K, et al. Phase II study of NK105, a paclitaxel-incorporating micellar nanoparticle, for previously treated advanced or recurrent gastric cancer. Invest New Drugs. 2012;30:1621–1627. doi: 10.1007/s10637-011-9709-2. [DOI] [PubMed] [Google Scholar]
- 23.Clark AJ, et al. CRLX101 nanoparticles localize in human tumors and not in adjacent, nonneoplastic tissue after intravenous dosing. Proc Natl Acad Sci USA. 2016;113:3850–3854. doi: 10.1073/pnas.1603018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ashton S, et al. Aurora kinase inhibitor nanoparticles target tumors with favorable therapeutic index in vivo. Sci Transl Med. 2016;8:325ra17. doi: 10.1126/scitranslmed.aad2355. [DOI] [PubMed] [Google Scholar]
- 25.Hirsch LR, et al. Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic resonance guidance. Proc Natl Acad Sci USA. 2003;100:13549–13554. doi: 10.1073/pnas.2232479100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maier-Hauff K, et al. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. J Neurooncol. 2011;103:317–324. doi: 10.1007/s11060-010-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maggiorella L, et al. Nanoscale radiotherapy with hafnium oxide nanoparticles. Future Oncol. 2012;8:1167–1181. doi: 10.2217/fon.12.96. [DOI] [PubMed] [Google Scholar]
- 28.Dritschilo A, et al. Phase I study of liposome-encapsulated c-raf antisense oligodeoxyribonucleotide infusion in combination with radiation therapy in patients with advanced malignancies. Clin Cancer Res. 2006;12:1251–1259. doi: 10.1158/1078-0432.CCR-05-1260. [DOI] [PubMed] [Google Scholar]
- 29.Elazar V, et al. Sustained delivery and efficacy of polymeric nanoparticles containing osteopontin and bone sialoprotein antisenses in rats with breast cancer bone metastasis. Int J Cancer. 2010;126:1749–1760. doi: 10.1002/ijc.24890. [DOI] [PubMed] [Google Scholar]
- 30.Davis ME, et al. Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature. 2010;464:1067–1070. doi: 10.1038/nature08956. This study reported the first therapeutic knockdown in humans by polymeric NP-based systemic siRNA delivery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tabernero J, et al. First-in-humans trial of an RNA interference therapeutic targeting VEGF and KSP in cancer patients with liver involvement. Cancer Discov. 2013;3:406–417. doi: 10.1158/2159-8290.CD-12-0429. [DOI] [PubMed] [Google Scholar]
- 32.Schultheis B, et al. First-in-human phase I study of the liposomal RNA interference therapeutic Atu027 in patients with advanced solid tumors. J Clin Oncol. 2014;32:4141–4148. doi: 10.1200/JCO.2013.55.0376. [DOI] [PubMed] [Google Scholar]
- 33.Jensen SA, et al. Spherical nucleic acid nanoparticle conjugates as an RNAi-based therapy for glioblastoma. Sci Transl Med. 2013;5:209ra152. doi: 10.1126/scitranslmed.3006839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Islam MA, et al. Biomaterials for mRNA delivery. Biomater Sci. 2015;3:1519–1533. doi: 10.1039/c5bm00198f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tolcher AW, et al. A phase 1 study of the BCL2-targeted deoxyribonucleic acid inhibitor (DNAi) PNT2258 in patients with advanced solid tumors. Cancer Chemother Pharmacol. 2014;73:363–371. doi: 10.1007/s00280-013-2361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yildiz I, Shukla S, Steinmetz NF. Applications of viral nanoparticles in medicine. Curr Opin Biotechnol. 2011;22:901–908. doi: 10.1016/j.copbio.2011.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yla-Herttuala S. Endgame: glybera finally recommended for approval as the first gene therapy drug in the European Union. Mol Ther. 2012;20:1831–1832. doi: 10.1038/mt.2012.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Naldini L. Gene therapy returns to centre stage. Nature. 2015;526:351–360. doi: 10.1038/nature15818. [DOI] [PubMed] [Google Scholar]
- 39.Shukla S, DiFranco NA, Wen AM, Commandeur U, Steinmetz NF. To target or not to target: active versus passive tumor homing of filamentous nanoparticles based on potato virus X. Cell Mol Bioeng. 2015;8:433–444. doi: 10.1007/s12195-015-0388-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Czapar AE, et al. Tobacco mosaic virus delivery of phenanthriplatin for cancer therapy. ACS Nano. 2016;10:4119–4126. doi: 10.1021/acsnano.5b07360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Batrakova EV, Kim MS. Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release. 2015;219:396–405. doi: 10.1016/j.jconrel.2015.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chow EK, et al. Nanodiamond therapeutic delivery agents mediate enhanced chemoresistant tumor treatment. Sci Transl Med. 2011;3:73ra21. doi: 10.1126/scitranslmed.3001713. [DOI] [PubMed] [Google Scholar]
- 43.Mochalin VN, et al. Adsorption of drugs on nanodiamond: toward development of a drug delivery platform. Mol Pharm. 2013;10:3728–3735. doi: 10.1021/mp400213z. [DOI] [PubMed] [Google Scholar]
- 44.Jiang T, et al. Furin-mediated sequential delivery of anticancer cytokine and small-molecule drug shuttled by graphene. Adv Mater. 2015;27:1021–1028. doi: 10.1002/adma.201404498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu Z, Robinson JT, Sun X, Dai H. PEGylated nanographene oxide for delivery of water-insoluble cancer drugs. J Am Chem Soc. 2008;130:10876–10877. doi: 10.1021/ja803688x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi KY, Liu G, Lee S, Chen X. Theranostic nanoplatforms for simultaneous cancer imaging and therapy: current approaches and future perspectives. Nanoscale. 2012;4:330–342. doi: 10.1039/c1nr11277e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng Z, Al Zaki A, Hui JZ, Muzykantov VR, Tsourkas A. Multifunctional nanoparticles: cost versus benefit of adding targeting and imaging capabilities. Science. 2012;338:903–910. doi: 10.1126/science.1226338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith DM, Simon JK, Baker JR., Jr Applications of nanotechnology for immunology. Nat Rev Immunol. 2013;13:592–605. doi: 10.1038/nri3488. A seminal review of various nanotechnologies and nanomaterials for a broad range of immunological applications, including cancer vaccine development. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Irvine DJ, Swartz MA, Szeto GL. Engineering synthetic vaccines using cues from natural immunity. Nat Mater. 2013;12:978–990. doi: 10.1038/nmat3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenthal JA, Chen L, Baker JL, Putnam D, DeLisa MP. Pathogen-like particles: biomimetic vaccine carriers engineered at the nanoscale. Curr Opin Biotechnol. 2014;28:51–58. doi: 10.1016/j.copbio.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Schellekens H. The immunogenicity of therapeutic proteins. Discov Med. 2010;9:560–564. [PubMed] [Google Scholar]
- 52.Kishimoto TK, et al. Improving the efficacy and safety of biologic drugs with tolerogenic nanoparticles. Nat Nanotechnol. 2016 doi: 10.1038/nnano.2016.135. http://dx.doi.org/10.1038/nnano.2016.1135. [DOI] [PubMed]
- 53.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02648269?term.
- 54.Garbuzenko OB, et al. Inhibition of lung tumor growth by complex pulmonary delivery of drugs with oligonucleotides as suppressors of cellular resistance. Proc Natl Acad Sci USA. 2010;107:10737–10742. doi: 10.1073/pnas.1004604107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liechty WB, Caldorera-Moore M, Phillips MA, Schoener C, Peppas NA. Advanced molecular design of biopolymers for transmucosal and intracellular delivery of chemotherapeutic agents and biological therapeutics. J Control Release. 2011;155:119–127. doi: 10.1016/j.jconrel.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yu M, Wu J, Shi J, Farokhzad OC. Nanotechnology for protein delivery: overview and perspectives. J Control Release. 2015 doi: 10.1016/j.jconrel.2015.10.012. http://dx.doi.org/10.1016/j.jconrel.2015.1010.1012. [DOI] [PMC free article] [PubMed]
- 57.Ramanathan RK, et al. Pilot study in patients with advanced solid tumors to evaluate feasibility of ferumoxytol (FMX) as tumor imaging agent prior to MM398, a nanoliposomal irinotecan (nalIRI) Cancer Res. 2014;74(Suppl) abstr. CT224. [Google Scholar]
- 58.Koukourakis MI, et al. Liposomal doxorubicin and conventionally fractionated radiotherapy in the treatment of locally advanced non-small-cell lung cancer and head and neck cancer. J Clin Oncol. 1999;17:3512–3521. doi: 10.1200/JCO.1999.17.11.3512. [DOI] [PubMed] [Google Scholar]
- 59.Arrieta O, et al. High liposomal doxorubicin tumour tissue distribution, as determined by radiopharmaceutical labelling with 99mTc-LD, is associated with the response and survival of patients with unresectable pleural mesothelioma treated with a combination of liposomal doxorubicin and cisplatin. Cancer Chemother Pharmacol. 2014;74:211–215. doi: 10.1007/s00280-014-2477-x. [DOI] [PubMed] [Google Scholar]
- 60.Daldrup-Link HE, et al. MRI of tumor-associated macrophages with clinically applicable iron oxide nanoparticles. Clin Cancer Res. 2011;17:5695–5704. doi: 10.1158/1078-0432.CCR-10-3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kalra AV, et al. Magnetic resonance imaging with an iron oxide nanoparticle demonstrates the preclinical feasibility of predicting intratumoral uptake and activity of MM-398, a nanoliposomal irinotecan (nal-IRI) Cancer Res. 2014;74(Suppl):2065. [Google Scholar]
- 62.Miller MA, et al. Tumour-associated macrophages act as a slow-release reservoir of nano-therapeutic Pt(IV) pro-drug. Nat Commun. 2015;6:8692. doi: 10.1038/ncomms9692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miller MA, et al. Predicting therapeutic nanomedicine efficacy using a companion magnetic resonance imaging nanoparticle. Sci Transl Med. 2015;7:314ra183. doi: 10.1126/scitranslmed.aac6522. This paper reported that imaging nanoprobes can be used to predict the accumulation and efficacy of therapeutic NPs, paving the road for potential patient selection for high EPR and personalized nanomedicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bashir MR, Bhatti L, Marin D, Nelson RC. Emerging applications for ferumoxytol as a contrast agent in MRI. J Magn Reson Imaging. 2015;41:884–898. doi: 10.1002/jmri.24691. [DOI] [PubMed] [Google Scholar]
- 65.Farokhzad OC, et al. Targeted nanoparticle-aptamer bioconjugates for cancer chemotherapy in vivo. Proc Natl Acad Sci USA. 2006;103:6315–6320. doi: 10.1073/pnas.0601755103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gu F, et al. Precise engineering of targeted nanoparticles by using self-assembled biointegrated block copolymers. Proc Natl Acad Sci USA. 2008;105:2586–2591. doi: 10.1073/pnas.0711714105. This paper described the development of self-assembled targeted NPs, enabling the creation and screening of libraries of targeted nanotherapeutics with optimal biophysicochemical properties. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01770353?term.
- 68.Harrington KJ, et al. Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Cancer Res. 2001;7:243–254. [PubMed] [Google Scholar]
- 69.Koukourakis MI, et al. High intratumoural accumulation of stealth liposomal doxorubicin (Caelyx) in glioblastomas and in metastatic brain tumours. Br J Cancer. 2000;83:1281–1286. doi: 10.1054/bjoc.2000.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seymour LW, et al. Hepatic drug targeting: phase I evaluation of polymer-bound doxorubicin. J Clin Oncol. 2002;20:1668–1676. doi: 10.1200/JCO.2002.20.6.1668. [DOI] [PubMed] [Google Scholar]
- 71.Lee H, et al. A gradient-loadable 64Cu-chelator for quantifying tumor deposition kinetics of nanoliposomal therapeutics by positron emission tomography. Nanomedicine. 2015;11:155–165. doi: 10.1016/j.nano.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 72.Hansen AE, et al. Positron emission tomography based elucidation of the enhanced permeability and retention effect in dogs with cancer using copper-64 liposomes. ACS Nano. 2015;9:6985–6995. doi: 10.1021/acsnano.5b01324. [DOI] [PubMed] [Google Scholar]
- 73.Yokoi K, et al. Serum biomarkers for personalization of nanotherapeutics-based therapy in different tumor and organ microenvironments. Cancer Lett. 2014;345:48–55. doi: 10.1016/j.canlet.2013.11.015. This study reported serum biomarkers for the EPR effect in tumours, which may aid in selecting patients with a higher likelihood of NP accumulation and thus therapeutic response. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yokoi K, et al. Capillary-wall collagen as a biophysical marker of nanotherapeutic permeability into the tumor microenvironment. Cancer Res. 2014;74:4239–4246. doi: 10.1158/0008-5472.CAN-13-3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 76.Sessa C, Guibal A, Del Conte G, Ruegg C. Biomarkers of angiogenesis for the development of antiangiogenic therapies in oncology: tools or decorations? Nat Clin Pract Oncol. 2008;5:378–391. doi: 10.1038/ncponc1150. [DOI] [PubMed] [Google Scholar]
- 77.Cedervall T, et al. Understanding the nanoparticle-protein corona using methods to quantify exchange rates and affinities of proteins for nanoparticles. Proc Natl Acad Sci USA. 2007;104:2050–2055. doi: 10.1073/pnas.0608582104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nel AE, et al. Understanding biophysicochemical interactions at the nano–bio interface. Nat Mater. 2009;8:543–557. doi: 10.1038/nmat2442. [DOI] [PubMed] [Google Scholar]
- 79.Mahmoudi M, et al. Protein–nanoparticle interactions: opportunities and challenges. Chem Rev. 2011;111:5610–5637. doi: 10.1021/cr100440g. [DOI] [PubMed] [Google Scholar]
- 80.Monopoli MP, Aberg C, Salvati A, Dawson KA. Biomolecular coronas provide the biological identity of nanosized materials. Nat Nanotechnol. 2012;7:779–786. doi: 10.1038/nnano.2012.207. This article reviewed the basic concept of NP corona and its structure and composition, and highlights how the properties of the corona may affect the biological responses of NPs. [DOI] [PubMed] [Google Scholar]
- 81.Salvador-Morales C, Zhang L, Langer R, Farokhzad OC. Immunocompatibility properties of lipid-polymer hybrid nanoparticles with heterogeneous surface functional groups. Biomaterials. 2009;30:2231–2240. doi: 10.1016/j.biomaterials.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Walkey CD, Olsen JB, Guo H, Emili A, Chan WC. Nanoparticle size and surface chemistry determine serum protein adsorption and macrophage uptake. J Am Chem Soc. 2012;134:2139–2147. doi: 10.1021/ja2084338. [DOI] [PubMed] [Google Scholar]
- 83.Ritz S, et al. Protein corona of nanoparticles: distinct proteins regulate the cellular uptake. Biomacromolecules. 2015;16:1311–1321. doi: 10.1021/acs.biomac.5b00108. [DOI] [PubMed] [Google Scholar]
- 84.Ogawara K, et al. Pre-coating with serum albumin reduces receptor-mediated hepatic disposition of polystyrene nanosphere: implications for rational design of nanoparticles. J Control Release. 2004;100:451–455. doi: 10.1016/j.jconrel.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 85.Salvati A, et al. Transferrin-functionalized nanoparticles lose their targeting capabilities when a biomolecule corona adsorbs on the surface. Nat Nanotechnol. 2013;8:137–143. doi: 10.1038/nnano.2012.237. [DOI] [PubMed] [Google Scholar]
- 86.Dong Y, et al. Lipopeptide nanoparticles for potent and selective siRNA delivery in rodents and nonhuman primates. Proc Natl Acad Sci USA. 2014;111:3955–3960. doi: 10.1073/pnas.1322937111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chanan-Khan A, et al. Complement activation following first exposure to pegylated liposomal doxorubicin (Doxil): possible role in hypersensitivity reactions. Ann Oncol. 2003;14:1430–1437. doi: 10.1093/annonc/mdg374. [DOI] [PubMed] [Google Scholar]
- 88.Walkey CD, Chan WC. Understanding and controlling the interaction of nanomaterials with proteins in a physiological environment. Chem Soc Rev. 2012;41:2780–2799. doi: 10.1039/c1cs15233e. [DOI] [PubMed] [Google Scholar]
- 89.Walkey CD, et al. Protein corona fingerprinting predicts the cellular interaction of gold and silver nanoparticles. ACS Nano. 2014;8:2439–2455. doi: 10.1021/nn406018q. [DOI] [PubMed] [Google Scholar]
- 90.Bigdeli A, et al. Exploring cellular interactions of liposomes using protein corona fingerprints and physicochemical properties. ACS Nano. 2016;10:3723–3737. doi: 10.1021/acsnano.6b00261. [DOI] [PubMed] [Google Scholar]
- 91.Hajipour MJ, Laurent S, Aghaie A, Rezaee F, Mahmoudi M. Personalized protein coronas: a “key” factor at the nanobiointerface. Biomater Sci. 2014;2:1210–1221. doi: 10.1039/c4bm00131a. [DOI] [PubMed] [Google Scholar]
- 92.Sakulkhu U, et al. Ex situ evaluation of the composition of protein corona of intravenously injected superparamagnetic nanoparticles in rats. Nanoscale. 2014;6:11439–11450. doi: 10.1039/c4nr02793k. [DOI] [PubMed] [Google Scholar]
- 93.Gref R, et al. Biodegradable long-circulating polymeric nanospheres. Science. 1994;263:1600–1603. doi: 10.1126/science.8128245. This pioneering work described the development of long-circulating polymeric NPs, which have since been used in several biomedical applications such as drug delivery, medical imaging and RNAi and gene therapy. [DOI] [PubMed] [Google Scholar]
- 94.Knop K, Hoogenboom R, Fischer D, Schubert US. Poly(ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem Int Ed. 2010;49:6288–6308. doi: 10.1002/anie.200902672. [DOI] [PubMed] [Google Scholar]
- 95.Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42:419–436. doi: 10.2165/00003088-200342050-00002. [DOI] [PubMed] [Google Scholar]
- 96.Schottler S, et al. Protein adsorption is required for stealth effect of poly(ethylene glycol)- and poly(phosphoester)-coated nanocarriers. Nat Nanotechnol. 2016;11:372–377. doi: 10.1038/nnano.2015.330. [DOI] [PubMed] [Google Scholar]
- 97.Key J, et al. Soft discoidal polymeric nanoconstructs resist macrophage uptake and enhance vascular targeting in tumors. ACS Nano. 2015;9:11628–11641. doi: 10.1021/acsnano.5b04866. [DOI] [PubMed] [Google Scholar]
- 98.Anselmo AC, et al. Elasticity of nanoparticles influences their blood circulation, phagocytosis, endocytosis, and targeting. ACS Nano. 2015;9:3169–3177. doi: 10.1021/acsnano.5b00147. [DOI] [PubMed] [Google Scholar]
- 99.Rodriguez PL, et al. Minimal “self” peptides that inhibit phagocytic clearance and enhance delivery of nanoparticles. Science. 2013;339:971–975. doi: 10.1126/science.1229568. This paper described a biologically inspired strategy in developing NPs that can reduce MPS recognition for enhanced drug delivery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hu CM, et al. Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform. Proc Natl Acad Sci USA. 2011;108:10980–10985. doi: 10.1073/pnas.1106634108. This article reported a unique biomimetic strategy to extend the systemic circulation of NPs by ‘tricking’ the immune system. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Parodi A, et al. Synthetic nanoparticles functionalized with biomimetic leukocyte membranes possess cell-like functions. Nat Nanotechnol. 2013;8:61–68. doi: 10.1038/nnano.2012.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hu CM, et al. Nanoparticle biointerfacing by platelet membrane cloaking. Nature. 2015;526:118–121. doi: 10.1038/nature15373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hu Q, et al. Anticancer platelet-mimicking nanovehicles. Adv Mater. 2015;27:7043–7050. doi: 10.1002/adma.201503323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hobson B, Denekamp J. Endothelial proliferation in tumours and normal tissues: continuous labelling studies. Br J Cancer. 1984;49:405–413. doi: 10.1038/bjc.1984.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nourshargh S, Alon R. Leukocyte migration into inflamed tissues. Immunity. 2014;41:694–707. doi: 10.1016/j.immuni.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 106.Ashina K, et al. Histamine induces vascular hyperpermeability by increasing blood flow and endothelial barrier disruption in vivo. PLoS ONE. 2015;10:e0132367. doi: 10.1371/journal.pone.0132367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Maeda H, Nakamura H, Fang J. The EPR effect for macromolecular drug delivery to solid tumors: improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv Drug Deliv Rev. 2013;65:71–79. doi: 10.1016/j.addr.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 108.Deli MA. Potential use of tight junction modulators to reversibly open membranous barriers and improve drug delivery. Biochim Biophys Acta. 2009;1788:892–910. doi: 10.1016/j.bbamem.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 109.Thurber GM, Weissleder R. A systems approach for tumor pharmacokinetics. PLoS ONE. 2011;6:e24696. doi: 10.1371/journal.pone.0024696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Matsumoto Y, et al. Vascular bursts enhance permeability of tumour blood vessels and improve nanoparticle delivery. Nat Nanotechnol. 2016;11:533–538. doi: 10.1038/nnano.2015.342. [DOI] [PubMed] [Google Scholar]
- 111.Seki T, Fang J, Maeda H. Enhanced delivery of macromolecular antitumor drugs to tumors by nitroglycerin application. Cancer Sci. 2009;100:2426–2430. doi: 10.1111/j.1349-7006.2009.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cabral H, et al. Accumulation of sub-100 nm polymeric micelles in poorly permeable tumours depends on size. Nat Nanotechnol. 2011;6:815–823. doi: 10.1038/nnano.2011.166. This study highlighted the effect of NP size on accumulation in hypovascular and hypervascular tumours. [DOI] [PubMed] [Google Scholar]
- 113.Park JH, et al. Magnetic iron oxide nanoworms for tumor targeting and imaging. Adv Mater. 2008;20:1630–1635. doi: 10.1002/adma.200800004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chauhan VP, et al. Fluorescent nanorods and nanospheres for real-time in vivo probing of nanoparticle shape-dependent tumor penetration. Angew Chem Int Ed. 2011;50:11417–11420. doi: 10.1002/anie.201104449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gentile F, et al. The effect of shape on the margination dynamics of non-neutrally buoyant particles in two-dimensional shear flows. J Biomech. 2008;41:2312–2318. doi: 10.1016/j.jbiomech.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 116.Kolhar P, et al. Using shape effects to target antibody-coated nanoparticles to lung and brain endothelium. Proc Natl Acad Sci USA. 2013;110:10753–10758. doi: 10.1073/pnas.1308345110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Smith BR, et al. Shape matters: intravital microscopy reveals surprising geometrical dependence for nanoparticles in tumor models of extravasation. Nano Lett. 2012;12:3369–3377. doi: 10.1021/nl204175t. A seminal work on the effect of particle geometry on extravasation and accumulation in different tumour models. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cheng H, et al. Nanoparticulate cellular patches for cell-mediated tumoritropic delivery. ACS Nano. 2010;4:625–631. doi: 10.1021/nn901319y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Roger M, et al. Mesenchymal stem cells as cellular vehicles for delivery of nanoparticles to brain tumors. Biomaterials. 2010;31:8393–8401. doi: 10.1016/j.biomaterials.2010.07.048. [DOI] [PubMed] [Google Scholar]
- 120.Choi MR, et al. A cellular trojan horse for delivery of therapeutic nanoparticles into tumors. Nano Lett. 2007;7:3759–3765. doi: 10.1021/nl072209h. [DOI] [PubMed] [Google Scholar]
- 121.Alizadeh D, Zhang L, Hwang J, Schluep T, Badie B. Tumor-associated macrophages are predominant carriers of cyclodextrin-based nanoparticles into gliomas. Nanomedicine. 2010;6:382–390. doi: 10.1016/j.nano.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.von Maltzahn G, et al. Nanoparticles that communicate in vivo to amplify tumour targeting. Nat Mater. 2011;10:545–552. doi: 10.1038/nmat3049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dreher MR, et al. Tumor vascular permeability, accumulation, and penetration of macromolecular drug carriers. J Natl Cancer Inst. 2006;98:335–344. doi: 10.1093/jnci/djj070. [DOI] [PubMed] [Google Scholar]
- 124.Rudnick SI, et al. Influence of affinity and antigen internalization on the uptake and penetration of anti-HER2 antibodies in solid tumors. Cancer Res. 2011;71:2250–2259. doi: 10.1158/0008-5472.CAN-10-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jain RK, Stylianopoulos T. Delivering nanomedicine to solid tumors. Nat Rev Clin Oncol. 2010;7:653–664. doi: 10.1038/nrclinonc.2010.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jain RK, Baxter LT. Mechanisms of heterogeneous distribution of monoclonal antibodies and other macromolecules in tumors: significance of elevated interstitial pressure. Cancer Res. 1988;48:7022–7032. [PubMed] [Google Scholar]
- 127.Awwad HK, el Naggar M, Mocktar N, Barsoum M. Intercapillary distance measurement as an indicator of hypoxia in carcinoma of the cervix uteri. Int J Radiat Oncol Biol Phys. 1986;12:1329–1333. doi: 10.1016/0360-3016(86)90165-3. [DOI] [PubMed] [Google Scholar]
- 128.Yoshii Y, Sugiyama K. Intercapillary distance in the proliferating area of human glioma. Cancer Res. 1988;48:2938–2941. [PubMed] [Google Scholar]
- 129.West CM, Cooper RA, Loncaster JA, Wilks DP, Bromley M. Tumor vascularity: a histological measure of angiogenesis and hypoxia. Cancer Res. 2001;61:2907–2910. [PubMed] [Google Scholar]
- 130.Wong C, et al. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc Natl Acad Sci USA. 2011;108:2426–2431. doi: 10.1073/pnas.1018382108. This study demonstrated a multistage NP delivery strategy with long circulation for the EPR effect and deep tumour penetration for delivery into the dense collagen matrix of the tumour. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chauhan VP, et al. Normalization of tumour blood vessels improves the delivery of nanomedicines in a size-dependent manner. Nat Nanotechnol. 2012;7:383–388. doi: 10.1038/nnano.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tong R, Chiang HH, Kohane DS. Photoswitchable nanoparticles for in vivo cancer chemotherapy. Proc Natl Acad Sci USA. 2013;110:19048–19053. doi: 10.1073/pnas.1315336110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sugahara KN, et al. Tissue-penetrating delivery of compounds and nanoparticles into tumors. Cancer Cell. 2009;16:510–520. doi: 10.1016/j.ccr.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ren Y, et al. Targeted tumor-penetrating siRNA nanocomplexes for credentialing the ovarian cancer oncogene. ID4 Sci Transl Med. 2012;4:147ra112. doi: 10.1126/scitranslmed.3003778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Pittet MJ, Weissleder R. Intravital imaging. Cell. 2011;147:983–991. doi: 10.1016/j.cell.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chauhan VP, Jain RK. Strategies for advancing cancer nanomedicine. Nat Mater. 2013;12:958–962. doi: 10.1038/nmat3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bilodeau MT, et al. Pentarins: improved tumor targeting through nanoparticle encapsulation of miniaturized biologic drug conjugates. Cancer Res. 2015;75(Suppl) abstr. 3674. [Google Scholar]
- 138.Vlahov IR, Leamon CP. Engineering folate-drug conjugates to target cancer: from chemistry to clinic. Bioconjug Chem. 2012;23:1357–1369. doi: 10.1021/bc2005522. [DOI] [PubMed] [Google Scholar]
- 139.Firer MA, Gellerman G. Targeted drug delivery for cancer therapy: the other side of antibodies. J Hematol Oncol. 2012;5:70. doi: 10.1186/1756-8722-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tasciotti E, et al. Mesoporous silicon particles as a multistage delivery system for imaging and therapeutic applications. Nat Nanotechnol. 2008;3:151–157. doi: 10.1038/nnano.2008.34. [DOI] [PubMed] [Google Scholar]
- 141.Xu R, et al. An injectable nanoparticle generator enhances delivery of cancer therapeutics. Nat Biotechnol. 2016;34:414–418. doi: 10.1038/nbt.3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Li HJ, et al. Stimuli-responsive clustered nanoparticles for improved tumor penetration and therapeutic efficacy. Proc Natl Acad Sci USA. 2016;113:4164–4169. doi: 10.1073/pnas.1522080113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Whitehead KA, Langer R, Anderson DG. Knocking down barriers: advances in siRNA delivery. Nat Rev Drug Discov. 2009;8:129–138. doi: 10.1038/nrd2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Davis ME. The first targeted delivery of siRNA in humans via a self-assembling, cyclodextrin polymer-based nanoparticle: from concept to clinic. Mol Pharm. 2009;6:659–668. doi: 10.1021/mp900015y. [DOI] [PubMed] [Google Scholar]
- 145.Zhu X, et al. Long-circulating siRNA nanoparticles for validating prohibitin1-targeted non-small cell lung cancer treatment. Proc Natl Acad Sci USA. 2015;112:7779–7784. doi: 10.1073/pnas.1505629112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shi J, Xiao Z, Kamaly N, Farokhzad OC. Self-assembled targeted nanoparticles: evolution of technologies and bench to bedside translation. Acc Chem Res. 2011;44:1123–1134. doi: 10.1021/ar200054n. [DOI] [PubMed] [Google Scholar]
- 147.Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3:16–20. doi: 10.1021/nn900002m. [DOI] [PubMed] [Google Scholar]
- 148.Howard M, et al. Vascular targeting of nanocarriers: perplexing aspects of the seemingly straightforward paradigm. ACS Nano. 2014;8:4100–4132. doi: 10.1021/nn500136z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pridgen EM, et al. Transepithelial transport of Fc-targeted nanoparticles by the neonatal fc receptor for oral delivery. Sci Transl Med. 2013;5:213ra167. doi: 10.1126/scitranslmed.3007049. This paper described the development of a novel NP technology that can successfully traverse across the digestive tract, potentially opening up new opportunities in cancer nanomedicine beyond intravenous administration, including oral delivery of anticancer macromolecules. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cheng Y, Morshed RA, Auffinger B, Tobias AL, Lesniak MS. Multifunctional nanoparticles for brain tumor imaging and therapy. Adv Drug Deliv Rev. 2014;66:42–57. doi: 10.1016/j.addr.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhu X, et al. Polymeric nanoparticles amenable to simultaneous installation of exterior targeting and interior therapeutic proteins. Angew Chem Int Ed. 2016;55:3309–3312. doi: 10.1002/anie.201509183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Leserman LD, Barbet J, Kourilsky F, Weinstein JN. Targeting to cells of fluorescent liposomes covalently coupled with monoclonal antibody or protein A. Nature. 1980;288:602–604. doi: 10.1038/288602a0. [DOI] [PubMed] [Google Scholar]
- 153.Heath TD, Fraley RT, Papahdjopoulos D. Antibody targeting of liposomes: cell specificity obtained by conjugation of F(ab’)2 to vesicle surface. Science. 1980;210:539–541. doi: 10.1126/science.7423203. [DOI] [PubMed] [Google Scholar]
- 154.Espelin CW, Leonard SC, Geretti E, Wickham TJ, Hendriks BS. Dual HER2 targeting with trastuzumab and liposomal-encapsulated doxorubicin (MM-302) demonstrates synergistic antitumor activity in breast and gastric cancer. Cancer Res. 2016;76:1517–1527. doi: 10.1158/0008-5472.CAN-15-1518. [DOI] [PubMed] [Google Scholar]
- 155.Gratton SE, et al. The effect of particle design on cellular internalization pathways. Proc Natl Acad Sci USA. 2008;105:11613–11618. doi: 10.1073/pnas.0801763105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Chithrani BD, Ghazani AA, Chan WC. Determining the size and shape dependence of gold nanoparticle uptake into mammalian cells. Nano Lett. 2006;6:662–668. doi: 10.1021/nl052396o. [DOI] [PubMed] [Google Scholar]
- 157.Commisso C, et al. Macropinocytosis of protein is an amino acid supply route in Ras-transformed cells. Nature. 2013;497:633–637. doi: 10.1038/nature12138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Narayanan V, Weekes CD. Nanoparticle albumin-bound (nab)-paclitaxel for the treatment of pancreas ductal adenocarcinoma. Gastrointest Cancer. 2015;5:11–19. [Google Scholar]
- 159.Thurber GM, et al. Single-cell and subcellular pharmacokinetic imaging allows insight into drug action in vivo. Nat Commun. 2013;4:1504. doi: 10.1038/ncomms2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chittajallu DR, et al. In vivo cell-cycle profiling in xenograft tumors by quantitative intravital microscopy. Nat Methods. 2015;12:577–585. doi: 10.1038/nmeth.3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Laughney AM, et al. Single-cell pharmacokinetic imaging reveals a therapeutic strategy to overcome drug resistance to the microtubule inhibitor eribulin. Sci Transl Med. 2014;6:261ra152. doi: 10.1126/scitranslmed.3009318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Dubach JM, et al. In vivo imaging of specific drug-target binding at subcellular resolution. Nat Commun. 2014;5:3946. doi: 10.1038/ncomms4946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kanasty R, Dorkin JR, Vegas A, Anderson D. Delivery materials for siRNA therapeutics. Nat Mater. 2013;12:967–977. doi: 10.1038/nmat3765. [DOI] [PubMed] [Google Scholar]
- 164.Ozpolat B, Sood AK, Lopez-Berestein G. Liposomal siRNA nanocarriers for cancer therapy. Adv Drug Deliv Rev. 2014;66:110–116. doi: 10.1016/j.addr.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zuckerman JE, Davis ME. Clinical experiences with systemically administered siRNA-based therapeutics in cancer. Nat Rev Drug Discov. 2015;14:843–856. doi: 10.1038/nrd4685. [DOI] [PubMed] [Google Scholar]
- 166.Chen Y, Zhu X, Zhang X, Liu B, Huang L. Nanoparticles modified with tumor-targeting scFv deliver siRNA and miRNA for cancer therapy. Mol Ther. 2010;18:1650–1656. doi: 10.1038/mt.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gilleron J, et al. Image-based analysis of lipid nanoparticle-mediated siRNA delivery, intracellular trafficking and endosomal escape. Nat Biotechnol. 2013;31:638–646. doi: 10.1038/nbt.2612. [DOI] [PubMed] [Google Scholar]
- 168.Sahay G, et al. Efficiency of siRNA delivery by lipid nanoparticles is limited by endocytic recycling. Nat Biotechnol. 2013;31:653–658. doi: 10.1038/nbt.2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Xu ZP, et al. Subcellular compartment targeting of layered double hydroxide nanoparticles. J Control Release. 2008;130:86–94. doi: 10.1016/j.jconrel.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 170.Cheng FY, et al. Stabilizer-free poly(lactide-co-glycolide) nanoparticles for multimodal biomedical probes. Biomaterials. 2008;29:2104–2112. doi: 10.1016/j.biomaterials.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 171.Boddapati SV, et al. Mitochondriotropic liposomes. J Liposome Res. 2005;15:49–58. doi: 10.1081/lpr-64958. [DOI] [PubMed] [Google Scholar]
- 172.Boddapati SV, D’Souza GG, Erdogan S, Torchilin VP, Weissig V. Organelle-targeted nanocarriers: specific delivery of liposomal ceramide to mitochondria enhances its cytotoxicity in vitro and in vivo. Nano Lett. 2008;8:2559–2563. doi: 10.1021/nl801908y. [DOI] [PubMed] [Google Scholar]
- 173.Marrache S, Dhar S. Engineering of blended nanoparticle platform for delivery of mitochondria-acting therapeutics. Proc Natl Acad Sci USA. 2012;109:16288–16293. doi: 10.1073/pnas.1210096109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yameen B, et al. Insight into nanoparticle cellular uptake and intracellular targeting. J Control Release. 2014;190:485–499. doi: 10.1016/j.jconrel.2014.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kalra AV, et al. Preclinical activity of nanoliposomal irinotecan is governed by tumor deposition and intratumor prodrug conversion. Cancer Res. 2014;74:7003–7013. doi: 10.1158/0008-5472.CAN-14-0572. [DOI] [PubMed] [Google Scholar]
- 176.Koizumi F, et al. Novel SN-38-incorporating polymeric micelles, NK012, eradicate vascular endothelial growth factor-secreting bulky tumors. Cancer Res. 2006;66:10048–10056. doi: 10.1158/0008-5472.CAN-06-1605. [DOI] [PubMed] [Google Scholar]
- 177.Nakajima TE, et al. Antitumor effect of SN-38-releasing polymeric micelles, NK012, on spontaneous peritoneal metastases from orthotopic gastric cancer in mice compared with irinotecan. Cancer Res. 2008;68:9318–9322. doi: 10.1158/0008-5472.CAN-08-2822. [DOI] [PubMed] [Google Scholar]
- 178.Hamaguchi T, et al. NK105, a paclitaxel-incorporating micellar nanoparticle formulation, can extend in vivo antitumour activity and reduce the neurotoxicity of paclitaxel. Br J Cancer. 2005;92:1240–1246. doi: 10.1038/sj.bjc.6602479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat Mater. 2013;12:991–1003. doi: 10.1038/nmat3776. This article reviewed the different types of stimuli-responsive NPs for controlled drug delivery. [DOI] [PubMed] [Google Scholar]
- 180.Xu X, et al. Ultra-pH-responsive and tumor-penetrating nanoplatform for targeted siRNA delivery with robust anti-cancer efficacy. Angew Chem Int Ed. 2016;55:7091–7094. doi: 10.1002/anie.201601273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wu J, et al. Hydrophobic cysteine poly(disulfide)-based redox-hypersensitive nanoparticle platform for cancer theranostics. Angew Chem Int Ed. 2015;54:9218–9223. doi: 10.1002/anie.201503863. [DOI] [PubMed] [Google Scholar]
- 182.Wang Y, et al. A nanoparticle-based strategy for the imaging of a broad range of tumours by nonlinear amplification of microenvironment signals. Nat Mater. 2014;13:204–212. doi: 10.1038/nmat3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Paris JL, Cabanas MV, Manzano M, Vallet-Regi M. Polymer-grafted mesoporous silica nanoparticles as ultrasound-responsive drug carriers. ACS Nano. 2015;9:11023–11033. doi: 10.1021/acsnano.5b04378. [DOI] [PubMed] [Google Scholar]
- 184.He Q, et al. NIR-responsive on-demand release of CO from metal carbonyl-caged graphene oxide nanomedicine. Adv Mater. 2015;27:6741–6746. doi: 10.1002/adma.201502762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19:1423–1437. doi: 10.1038/nm.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Psaila B, Lyden D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer. 2009;9:285–293. doi: 10.1038/nrc2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Neri D, Bicknell R. Tumour vascular targeting. Nat Rev Cancer. 2005;5:436–446. doi: 10.1038/nrc1627. [DOI] [PubMed] [Google Scholar]
- 188.Murphy EA, et al. Nanoparticle-mediated drug delivery to tumor vasculature suppresses metastasis. Proc Natl Acad Sci USA. 2008;105:9343–9348. doi: 10.1073/pnas.0803728105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hood JD, et al. Tumor regression by targeted gene delivery to the neovasculature. Science. 2002;296:2404–2407. doi: 10.1126/science.1070200. [DOI] [PubMed] [Google Scholar]
- 190.Santel A, et al. RNA interference in the mouse vascular endothelium by systemic administration of siRNA-lipoplexes for cancer therapy. Gene Ther. 2006;13:1360–1370. doi: 10.1038/sj.gt.3302778. [DOI] [PubMed] [Google Scholar]
- 191.Fehring V, et al. Delivery of therapeutic siRNA to the lung endothelium via novel lipoplex formulation DACC. Mol Ther. 2014;22:811–820. doi: 10.1038/mt.2013.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dahlman JE, et al. In vivo endothelial siRNA delivery using polymeric nanoparticles with low molecular weight. Nat Nanotechnol. 2014;9:648–655. doi: 10.1038/nnano.2014.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Murakami M, et al. Docetaxel conjugate nanoparticles that target α-smooth muscle actin-expressing stromal cells suppress breast cancer metastasis. Cancer Res. 2013;73:4862–4871. doi: 10.1158/0008-5472.CAN-13-0062. [DOI] [PubMed] [Google Scholar]
- 194.Mantovani A, Sica A. Macrophages, innate immunity and cancer: balance, tolerance, and diversity. Curr Opin Immunol. 2010;22:231–237. doi: 10.1016/j.coi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 195.Zhang X, et al. Hydrazinocurcumin encapsuled nanoparticles “re-educate” tumor-associated macrophages and exhibit anti-tumor effects on breast cancer following STAT3 suppression. PLoS ONE. 2013;8:e65896. doi: 10.1371/journal.pone.0065896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhu S, Niu M, O’Mary H, Cui Z. Targeting of tumor-associated macrophages made possible by PEG-sheddable, mannose-modified nanoparticles. Mol Pharm. 2013;10:3525–3530. doi: 10.1021/mp400216r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Sengupta S, et al. Temporal targeting of tumour cells and neovasculature with a nanoscale delivery system. Nature. 2005;436:568–572. doi: 10.1038/nature03794. [DOI] [PubMed] [Google Scholar]
- 198.Guo S, et al. Co-delivery of cisplatin and rapamycin for enhanced anticancer therapy through synergistic effects and microenvironment modulation. ACS Nano. 2014;8:4996–5009. doi: 10.1021/nn5010815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Park J, et al. Combination delivery of TGF-β inhibitor and IL-2 by nanoscale liposomal polymeric gels enhances tumour immunotherapy. Nat Mater. 2012;11:895–905. doi: 10.1038/nmat3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Mueller MM, Fusenig NE. Friends or foes—bipolar effects of the tumour stroma in cancer. Nat Rev Cancer. 2004;4:839–849. doi: 10.1038/nrc1477. [DOI] [PubMed] [Google Scholar]
- 201.Schroeder A, et al. Treating metastatic cancer with nanotechnology. Nat Rev Cancer. 2012;12:39–50. doi: 10.1038/nrc3180. This review highlighted the opportunities and challenges in developing nanotechnologies to treat metastatic cancer. [DOI] [PubMed] [Google Scholar]
- 202.Tsukigawa K, et al. Synthesis and therapeutic effect of styrene-maleic acid copolymer-conjugated pirarubicin. Cancer Sci. 2015;106:270–278. doi: 10.1111/cas.12592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Dozono H, et al. HPMA copolymer-conjugated pirarubicin in multimodal treatment of a patient with stage IV prostate cancer and extensive lung and bone metastases. Target Oncol. 2016;11:101–106. doi: 10.1007/s11523-015-0379-4. [DOI] [PubMed] [Google Scholar]
- 204.Swami A, et al. Engineered nanomedicine for myeloma and bone microenvironment targeting. Proc Natl Acad Sci USA. 2014;111:10287–10292. doi: 10.1073/pnas.1401337111. This paper described NPs that target the bone microenvironment as an alternative targeting strategy for cancer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Alexis F, Pridgen E, Molnar LK, Farokhzad OC. Factors affecting the clearance and biodistribution of polymeric nanoparticles. Mol Pharm. 2008;5:505–515. doi: 10.1021/mp800051m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Perrault SD, Walkey C, Jennings T, Fischer HC, Chan WC. Mediating tumor targeting efficiency of nanoparticles through design. Nano Lett. 2009;9:1909–1915. doi: 10.1021/nl900031y. [DOI] [PubMed] [Google Scholar]
- 207.Karnik R, et al. Microfluidic platform for controlled synthesis of polymeric nanoparticles. Nano Lett. 2008;8:2906–2912. doi: 10.1021/nl801736q. [DOI] [PubMed] [Google Scholar]
- 208.Valencia PM, et al. Single-step assembly of homogenous lipid-polymeric and lipid-quantum dot nanoparticles enabled by microfluidic rapid mixing. ACS Nano. 2010;4:1671–1679. doi: 10.1021/nn901433u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rhee M, et al. Synthesis of size-tunable polymeric nanoparticles enabled by 3D hydrodynamic flow focusing in single-layer microchannels. Adv Mater. 2011;23:H79–H83. doi: 10.1002/adma.201004333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chen D, et al. Rapid discovery of potent siRNA-containing lipid nanoparticles enabled by controlled microfluidic formulation. J Am Chem Soc. 2012;134:6948–6951. doi: 10.1021/ja301621z. [DOI] [PubMed] [Google Scholar]
- 211.Kim Y, et al. Mass production and size control of lipid-polymer hybrid nanoparticles through controlled microvortices. Nano Lett. 2012;12:3587–3591. doi: 10.1021/nl301253v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Rolland JP, et al. Direct fabrication and harvesting of monodisperse, shape-specific nanobiomaterials. J Am Chem Soc. 2005;127:10096–10100. doi: 10.1021/ja051977c. [DOI] [PubMed] [Google Scholar]
- 213.Xu J, et al. Future of the particle replication in nonwetting templates (PRINT) technology. Angew Chem Int Ed. 2013;52:6580–6589. doi: 10.1002/anie.201209145. This article reviewed the PRINT technology and its application in the biomedical and material sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Toh YC, et al. A microfluidic 3D hepatocyte chip for drug toxicity testing. Lab Chip. 2009;9:2026–2035. doi: 10.1039/b900912d. [DOI] [PubMed] [Google Scholar]
- 215.Huh D, et al. Reconstituting organ-level lung functions on a chip. Science. 2010;328:1662–1668. doi: 10.1126/science.1188302. This report described the development of ‘organ-on-a-chip’ and its potential for use in screening drugs and nanotherapeutics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Albanese A, Lam AK, Sykes EA, Rocheleau JV, Chan WC. Tumour-on-a-chip provides an optical window into nanoparticle tissue transport. Nat Commun. 2013;4:2718. doi: 10.1038/ncomms3718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Choi SY, et al. Lessons from patient-derived xenografts for better in vitro modeling of human cancer. Adv Drug Deliv Rev. 2014;79–80:222–237. doi: 10.1016/j.addr.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 218.Sharpless NE, Depinho RA. The mighty mouse: genetically engineered mouse models in cancer drug development. Nat Rev Drug Discov. 2006;5:741–754. doi: 10.1038/nrd2110. [DOI] [PubMed] [Google Scholar]
- 219.Lin D, et al. High fidelity patient-derived xenografts for accelerating prostate cancer discovery and drug development. Cancer Res. 2014;74:1272–1283. doi: 10.1158/0008-5472.CAN-13-2921-T. [DOI] [PubMed] [Google Scholar]
- 220.Rongvaux A, et al. Development and function of human innate immune cells in a humanized mouse model. Nat Biotechnol. 2014;32:364–372. doi: 10.1038/nbt.2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Hubbard GK, et al. Combined MYC activation and Pten loss are sufficient to create genomic instability and lethal metastatic prostate cancer. Cancer Res. 2016;76:283–292. doi: 10.1158/0008-5472.CAN-14-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Lim JM, et al. Ultra-high throughput synthesis of nanoparticles with homogeneous size distribution using a coaxial turbulent jet mixer. ACS Nano. 2014;8:6056–6065. doi: 10.1021/nn501371n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bangham AD, Horne RW. Negative staining of phospholipids and their structural modification by surface-active agents as observed in the electron microscope. J Mol Biol. 1964;8:660–668. doi: 10.1016/s0022-2836(64)80115-7. [DOI] [PubMed] [Google Scholar]
- 224.Folkman J, Long DM. The use of silicone rubber as a carrier for prolonged drug therapy. J Surg Res. 1964;4:139–142. doi: 10.1016/s0022-4804(64)80040-8. [DOI] [PubMed] [Google Scholar]
- 225.Langer R, Folkman J. Polymers for the sustained release of proteins and other macromolecules. Nature. 1976;263:797–800. doi: 10.1038/263797a0. [DOI] [PubMed] [Google Scholar]
- 226.Samyang Biopharm. History. SamyangBiopharm. 2016 https://www.samyangbiopharm.com/eng/Aboutus/history.
- 227.US National Library of Medicine. ClinicalTrials.gov. 2013 https://clinicaltrials.gov/ct2/show/NCT00689065?term.
- 228.MagForce. MagForce Nanotechnologies AG receives European regulatory approval for its Nano Cancer® therapy. magforce.de. 2010 http://www.magforce.de/en/presse-investoren/news-events/detail/article/magforce-nanotechnologies-ag-erhaelt-europaeische-zulassung-fuer-die-nano-krebsR-therapie.html.
- 229.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01300533?term.
- 230.Inman S. FDA approves second-line MM-398 regimen for metastatic pancreatic cancer. OncLive. 2015 http://www.onclive.com/web-exclusives/fda-approves-mm-398-regimen-for-metastatic-pancreatic-cancer.
- 231.Stathopoulos GP, et al. Liposomal cisplatin combined with paclitaxel versus cisplatin and paclitaxel in non-small-cell lung cancer: a randomized phase III multicenter trial. Ann Oncol. 2010;21:2227–2232. doi: 10.1093/annonc/mdq234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01644890?term.
- 233.US National Library of Medicine. ClinicalTrials.gov. 2008 doi: 10.1080/15360280801989377. https://clinicaltrials.gov/ct2/show/NCT00377936?term. [DOI] [PubMed]
- 234.US National Library of Medicine. ClinicalTrials.gov. 2010 https://clinicaltrials.gov/ct2/show/NCT00542048?term.
- 235.US National Library of Medicine. ClinicalTrials.gov. 2013 https://clinicaltrials.gov/ct2/show/NCT01537536?term.
- 236.US National Library of Medicine. ClinicalTrials.gov. 2012 https://clinicaltrials.gov/ct2/show/NCT00448305?term.
- 237.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02494570?term.
- 238.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02646319?term.
- 239.US National Library of Medicine. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT01380769?term.
- 240.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02187302?term.
- 241.US National Library of Medicine. ClinicalTrials.gov. 2014 https://clinicaltrials.gov/ct2/show/NCT01652079?term.
- 242.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02213744?term.
- 243.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01792479?term.
- 244.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02283320?term.
- 245.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01812746?term.
- 246.US National Library of Medicine. ClinicalTrials.gov. 2014 https://clinicaltrials.gov/ct2/show/NCT00964080?term.
- 247.US National Library of Medicine. ClinicalTrials.gov. 2014 https://clinicaltrials.gov/ct2/show/NCT01702129?term.
- 248.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02112656?term.
- 249.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01696084?term.
- 250.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT00361842?term.
- 251.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT00848042?term.
- 252.US National Library of Medicine. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT01679470?term.
- 253.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02379845?term.
- 254.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02340156?term.
- 255.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02340117?term.
- 256.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01733238?term.
- 257.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02226965?term.
- 258.US National Library of Medicine. ClinicalTrials.gov. 2014 https://clinicaltrials.gov/ct2/show/NCT01435720?term.
- 259.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01808638?term.
- 260.US National Library of Medicine. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT01262235?term.
- 261.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02191878?term.
- 262.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT02314052?term.
- 263.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01829971?term.
- 264.US National Library of Medicine. ClinicalTrials.gov. 2011 https://clinicaltrials.gov/ct2/show/NCT00882180?term.
- 265.US National Library of Medicine. ClinicalTrials.gov. 2012 https://clinicaltrials.gov/ct2/show/NCT01158079?term.
- 266.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01591356?term.
- 267.US National Library of Medicine. ClinicalTrials.gov. 2016 https://clinicaltrials.gov/ct2/show/NCT01505153?term.
- 268.US National Library of Medicine. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT00409188?term.
- 269.US National Library of Medicine. ClinicalTrials.gov. 2012 https://clinicaltrials.gov/ct2/show/NCT00952692?term.
- 270.US National Library of Medicine. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT01095848?term.
- 271.US National Library of Medicine. ClinicalTrials.gov. 2012 https://clinicaltrials.gov/ct2/show/NCT01052142?term.
- 272.US National Library of Medicine. ClinicalTrials.gov. 2014 https://clinicaltrials.gov/ct2/show/NCT00860522?term.
- 273.US National Library of Medicine. ClinicalTrials.gov. 2012 https://clinicaltrials.gov/ct2/show/NCT00356980?term.
- 274.Tardi PG, et al. Drug ratio-dependent antitumor activity of irinotecan and cisplatin combinations in vitro and in vivo. Mol Cancer Ther. 2009;8:2266–2275. doi: 10.1158/1535-7163.MCT-09-0243. [DOI] [PubMed] [Google Scholar]
- 275.Zhang YF, Wang JC, Bian DY, Zhang X, Zhang Q. Targeted delivery of RGD-modified liposomes encapsulating both combretastatin A-4 and doxorubicin for tumor therapy: in vitro and in vivo studies. Eur J Pharm Biopharm. 2010;74:467–473. doi: 10.1016/j.ejpb.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 276.Shim G, et al. Trilysinoyl oleylamide-based cationic liposomes for systemic co-delivery of siRNA and an anticancer drug. J Control Release. 2011;155:60–66. doi: 10.1016/j.jconrel.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 277.Xu Z, et al. The characteristics and performance of a multifunctional nanoassembly system for the co-delivery of docetaxel and iSur-pDNA in a mouse hepatocellular carcinoma model. Biomaterials. 2010;31:916–922. doi: 10.1016/j.biomaterials.2009.09.103. [DOI] [PubMed] [Google Scholar]
- 278.Yang Y, et al. Nanoparticle delivery of pooled siRNA for effective treatment of non-small cell lung cancer. Mol Pharm. 2012;9:2280–2289. doi: 10.1021/mp300152v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Ko YT, Falcao C, Torchilin VP. Cationic liposomes loaded with proapoptotic peptide D-(KLAKLAK)2 and Bcl-2 antisense oligodeoxynucleotide G3139 for enhanced anticancer therapy. Mol Pharm. 2009;6:971–977. doi: 10.1021/mp900006h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Lv S, et al. Co-delivery of doxorubicin and paclitaxel by PEG-polypeptide nanovehicle for the treatment of non-small cell lung cancer. Biomaterials. 2014;35:6118–6129. doi: 10.1016/j.biomaterials.2014.04.034. [DOI] [PubMed] [Google Scholar]
- 281.Duan X, et al. Smart pH-sensitive and temporal-controlled polymeric micelles for effective combination therapy of doxorubicin and disulfiram. ACS Nano. 2013;7:5858–5869. doi: 10.1021/nn4010796. [DOI] [PubMed] [Google Scholar]
- 282.Tang S, et al. Inhibition of metastasis and growth of breast cancer by pH-sensitive poly (β-amino ester) nanoparticles co-delivering two siRNA and paclitaxel. Biomaterials. 2015;48:1–15. doi: 10.1016/j.biomaterials.2015.01.049. [DOI] [PubMed] [Google Scholar]
- 283.Ediriwickrema A, Zhou J, Deng Y, Saltzman WM. Multi-layered nanoparticles for combination gene and drug delivery to tumors. Biomaterials. 2014;35:9343–9354. doi: 10.1016/j.biomaterials.2014.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Wang Y, Gao S, Ye WH, Yoon HS, Yang YY. Co-delivery of drugs and DNA from cationic core-shell nanoparticles self-assembled from a biodegradable copolymer. Nat Mater. 2006;5:791–796. doi: 10.1038/nmat1737. [DOI] [PubMed] [Google Scholar]
- 285.Lee SJ, et al. Co-delivery of VEGF and Bcl-2 dual-targeted siRNA polymer using a single nanoparticle for synergistic anti-cancer effects in vivo. J Control Release. 2015;220:631–641. doi: 10.1016/j.jconrel.2015.08.032. [DOI] [PubMed] [Google Scholar]
- 286.Devulapally R, et al. Polymer nanoparticles mediated codelivery of antimiR-10b and antimiR-21 for achieving triple negative breast cancer therapy. ACS Nano. 2015;9:2290–2302. doi: 10.1021/nn507465d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Xu X, et al. Enhancing tumor cell response to chemotherapy through nanoparticle-mediated codelivery of siRNA and cisplatin prodrug. Proc Natl Acad Sci USA. 2013;110:18638–18643. doi: 10.1073/pnas.1303958110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Deng ZJ, et al. Layer-by-layer nanoparticles for systemic codelivery of an anticancer drug and siRNA for potential triple-negative breast cancer treatment. ACS Nano. 2013;7:9571–9584. doi: 10.1021/nn4047925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Jiang T, Mo R, Bellotti A, Zhou J, Gu Z. Gel-liposome-mediated co-delivery of anticancer membrane-associated proteins and small-molecule drugs for enhanced therapeutic efficacy. Adv Funct Mater. 2014;24:2295–2304. [Google Scholar]
- 290.Zheng M, et al. Single-step assembly of DOX/ICG loaded lipid—polymer nanoparticles for highly effective chemo-photothermal combination therapy. ACS Nano. 2013;7:2056–2067. doi: 10.1021/nn400334y. [DOI] [PubMed] [Google Scholar]
- 291.Werner ME, et al. Folate-targeted nanoparticle delivery of chemo- and radiotherapeutics for the treatment of ovarian cancer peritoneal metastasis. Biomaterials. 2011;32:8548–8554. doi: 10.1016/j.biomaterials.2011.07.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Han L, et al. Plasmid pORF-hTRAIL and doxorubicin co-delivery targeting to tumor using peptide-conjugated polyamidoamine dendrimer. Biomaterials. 2011;32:1242–1252. doi: 10.1016/j.biomaterials.2010.09.070. [DOI] [PubMed] [Google Scholar]
- 293.Lee IH, et al. Targeted chemoimmunotherapy using drug-loaded aptamer-dendrimer bioconjugates. J Control Release. 2011;155:435–441. doi: 10.1016/j.jconrel.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 294.Fang JH, et al. Magnetic core-shell nanocapsules with dual-targeting capabilities and co-delivery of multiple drugs to treat brain gliomas. Adv Healthc Mater. 2014;3:1250–1260. doi: 10.1002/adhm.201300598. [DOI] [PubMed] [Google Scholar]
- 295.Wang L, et al. Synergistic anticancer effect of RNAi and photothermal therapy mediated by functionalized single-walled carbon nanotubes. Biomaterials. 2013;34:262–274. doi: 10.1016/j.biomaterials.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 296.Xiao Z, et al. DNA self-assembly of targeted near-infrared-responsive gold nanoparticles for cancer thermo-chemotherapy. Angew Chem Int Ed. 2012;51:11853–11857. doi: 10.1002/anie.201204018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Liu T, et al. Drug delivery with PEGylated MoS2 nano-sheets for combined photothermal and chemotherapy of cancer. Adv Mater. 2014;26:3433–3440. doi: 10.1002/adma.201305256. [DOI] [PubMed] [Google Scholar]